Keeping Infants Warm
advertisement

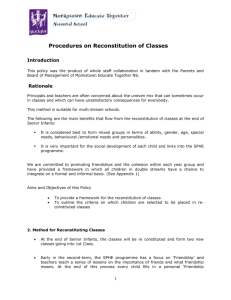
10984-03_ANC801-Mance.qxd 1/30/08 11:58 AM Page 6 MARY A. SHORT, RN, MSN • Section Editor Keeping Infants Warm Challenges of Hypothermia Martha J. Mance, MS, RN, NNP, CPNP ABSTRACT Hypothermia is a major cause of morbidity and mortality in infants; therefore, maintaining normal body temperatures in the delivery room is crucial. An understanding of how infants produce heat and what can be done to maintain normal body temperatures in full-term and preterm infants is essential for the preservation of thermal stability in this population. This article reviews the consequences of hypothermia, mechanisms of heat exchange and heat production in full-term and low birth-weight infants, and discusses interventions in the delivery room to alleviate hypothermia. KEY WORDS: hypothermia, temperature regulation, neonate, delivery room ypothermia is a major cause of morbidity and mortality in infants, underscoring the importance of maintaining normal body temperature in the delivery room. The World Health Organization (WHO) lists hypothermia as a “top killer” during the neonatal period1 and suggests that it is widely underreported and underestimated as a cause of death.2 Cold stress is associated with lethargy, hypotonia, poor feeding, weight loss, abdominal distention, vomiting, restlessness, pallor, cool skin, tachypnea, respiratory distress, and a significantly reduced core temperature.3 Hypothermia has been related to hypoglycemia, hypoxia, metabolic acidosis, coagulation defects, and severe intraventricular hemorrhage.4 Reductions in body temperature may delay transition from fetal to neonatal circulation at birth secondary to the effect of temperature on pulmonary vasomotor tone and acid-base homeostasis.5 Pulmonary hemorrhage may result from acidosis secondary to shock and hypoxia, causing left ventricular failure and increased pulmonary capillary pressure.3 Cold stress may have an important role in stimulating the onset of breathing6 and protecting the brain following a hypoxic, ischemic event but can have disastrous consequences if not stopped,7-10 making early intervention in the delivery suites imperative. This article reviews the consequences H Address correspondence to Martha J. Mance, MS, RN, CPNP, Nurse Practitioner, Neonatal Intensive Care Unit, Women and Infants’ Hospital, 101 Dudley Street, Providence, RI 02903; reignamjm@aol.com. Author Affiliation: Women and Infants’ Hospital, Providence, Rhode Island. Copyright 2008 © by the National Association of Neonatal Nurses. 6 of hypothermia and mechanisms of heat exchange and heat production in full-term and low birth-weight infants and discusses routine interventions that can be implemented in the delivery room to minimize hypothermia. A CONTINUING PROBLEM A number of studies have reported the problem of cold stress in neonates. The EPIcure study, a large prospective observational study in the United Kingdom and the Republic of Ireland, evaluated outcomes of infants between 20 and 25 weeks’ gestation (n = 843). The purpose of the study was to describe survival and health problems in this population of infants at the minimal levels of viability. The results demonstrated that 40% of the infants were hypothermic (temperatures < 35°C; P < .001). These infants were in more critical condition than were those with normal temperatures upon admission to the NICU.11 A second study reported that 29% of infants less than 30 weeks’ gestation born by cesarean section were admitted to the neonatal intensive care unit (NICU) with axillary temperatures lower than 35.6°C.12 Another research team13 found that more than one-quarter of the infants were hypothermic, despite implementation of the Neonatal Resuscitation Program14 (NRP) guidelines to prevent cold stress. Cold stress in the delivery room contributes to increased oxygen consumption and potentially interferes with an effective resuscitation.15 Others have described low admission temperatures in 15 centers of the National Institute of Child Health and Human Development Neonatal Research Network,16 and hospitals in developing countries1 continue to document the problem of hypothermia on admission. These