Page 1 of 26 3/13/2006 http://www.utdol.com/utd/content/topic.do

http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print
Page 1 of 26
Licensed to Frank Tenney, MD
©2006 UpToDate
® printer-friendly format print this for a colleague e-mail this to a colleague
New Search Table Of Contents My UpToDate Feedback Help Log Out
Official reprint from UpToDate
® www.uptodate.com
Definition and diagnosis of hypertension in children and adolescents
Tej K Mattoo, MD, DCH, FRCP
UpToDate performs a continuous review of over 350 journals and other resources. Updates are added as important new information is published. The literature review for version 14.1 is current through
December 2005; this topic was last changed on July 5, 2005. The next version of UpToDate (14.2) will
be released in June 2006.
INTRODUCTION — Hypertension (HTN) is a well established risk factor for cardiovascular disease
(CVD) in adults [ 1,2 ]. Although the incidence of persistent HTN is low in children, it has become clear that HTN begins in childhood and adolescence and can contribute to the early development of CVD as illustrated by the following observations: z
There is increasing evidence that essential HTN has its antecedents during childhood, as childhood blood pressure (BP) predicts adult BP [ 3 ]. z
Among children and adolescents with borderline or established essential HTN, left ventricular hypertrophy is present in approximately 40 to 45 percent of cases [ 4,5 ]. HTN in adults has also been associated with increased left ventricular mass, which is a known risk factor for CVD [ 1,2,6 ]. z
Two autopsy studies in children and young adults who died of noncardiovascular causes, have demonstrated early development of atherosclerosis [ 7,8 ]. In a report from the Bogalusa Heart
Study, the extent of fatty streaks and fibrous plaques in the aorta and coronary arteries was associated with BP [ 7 ]. An association of BP with plaque formation in the aorta and coronary arteries has also been described in African-American subjects [ 8 ]. z
Noninvasive methods of assessment of vascular changes related to atherosclerosis demonstrate an association of BP with predictors of CVD including arterial stiffness measured by pulse wave velocity [ 9 ], arterial calcification [ 10,11 ] and carotid intimal medial thickness evaluated by computed tomography [ 11 ] or echocardiography [ 12 ].
Based upon these observations, identifying children at risk for hypertension could have an important impact on long-term outcomes of CVD.
The definition, prevalence, and diagnostic evaluation of HTN in children will be reviewed here. The treatment of HTN in children is discussed separately. ( See "Treatment of hypertension in children and adolescents" ).
DEFINITION — The National High Blood Pressure Education Program Working Group (NHBPEP) established guidelines for the definition of normal and elevated blood pressures in children in 1987
[ 13 ]. These guidelines were updated in 2004 [ 14 ].
3/13/2006
Page 2 of 26
The definition of childhood hypertension (HTN) is statistically defined based upon the normative distribution of blood pressure (BP) in healthy children as opposed to adult HTN, which is largely defined clinically as the level of BP at which trials of antihypertensive therapy have demonstrated improvements in clinical outcome [ 2,13,14 ]. ( See "Overview of hypertension in adults" ). This clinical definition cannot be applied to children since cardiovascular events other than left ventricular hypertrophy do not typically occur until adulthood.
In children, the following definitions based upon NHBPEP Working Group recommendations are used to classify BP measurements [ 14 ]. BP percentiles are based on gender, age, and height and upon measurements on three separate occasions ( show table 1A-1B and show table 2A-2B ). ( See "Number of measurements" below ). z
Normal — Systolic and diastolic BP <90th percentile z
Prehypertension — Systolic and/or diastolic BP 90th percentile but <95th percentile, or if BP exceeds 120/80 mmHg even if <90th percentile. A systolic pressure of 120 mmHg may typically occur at 12 years of age, while a diastolic pressure of 80 mmHg typically occurs at 16 years of age. z
Stage 1 hypertension — Systolic and/or diastolic BP between the 95th percentile and 5 mmHg above the 99th percentile. z
Stage 2 hypertension — Systolic and/or diastolic BP 99th percentile plus 5 mmHg.
The systolic and diastolic BP are of equal importance; if there is a disparity in category, the higher value determines the severity of the HTN.
Body size is the most important determinant of BP in children and adolescents. Thus, classification of
BP is more accurate when the values are adjusted for height as well as age and gender to avoid misclassifying children at the extremes of normal growth ( show table 1A-1B and show table 2A-2B )
[ 14,15 ].
A limitation to using percentiles derived from study populations to define normal BP is the need to account for secular trends, which may vary among countries as illustrated by the following observations: z
The systolic and diastolic pressures among children and adolescents in the United States increased by an average of 1.4 mmHg and 3.3 mmHg, respectively, between NHANES III (1988 to 1994) and
NHANES 1999 to 2000, in part related to the increased prevalence of overweight and obese children [ 16 ]. z
In contrast, there was a decrease in both systolic (range of decrease 7.7 to 10 mmHg) and diastolic (range of decrease 8.8 to 11 mmHg) BPs in two representative cohorts of adolescents from Northern Ireland over a ten year period from 1989-1990 to 1999-2000 [ 17 ]. The findings in the Irish study were independent of body composition or birth weight and found in both males and females at two different ages (12 and 15 years).
Severity — The decision process for evaluation varies with the severity of the HTN. As noted above, the NHBPEP Working Group recommendation defines two stages for HTN [ 14 ]. Stage 2 identifies those children who need more prompt evaluation and pharmacologic treatment; stage 1 allows time for evaluation and treatment with nonpharmacologic therapy unless the patient is symptomatic. ( See
"Treatment of hypertension in children and adolescents" ).
These definitions apply only to chronic HTN in which the development of arterial hypertrophy protects the capillary circulation. With acute HTN, as can occur in acute glomerulonephritis, acute renal failure, http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 3 of 26 pheochromocytoma, or preeclampsia, it is the magnitude of the increase above baseline that determines the risk. In these settings, malignant HTN can develop at absolute BPs that might otherwise be considered to represent mild or moderate HTN. ( See "Hypertensive emergencies: Malignant hypertension and hypertensive encephalopathy" , section on Mechanisms of vascular injury).
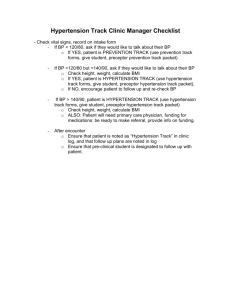
PREVALENCE — The NHANES III national health survey in adults in the United States showed that the prevalence of HTN is highly age-dependent, increasing progressively with age ( show figure 1A-1B ) [ 18 ].
