Improving Pain Management for long bone fractures
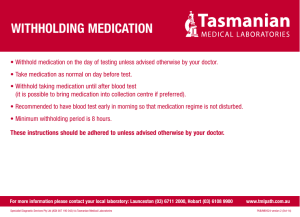
advertisement

Improving Pain Management for long bone fractures in ED through Peer Review and Feedback: a Children’s Hospital Emergency Department QI initiative Manu Madhok, MD, MPH, Meixia Liu, MS Introduction: Pain is the most common cause for seeking care in Emergency Departments (EDs) [1, 2, 3]. As many as three-quarters of ED patients list pain as part of the reason for their presentation. Despite this high prevalence, pain is often poorly treated in ED settings [4, 5, 6, 7] .This finding has been especially pronounced in the subgroup of pediatric patients. Acute long bone fracture is the most common presenting complaint for pediatric ED patients in moderate to severe pain. A clinical report published in Pediatrics in 2004 stated that “optimal pain management requires expeditious pain assessment and the rapid administration of systemic opioid medication to patients in severe pain.” [9]. This report also provided guidance for appropriate goals related to acute pain management. Even with this guidance, the timely and effective elimination of fracture pain in children is often not achieved [10-14]. "Defining Quality Performance Measures for Pediatric Emergency Care” [10,11] is published by Emergency Medical Services for Children (EMSC) program and is in response to “Emergency Care for Children: Growing Pains,” the 2006 Institute of Medicine (IOM) report that recommends the development of national standards for emergency care performance measurement. They recommend utilizing age-appropriate pain scale and show documented improvement in pain score within 90 minutes of arrival. This quality assurance and improvement project seeks to improve the health care of children by optimizing the treatment of pain associated with long bone fractures. Objectives Baseline Data phase 1. To calculate the baseline data for time to pain medication for long bone fractures in children presenting to ED. 2. To improve the time to pain medication for long bone fractures in children presenting to ED by 20% in 12 months with a goal to exceed national benchmark of 60 minutes. Quality Improvement Phase To improve pain management processes by adopting ‘Long Bone Fracture Bundle’. Evaluate if peer pressure affects performance at provider level. Evaluate if the change in pain assessment at triage translates to minimizing the disparity in time to pain medication for minorities. Methods A retrospective chart review of patients with diagnosis of long bone fractures seen in the Children’s Hospitals and Clinics of Minnesota Emergency Department from 1/1/08 to 12/31/10 was accomplished using computerized database. Minneapolis and St. Paul are the Twin Cities of Minnesota and have their own Children’s Hospital campus and see about 45,000 patients per year at each site. The long bone fractures included fractures of humerus, radius-ulna, femur, ankle and tibia-fibula. Time to pain medication was calculated as the time between arrival to ED and medication administration. For each patient encounter multiple data fields were collected including demographic, social and economic indicators along with clinical variables of pain score, type of fracture, type of pain medication, time of day etc. 1 Quality Improvement Initiatives: Based on the results of baseline study, QI measures were initiated to address following issues. The median time to pain medication exceeded national benchmark when data for all patients was analyzed. However, it varied significantly when different variables were analyzed. The study identified three primary opportunities for intervention and improvement: 1.) Whites received medication faster and by IV route when compared to non-whites 2.) Pain medication by IV treatment was fastest but utilized in 54% patients 3.) Certain physicians were faster at administering medication Emergency Department designed ‘Long Bone Fracture Bundle’ to address these discrepancies via an innovative program. It included education at nursing level where assessment and timely treatment of pain was discussed at monthly meetings and daily huddles. The variation in time to pain medication amongst patients was presented and possible explanations were explored. The racial difference for pain tolerance was explored in detail. We attempted to compensate for this difference by considering an additional point on pain score when assessing in triage. This was felt to be not appropriate as pain score recorded is patients’ self reporting of pain on FACES scale. A change in hospital sedation policy was instituted where Intranasal Fentanyl administration was established as analgesia and not sedation. Nurses were educated regarding appropriate monitoring when administering Intranasal Fentanyl and did not need to fill sedation paperwork. This removes hesitancy on using Fentanyl in a