studies11,16,17 reveal reduced survival rates in infants Advances in Neonatal Care • Vol. 8, No. 1 • pp. 6-12 10984-03_ANC801-Mance.qxd 1/30/08 11:58 AM Page 7 Keeping Infants Warm TABLE 1. Normative Values Neutral Thermal Environment An Environment in Which Body Temperature is Maintained with the Lowest Expenditure of Energy and Oxygen Consumptiona Normothermia 36.5°C-37.5°Cb Hypothermia < 36.5°Cb Hyperthermia > 37.5°Cb a From Vohra et al.21 From World Health Organization (WHO).1 b admitted to facilities with temperatures less than 36°C. Although the consequences of hypothermia are severe, difficulty exists in delineating what is normal body temperature for infants.1,3,4,17-23 Table 1 outlines normative values for a neutral thermal environment, normothermia, hypothermia, and hyperthermia. HEAT LOSS Cold stress is a condition in which heat loss is greater than heat production, resulting in the inability to maintain core temperature. Maintenance of body temperature is dependent on an intact central nervous system, the ability to produce heat, the availability of oxygen, and an energy source. Infants exchange heat with the environment through evaporation, con- duction, convection, and radiation. Table 2 discusses the mechanisms of heat loss and interventions that can be implemented at delivery to minimize heat loss that occurs from each mechanism. Low birth-weight infants are less able to prevent heat loss or to produce heat than healthy full-term infants, making them more susceptible to cold stress, particularly at birth. Risk factors identified that increase the risk of hypothermia include prematurity (gestational age [GA] < 37 weeks), low birth-weight,24,25 intrauterine growth restriction, small-for-gestationalage (SGA) infants,26 low ambient or environmental temperature, asphyxia,24 impaired central nervous system function,16 and maternal temperature.25 Open defects in the skin, including omphalocele, gastroschisis, and neural tube defects, also place the infant at an increased risk of heat loss. Very premature infants and infants with a birth weight of less than 1000 g have high evaporative heat losses and immature thermoregulatory mechanisms with reduced vasomotor response to cold stress during the first days after birth.27 The primary goal when caring for extremely low birth-weight (ELBW) infants is to provide a neutral thermal environment in which heat loss can be prevented28 and oxygen consumption is maintained at resting levels.15 Extremely low birthweight29 and SGA26 infants are already predisposed to cold stress because of their physical characteristics. These infants have insufficient subcutaneous fat necessary for insulation, reduced amounts of brown adipose tissue (BAT), a limited ability to mobilize norepinephrine and fat for energy production, and a diminished capacity to increase their oxygen consumption. In TABLE 2. Mechanisms of Heat Loss in the Infant33 Mechanism Definition Intervention Evaporation Heat loss occurs as moisture on the body surface or from the respiratory tract vaporizes. The loss depends on air speed and relative humidity. • • • • • Dry well Add humidity to the environment Humidify oxygen Use polyethylene wraps Decrease air currents around the infant Conduction Transfer of heat from one surface to another by contact. Determined by a temperature gradient as heat moves from an area of higher temperature to lower. • • • • Prewarm radiant warmers Cover scale with warm blanket Have many warm blankets available Use portable warming mattress Convection Heat is dissipated from the interior of the body to the skin surface through the blood. It is conducted from the body surface to the surrounding air and will be displaced from the skin and carried away by diffusion to moving air particles at the skin surface. • • • • Place hat on a well-dried head Swaddle infant Avoid drafts Use warmed gas for resuscitation Radiation Transfer of radiant energy from one body surface to surrounding cooler or warmer surfaces. Heat loss is independent of ambient temperature, air speed, or other heat loss mechanisms. • Prewarm the radiant warmer and the transport bed • Keep warmers away from external walls, windows and direct sunlight Advances in Neonatal Care • Vol. 8, No. 