Relatively few adults under age 30 are affected, particularly women. The great majority of these patients have essential HTN.
The prevalence of persistent HTN in children is lower than in adults but is increasing. In a 1989 report of almost 15,000 junior high school-aged children in the United States, the prevalence was 1.1 percent after measurements on three occasions [ 19 ]. A higher prevalence was noted in a later schoolbased study in the United States. BP screening and measurement of height and weight were performed in 5102 children (mean age 13.5 years) in 2002 [ 20 ]. The prevalence of HTN was 4.5 percent after BP measurement on three occasions. The difference between these two observations probably reflects in part an increase in mean body mass index (BMI) between these two time periods
[ 16 ]. However, in some other populations, as in Northern Ireland, the mean systolic and diastolic pressures fell over the same time period [ 17 ].
Younger children generally have an identifiable cause (ie, secondary HTN), whereas essential HTN accounts for most cases in adolescents [ 21 ]. ( See "Secondary hypertension" below ).
Obesity — The increasing prevalence of HTN in school-aged children is in part due to the increased prevalence of obesity [ 16,20,22 ]. This was illustrated in the 2002 school-based study, described above, in which the prevalence of HTN increased with increasing BMI (2 versus 11 percent among those with
BMI 5th and 95th percentile, respectively) [ 20 ]. Another study of Canadian children (aged 9 to 16 years) also reported a consistent association between BP and BMI [ 22 ]. ( See "Definition; epidemiology; and etiology of obesity in children and adolescents" and see "Comorbidities and complications of obesity in children and adolescents" ).
Race — NHANES III showed that the incidence of HTN in adults was affected by race and ethnicity, being more common in non-Hispanic African Americans ( show figure 1A-1B ) [ 18 ]. The age-adjusted prevalence of HTN was 32 percent in the non-Hispanic African American population compared to 23 percent in the non-Hispanic white and Mexican American populations. African Americans also may be more likely to develop hypertensive complications, particularly renal disease. The relative importance of environmental and genetic factors has not been established [ 23 ]. ( See "Hypertensive complications in blacks" ).
Data are more limited and somewhat conflicting in children. The Bogalusa Heart Study provided evidence supporting significantly higher pressures in African American compared to white children
[ 24,25 ]. The increase in BP was associated with sodium intake and lower plasma renin activity [ 25 ]. In contrast, a much larger survey found no overall BP difference between African American and white children and adolescents [ 26 ]. However, African Americans had higher pressures at lower levels of body mass index (BMI) and lower pressures at higher levels of BMI. This observation is compatible with the finding in the Bogalusa Heart Study and another report that obesity was not as closely related to BP in African American children as it was in white children [ 27,28 ].
There is also evidence suggesting that higher pressures are seen in United States children who are of
Asian descent [ 29,30 ]. This finding is inconsistent, particularly after adjustment for weight [ 20 ].
Family history — A family history of HTN is present in as many as 70 to 80 percent of all patients with essential HTN (compared to 40 percent or less for patients with secondary HTN) [ 31 ] and in approximately 50 percent of hypertensive children [ 32 ]. The percentage of hypertensive children is determined in part by the presence of normotension (N) or hypertension (H) in the parents. The relationship between the BP in the parents and the incidence of children with HTN was evaluated in a http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 4 of 26 review from Japan [ 33 ]: z z z
N x N matings — 4.2 to 17.6 percent hypertensive children
N x H matings — 15.9 to 56.8 percent
H x H matings — 44.0 to 73.3 percent
In another study, it was estimated that the risk of HTN in the offspring increased 2.5-fold with H x H compared to N x N matings [ 34 ]. In addition, normotensive relatives of hypertensive patients may have a somewhat higher BP than normotensive subjects without a family history of HTN [ 35,36 ].
When examined in the reverse order, hypertensive children had a greater prevalence of HTN in their parents (27 versus 8 percent in normotensive children), grandparents (47 versus 23 percent), and siblings (14 versus 5 percent) [ 37 ].
Familial aggregation alone does not distinguish between genetic factors and shared environmental factors (eg, greater likelihood of obesity, sedentary lifestyle, and high salt intake ). ( See "Treatment of hypertension in children and adolescents" , section on Nonpharmacologic therapy, for a review of the major environmental factors).
It has been estimated that genetic factors account for approximately 30 percent of the variation in blood pressure in various populations [ 38,39 ] and as much as 60 to 70 percent of HTN in families [ 40 ].
( See "Genetic factors in the pathogenesis of essential hypertension" ).
The best evidence for genetic factors comes from BP correlations within families: z
The BP correlation is stronger between parents and children than between spouses [ 41 ]. z
There is no significant BP correlation between parents and adopted children [ 42,43 ]. z
Most studies in twins have shown evidence for a genetic component of blood pressure since the BP correlation is stronger between identical (monozygotic) twins than between fraternal (dizygotic) twins or siblings [ 41,44 ]. Comparison of dizygotic with monozygotic twins supports a hereditary estimate of 0.72 and 0.28 for diastolic BP and systolic BP, respectively [ 44 ]. However, the observation that the BP correlation is stronger among dizygotic twins than other first-degree relatives indicates a nongenetic environmental effect [ 45 ]. The Montreal twin adoption study on normal blood pressure estimated the relative contributions of shared genes (33 percent), across generation shared environment (24 percent), and the environment shared within generations (43 percent) [ 43,46 ].
Inheritance of essential HTN is likely to be polygenic. A number of different genes have been evaluated but their role remains uncertain. ( See "Genetic factors in the pathogenesis of essential hypertension" ).
Breastfeeding — There is evidence that breastfeeding may be associated with lower BPs in childhood
[ 47-49 ]. This was illustrated in two prospective cohort studies. z
In the first study, 7276 infants were evaluated at 7.5 years of age [ 47 ]. Those who were breastfed as infants had systolic and diastolic BPs that were 1.2 mmHg and 0.9 mmHg lower than in infants who were never breastfed [ 47 ]. The reduction in both systolic and diastolic pressures was greater in infants who were exclusively breastfed, and the systolic BP reduction increased with the duration of breastfeeding. z
Similar findings were found in 7223 singleton infants evaluated at 5 years of age [ 49 ]. Those who were breastfed for 6 months had systolic BP that was lower 1.2 mmHG lower than in infants who http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 5 of 26 had been breastfed less than 6 months or not at all [ 49 ].
