Neonatal Resource Services Clinical Guideline Thermoregulation
advertisement

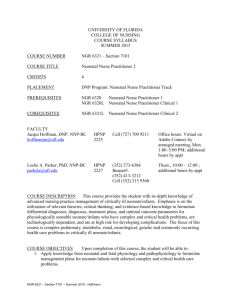
Neonatal Resource Services Clinical Guideline Thermoregulation Guideline Purpose: To explain the importance of the principles of thermoregulation in the NICU Background Definitions Control of thermoregulation is one of the critically important factors in physiological maintenance of the neonate in the NICU. The neonate is no exception to the general rule that body temperature is the result of a balance between heat production and heat loss. Heat loss in the neonate, especially the very small premature neonate is the due to properties of the skin, low insulation (i.e., fat), high evaporation and limited ability to vasoconstrict. Importantly, the body surface area is high in relation to weight in the neonate; a factor that significantly facilitates heat loss in this group. The ability to maintain normal core body temperature is inversely proportional to the gestational age of the neonate. The appropriate for gestational age neonate needs support until approximately 35 weeks corrected gestational age. Maintenance of thermoregulation in the neonate involves reducing one or more of the four mechanisms of heat loss: convection, conduction, evaporation and radiation. The neutral thermal environment is the range of ambient temperature within which the metabolic rate is at a minimum and within which the temperature regulation is achieved by nonevaporative processes alone. The four mechanisms of heat loss in the neonate include the following: Conduction: transfer of heat through the body to the skin surface and from the skin surface to that which is in contact with the skin Convection: transfer of heat at the skin surface to the surrounding air Evaporation: transfer of heat from the skin or mucous membranes through loss of water Radiation: transfer of heat from a warmer surface to a cooler surface without the need for direct contact or an interceding medium Thermoregulation The use of an incubator/radiant warmer to facilitate maintenance of a thermoneutral environment is routine practice in the NICU until the neonate is able to maintain his/her own thermoregulatory control . A key criterion to determine if the neonate is ready for discharge is his/her ability to maintain their temperature without incubator/radiant warmer support. Client Target Population Any neonate in the NICU; however, these guidelines are applicable to those neonates who require assistance in maintaining their neutral thermal environment Clinical Management There is no absolute standard of care for maintenance of a neutral thermal environment and the subsequent weaning of the neonate from either the incubator or the radiant warmer. However the following guidelines are in general use in the majority of NICUs in this country: Neonatal Resource Services Thermoregulation April 2013 2013 OptumHealth. Confidential and Proprietary—Do Not Distribute 1 Medical Director Escalation Incubator Temperature: Generally the neonate may be weaned from the incubator when the temperature of the incubator is less or equal to 28 degrees C Corrected Gestational Age: When this parameter reaches approximately 34 36 weeks Consistent Weight Gain: A consistent weight gain of 15-20 g/kg/d Enteral Feeding: The neonate should tolerate full enteral nutrition Apnea, Bradycardia and Desaturations: A/B/D episodes should not require stimulation Cardiovascular Stability: The neonate should evidence cardiovascular stability; i.e., stable vital signs The Nurse Case Manager should refer the case to the Medical Director if the neonate is still in the incubator when the temperature of the incubator is less or equal to 28 degrees C, assuming no skilled nursing services are required. Best Practices Infants < 32 week should be placed on a chemical heating mattress and or in a polyethylene wrap in the delivery room for transfer to the NICU to improve to reduce insensible water and improve admission temperature Weaning should occur prior to achieving full enteral feeds. This proactive approach has been shown to reduce LOS by an average of ~ 2.5 days. Neonatal Resource Services Thermoregulation April 2013 2013 OptumHealth. Confidential and Proprietary—Do Not Distribute 2 Bibliography Baumgart S. Thermal regulation in the fetus and newborn. Intensive Care of the Fetus and Neonate. Mosby, 1996 Chantaroi S Yechasatid W. Effect of polyethylene bag to prevent heat loss in preterm infants at a birth; a randomized controlled trial. J Med Asssoc Thai 2011:Suppl; 7 S 32-7 Cochrane Review entitled Transfer of preterm infants from incubator to open cot at lower verses higher body weight. The reviewers are K. New, V Flenady and MW Davies. It was first published in 2004 and revised in 2007 and revised in 2011 Doyle K.J.Bradshaw W.T. Sixty golden minutes Neonatal Network 2012: 5: 289-294 Flenady VJ, Woodgate PG. Radiant warmer vs incubators in newborn infants. Cochrane Systematic Reviews. 2003; Issue 4 Gaylord, M, et al. Improved Fluid Management Utilizing Humidified Incubators in Extremely Low Birth Weight Infants. J Perinat 2001; 21: 438-443 Hammarlund K and Sedin, G. Transepidermal Water Loss in newborn Infants, 111: relation to Gestational Age. Acta Paed Scand. 1988; 68: 795-801 Meyer, M, et al. A Clinical Comparison of Radiant Warmer and Incubator Care for Preterm Infants from Birth to 1800 Grams. Pediatrics 2001; 108: 395-401 Sauer PJJ Neonatal Thermoregulation in Cowett RM (editor) Principles of Perinatal Neonatal Metabolism Vol 2 Springer Verlag Pages 1027 – 1044. 1998. Sutter et al. Weaning of premature infants from the incubator to an open crib. Journal of Perinatology1988: 8:193-198 Neonatal Resource Services Thermoregulation April 2013 2013 OptumHealth. Confidential and Proprietary—Do Not Distribute 3