Anxiety And Pain Control In 2008
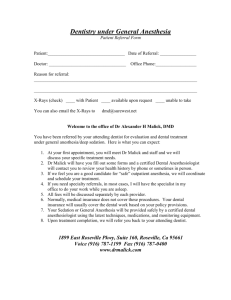
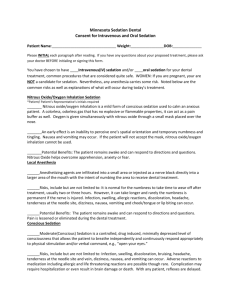
advertisement

Anxiety and Pain Control in 2008: An Update on Local Anesthesia and Minimal Sedation via the Oral and Inhalational Route Iowa Dental Assoc. May 4, 2008 J. Bruce Bavitz, DMD ADA CELL Seminar Series Today's ADA CELL Seminar Series is produced by the AMERICAN DENTAL ASSOCIATION. This valuable member service is partially underwritten by generous grants from: For further information about scheduling an ADA CELL Seminar Series program, please call (312) 440-2908 or email seminarseries@ada.org. ADA Membership Call 1.800.232.1382 and join 152,000 member dentists. Learn about member benefits at www. ADA.org. Collect Data, Formulate Tx Plan History Follow-up questions Exam Lab tests Why bother with the medical history and physical exam? Will they get numb and sit still?* Will they have a medical emergency?* Will they stop bleeding?* Will they resist infection?** Will they heal?** Will the operation ―work‖?** *An intra-operative problem **A post-operative problem Common Changes/Modifications from Normal Surgical Routine Antibiotic Pre-medication D/c anticoagulants Prior Radiation Therapy ? Consider HBO Oral, Nitrous oxide, or IV sedation M.D. consult for tune up or ―clearance‖ Allergy (penicillin, latex, sulfite etc) Abs + BCP…… Consider warning patient Delay Elective TX (Pregnancy, MI, CVA) Long acting or quickly metabolized local anesthetics Limit epi to .04 mg for ―cardiac‖ patients Insulin dose modification for major oral surgery Bisphosphonate subplots Rationale: Local Anesthesia Adequately Controls Procedural Pain for Most Patients, However: Local anesthesia does not control all pain on all patients (the perception of pain is highly subjective). Local anesthesia does not treat fear or anxiety. Although pain is subjective, we do know it is proportional to anxiety. Most patients who claim they are “unable to get numb” have not had their anxiety diagnosed and treated….the local anesthesia is working just fine. Rationale ….continued Most patients dislike receiving local anesthesia (The Needle) About 10 -30% of the U.S. Population avoid dental care because of fear* Treating the ―stressed‖ patient is among the least pleasant tasks for you and your staff *Even 10% of the population in your area = many untreated patients Rationale ….continued Nervous patients are more likely to have medical emergencies and nervous dentists are more likely to make mistakes Some patients are unwilling or unable to cooperate enough to receive local anesthesia (extremes of age, mentally compromised, cerebral palsy) Rarely, a patient may have a true local anesthesia allergy Rationale ….continued Some patients like, and are willing to pay for, sedation. It is difficult to obtain profound local anesthesia for some procedures (I+D, endodontic access on acutely inflamed pulps, reducing facial fractures, extracting deeply impacted 3rds). So, dentists should be able treat pain/fear/anxiety with techniques other than local anesthesia alone. How To Diagnose Anxiety or Which Patients Should I Offer To Sedate? From positive answers to fear/anxiety questions on written medical history form From physical exam (elevated B.P., pulse, ―nervous‖ behavior) Information from your staff Past visits Patient tells you, or you ask Pain/Anxiety Control Techniques Pharmacologic Oral Inhalation I.M. I.V. Submucosal Others Non-Drug Hypnosis Iatrosedation Electronic/TENS Acupuncture Odontology. 2004 Sep;92(1):54-60. Effects of sounds generated by a dental turbine and a stream on regional cerebral blood flow and cardiovascular responses. Mishima R, Kudo T, Tsunetsugu Y. Effects of sound generated by a dental turbine and a small stream (murmur) and the effects of no sound (null, control) on heart rate, systolic and diastolic blood pressure, and hemodynamic changes evaluated. Blood pressures changed in response to the murmur, null, and turbine sound stimuli were as expected: lower than the control level, unchanged, and higher than the control level, respectively. Mean blood pressure values tended to increase gradually over the recording time even during the null sound stimulation, possibly because of the recording environment. Surprisingly, heart rate measurements remained fairly stable in response to the stimulatory noises. In conclusion, we demonstrate here that sound generated by a dental turbine may affect cerebral blood flow and metabolism as well as autonomic responses. Anesthesia and Pain Control Current Guidelines and Policy Statement (Updated October 2007) ADA Policy Statement: The Use of Sedation and General Anesthesia by Dentists Guidelines for the Use of Sedation and General Anesthesia by Dentists | PDF file/111k Guidelines for Teaching Pain Control and Sedation to Dentists and Dental Students | PDF file/105k “Sedation Depth is a Continuum” Anxious Minimal,.…Moderate,….Deep,.......GA Iatrosedation Also known as good chair-side manner, is a non-drug technique where the doctor and his/her staff lessen a patient’s fear/anxiety. If a patient perceives empathy, competence, and caring in the dental team, then anxiety is lessened leading to a more positive experience. There are no contraindications to iatrosedation, and it therefore should be applied to all patients. Anxiolysis (Minimal Sedation) The diminution or elimination of anxiety Respond normally to verbal commands Conscious (Moderate) Sedation A medically controlled state of depressed consciousness that : 1. Allows protective reflexes to be maintained 2. Retains the patient’s ability to maintain a patent airway independently and continuously 3. Permits appropriate response by the patient to physical stimuli or verbal command Deep Sedation A medically controlled state of depressed consciousness or unconsciousness from which the patient is not easily aroused. It may be accompanied by a partial or complete loss of protective reflexes, including