1 7 10984-03_ANC801-Mance.qxd 8 1/30/08 11:58 AM Page 8 Mance addition, they have large surface-area-to-mass ratios and an extended posture that further increases the surface area from which they may lose heat. A higher total body water content and thin, immature skin without a well-defined stratum corneum exposes them to increased transepidermal water loss (TEWL) and increased heat loss.28,30 Decreased glycogen stores31 and poor vasomotor control further increase the risk for hypothermia in ELBW infants.27,30 Reduction of TEWL can be achieved by maintaining elevated levels of humidity in the environment. Increasing the humidity in the premature infant’s environment improves temperature control and fluid balance in infants.31,32 Radiant warmers are competent at supplying an adequate heat source for premature infants but increase the amounts of insensible water loss. The infant is left exposed to air movement around the warmer, increasing convective heat loss.23 Placing plastic wrap over, but not touching, the infant’s skin and adding water vapor under this covering will help to reduce evaporative and conductive losses.30 Transferring the infant to an isolette with added humidity will also reduce loss of heat from evaporation. HEAT PRODUCTION Body temperature is maintained by controlling the balance between heat production and heat loss. The 3 mechanisms by which infants can produce heat to alleviate cold stress are: • Vasoconstriction • Brown fat lipolysis • Alterations of body position In response to cold, the sympathetic nervous system stimulates the peripheral vasculature, resulting in vasoconstriction, reducing skin blood flow and heat loss through conduction. It also induces brown fat lipolysis, resulting in heat production by nonshivering thermogenesis.33 Healthy, full-term infants are able to shiver, but at birth they are able to generate more heat via nonshivering thermogenesis (metabolism of brown fat). Premature infants have a diminished capacity to shiver as well as limited stores of BAT.23 The final method for heat conservation is alteration in body position by flexion of the extremities in an effort to conserve heat (decreasing the exposed surface area) or by increasing motor activity.34 Thermal receptors in the skin and core send information to the hypothalamus, which detects deviations in temperature from a set point and mediates a response through the autonomic, somatic, and endocrine systems.3 Infants respond to cold stress by increasing their oxygen consumption,15 which initially results in oxidative metabolism of glucose, fat, and protein to produce heat. Nonshivering thermogenesis is the primary mode of this heat production in the infant. Brown adipose tissue first appears in the infant around 26 to 30 weeks’ gestation and continues to develop for several weeks postnatally. It is found in the mediastinum, around the great vessels, and around the kidneys, and adrenalglands. Stores are also found in the axilla, the nape of the neck, and between the shoulder blades. It has numerous fat vacuoles and mitochondria with large stores of glycogen and an extensive blood and nerve supply.33 A drop in skin temperature results in the initiation of nonshivering thermogenesis (metabolism of BAT) by hormonal mediators and the sympathetic nervous system. The BAT breaks down into glycerol and nonesterified fatty acids, which release heat. Brown adipose tissue is dependent on oxygen for the lipolysis of this fat during this production of heat. Hypoxia disrupts thermoregulation by causing a redistribution of circulation and ineffective capillary blood supply in BAT.35,36 Prolonged cold stress reduces energy stores and leads to a cascade of events as hypoglycemia aggravates metabolic acidosis, which delays fetal transition.5 Although infants are able to increase their metabolic rate in response to the low environmental temperatures found in delivery rooms, all infants have an initial drop in body temperature.33 The temperature gradient between the infant’s skin and the environment is the critical factor that elicits an increase in oxygen consumption and metabolic rate, potentially resulting in an accumulation of aerobic waste products.15 If the cold stress is not removed