White coat hypertension — White coat or isolated office HTN is defined as office BP readings 95th percentile but with normal values outside the office setting. Studies suggest a prevalence as high as
35 percent in children being evaluated for persistently elevated casual BP [ 50 ] and approximately 44 percent in children with a positive family history of essential HTN [ 51 ]. The prevalence of white coat
HTN is higher when the office values reveal borderline or mild HTN, and much lower with moderate or severe HTN [ 52 ].
It is possible that white coat HTN in children represents two populations: one that is destined to develop essential HTN [ 53 ] and one that has persistent white coat HTN or reverts to normotension.
Studies in adults suggest that as many as 20 to 25 percent of patients have white coat HTN [ 54 ].
These patients have a relatively benign outcome compared to those with sustained HTN [ 55 ]. They may be at increased risk for eventual sustained HTN and cardiovascular disease, although the risk of cardiovascular complications appears to be low as long as the ambulatory pressure remains normal.
( See "Ambulatory blood pressure monitoring in children" ).
MEASUREMENT OF BLOOD PRESSURE — The importance of technique in BP measurement was illustrated in a comparison of normal BP readings reported by 10 different investigators in which the highest and lowest percentile values (50th and 95th) for boys differed by as much as 20 mmHg [ 56 ].
Confounding factors included cuff size, the number of measurements made, type of instruments used, patient position (supine or sitting), and the choice of heart sound (fourth or fifth Korotkoff sound) used for determining diastolic BP. ( See "Technique of BP measurement" below ).
Current recommendations of the National High Blood Pressure Education Program Working Group and the American Heart Association Council on High Blood Pressure Research for the measurement of blood pressure (BP) in children are [ 14,57 ]: z
All children >3 years old who are seen in a medical setting should have their BP measured.
Children <3 years old should have their BP measured if they have a history of neonatal complications requiring neonatal intensive care, congenital heart disease, recurrent urinary tract infection, hematuria, proteinuria, known renal or urologic disease, family history of congenital renal disease, solid organ or bone marrow transplantation, malignancy, treatment of drugs known to raise BP, other systemic illnesses associated with HTN, or evidence of increased intracranial pressure. z
An appropriate cuff size to the size of the child's upper arm is required for accurate measurement.
( See "Cuff size" below ). z
The preferred method of BP measurement is auscultation using a standard clinical sphygmomanometer. Although the mercury sphygmomanometer is the most accurate and widely used instrument, its availability is restricted because of the potential risk of mercury poisoning. The aneroid manometers are accurate but need to be calibrated on a semi-annual basis and should be used if a mercury manometer is not available. z
Confirmation of elevated of BP on three repeated and separate visits are needed prior to the diagnosis of HTN. ( See "Number of measurements" below ). z
Oscillometric BP measurements that exceed the 90th percentile should be confirmed by auscultation. ( See "Oscillometric devices" below ).
Cuff size — A variety of different cuff sizes are available, including oversized and adult cuffs that may be used in obese adolescents. The correct choice of cuff is important for accurate measurements. If too small a cuff is used, the pressure generated by inflating the cuff may not be fully transmitted to http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 6 of 26 the brachial artery. In this setting, the pressure in the cuff may be considerably higher than the intraarterial pressure, leading to overestimation of the systolic pressure. On the other hand, too wide a cuff may produce lower than arterial readings.
The cuff size should have a bladder width approximately 40 percent of the circumference of the upper arm midway between the olecranon and the acromion ( show figure 2 ). The cuff bladder should cover 80 to 100 percent of the circumference of the upper arm [ 14,57,58 ]. The bladder width-to-length should be at least 1:2 ( show table 3 ).
The accuracy of BP readings with recommended bladder cuff widths compared to direct intraarterial measurements was evaluated in a review of 65 stable children [ 59 ]. Cuff widths using the 40 percent upper arm circumference criterion gave comparable readings to intraarterial measurements for systolic BP but overestimated diastolic BP by a mean of 7 mmHg. In comparison, cuffs with widths chosen by the previously recommended criteria (equal to two-thirds to three-fourths of the length of the upper arm) resulted in substantially and significantly lower values for both systolic BP (15 to 17 mmHg) and diastolic BP (6 to 7 mmHg) because of the use of larger arm cuffs.
Another study confirmed the overestimation of appropriate cuff size using these criteria and also noted that many pediatricians use a larger cuff than recommended by the 40 percent upper arm circumference criterion, particularly in older children [ 60 ].
Technique of BP measurement — The following steps are recommended for the accurate measurement of BP [ 14,57,58,61 ]. ( See "Technique of blood pressure measurement in the diagnosis of hypertension" ). z
Prior to BP measurement, stimulant drugs or food should be avoided. z
The BP should be measured after five minutes of rest in the seated position with the child's back and feet supported in a quiet enviroment. Because anxiety acutely raises both the heart rate and
BP, the most reproducible readings are obtained when the pulse rate is both steady and within the normal range. Measurements made in noncooperative, agitated children are often misleading. The likelihood of obtaining falsely elevated readings can be minimized by repeated measurements of the heart rate until the rate is normal and/or reproducible. ( See "White coat hypertension" below ). z
The BP is measured with a stethoscope placed over the brachial artery pulse in the cubital fossa
( show figure 3 ). The BP should be taken with the patient's right arm supported at the level of the heart. The right arm is preferred in repeated measures of BP for consistency and comparison with standard tables. In addition, the possibility of coarctation of the aorta would lead to falsely low BP readings in the left arm.
Allowing the arm to hang below the heart will elevate BP levels by the added hydrostatic pressure induced by gravity (as much as 10 to 12 mmHg in adults) [ 62 ]. The mercury manometer should be visible but does not have to be at the level of the heart [ 61 ]. z
The cuff should be inflated to 20 to 30 mmHg above the systolic BP and then deflated slowly at a rate of 2 to 3 mmHg per heartbeat. The systolic BP is equal to the pressure at which the brachial pulse can first be palpated as blood flow is restored through the previously compressed vessel, which is also when the pulse is first heard by auscultation (Korotkoff phase I). As the cuff is deflated below the systolic BP, the pulse continues to be heard until there is abrupt muffling (phase
IV) followed by disappearance of sound (phase V) [ 63 ].
