Morphine Sulfate - Essentials of Medicine
advertisement

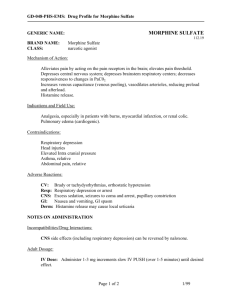
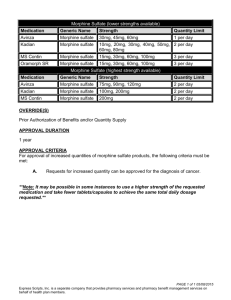
Morphine Sulfate Essentials of Medicine Last Updated: July 2013 Morphine Sulfate M-Eslon SR MS Contin® Avinza® Kadian® Oramorph SR® M.O.S. SR, M.O.S. Sulfate Ratio-Morphine Morphine HP Injection Morphine LP Epidural MS IR® (Morphine Sulfate Immediate Release) M.S. Contin MS-IR, PMS-Morphine Sulfate SR Ratio-Morphine SR Drug Class: Narcotic Pain killer Indications: Pain management m-Eslon capsules produce peak morphine levels at steady state in approximately 3 to 4 hours following administration. m-Eslon have an extended release action, when compared to oral morphine sulphate syrup, as characterized Therapeutic levels are maintained over a period of 12 hours. Due to extensive first-pass metabolism in the liver and gut, the effect of an oral dose is less than after parenteral administration. With repeated regular dosing, orally administered morphine is about one-third as potent as when given by intramuscular injection. Generic name: Brand names: Pharmacology: Preparations: M.S. Contin®: 15 mg, 30 mg, 60 mg, 100 mg, 200 mg Capsule M-Eslon®: 10 mg, 15, 30 mg, 60 mg, 100 mg, 200 mg Capsule Kadian®: 10 mg, 20 mg, 50 mg, 100 mg Tablets MOS®: 5 mg, 10 mg, 20 mg, 50 mg, 60 mg Tablet MOS SR®: 30 mg, 60 mg MS IR® (Morphine Sulfate Immediate Release): 5 mg, 10 mg, 20 mg, 30 mg Oramorph SR®: 15 mg, 30 mg, 60 mg, 100 mg www.EssntialsOfMedicine.com Page 1 Morphine Sulfate Essentials of Medicine Last Updated: July 2013 Dosing: MS Contin: 15-60mg orally every 8 to 12 hours. M-Eslon: o PO: 10 to 30 mg po q4h prn, better to be given q12h o SQ/IM: 5-20 mg/70 kg q4h prn One or two 10 mg capsules twice daily is the recommended starting dosage for a patient presenting with severe pain. When m-Eslon SR capsules are to be given for the relief of post-operative pain, it is not advisable to administer it during the first 24 hours. Following this initial period, the dosage should be at the physician's discretion. Prior to long term prescription, a trial of m-Eslon SR capsules or shorter acting opioid analgesics should be undertaken (e.g. for a period of four to six weeks). Long term administration of m-Eslon SR capsules should only occur if this trial demonstrates that the pain is opioid sensitive. Opioid naive patients who require rapid dose escalation with no concomitant pain relief within the trial period should generally be considered inappropriate for long term therapy. A single doctor should be responsible for the prescription and monitoring of the patient’s opioid use. o Gastrointestinal: o Abdominal pain, anorexia, constipation, dry mouth, dyspepsia, nausea, o o Adverse effects: o o o o o vomiting. o Biliary pain, gastrointestinal disorders, ileus, taste perversion. CNS: o Asthenia, confusion, headache, insomnia, involuntary muscle contractions, somnolence, thought abnormalities. o Agitation, dysphoria, euphoria, hallucinations, malaise, mood changes, respiratory depression, seizure, paresthesia, vertigo, vision abnormalities, withdrawal syndrome. Genitourinary: o Amenorrhea, decreased libido, impotence, urinary retention. Cardiovascular: o Hypotension, syncope Metabolic: o Peripheral edema, pulmonary edema Respiratory: o Bronchospasm, cough decreased, respiratory depression. Dermatological: o Rash o Urticaria General: o Chills, pruritus, sweating. o Allergic reaction, anaphylactic/anaphylactoid reactions, drug dependence, facial flushing, hypertonia, miosis, tolerance. www.EssntialsOfMedicine.com Page 2 Morphine Sulfate Essentials of Medicine Last Updated: July 2013 o CNS depressants such as alcohol, anaesthetics, hypnotics and sedatives, tricyclic o o o o o o o Drug interactions: o o o o o o o antidepressants, phenothiazines and antipsychotics may enhance the depressant effects of morphine. This may result in respiratory depression, hypotension, profound sedation or coma and death. To avoid such side effects dosage adjustment may be required. Antihistamines, beta-blockers and skeletal muscle relaxants may also enhance the depressant effects of morphine. Agonist/antagonist analgesics e.g. buprenorphine should not be administered to a patient who has received or is receiving a course of therapy with a pure opioid agonist analgesic. The analgesic effect may be reduced or withdrawal symptoms may occur. Alcohol o Experimental studies have shown that alcohol increases morphine release from the microgranules in the capsule which may lead to the rapid release and absorption of a potentially toxic dose of morphine. Amphetamines o Amphetamines potentiate the analgesic effect of morphine. Anticholinergics o The concomitant use of anticholinergics (e.g. TCAs) with opioids may result in an increased risk of severe constipation and urinary retention. This may increase the likelihood of adverse effects such as confusion and constipation. Cimetidine o Cimetidine inhibits the metabolism of morphine. Cyclizine o Cyclizine may counteract the haemodynamic benefits of opioid analgesics. Diuretics o Morphine reduces the efficacy of diuretics by inducing the release of antidiuretic hormone. MAO inhibitors o MAOIs intensify the effects of morphine and other opioids which can cause anxiety, confusion and significant depression of respiration and even coma. Narcotic antagonists o Concomitant use of narcotic antagonists may result in reversal of analgesia, and may precipitate withdrawal symptoms in