or the infant becomes hypoxic, the oxygen demand becomes greater than supply, and an accumulation of anaerobic waste products occurs, which compounds the resulting metabolic acidosis. The colder the infant, the more severe the hypoxia and acidosis become.5 ACHIEVING NORMAL BODY TEMPERATURES Heat is transferred along a gradient from areas of higher temperatures to lower temperatures. Infants are delivered from a warm, shielded uterine environment into a cold, dry delivery room, the perfect setting for heat loss. This is why it is essential for providers to implement interventions to prevent hypothermia.20 Because of the potential detrimental consequences of hypothermia, interventions such as routine care and polyethylene wraps have been studied to determine if they help to reduce or prevent the drop in temperature so frequently noted in infants. Routine Care in the Delivery Room Ambient temperature has a significant influence on heart rate (HR), HR variability, respiratory rate, oxygen consumption, and insensible water loss in ELBW.28 Body temperature and oxygen consumption are inversely related; as body temperature falls, the fraction of inspired oxygen required for survival increases.28 The WHO advocates maintaining the www.advancesinneonatalcare.org 10984-03_ANC801-Mance.qxd 1/30/08 11:58 AM Page 9 Keeping Infants Warm temperature in the delivery room at 25°C.1 It is known that the environmental temperature of the delivery room has a direct impact on heat loss in all infants; maintaining delivery room temperature is a simple intervention to implement.36 Drying and then placing a newly delivered infant under a radiant warmer has been shown to limit the fall in body temperature.37 Even with this simple intervention, a fall in body temperature occurs. By modulating the environmental temperature to reduce the gradient between skin and air, the infant’s metabolic rate can be maintained, energy stores conserved, and acidosis prevented.15 Routine thermal care includes maintaining the delivery room at a minimum of 25°C,1 placing the infant under a radiant warmer, and immediately drying the infant, paying careful attention to drying the head. Wet linens should be removed quickly, and the head should be covered with a hat. The infant should be wrapped in prewarmed blankets, and any other contact surfaces such as a scale, should be prewarmed. Drafts should be avoided.22 The competency checklist outlines procedures for routine care in the delivery room (Table 3). Employing Polyethylene Wraps Several studies have demonstrated the success of utilizing polyethylene occlusive wraps to keep LBW infants warm at the time of delivery.17,21,24,25,38 Following delivery, providers place the wet infant into a polyurethane bag on the warmer, keeping the infant’s head exposed (Figure 1). The head and face are then dried, and resuscitation continues following NRP guidelines.14 The clear plastic wrap permits visualization of the infant39 and any interventions needed are performed with the infant in the bag. For more extensive resuscitation requiring umbilical or peripheral lines, healthcare providers cut holes in the bag to gain access.17 The infant is then placed on warmed blankets and transferred to the NICU, where the infant is placed on a radiant warmer and the polyethylene bag is removed.25 Polyethylene bags permit heat to be gained by the infant through radiation and reduce the amount of evaporative heat loss.32,39 TABLE 3. Competency Checklist for Maintaining Infant’s Temperature in the Delivery Room Healthy Full-term Infant 1. Radiant warmer in delivery room should be set up ahead of time per hospital routine with warm blankets over the mattress. 2. Have radiant warmer set to 25% maximum power at all times. Prior to delivery, the warmer should be on manual mode and reset to maximal power. 10. Have a clean, warmed blanket available to wrap the infant prior to presentation to the parents. 11. Maintain an environment that promotes a neutral thermal environment, avoiding drafts and keeping the room warm. a. Additional blankets can be brought in from blanket warmer just before the birth. 