new route. Pharmacist provided teaching on new atomizers that need to be connected to syringe when administering intranasal Fentanyl. Physicians were provided their individual data on median time to pain medication and the data of their peers in a blinded fashion. The idea of un-blinding top performers was discussed amongst all providers but not instituted as many factors influence this time which may not be under direct control of treating physician. The data from first quarter was compared to third quarter as all education and interventions were instituted in the second quarter. Statistics Frequency distributions for dichotomous variables such as gender and race, and median (range) for continuous variables such as age were used to describe the data. Non-parametric Mann-Whitney test or Kruskal-Wallis H test were used to compare the time to pain medication administration between different variables as appropriate. Chi-square test was used to compare the dichotomous variables between different groups. All statistical analyses were done using SPSS 15.0. Results of baseline data 2206 patients (Male 1386, Female 820) meeting ICD9 codes and valid data fields were included in data analysis. There was no significant difference in the three years (2008 with756 patients, 2009 with 708 patients and 2010 with 841 patients). The distribution of type of fractures is described below. Humerus Radius/Ulna Femur Tibia/Fibula Ankle 566 1116 162 173 189 2 Median time to Pain medication administration was 50.35 minutes in baseline data. It did not vary significantly over 3 years. 2008: 49.20 min 2009: 51.75 min 2010: 49.20 min Amongst various parameters, It varied significantly with regards to Gender, Race, Language spoken, Insurance status, Triage acuity level, Pain score and Type of Pain medication. (Table 1). The median time to pain medication varied amongst Providers from 35 minutes to 90 minutes. There was no significant difference when interpreter services were used. When Race and Route were studied, non-white patients were less likely to receive IV pain medication when compared to white patients (48.4% vs. 57.8%, p<0.001). Table 1 Clinical Parameters and variability in time to pain medication Clinical parameter Gender Female (n=820) Male (n=1386) Race, White No (n=768) Yes (n=1278) Language, English No (n=300) Yes (n=1906) Arrival Hour 7Am-3PM (n=571) 3PM-11PM (n=1508) 11PM-7AM (n=127) Medicaid No (n=1520) Yes (n=686) Acuity Level Emergent (n=10) Critical (n=1119) Acute (n=324) Urgent (n=737) Non-urgent (n=16) Pain score <=4 (n=684) >4 (n=1374) Route Oral (n=1014) IV/IM (n=1147) Nasal (n=45) Narcotics No (n=987) Yes (n=1211) Minute to pain medication administration P-value 0.003 53.2 (1, 335) 48.4 (0, 460) 0.007 53.4 (1, 460) 48.4 (0, 350) 0.023 53.4 (1, 312) 49.9 (0, 460) 0.004 45.8 (2, 460) 50.6 (0, 452) 56.6 (1, 205) 0.006 48.6 (0, 350) 53.8 (1, 460) <0.001 38.2 (4, 156) 39.2 (0, 460) 62.9 (2, 452) 67.6 (2, 336) 53.6 (34, 210) <0.001 61.3 (1, 452) 45.0 (0, 460) <0.001 62.2 (0, 350) 43.3 (1, 460) 35.1 (4, 220) <0.001 62.5 (0, 318) 43.3 (1, 460) 3 Results of Quality Improvement Phase This hospital’s quality improvement project to improve the time-to-pain medication associated with long bone fractures, racial differences and provider variability took place in second quarter of 2011. A chart review using institutional computerized database was performed for first (Jan-March) quarter and third (June-August) quarter of 2011. It identified 387 pediatric patients with acute long bone fractures. Table 2 lists patient characteristics and other comparisons between Pre and Post groups which showed no difference amongst the two groups. Table 3 shows improvement in median time in minutes to pain medication for various groups by race. Table 4 illustrates change in median time in minutes to pain medication over the course of study time. There was increase in utilization of intranasal Fentanyl from 3.4% in baseline data to 16.2% in pre-intervention and 25.9% in post-intervention periods. There was not enough data to compare change in provider variability because of smaller sample size. However, a new standing order protocol for pain medication is being instituted where a practitioner can activate the treatment in triage and nurse can initiate the pain control in an expedited manner. Table 2 Patient Characteristics and other Comparisons between Pre and Post groups Pre-group (n=132) Post-group (n=255) (Jan-Mar 2011) (Jun-Aug 2011) Gender, male 84 (63.6%) 153 (60.0%) Language, English 115 (87.1%) 215 (84.3%) Race Asian 4 (3.2%) 20 (8.3%) Black/African American 23 (18.5%) 47 (19.5%) Hispanic/Latino 14 (11.3%) 16 (6.6%) White/Caucasian 74 (59.7%) 136 (56.4%) Other 9 (7.3%) 22 (9.1%) Arrival Hour 7AM-3PM 41 (31.1%) 82 (32.2%) 3PM-11PM 87 (65.9%) 148 (58.0%) 11PM-7AM 4 (3.0%) 25 (9.8%) Campus MPLS 70 (53.0%) 126 (49.4%) STP 62 (47.0%) 129 (50.6%) Acuity level Emergent 0 5 (2.0%) Critical 58 (43.9%) 128 (50.2%) Acute 42 (31.8%) 75 (29.4%) Urgent 31 (23.5%) 47 (18.4%) Non-urgent 1 (0.8%) 0 Medicaid 49 (37.1%) 91 (35.7%) Interpreter used 8 (6.1%) 22 (8.6%) Route IV 58 (43.9%) 103 (40.4%) Nasal 20 (15.2%) 61 (23.9%) PO 54 (40.9%) 91 (35.7%) Narcotics 78 (59.5%) 164 (64.3%) White 74 (59.7%) 136 (56.4%) Pain score* 6.0 (1, 10) 7.0 (1, 10) p-value 0.486 0.460 0.208 0.035 0.5 0.082 0.078 0.371 0.129 0.359 0.552 0.325 4 Table 3 Median minutes to pain medication Pre Median time to pain medication n Post p-value Median (range) n Median (range) 57.5 (3, 335) 255 46 (1, 237) 0.008 Other 23 14 74 9 60 (16, 88) 64 (12, 232) 79 (25, 180) 45 (6, 335) 71 (18, 181) 20 47 16 136 22 50.5 (19, 129) 56 (11, 232) 40.5 (1, 141) 45 (4, 237) 42 (14, 190) 0.970 0.059 0.064 0.528 0.174 White Non-white 74 50 45 (6, 335) 67.5 (12, 232) 136 105 45 (4, 237) 49 (1, 232) 0.528 0.004 English Non-English 115 17 55 (6, 335) 64 (31, 232) 215 40 46 (1, 127) 50.5 (11, 141) 0.035 0.06 Asian 3 15 12 56 8 6 (4, 10) 8 (1, 10) 5.5 (2, 10) 6.5 (1, 10) 8 (2, 10) 13 38 14 105 18 4 (1, 10) 8 (1, 10) 6.5 (2, 10) 7 (1, 10) 8.5 (1, 10) 0.364 0.686 0.252 0.440 0.724 Median time to pain 132 medication (min)-overall Race Asian 4 Black/African American Hispanic/Latino White/Caucasian Race Language Pain Score Race Black/African American Hispanic/Latino White/Caucasian Other Table 4 Median minutes to pain medication by admission Month Month Jan Feb Mar Jun Jul Aug n 38 48 46 111 75 69 Median (range) 61 (11, 185) 58.5 (9, 335) 47.5 (6, 214) 49 (5, 232) 48 (1, 237) 39 (4, 204) Conclusion The time to pain medication at Children's Hospital exceeds national benchmark and quality improvement interventions improved time to pain medication for all races. There was an increase in utilization of intranasal Fentanyl after the change in hospital sedation policy. A standing order protocol for pain medication may help expedite the pain medication. The disparity in care based on language, race and insurance status supports need for improvement in these spheres. This difference has also been reported in previous studies. Racial and cultural differences need to be studied further to identify if there is truly a variable tolerance to pain or hesitation to reporting based on socio-cultural factors or health literacy. 5 References: 1.Cordell, W. H., Keene, K. K., Giles, B. K., Jones, J. B., Jones, J. H. and Brizendine, E. J., The high prevalence of pain in emergency medical care, Am J Emerg Med, 2002, 20(3):165-169. 2.Johnston, C. C., Gagnon, A. J., Fullerton, L., Common, C., Ladores, M. and Forlini, S., One-week survey of pain intensity on admission to and discharge from the emergency department: a pilot study, J Emerg Med, 1998, 16(3):377-382. 3.Tanabe, P. and Buschmann, M., A prospective study of ED pain management practices and the patient's perspective, J Emerg Nurs, 1999, 25(3):171-177. 4.Hostetler, M. A., Auinger, P. and Szilagyi, P. G., Parenteral analgesic and sedative use among ED patients in the United States: combined results from the National Hospital Ambulatory Medical Care Survey (NHAMCS) 1992-1997, Am J Emerg Med, 2002, 20(3):139-143. 5.Lewis, L. M., Lasater, L. C. and Brooks, C. B., Are emergency physicians too stingy with analgesics?, South Med J, 1994, 87(1):7-9. 6.Petrack, E. M., Christopher, N. C. and Kriwinsky, J., Pain management in the emergency department: patterns of analgesic utilization, Pediatrics, 1997, 99(5):711-714. 7.Rupp, T. and Delaney, K. A., Inadequate analgesia in emergency medicine, Ann Emerg Med, 2004, 43(4):494-503. 8.Todd, K. H., Ducharme, J., Choiniere, M., Crandall, C. S., Fosnocht, D. E., Homel, P. and Tanabe, P., Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study, J Pain, 2007, 8(6):460-466. 9.Zempsky, W. T. and Cravero, J. P., Relief of pain and anxiety in pediatric patients in emergency medical systems, Pediatrics, 2004, 114(5):1348-1356. 10. http://www.childrensnational.org/EMSC/PubRes/OldToolboxPages/Hospitalbased_Performance_Measures.aspx 11. American Academy of Pediatrics, Committee on Psychosocial Aspects of Child and Family Health; American Pain Society,Task Force on Pain in Infants Children and Adolescents. The assessment and management of acute pain in infants, children,and adolescents. Pediatrics. 2001;108(3):793–797 12. Zempsky WT, Cravero JP; American Academy of Pediatrics,Committee on Pediatric Emergency Medicine and Section on Anesthesiology and Pain Medicine. Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics.2004;114(5):1348–1356 13. Bhargava R, Young KD. Procedural pain management patterns in academic pediatric emergency departments. Acad Emerg Med 2007;14(5):479–482 14. MacLean S, Obispo J, Young KD. The gap between pediatric emergency department procedural pain management treatmentsavailable and actual practice. Pediatr Emerg Care. 2007;23(2):87–93. 6