Phase V is recommended for diastolic pressure determination in children [ 14 ] as well as adults [ 2 ]. In some children, Korotkoff sounds can be heard to 0 mmHg. If this occurs, BP measurement should be repeated with less pressure on the head of the stethoscope. If phase V is still very low, phase IV
(muffling) should be recorded as the diastolic BP [ 14 ]. http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 7 of 26 z
Coarctation of the aorta is one of the more common causes of HTN in young children. Thus, the BP should be measured in both arms and legs on the first visit, particularly if the pulses in the legs are absent or weak. The BP in the leg is measured by ausculation over the popliteal fossa using the appropriate size cuff. If the systolic BP in the legs is lower than 10 mmHg than that measured in the arms, further studies for coarctation of the aorta should be performed [ 57 ]. ( See "Clinical manifestations and diagnosis of coarctation of the aorta" ).
Number of measurements — The BP should be taken at least twice on each visit, with the measurements separated by one to two minutes to allow the release of trapped blood. If the second value is more than 5 mmHg different from the first, continued measurements should be made until a stable value is attained. The recorded value on the patient's chart should be the average of the last two measurements [ 64 ].
The new diagnosis of HTN should not be made until the BP measurement is 95th percentile on at least three separate visits, separated by days or weeks apart [ 14,57,65 ]. Many patients (both adults and children) have substantial reductions in BP between the first and third visits to a new doctor
[ 19,66,67 ]. The magnitude of this effect in children was illustrated in a report of almost 15,000 junior high school-aged children [ 19 ]. The incidence of systolic and/or diastolic HTN fell from 3.5 percent on initial screening examination to 1.1 percent after two additional examinations.
The frequent fall in BP with serial measurements is primarily due to two factors: an accommodation effect, due to reduced anxiety over time, and regression to the mean [ 14 ].
Oscillometric devices — Oscillometric devices are used when auscultation is difficult as with infants and neonates, and/or in the intensive care unit when frequent BP measurement is needed [ 57 ]. Two advantages are their ease of use and decrease in observer bias.
Automated oscillometric devices measure mean arterial BP based upon pressure oscillations and calculate the systolic and diastolic BP from these values. Manufacturers of oscillometric devices use different algorithms for these calculations. Comparison of different devices has shown a wide variation, with 30 percent of individual systolic BP differences being more than 10 mmHg [ 68 ]. In addition, when compared to auscultated BP measurements, oscillometric systolic BP readings were 10 mmHg higher [ 69 ].
Based upon these observations, it is recommended that BP readings >90th percentile obtained with an oscillometric device be confirmed by auscultation [ 14 ].
Another concern is that oscillometric devices require maintenance and repeated calibration that are rarely followed and therefore limit their use in usual outpatient clinical settings. Caution should be used when interpreting BP results with these devices [ 14 ].
HOME BP MEASUREMENT — Home BP measurements are widely used in adults and are being increasingly used for diagnostic and therapeutic purposes in children. Standards for taking and interpreting home BP values in children vary considerably among clinicians [ 70 ].
We encourage home BP measurements, particularly in children with acute or unstable HTN. In addition to permitting better management of the HTN, it is an excellent educational tool for the patient and/or the parents.
AMBULATORY BP MEASUREMENTS — Blood pressure (BP) changes continually in response to physiologic and environmental stimuli. In adults, ambulatory BP measurements (ABPM) have better reproducibility and better correlation with the risk of hypertensive cardiovascular complications and target organ damage than office BP. Data are more limited in children, but also indicate an important role of ABPM in the evaluation of HTN [ 71 ]. In particular, by providing multiple measurements during regular activities (including sleep), ABPM can be used to detect white coat HTN. It can also give useful http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 8 of 26 information regarding the BP pattern in patients with chronic kidney disease, diabetes, autonomic dysfunction, or episodic HTN. These issues are discussed in detail elsewhere. ( See "Ambulatory blood pressure monitoring in children" ).
DIAGNOSTIC EVALUATION — As of 2002, approximately 4.5 percent of children have hypertension
(HTN), defined as BP values 95th percentile, that persists on at least three measurements [ 20 ]. Most hypertensive children, particularly those who are likely not to have essential hypertension (eg, prepubertal or nonobese children or those with severe hypertension) should be referred to a pediatric nephrologist or other physician with experience in HTN.
The following evaluation is based upon the recommendations of the 2004 NHBPEP Working Group
[ 14 ]. The goals of the evaluation are to: z
Identify any child with secondary HTN who may have a curable disease ( show table 4 ) z
Identify other comorbid risk factors (obesity, hyperlipidemia and/or diabetes mellitus) for cardiovascular disease ( see "Comorbidities and complications of obesity in children and adolescents" ) z
Identify children who should be treated with antihypertensive drug therapy
History and physical examination — The history and physical examination in children with confirmed hypertension need to look for findings that are associated with specific underlying etiologies for HTN
( show table 5 and show table 6 ) [ 14 ]. Emphasis should also be placed on the possible presence of one or more of the following: z
Family history of hypertension, diabetes, obesity, sleep disorders, cardiovascular disease
(hyperlipidemia, stroke and myocardial infarction), renal and endocrine diseases. z
Comorbid risk factors for cardiovascular disease (CVD) such as obesity and abnormal sleep patterns, including snoring, since there is an association of sleep apnea with HTN and obesity. z
Drug history including over the counter, prescription, and illicit drugs and specific questions about smoking, alcohol consumption, and the use of drugs or preparations that enhance athletic performance. z
Retinal examination in hypertensive children and in prehypertensive children (BP between the 90 to
94th percentile) with comorbid risk factors such as obesity, hyperlipidemia, and/or diabetes.
Laboratory evaluation the following [ 14 ]:
— Initial laboratory evaluation in all children with persistent HTN should include z
Measurement of serum BUN, creatinine, and electrolytes, and collection of urine for urinalysis and culture. These tests permit quick assessment of renal function and abnormalities in glucose or potassium homeostasis. z
Complete blood count, looking for anemia that may reflect chronic diseases such as vasculitis and chronic renal disease. z
Renal ultrasonography, which will detect any renal scar, congenital anomaly, difference in renal size, or adrenal mass. z
Measurement of fasting plasma glucose and lipids. These tests should also be performed in prehypertensive children who are obese, have a family history of HTN or CVD or have chronic renal http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 9 of 26 disease. z
An echocardiogram to evaluate left ventricular mass. Left ventricular hypertrophy (LVH) is the most prominent clinical evidence in children of target-organ damage from HTN [ 14 ]. LVH has been reported in 34 to 38 percent of children and adolescents with mild and untreated HTN [ 12,72,73 ]. It is an indication to initiate or intensify antihypertensive therapy [ 74 ]. Prehypertensive children with obesity, hyperlipidemia, diabetes mellitus, or chronic renal disease should also have echocardiographic assessment of left ventricular mass.
