LECTURE OUTLINE CHAPTER 21
advertisement

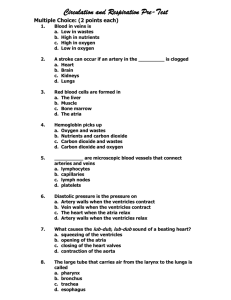
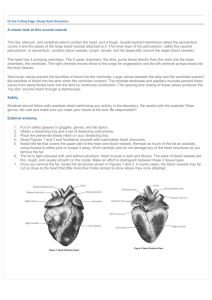
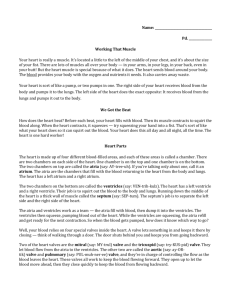
LECTURE OUTLINE CHAPTER 19 Marieb The Cardiovascular System; The Heart Lecture Outline Your heart is about as big as your fist and your aorta is about as big as your thumb- you are proportioned to yourself. (Physical fit is a problem in heart transplants.) I. Location A. in pericardial space B. inside mediastinum C. inside thoracic cavity D. which is the superior portion of the ventral cavity E. in center of chest deep to sternum, apex tipped toward the left; base superior II. Structure A. Pericardium - covering 1. fibrous pericardium - tough, collagenous 2. which is lined by the serous parietal pericardium 3. which encloses the pericardial space 4. serous visceral pericardium adheres to the heart surface 5. also known as the epicardium C. Heart wall 1. epicardium (= visceral pericardium) 2. myocardium = heart muscle – “functional syncytium” a. striated, aerobic, interwoven, autorhythmic b. intercalated discs - gap junctions, strong desmosomes, anchor for myofibrils 3. fibrous skeleton - collagen and elastin a. encircle bases of great vessels b. encircle bases of valves c. isolate atria from ventricles electrically d. reinforce myocardium itself 4. endocardium (epithelium) 5. contains specialized conductive cells D. Superficial anatomy 1. four hollow chambers a. right & left (superior) atria with (de)attached auricles b. right & left (inferior) ventricles 2. base of heart is top with major vessels attached a. superior and inferior venae cavae enter right atrium b. pulmonary veins return to left atrium c. pectinate muscles - interior of atria d interatrial septum - wall between atria 3. apex is inferior point of heart, usually somewhat left of center 1 4. atrioventricular sulci lie between atria & ventricles - sites of coronary arteries and veins from which distributing arteries arise. 5. ventricles a. atrioventricular valves between atria and ventricles b. papillary muscles on interior walls c. trabeculae carnae - scaffolding on interior walls d. moderator band in right only - prevents over distension e. interventricular septum - wall between ventricles f. conus arteriosus - funnel leading from right to pulmonary trunk g. aorta exits from left ventricle through aortic valve E. Internal anatomy 1. atria, thin walled, pectinate muscle internally 2. atria separated by an interatrial septum 3. ventricles – thick walled with trabeculae carneae & papillary muscles right chamber is thinner walled than left 4. ventricles separated by an interventricular septum 5. atria and ventricles separated by atrioventricular valves a. tricuspid on the right b. bicuspid (mitral) on the left 6. valves are restrained by chordae tendinae which are in turn attached to papillary muscles 7. skeleton of the heart is a fibrous ring surrounding the base of all four valves. F. Structure and Function of Valves 1. prevent backflow of blood 2. close passively under blood pressure 3. heart sounds produced by valve closure 4. restrained by chordae tendinae attached to papillary muscles III. Blood flow pattern through the heart A. Blood enters right atrium B. Passes tricuspid valve into right ventricle C. Leaves by way of pulmonary trunk into lungs to be oxygenated D. Passes pulmonary valves on the way to lungs E. Returns from the lung by way of pulmonary veins into the left atrium F. Left atrium past bicuspid valve into left ventricle G. Leaves left ventricle past aortic valve into aorta H. Distributed to rest of the body IV. Coronary circulation A. Coronary arteries from base of aorta, down stream from valve 1. right coronary artery- follows atrioventricular sulcus-supplies right atrium and parts of both ventricles a. atrial branches - supply right atrium b. ventricular branches i. marginal branch ii. posterior interventricular branch 2 iii. branches to conduction system 2. left coronary artery - branches almost immediately to a. circumflex artery - curves left in atrioventricular sulcus b. anterior interventricular branch - follows interventricular sulcus - supplies ventricles with anastomoses B. Cardiac veins - drain myocardium 1. great cardiac vein 2. middle cardiac vein - both empty into coronary sinus in right atrium V. Cardiac cycle The actual physical contraction pattern of the myocardium as determined by the conduction The two atria are in systole and diastole together as are the two ventricles A. Contraction is systole B Relaxation is diastole VI. Conduction system of heart Specialized muscle cells which conduct action potentials to time and synchronize the action of the chambers A. SA (sinoatrial) node -pacemaker, spontaneously depolarizes most rapidly and initiate heart beat, positioned on the back wall of the right atrium , transmits action potential to B. AV (atrioventricular) node - (where the four chambers meet). C. AV (atrioventricular) bundle transmits down the top of the interventricular septum where it divides into two D. Bundle branches, one of which supplies each ventricle where they branch into E. Purkinje fibers which reflect up the external walls of the ventricles and stimulate contraction of cardiac muscle cells as a unit. F. Purkinje fibers extend into papillary muscles as well G. ECG (EKG) - electrical tracing of action potential 1. P wave – depolarization of atria, precedes atrial systole 2. QRS wave is depolarization of ventricles, precedes ventricular systole 3. atrial repolarization also occurs at QRS 4. T wave indicates ventricular repolarization 5. entire sequence takes about 0 .8 sec. VII. Autonomic Control of Heart Rate The heart has dual innervation and the rate and pressure can be accelerated or retarded. A. Norepinephrine - increases both rate and strength of contraction by way of Beta receptors B. Ach decreases both rate and strength of contraction by way of muscarinic receptors C. Cardioacceleratory centers I medulla - sympathetic fibers by release of NE D. Cardioinhibitory centers - reduce rate and pressure by release of ACh 3 by the parasympathetic. E. Sensed by baroreceptors and chemoreceptors 4