patients who are physically dependent on opioids. Oral anticoagulants o Morphine may increase the anti-coagulant activity of coumarin and other anticoagulants. Skeletal muscle relaxants o Morphine may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. Zidovudine o Morphine may competitively inhibit the hepatic gluconuronidation of zidovudine thus reducing its clearance. Concurrent use of morphine and zidovudine should be avoided because the toxicity of either or both medicines may be potentiated. Food www.EssntialsOfMedicine.com Page 3 Morphine Sulfate Essentials of Medicine Last Updated: July 2013 o The bioavailability of morphine is not significantly affected by food Contraindications Metabolism: Warning: Pregnancy: Co-ingestion with alcohol (in the presence of alcohol, dose-dumping of opioid to potentially fatal plasma levels may occur, even in opioid-tolerant patients) Respiratory depression may occur especially if the person has excessive bronchial secretion, obstructive airways disease, known morphine sensitivity or acute hepatic disease. Acute alcoholism, severe cirrhosis, delirium tremens. Severe CNS depression Convulsive disorders (may lower the seizure threshold) Head injuries, brain tumours and other conditions in which cerebrospinal or intracranial pressure is raised Acute attacks of bronchial asthma Heart failure secondary to chronic lung disease, cor pulmonale. Cardiac arrhythmias. Hypotension. Surgical anastomosis Concurrent administration with or within 2 weeks of discontinuation of monoamine oxidase inhibitors (MAOIs). Paralytic ileus, Acute abdomen Delayed gastric emptying. Patients with phaeochromocytoma as morphine appears to increase catecholamine levels M-Eslon is not to be used as a pre-operative medication. Patients with chronic pain of non-malignant origin who have a prior history of substance abuse. Children under the age of 6 months. Renal excretion: caution should be exercised in patients with clinically significant impairment of the renal function The elimination half-life of morphine is 2 to 3 hours with great interpatient variability. About 90% of total morphine is excreted in 24 hours with traces in urine for 48 hours or more. Morphine should be administered with caution to patients in circulatory shock as its vasodilatory effects may further reduce cardiac output and blood pressure. Morphine may lead to acute retention of urine by causing spasm of the sphincter of the bladder especially in men with prostatism. M-Eslon SR is not recommended for use in pregnancy. Although morphine is secreted in breast milk, it is usually considered safe due to the relatively low transfer into milk at about 0.4% of the maternal dose, and its subjection www.EssntialsOfMedicine.com Page 4 Morphine Sulfate Essentials of Medicine Last Updated: July 2013 to high first-pass metabolism. Special precautions: Reduced dosing is necessary in patients with renal or hepatic dysfunction, and also in the elderly due to increased sensitivity to its effect. Withdrawal symptoms: o Chronic use of opioid analgesics may be associated with the development of physical dependence and may occur when opioid administration is abruptly discontinued or opioid antagonists administered. o Withdrawal symptoms include body aches, diarrhoea, piloerection, anorexia, nervousness or restlessness, rhinorrhoea, sneezing, tremors or shivering, abdominal colic, nausea, sleep disturbances, unusual increase in sweating and yawning, weakness, tachycardia and unexplained fever. Note: This document is prepared by Siavash Jafari, MD, FRCPC and Dr Ronald Joe, BHB, MBChB, MSc (HINF). This document is provided for information purposes only and does not necessarily represent endorsement by or an official position of the Essentials of Medicine. Advice on the treatment or care of an individual patient should be obtained through consultation with a physician who has examined that patient or is familiar with that patient's medical history. References: o o o o o o o o o Hanks GW, De Conno F, Ripamonti C, et al. Morphine in cancer pain: modes of administration. Bm J. 1996;312:823– 826. Klepstad P, Kaasa S, Skauge M, Borchgrevink PC. Pain intensity and side effects during titration of morphine to cancer patients using a fixed schedule dose escalation. Acta Anaesthesiol Scand. 2000;44:656–664. Borgbjerg FM, Nielsen K, Franks J. Experimental pain stimulates respiration and attenuates morphine-induced respiratory depression: a controlled study in human volunteers. Pain. 1996;64:123–128. Von Korff M and Deyo R Potent opioids for chronic musculoskeletal pain: Flying blind? Pain 109 (2004) 207–209. Sansom LN e. Australian pharmaceutical formulary and handbook. 21 ed. Canberra: Pharmaceutical Society of Australia; 2009. Jordan KM, Cameron JS, Snaith M, Zhang W, Doherty M, Seckl J, et al. British Society for Rheumatology and British Health Professionals in Rheumatology guideline for the management of gout. Rheumatology (Oxford). 2007; 46(8): 1372-4. Neuropathic pain: the pharmacological management of neuropathic pain in adults in nonspecialist settings. NICE clinical guideline 96 (2010). Accessed july 2013 at: http://www.nice.org.uk/guidance/CG96 Armstrong SC, Cozza KL. Pharmacokinetic drug interactions of morphine, codeine, and their derivatives: theory and clinical reality, Part I. Psychosomatics 2003;44:167–71. Quigley C. Hydromorphone for acute and chronic pain. Cochrane Database Syst Rev 2002:CD003447 www.EssntialsOfMedicine.com Page 5