Based upon the history, physical examination, and initial laboratory evaluation, the clinician should be able to establish whether the HTN is essential (primary) or secondary. This distinction will determine whether further evaluation is performed for a potentially reversible cause of secondary HTN.
Essential hypertension — Essential hypertension, which is the most common cause in older children, is a diagnosis of exclusion. It is more likely in children who are older than 10 years, particularly if postpubertal, or who have a family history of hypertension ( see "Family history" above ), are overweight or obese, or have only mild hypertension (BP at or just above the 95th percentile). It is more common in African Americans.
Hypertensive children who fit the essential hypertension profile may need no further laboratory evaluation beyond the routine testing cited above [ 14 ].
The BMI (weight in kg divided by height in m2) should be calculated. Values less than 25, 25 to 29.9,
30 to 39.9, and above 40 are considered normal, overweight, obese, and markedly obese, respectively ( show figure 4 ). In a school health screening program, 30 percent of overweight adolescents were hypertensive (BP 95th percentile on three occasions) and the prevalence of HTN increased with higher values of BMI [ 75 ].
Obesity and high BP are also associated with the metabolic syndrome, which is an important risk factor for the subsequent development of type 2 diabetes and/or CVD. Although a consensus definition has not been established in children, most definitions require three or more of the following: elevated serum triglyceride levels, low serum high-density lipoprotein cholesterol, impaired glucose tolerance, and HTN. The prevalence of the metabolic syndrome increases with BMI and is as high as 30 to 50 percent in obese children. These issues are discussed in detail elsewhere. ( See "The metabolic syndrome
(Insulin resistance syndrome or syndrome X)" , section on Children and adolescents).
Thus, among obese hypertensive children, measurement of hemoglobin A1c may be indicated, particularly if there is a strong family history of type 2 diabetes.
Sleeping disorders, especially sleep apnea, are associated with HTN and CVD in adults. In children, limited data suggest an association between sleep-disordered breathing and HTN [ 76,77 ]. Based upon this information, the NHBPEP Working Group recommended that a sleep history should be obtained in a child with HTN, especially if he or she is overweight. If a history of either sleep apnea or loud and frequent snoring is obtained, polysomnography should be considered to identify sleep disorder [ 14 ].
( See "Evaluation of the child with snoring or suspected obstructive sleep apnea" ).
There is little data on the usefulness of plasma levels of uric acid, homocysteine, and lipoprotein(a), usually referred to as Lp(a), in the evaluation of pediatric essential hypertension. The NHBPEP
Working Group does not recommend these studies unless there is a strong family history of an abnormality [ 14,78 ].
Secondary hypertension — Secondary hypertension should be suspected in children with the following findings, and further evaluation is warranted: z
Prepubertal, particularly under age 10 years http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 10 of 26 z
Stage 2 hypertension (BP >5 mmHg above the 95th percentile) z
Stage 1 hypertension (BP 95th percentile but less than stage 2) with clinical signs that suggest systemic disease z
An acute rise in BP above a previously stable baseline z
A thin child with a negative family history for hypertension
Etiologies — There are a number of causes of secondary hypertension ( show table 4 ), and specific symptoms ( show table 5 ) and findings ( show table 6 ) may point to a particular disorder. In a review of
636 children with sustained hypertension from Poland, 351 (55 percent) had a known secondary cause
[ 21 ]. The most common were renal disease (68 percent) and endocrine and renovascular diseases (11 and 10 percent, respectively). Almost all children (98 percent) younger than 15 years of age had a secondary cause, whereas 75 percent of adolescents had essential hypertension.
The following discussion reviews different etiologies of secondary hypertension including diagnostic evaluation and/or clinical findings. z
Findings suggestive of underlying intrinsic renal disease include an abnormal urinalysis and/or an elevation in the BUN and serum creatinine concentrations. The most common mechanisms of hypertension are volume expansion (as in acute poststreptococcal glomerulonephritis) and activation of the renin-angiotensin system. ( See "Hypertension in renal disease" ).
A past history of urinary tract infection, particularly in early childhood, raises the possibility of reflux nephropathy. However, some children with reflux nephropathy do not have a history of documented urinary tract infection in early childhood. Renal scarring may be detected by renal ultrasound but
DMSA or glucoheptonate renal scan is more sensitive. ( See "Clinical manifestations and diagnosis of vesicoureteral reflux" ). z
Renovascular disease in children is caused by a diverse group of lesions, with almost half of the cases due to fibromuscular dysplasia [ 79,80 ]. Other etiologies include renal artery hypoplasia, midaortic syndrome (segmental narrowing of the proximal abdominal aorta), arteritis, and neurofibromatosis type 1 [ 80,81 ]. Evaluation for renovascular disease should also be considered in the hypertensive infant with prior placement of an umbilical artery catheter. ( See "Neurofibromatosis type 1 (von Recklinghausen's disease)" and see "Neonatal hypertension" ).
Current golden standard evaluation of renovascular disease in children includes standard intraarterial angiography or digital-subtraction angiography (DSA). There is limited experience in children with newer radiological imaging technology including magnetic resonance arteriography (MRA), spiral computed tomography (CT), or three-dimensional CT. These modalities may become the method of choice with accumulation of more experience. If renovascular evaluation is needed, a radiological center with pediatric experience should be chosen. ( See "Screening for renovascular hypertension" ).
The plasma renin activity is higher in children with renovascular hypertension but, as is true in adults, it is a relatively insensitive test. Approximately 15 percent of children with arteriographically evident renal artery stenosis have normal renin levels [ 82,83 ]. z
Catecholamine excess symptoms include headache, sweating, and tachycardia in addition to hypertension. Pheochromocytoma, neuroblastoma or use of sympathomimetic drugs including phenylpropanolamine (over-the-counter decongestant), cocaine, amphetamines, phencyclidine , epinephrine, phenylephrine , and terbutaline , and the combination of a monoamine oxidase (MAO) inhibitor plus ingestion of tyramine-containing foods are possible etiologies. The diagnosis is confirmed with elevated levels of plasma and urine catecholamines and metabolites. http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 11 of 26
In pheochromocytoma, not all patients have the three classic symptoms, but most have two of the three. These symptoms are usually accompanied by hypertension that is typically sustained rather than paroxysmal. Pheochromocytoma is often sporadic but can occur with certain genetic disorders such as neurofibromatosis, multiple endocrine neoplasia type 2, von Hippel-Lindau syndrome, and hereditary paragangliomas. Some patients with these disorders have no family history of the disease.
