Varicose Veins

PATIENT INFORMATION SHEET
Varicose Veins
Varicose veins are abnormal enlarged twisted veins, typically affecting the superficial veins of the legs. Normally, superficial veins have one-‐way valves that help blood to flow back to the heart. If these valves become incompetent
(open and non-‐functioning), blood pools in the veins causing them to become swollen and varicose. Sometimes varicose veins can also arise from structural weaknesses in the vein wall, or from higher than normal blood pressure in the veins.
Varicose veins are a common problem, affecting nearly 20-‐
30% of the population, with women more often affected than men by 2-‐3 times. The most common type of varicose veins is telangectasias. Due to their appearance, they may also be called spider veins, star bursts, thread veins, or matted veins. Varicose veins can be more common in people who are on their feet a lot, women following child birth and those that have a family history of varicose veins.
Symptoms
Some patients experience no symptoms, but choose to see their doctor because they find the cosmetic appearance of varicose veins unsightly. Symptomatic patients may experience:
•
No general anaesthetics’
•
Fantastic success rate
•
Follow up’s are for life via clinic visits and ultrasounds. All follow up's bulk billed.
Treatment is performed using ambulatory phlebectomy, endovenous laser ablation and sclerotherapy. Some patients will require only one of these treatments others may require a combination of 2 -‐ 3 to ensure the best possible outcome.
Treatment Options
Conservative treatment
Patients, who are having mild symptoms such as ache or swelling, are advised to avoid prolonged standing and to try compressive stockings.
• dull ache or pressure in the legs after prolonged standing or walking
• sensation of “heaviness” of the legs
• skin changes (such as itchiness, pigmentation, induration)
• recurrent or persistent ulceration
• inflammation of the vein (phlebitis)
• clots in the vein (thrombosis)
Ambulatory Phlebectomy
The technique of phlebectomy dates back to 56 BC, when
Aulus Cornelius Celcus first described it. Modern ambulatory phlebectomy involves the removal of varicose veins through small cuts in the skin. It is a minor procedure performed using only local anaesthetic that allows the patient to return to normal activities immediately.
The procedure first involves marking out the varicose veins on the patient’s legs. Local anaesthetic is given and small, key-‐hole incisions are made in the skin along the length of the varicose vein. The varicose vein is then extracted by using a special phlebectomy hook to gently tease it out. The incisions made in the skin are small enough (4-‐5mm) that they do not require stitches, and leave only tiny (if any) scars. Afterwards, the patient is required to wear compression stockings for up to 2-‐6 weeks.
Ambulatory phlebectomy is generally very well tolerated.
Complications are rare, but may include skin pigmentation, bruising, skin blisters, dermatitis, and infection. The long term success rate is high with >90% patients reporting no recurrence of their varicose veins.
Benefits of Endovascular WA's treatment
• The treatment is minimally invasive, which means patients walk in walk out.
•
Very little, if no scarring
•
No hospital visit or hospital fees
Endovenous Ablation
Endovenous ablation procedures are able to effectively obliterate the internal vein space with faster recovery and better cosmetic results than surgery. There are currently a number of Endovenous ablation methods available:
EVLT utilises a laser to close the varicose vein. A laser fibre is passed through a small incision in the ankle or knee into the varicose vein.
© 2010 Endovascular WA
221 Stirling Highway, Claremont WA 6010
| T ( 08) 9284 2900 |F (08) 9 384 5725 | E reception@endovascularwa.com.au | W www.endovascularwa.com.au
Once guided into place by ultrasound, the laser is fired, delivering laser energy to the wall of the vein. This causes the blood to boil and damages the vein walls, which fibrose and close off. After the procedure, the patient will need to wear compression bandages for a number of days. This procedure usually only requires local anaesthesia.
EVLT has a high success rate, with >95% patients experiencing an improvement in their symptoms. Patients are able to return to normal activities almost immediately.
One Australian study showed that after 3 years, 80% of patients had veins that remained closed.
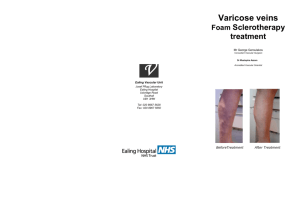
Foam Sclerotherapy
Sclerotherapy involves injecting a chemical agent (a sclerosant) to induce blood vessel scarring and closure.
Sclerotherapy has a long history and has been used to treat varicose veins for over 150 years. The advent of duplex ultrasound and foam sclerosants has marked its return as a simple but effective treatment for varicose veins.
PATIENT INFORMATION SHEET
Varicose Veins
i.
compression stockings ii.
Ensure you have someone to take you to and from the clinic on the day of your procedure (they can even stay with you through the whole procedure) iii.
Make sure you have returned your signed information to our Patients' Service team at reception iv.
Have a shower on the morning of your procedure v.
Wear comfortable loose clothing
Post Procedure Patient Care
You will be provided with post procedure instructions on the day of your procedure. Your doctor will explain all care instructions to you along with nursing staff and answer any questions you may have.
In foam Sclerotherapy, air is mixed with the liquid sclerosant to create foam. When this is injected into the varicose vein (under ultrasound guidance), it displaces the blood within the vein and fills the vein. This causes the vein to spasm and scar.
The vein can be checked with the ultrasound to see if the injection has been successful. The patient is usually asked to wear elastic compression stockings for 1-‐2 weeks after the procedure. No anaesthetic is required for the procedure, and patients are able to return to normal activities straight away.
Foam Sclerotherapy has a good success rate, with 80-‐90% of veins remaining closed after 3 years. To improve the success rate, veins may need to be re-‐injected.
Complications are infrequent but may include skin pigmentation, skin sloughing, vein inflammation, transiently enlarged lymph nodes and allergic reaction. A number of studies are currently being undertaken to determine the best sclerosant and technique, as well as the long term outcomes of foam Sclerotherapy.
Patient Preparation
Prior to a procedure for the treatment of varicose veins, patients are required to complete the following
Making an appointment
Making an appointment to see one of or physicians is easy.
We have two options:
1.
Phone our Claremont clinic on (08) 9284 2900 and you will speak directly to one of our friendly Patients’
Service team members who will book your appoint and answer any of your questions.
2.
Patients can book online by going to our website www.endovascularwa.com.au
. The booking is tentative until you receive a follow email or call from our Patient’s Service team confirming your appointment. Booking will be confirmed within one working day, if not sooner.
© 2010 Endovascular WA
221 Stirling Highway, Claremont WA 6010
| T ( 08) 9284 2900 |F (08) 9 384 5725 | E reception@endovascularwa.com.au | W www.endovascularwa.com.au