12. Skin-to-skin care can be initiated once infant and mother have been dried and a hat has been placed on the infant’s head. (This can be accomplished on the motherís abdomen.) Once skin-to-skin care is initiated, a warm blanket should be placed over the infant, cocooning the infant with the mother. b. Have a warmed, dry blanket ready to receive the infant upon birth. Preterm Infant 1. Follow steps 1–3 for the healthy full-term infant. 3. Place drying towels directly under the warmer and over the drying blanket. 4. Once the infant is brought to the warmer, he/she should be dried quickly with the warmed, dry blanket. 5. Remove the wet blanket and continue drying with the towels and blanket on the warmer. 6. Dry the head thoroughly and place a hat on the infant’s head. 7. The infant can remain on the warmer for further evaluation and resuscitation. 8. Place a temperature probe on the infant’s abdomen, switch the warmer to servocontrol set at 37.5°C. 9. Place warmed blanket on scale prior to weighing the infant. Advances in Neonatal Care • Vol. 8, No. 1 9 2. Add a portable warming mattress to the radiant warmer. 3. Place a polyethylene occlusive wrap on the warmer to await infant < 29 weeks’ gestation. 4. Once the infant is brought to the warmer, remove the wet blanket and place wet infant under the wrap or in the bag and close, leaving the infant’s head out. Place the infant on the warming mattress. 5. Dry head and place hat on infant. 6. Continue with resuscitation as needed. 7. Any infant being brought to the NICU should be placed in a warm transport bed and weighed on arrival to the NICU. 10984-03_ANC801-Mance.qxd 10 1/30/08 11:58 AM Page 10 Mance FIGURE 1. Transparent Bags to Limit Heat Loss in the Delivery Room Transparent bags can be used to limit heat loss in the delivery room. A retrospective study of infants born at less than 28 weeks’ gestation (n = 77) evaluated the use of polyethylene wraps to increase NICU admission temperatures. The researchers found that the wrapped infants’ axillary temperature was greater than that of infants receiving routine care (P < .001). This study supports the use of polyethylene wraps to prevent hypothermia in premature infants less than 28 weeks’ gestation.40 A retrospective preintervention audit of infants’ admission temperatures found that many premature infants admitted to the NICU were cold. Then the investigators performed a prospective postintervention audit following the introduction of polyethylene wraps in infants less than 30 weeks’ gestation (n = 141). The primary objective was to determine the effect of admission temperature when the polyethylene wrap was used immediately after delivery of these infants. The intervention improved admission temperatures in infants less than 27 weeks’ gestation (P < .01).12 A prospective randomized controlled trial of infants less than 30 weeks’ gestation (n = 88) evaluated the effect of using polyurethane bags at delivery in infants less than 29 weeks’ gestation. The wrapped infants were less likely to have admission temperatures of less than 36.4°C (P < .01) and had higher admission temperatures (P < .003).25 In a randomized controlled trial of infants less than 32 weeks’ gestation (n = 62), the effect of polyethylene wrap on rectal temperature was evaluated. Higher admission temperatures were found in the infants less than 28 weeks’ gestation (P < .001), but there was no difference in admission temperatures in infants between 28 and 31 weeks’ gestation (P = .47), lending support to the use of polyethylene occlusive wraps in very low birth-weight (VLBW) infants in the delivery room to help preserve core temperature.24 A second randomized controlled study of infants less than 28 weeks’ gestation (n = 55) was undertaken by the same group to determine whether or not the occlusive wrap used at delivery of VLBW infants would www.advancesinneonatalcare.org 10984-03_ANC801-Mance.qxd 1/30/08 11:58 AM Page 11 Keeping Infants Warm prevent heat loss after delivery better than would conventional drying and whether the benefit was sustained once the wrap was removed. The investigators found higher rectal temperatures on admission in the wrapped infants (P < .002) but no difference between groups in rectal temperature at 1 hour of life. This corroborates previous findings demonstrating prevention in