( See "Pheochromocytoma in children" ). z
Otherwise unexplained hypokalemia and metabolic alkalosis with urinary potassium wasting is strongly suggestive of primary mineralocorticoid excess. Such patients do not present with edema.
( See "Clinical features of primary aldosteronism" , section on Lack of edema).
Aldosterone-secreting tumors are most common in adults, but the most frequent cause in children is excess deoxycorticosterone secretion in congenital adrenal hyperplasia due to CYP11B1 (11-beta hydroxylase) and CYP17 (17-alpha-hydroxylase) deficiencies. The former is characterized by ambiguous genitalia in females (clitoral enlargement, labial fusion, formation of a urogenital sinus) and penile enlargement in males, while the latter usually presents at about the time of expected puberty with hypogonadism. ( See "Congenital adrenal hyperplasia due to CYP11B1 (11-beta-hydroxylase) deficiency" and see "Uncommon causes of congenital adrenal hyperplasia" ).
Aldosterone-secreting tumors are rare in children, but primary hypersecretion of aldosterone may result from the genetic disorder glucocorticoid-remediable hyperaldosteronism (GRA). Hypokalemia is absent in more than one-half of patients. In the absence of hypokalemia at presentation, the diagnosis may be suspected from the family history of early hypertension (before age 21 years) and the frequent development of marked hypokalemia after the administration of a thiazide diuretic. ( See
"Glucocorticoid-remediable aldosteronism" ).
Plasma renin levels will be very low or unmeasurable in these disorders. Further work-up would include plasma and urine steroid levels to identify the endocrine abnormality. ( See "Approach to the patient with hypertension and hypokalemia" ). z
Coarctation of the aorta is one of the major causes of hypertension in young children. The classic findings are hypertension in the upper extremities, diminished or delayed femoral pulses, and low or unobtainable systolic pressure in the lower extremities. However, patient age, the site of origin of the left subclavian artery, and the severity of the coarctation affect the pattern of blood pressure findings. In most cases, the origin of the left subclavian artery is proximal to the coarctation, resulting in hypertension in both arms. However, when the origin of the left subclavian artery is just distal to the coarctation, the left brachial pulse is diminished compared to the right and equal to the femoral pulse. ( See "Clinical manifestations and diagnosis of coarctation of the aorta" ). z
Oral contraceptives often raise the blood pressure within the normal range but can induce overt hypertension. ( See "Effect of oral contraceptives and postmenopausal hormone therapy on blood pressure" ).
ACKNOWLEDGMENT — The editorial staff at UpToDate, Inc. would like to acknowledge that Alan B
Gruskin, MD, who contributed to an earlier version of this topic review, passed away in April 2003.
Use of UpToDate is subject to the Subscription and License Agreement.
1.
2.
REFERENCES
Lewington, S, Clarke, R, Qizilbash, N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903.
Chobanian, AV, Bakris, GL, Black, HR, Cushman, WC. The Seventh Report of the Joint National
Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7
Report. JAMA 2003; 289:2560.
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 12 of 26
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
25.
26.
27.
Lauer, RM, Clarke, WR. Childhood risk factors for high adult blood pressure: The Muscatine Study.
Pediatrics 1989; 84:633.
Daniels, SR, Witt, SA, Glascock, B, et al. Left atrial size in children with hypertension: the influence of obesity, blood pressure, and left ventricular mass. J Pediatr 2002; 141:186.
Daniels, SR, Loggie, JM, Khoury, P, Kimball, TR. Left ventricular geometry and severe left ventricular hypertrophy in children and adolescents with essential hypertension. Circulation 1998;
97:1907.
Whelton, PK, He J, Appel LF, et al. Primary prevention of hypertension: clincial and public advisory from The National High Blood Pressure Education Program. JAMA 2002; 288:1882.
Berenson, GS, Srinivasan, SR, Bao, W, et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med
1998; 338:1650.
McGill, HC Jr, McMahan, CA, Zieske, AW, et al. Effects of nonlipid risk factors on atherosclerosis in youth with a favorable lipoprotein profile. Circulation 2001; 103:1546.
Li, S, Chen, W, Srinivasan, SR, Berenson, GS. Childhood blood pressure as a predictor of arterial stiffness in young adults: the bogalusa heart study. Hypertension 2004; 43:541.
Mahoney, LT, Burns, TL, Stanford, W, et al. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: the Muscatine Study. J
Am Coll Cardiol 1996; 27:277.
Davis, PH, Dawson, JD, Mahoney, LT, Lauer, RM. Increased carotid intimal-medial thickness and coronary calcification are related in young and middle-aged adults. The Muscatine study.
Circulation 1999; 100:838.
Sorof, JM, Alexandrov, AV, Cardwell, G, Portman, RJ. Carotid artery intimal-medial thickness and left ventricular hypertrophy in children with elevated blood pressure. Pediatrics 2003; 111:61.
Report of the Second Task Force on Blood Pressure Control in Children. Pediatrics 1987;79:1.
14. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004; 114:555.
15. Rosner, B, Prineas, RJ, Loggie, JM, Daniels, SR. Blood pressure nomograms for children and adolescents, by height, sex, and age, in the United States. J Pediatr 1993; 123:871.
16.
17.
Muntner, P, He, J, Cutler, JA, et al. Trends in blood pressure among children and adolescents. JAMA
2004; 291:2107.
Watkins, D, McCarron, P, Murray, L, et al. Trends in blood pressure over 10 years in adolescents: analyses of cross sectional surveys in the Northern Ireland Young Hearts project. BMJ 2004;
329:139.
18.
19.
Burt, VL, Whelton, P, Roccella, EJ, et al. Prevalence of hypertension in the US adult population.
Results from the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension
1995; 25:305.
Sinaiko, AR, Gomez-Marin, O, Prineas, RJ. Prevalence of "significant" hypertension in junior high school-aged children: the Children and Adolescent Blood Pressure Program. J Pediatr 1989;
114:664.
20.
21.
22.
23.
Sorof, JM, Lai, D, Turner, J, et al. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics 2004; 113:475.
Wyszynska, T, Cichocka, E, Wieteska-Klimczak, A, et al. A single pediatric center experience with
1025 children with hypertension. Acta Paediatr 1992; 81:244.
Paradis, G, Lambert, M, O'Loughlin, J, et al. Blood pressure and adiposity in children and adolescents. Circulation 2004; 110:1832.
Cooper, R, Rotimi, C, et al. Hypertension in blacks. Am J Hypertens 1997; 10:804.
24. Voors, AW, Foster, TA, Frerichs, RR, et al. Studies of blood pressures in children, ages 5-14 years, in a total biracial community: the Bogalusa Heart Study. Circulation 1976; 54:319.
Berenson, GS, Voors, AW, Webber, LS, et al. Racial differences of parameters associated with blood pressure levels in children--the Bogalusa heart study. Metabolism 1979; 28:1218.
Rosner, B, Prineas, R, Daniels, SR, Loggie, J. Blood pressure differences between blacks and whites in relation to body size among US children and adolescents. Am J Epidemiol 2000; 151:1007.
Berenson, GS, Webber, LS, Srinivasan, SR. Pathogenesis of hypertension in black and white children. Clin Cardiol 1989; 12:IV3.
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 13 of 26
28.
29.
Daniels, SR, McMahon, RP, Obarzanek, E, et al. Longitudinal correlates of change in blood pressure in adolescent girls. Hypertension 1998; 31:97.
Munger, RG, Gomez-Marin, O, Prineas, RJ, Sinaiko, AR. Elevated blood pressure among Southeast
Asian refugee children in Minnesota. Am J Epidemiol 1991; 133:1257.
30. Hohn, AR, Dwyer, KM, Dwyer, JH. Blood pressure in youth from four ethnic groups: the Pasadena
Prevention Project. J Pediatr 1994; 125:368.
31. Simon, N, Franklin, SS, Bleifer, KH, Maxwell, MH. Clinical characteristics of renovascular hypertension. JAMA 1972; 220:1209.
32. Jung, FF, Ingelfinger, JR. Hypertension in childhood and adolescence. Pediatr Rev 1993; 14:169.
33. Miyao, S, Furusho, T. Genetic study of essential hypertension. Jpn Circ J 1978; 42:1161.
34. Deutscher, S, Epstein, FH, Kjelsberg, MO. Familial aggregation of factors associated with coronary heart disease. Circulation 1966; 33:911.
35. Bianchi, G, Cusi, D, Barlassina, C, et al. Renal dysfunction as a possible cause of essential hypertension in predisposed subjects. Kidney Int 1983; 23:870.
36.
37.
Grim, CE, Luft, FC, Miller, JZ, et al. Effects of sodium loading and depletion in normotensive firstdegree relatives of essential hypertensives. J Lab Clin Med 1979; 94:764.
Cassimos, C, Aivazis, V, Karamperis, S, et al. Arterial blood pressure lipids and cardiovascular complications in families of hypertensive children. Acta Paediatr Scand 1982; 71:235.
38. Hunt, SC, Ellison, RC, Atwood, LD, et al. Genome scans for blood pressure and hypertension: the
National Heart, Lung, and Blood Institute Family Heart Study. Hypertension 2002; 40:1.
39. Kaplan, NM. Primary hypertension: Pathogenesis. In: Kaplan's Clinical Hypertension, 8th ed,
Kaplan, NM (Ed), Lippincott Williams Wilkins, Philadelphia 2002. p.58.
40. Ward, R. Familial aggregation and genetic epidemiology of blood pressure. In: Hypertension-
Pathophysiology, Diagnosis and Management, Laragh, J, Brenner, B (Eds), Raven Press, New York
1990. p.81.
41.
42.
43.
Havlik, RJ, Feinleib, M. Epidemiology and genetics of hypertension. Hypertension 1982; 4:III121.
Biron, P, Mongeau, JG, Bertrand, D. Familial aggregation of blood pressure in 558 adopted children.
Can Med Assoc J 1976; 115:773.
Annest, JL, Sing, CF, Biron, P, Mongeau, JG. Familial aggregation of blood pressure and weight in adoptive families. II. Estimation of the relative contributions of genetic and common environmental factors to blood pressure correlations between family members. Am J Epidemiol 1979; 110:492.
44. Christian, JC. Twin studies of blood pressure. In: Children's Blood Pressure 1985. Report of the
85th Ross Conference on Pediatric Research 1985. p.51.
45. Feinleib, M, Garrison, R, Borhani, N, et al. Studies of hypertension in twins. In: Epidemiology and
Control of Hypertension, Paul, 0 (Ed), Stratton Intercontinental Medical Book Corp, New York 1975. p.3.
46. Mongeau, JG, Biron, P, Sing, CF. The influence of genetics and household environment on the variability of normal blood pressure: The Montreal Adoption Survey. In: Children's Blood Pressure.
Report of the 85th Ross Conference on Pediatric Research, 1985. p.55.
47.
48.
Martin, RM, Ness, AR, Gunnell, D, et al. Does breast-feeding in infancy lower blood pressure in childhood? The Avon LongituRRdinal Study of Parents and Children (ALSPAC). Circulation 2004;
109:1259.
Wilson, AC, Forsyth, JS, Greene, SA, et al. Relation of infant diet to childhood health: seven year follow up of cohort of children in Dundee infant feeding study. BMJ 1998; 316:21.
49. Lawlor, DA, Najman, JM, Sterne, J, et al. Associations of parental, birth, and early life characteristics with systolic blood pressure at 5 years of age: findings from the Mater-University study of pregnancy and its outcomes. Circulation 2004; 110:2417.
50.
51.
52.
Ocon-Pujadas, J, Mora-Macia, J. White coat hypertension and related phenomena. A clinical approach. Drugs 1993; 46 Suppl 2:95.
Hornsby, JL, Mongan, PF, Taylor, AT, Treiber, FA. 'White coat' hypertension in children. J Fam Pract
1991; 33:617.
Sorof, JM, Poffenbarger, T, Franco, K, Portman, R. Evaluation of white coat hypertension in children: importance of the definitions of normal ambulatory blood pressure and the severity of casual hypertension. Am J Hypertens 2001; 14:855.
53.
Matthews, KA, Woodall, KL, Allen, MT. Cardiovascular reactivity to stress predicts future blood http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 14 of 26
54. pressure status. Hypertension 1993; 22:479.