heat loss at delivery of premature infants. The group also found that the size of the infant had a direct effect on core temperature, with the smaller infants having the lower temperatures.21 Because of the VLBW infant’s need for greater thermal protection at birth,21 the primary focus at delivery is to immediately reduce heat loss. These studies support the recommendation for employing polyethylene wraps at the delivery of VLBW infants to reduce hypothermia in infants less than 28 weeks’ gestation. The major limitation of all of these studies is the small sample size. IMPLICATIONS FOR FUTURE RESEARCH The use of polyethylene bags has been demonstrated to work in infants less than 28 weeks’ gestation. Even though it appears that infants greater than 28 weeks’ gestation do not benefit from this intervention, future research could be directed to expanding this population to severely SGA infants, using the polyethylene bags for transportation of premature and full-term infants born outside of the hospital or sick infants with poor peripheral perfusion. Infants lose a significant amount of heat from their heads, so investigations into head covering with or without the use of the polyethylene bags would be helpful. The type of head covering is also an area for additional research. IMPLICATIONS FOR FUTURE EDUCATION Hypothermia in the delivery room can interfere with normal neonatal transition to extrauterine life. Frequent audits of NICU admission temperatures are needed to ensure hypothermia is minimized. The competency checklist describes interventions to prevent cold stress in full-term and premature infants. The most important thing to remember is to dry the infant well to the diminish evaporative heat loss that normally occurs at delivery. CONCLUSION Simple and easy interventions can make large differences in the thermal stability of infants. A warm environment in the delivery suite in conjunction with prompt interventions of routine care, utilizing polyethylene occlusive wraps, and environmental humidity for LBW infants, can help maintain body temperaAdvances in Neonatal Care • Vol. 8, No. 1 11 ture and protect infants against the detrimental effects of hypothermia. References 1. World Health Organization (WHO). Thermal control of the newborn: a practical guide. Maternal Health and Safe Motherhood Programme (WHO/FHE/ MSM/93.2). Geneva: WHO; 1996. 2. Davanzo R. Newborns in adverse conditions: issues, challenges, and interventions. J Midwifery Womens Health. 2004;49(Suppl):29-35. 3. Hackman PS. Recognizing and understanding the cold-stressed term infant. Neonatal Netw. 2001;20:35-41. 4. Bartels DB, Kreienbrack L, Dammann O, Wenzlaff P, Poets CF. Population based study on the outcome of small for gestational age newborns. Arch Dis Fetal Neonatal Ed. 2005;90:53-59. 5. Gandy GM, Adamsons K, Cunningham N, Silverman WA, James LS. Thermal environment and acid-base homeostasis in human infants during the first few hours of life. J Clin Invest. 1964;43:751-758. 6. Kuipers IM, Maertzdorf WJ, De Jong DS, Hanson MA, Blanco CE. Initiation and maintenance of continuous breathing at birth. Pediatr Res. 1997;42:163-168. 7. Simbruner G, Ruttner EM, Schulze A, Perzlmaier K. Premature infants are less capable of maintaining thermal balance of head and body with increases of thermal environment than with decreases. Am J Perinatol. 2005;22:25-33. 8. Edwards AD, Wyatt JS, Thoresen M. Treatment of hypoxic-ischemic brain damage by moderate hypothermia. Arch Dis Child Fetal Neonatal Ed. 1998;78:F85-F91. 9. Gunn AJ, Bennet L. Is temperature important in delivery room resuscitation? Semin Neonatol. 2001;6:241-249. 10. Laptook AR, Corbett RJT. The effects of temperature on hypoxic-ischemic brain injury. Clin Perinatal. 2002;29:623-649. 11. Costeloe K, Hennessy E, Gibson AT, Marlow N, Wilkinson AR. The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics. 2000;106:659-671. 12. Bredemeyer S, Reid S, Wallace M. Thermal management for premature births. J Adv Nurs. 2005;52:482-489. 13. Mitchell A, Niday P, Boulton J, Chance G, Dulberg C. A prospective clinical audit of neonatal resuscitation practices in Canada. Adv Neonatal Care. 2002;2:316-326. 14. Kattwinkel J, ed. Textbook of Neonatal Resuscitation. 