Pickering, TG, James, GD, Boddie, C, et al. How common is white coat hypertension? JAMA 1988;
259:225.
55.
56. Park, MK, Troxler, RG. Systemic hypertension. In: Pediatric Cardiology for Practitioners, 4th ed,
Park, MK (Ed), Mosby, St. Louis 2002. p.408.
57.
Khattar, AS, Senior, R, Lehiri, A. Cardiovascular outcome in white-coat versus sustained mild hypertension: A 10-year follow-up study. Circulation 1998; 98:1892.
Pickering, TG, Hall, JE, Appel, LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the subcommittee of professional and public education of the American Heart
Association Council on High Blood Pressure Research. Circulation 2005; 111:697.
58. Williams, CL, Hayman, LL, Daniels, SR, Robinson, TN. Cardiovascular health in childhood: A statement for health professionals from the Committee on Atherosclerosis, Hypertension, and
Obesity in the Young (AHOY) of the Council on Cardiovascular Disease in the Young, American
Heart Association. Circulation 2002; 106:143.
59. Clark, JA, Lieh-Lai, MW, Sarnaik, A, Mattoo, TK. Discrepancies between direct and indirect blood pressure measurements using various recommendations for arm cuff selection. Pediatrics 2002;
110:920.
60. Arafat, M, Mattoo, TK. Measurement of blood pressure in children: recommendations and perceptions on cuff selection. Pediatrics 1999; 104:e30.
61. Recommendations for routine blood pressure measurement by indirect cuff sphygmomanometry.
American Society of Hypertension. Am J Hypertens 1992; 5:207.
62. Beevers, G, Lip, GY, O'Brien, E. ABC of hypertension. Blood pressure measurement. Part II
Conventional sphygmomanometry: Technique of auscultatory blood pressure measurement. BMJ
2001; 322:1043.
63.
64.
65.
Sinaiko, AR, Gomez-Marin, O, Prineas, RJ. Diastolic fourth and fifth phase blood pressure in 10-15year-old children. The Children and Adolescent Blood Pressure Program. Am J Epidemiol 1990;
132:647.
Bailey, RH, Bauer, JH. A review of common errors in the indirect measurement of blood pressure.
Sphygmomanometer. Arch Intern Med 1993; 153:2741.
Gillman, MW, Cook, NR. Blood pressure measurement in childhood epidemiological studies.
Circulation 1995; 92:1049.
66.
67.
Hartley, RM, Velez, R, Morris, RW, et al. Confirming the diagnosis of mild hypertension. Br Med J
1983; 286:287.
Watson, RD, Lumb, R, Young, MA, et al. Variation in cuff blood pressure in untreated outpatients with mild hypertension Implications for initiating antihypertensive treatment. J Hypertens 1987;
5:207.
68.
69.
70.
71.
72.
Kaufmann, MA, Pargger, H, Drop, LJ. Oscillometric blood pressure measurements by different devices are not interchangeable. Anesth Analg 1996; 82:377.
Park, MK, Menard, SW, Yuan, C. Comparison of auscultatory and oscillometric blood pressures.
Arch Pediatr Adolesc Med 2001; 155:50.
Bald, M, Hoyer, PF. Measurement of blood pressure at home: survey among pediatric nephrologists. Pediatr Nephrol 2001; 16:1058.
Lurbe, E, Sorof, JM, Daniels, SR. Clinical and research aspects of ambulatory blood pressure monitoring in children. J Pediatr 2004; 144:7.
Belsha, CW, Wells, TG, McNiece, KL, et al. Influence of diurnal blood pressure variations on target organ abnormalities in adolescents with mild essential hypertension. Am J Hypertens 1998;
11:410.
73. Hanevold, C, Waller, J, Daniels, S, et al. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the
International Pediatric Hypertension Association. Pediatrics 2004; 113:328.
74. Gidding, SS. The aging of the cardiovascular system: when should children be treated like adults?.
J Pediatr 2002; 141:159.
75. Sorof, J, Daniels, S. Obesity hypertension in children: a problem of epidemic proportions.
Hypertension 2002; 40:441.
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 15 of 26
76.
77.
78.
79.
80.
81.
82.
Marcus, CL, Greene, MG, Carroll, JL. Blood pressure in children with obstructive sleep apnea. Am J
Respir Crit Care Med 1998; 157:1098.
Enright, PL, Goodwin, JL, Sherrill, DL, et al. Blood pressure elevation associated with sleep-related breathing disorder in a community sample of white and Hispanic children: the Tucson Children's
Assessment of Sleep Apnea study. Arch Pediatr Adolesc Med 2003; 157:901.
Feig DI, Nakagawa, T, Karumanchi, SA, et al.Hypothesis: Uric acid, nephron number, and the pathogenesis of essential hypertension. Kidney Int 2004; 66:281.
Deal, JE, Snell, MF, Barratt, TM, Dillon, MJ. Renovascular disease in childhood. J Pediatr 1992;
121:378.
Piercy, KT, Hundley, JC, Stafford, JM, et al. Renovascular disease in children and adolescents. J
Vasc Surg 2005; 41:973.
Fossali, E, Signorini, E, Intermite, RC, Casalini, E. Renovascular disease and hypertension in children with neurofibromatosis. Pediatr Nephrol 2000; 14:806.
Dillon, MJ, Ryness, JM. Plasma renin activity and aldosterone concentration in children. Br Med J
1975; 4:316.
83. Guzzetta PC; Potter BM; Ruley EJ; Majd M; Bock GH. Renovascular hypertension in children: current concepts in evaluation and treatment. J Pediatr Surg 1989;24:1236.
GRAPHICS
Normal BP boys-I
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 16 of 26
Normal BP boys-II
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 17 of 26
Normal BP girls-I
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 18 of 26
Normal BP girls-II
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 19 of 26
Prevalence of HTN in men
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 20 of 26
Prevalence of HTN in women
Determining BP cuff size
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 21 of 26
BP cuff sizes
Blood pressure measurement
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 22 of 26
Causes HTN children
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 23 of 26
History for hypertensive child
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 24 of 26
PE for hypertensive child
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 25 of 26
Nomogram for BMI
http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006
Page 26 of 26
New Search Table Of Contents My UpToDate Feedback
©2006 UpToDate
®
• www.uptodate.com
Licensed to Frank Tenney, MD
Server: WEB005
Help Log Out http://www.utdol.com/utd/content/topic.do?topicKey=pedineph/11964&view=print 3/13/2006