5th ed. Elk Grove, IL: American Academy of Pediatrics and American Heart Association; 2006. 15. Adamson SK, Gandy GM, James LS. The influence of thermal factors upon oxygen consumption of the newborn human infant. J Pediatrics. 1965; 66:495-508. 16. Laptook AR, Salhab W, Bhaskar B. Admission temperature of low birth weight infants: predictors and associated morbidities [abstract]. Presented at 2005 Pediatric Academic Societies’ Meeting; May 14-17, 2005; Washington, DC. 17. Lyon AJ, Stenson B. Cold comfort for infants. Arch Dis Child Neonatal Ed. 2004;89:F93-F94. 18. Christensson K, Bhat GJ, Amadi BC, Eriksson B, Hojer B. Randomised study of skin-to-skin versus incubator care for rewarming low-risk hypothermic infants. Lancet. 1998;352:1115. 19. Newton T, Watkinson M. Preventing hypothermia at birth in preterm infants: at a cost of overheating some? Arch Dis Child Fetal Neonatal Ed. 2003;88:F256. 20. McCall EM, Alderice FA, Halliday HL, Jenkins JG, Vohra S. Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. The Cochrane Database of Systemic Reviews 2005, Issue 1. Art No.: CD004210.pub2. DOI:10.1002/14651858.CD004210.pub2. 21. Vohra S, Roberts RS, Zhang B, Janes M, Schmidt B. Heat loss prevention (HeLP) in the delivery room: a randomized controlled trial of polyethylene occlusive skin wrapping in very preterm infants. J Pediatr. 2004;145:750-753. 22. Rieger-Fackeldey E, Schaller-Bals S, Schulze A. Effect of body temperature on the pattern of spontaneous breathing in extremely low birth weight infants supported by proportional assist ventilation. Pediatr Res. 2003;54:332-336. 23. Thomas K. Thermoregulation in infants. Neonatal Netw. 1994;13:15-22. 24. Vohra S, Frent GA, Campbell VC, Abbott AM, Whyte RK. Effect of polyethylene occlusive skin wrapping on heat loss in very low birth weight infants at delivery: a randomized trial. J Pediatr. 1999;134:547-551. 25. Knoebel RB, Wimmer JE, Holbert D. Heat loss prevention for preterm infants in the delivery room. J Perinatol. 2005;25:304-308. 26. Doctor BA, O’Riordan MA, Kirchner HL, Shah D, Hack M. Perinatal correlates and neonatal outcomes for small for gestational age infants born at term gestation. Am J Obstet Gynecol. 2001;185:652-659. 27. Lyon AJ, Pikaar ME, Badger P, McIntosh N. Temperature control in very low birthweight infants during first five days of life. Arch Dis Child Neonatal Ed. 1997;76:F47-F50. 28. Horns KM. Comparison of two microenvironments and nurse caregiving on thermal stability of ELBW infants. Adv Neonatal Care. 2002;2:149-160. 29. Finer NN, Rich WD. Neonatal resuscitation: raising the bar. Curr Opin Pediatr. 2004;16:157-162. 10984-03_ANC801-Mance.qxd 12 1/30/08 11:58 AM Page 12 Mance 30. Rutter N. Clinical consequences of an immature barrier. Semin Neonatol. 2000;5:281-287. 31. Hammarlund K, Nilsson GE, Oberg PA, Sedin G. Transepidermal water loss in newborn infants. V. Evaporation from the skin and heat exchange during the first hours of life. Acta Paediatr Scand. 1980;69:385-392. 32. Sedin G. To avoid heat loss in very preterm infants. J Pediatr. 2004;145: 720-722. 33. Blackburn S. Maternal, Fetal & Neonatal Physiology: A Clinical Perspective. 2nd ed. St. Louis, MO: Saunders; 2003:713-714. 34. Altimier L, Warner B, Amlung S, Kenner, C. Neonatal thermoregulation: bed surface transfers. Neonatal Netw. 1999;18:35-38. 35. Schubring C. Temperature regulation in healthy and resuscitated newborns immediately after birth. J Perinat Med. 1986;14:27-33. 36. Trevisanuto D, Doglioni N, Ferrarese P, Zanardo V. Thermal management of the extremely low birth weight infants at birth. J Pediatr. 2005;147: 716-717. 37. Dahm LS, James LS. Newborn temperature and calculated heat loss in the delivery room. Pediatrics. 1972;49:504-513. 38. Leone TA, Rich W, Finer NN. A survey of delivery room resuscitation practices in the United States. Pediatrics [serial online]. 2006;117:e164-e167. http://www.pediatrics.org. Accessed February 21, 2006. 39. Narendran V, Hoath SB. Thermal management of the low birth weight infant: a cornerstone of neonatology. J Pediatr. 1999;134:529-531. 40. Björklund LJ, Hellström-Westas L. Reducing heat loss at birth in very preterm infants. J Pediatr. 2000;137:739-740. www.advancesinneonatalcare.org