the inability to maintain a patent airway and/or respond to verbal command. General Anesthesia A medically controlled state of unconsciousness accompanied by a loss of protective reflexes, including the inability to maintain and airway and respond purposefully to physical stimulation or verbal command. The elimination of all sensation, with total amnesia for the surgical procedure. General Anesthesia The trip from awake and alert to general anesthesia has been divided into 4 stages by Guedel. – Stage 1 corresponds to conscious sedation, with stage 3 equating to general anesthesia. – Stage 2 is heralded by excitement and delirium (insert video of relative at wedding reception), with stage 4 being near cardiovascular collapse. You have consciously (moderate, stage 1) sedated a patient with IM Demerol and Versed for extraction of six teeth. What is true about the local anesthesia with epinephrine? A. Optional; may use if hemostasis is desired B. Contraindicated; epinephrine and narcotics can produce arrhythmias C. Necessary for adequate pain control D. Unnecessary; pain control achieved through your narcotic premed Sedation Golden Rules Most patients do well with iatrosedation, and one drug, the local anesthetic. When administering sedative drugs, one should still use good chair side techniques. If you are sedating a patient, then you need to know their medical history even better than if using L.A. alone. Sedation Golden Rules All sedatives/anxiolytics, regardless of the route of drug administration, can place the patient into deep sedation or general anesthesia. Most morbidity/mortality from dental office sedations are from respiratory arrest. You should be able to manage (rescue) patient one level beyond your intended depth (~manage pulp exposure if doing operative) Sedation Golden Rules Patients under 6 or over 65 require special precautions. A consciously sedated patient is less likely to have a medical emergency than a person with local anesthesia alone, but general anesthesia is risky on the medically compromised person. Each state has its own rules and regulations regarding sedation in the dental office. Analgesia: The diminution of pain in the conscious patient. Local Anesthesia: The elimination of sensations, especially pain, in one part of the body by the topical application or regional injection of a drug. Iatrosedation Deep Sedation Anxious Dead Cs Sedation G.A. Fasting not necessary…light meal Fasting recommended…clear liquids OK Fasting mandatory SBP < 120 and DBP < 80 B.P. All new patients and prior to giving local anesthesia No modification necessary SBP > 120 or DBP > 80 Iatrosedation Consider nitrous oxide or oral sedation Repeat BP in 5-10 minutes SBP DBP 120-159 and 80-99 SBP > 160 or DBP > 100 SBP < 120 and DBP < 80 No modification necessary but consider sedation for future appointments Hypertensive symptoms? Headache, chest pain Shortness of breath Visual changes, confusion Urgent physician or emergency room referral Proceed with procedure but limit epinephrine to .04 to .06 mg/ 15 minutes. Inform patient of elevated BP and refer to physician No Hypertensive Symptoms (Post dental care physician referral for all below scenarios) Elective Dental Care ASA I > 10 MET Proceed as planned. Limit time and epinephrine ASA II-IV < 10 MET No invasive care. Prescribe meds as necessary Emergency Dental Care ASA I > 4 MET Proceed with emergency care Limit time and epinephrine ASA II-IV < 4 MET Physician phone consult. Minimal emergency care only (I & D, simple extractions) The concept of metabolic equivalent or METS is in vogue. One MET is defined as 3.5 ml of 02/Kg/min. It essentially is a test of the patient’s ability to perform physical work. Some examples are: 1-4 METS (eating, dressing, walking around house, dishwashing) 4-10 METS (climbing stairs – 1 flight, walking level ground 6.4 km/hr, running short distance, game of golf) > 10 METS (swimming, singles tennis, football) People with capacities of 4 METS or less are at high risk for medical complications, while those who can perform 10 METS or more at very low risk. A person who is anxious with a BP 200/115 but can perform 10 METS of work would likely have no problems with a simple extraction. Sedation Lowers BP Grossman looked at treating hypertensive patients with 5 mg of diazepam versus the ACE inhibitor, captopril. Patients in this study presented to the emergency room with blood pressure readings greater than 190/100 and responded equally well to both treatments, reducing, on average their systolic blood pressure by an impressive 30 mm Hg, and diastolic values by 25 mm. Grossman E, Nadler M, Sharabi Y, Thaler M, Shachar A, Shamiss A. Antianxiety treatment in patients with excessive hypertension. Am J Hypertens 2005; 18(9 Pt 1):1174-7. Prevent serious medical emergencies in your practice by: Placing the office in the 3rd or 4th floor of a building without an elevator Sedation...Why not? Possible serious complications Hassles with permits Mandated CE Hours Increased malpractice $ Doing OK without it Never taught how Need to buy more equipment Once the sedation decision is made, you select: Which drug(s). Which route of drug administration. Don’t Forget: Signed Written Informed Consent for Anesthesia and the Procedure Must NOT be under influence of sedative agent while signing, or validity might be questioned Need parent/guardian’s signature for minor Practical Oral Sedation in Dentistry Part I: Pre-Sedation Consideration and Preparation Compendium, Vol 27:6, 2006 Dominic P Lu, DDS; Winston I Lu, PharmD Drug Titration The ―Bell‖ Curve -- everybody is different Routes of drug administration that allow you to quickly achieve peak blood levels give you the ability to predictably achieve the desired level of sedation. Only the I.V. and inhalational route allow for this, which is why deep sedation and G.A. are safely achieved via these routes. Bell Curve: Response after 10 mg Diazepam 0 = No Response, 10 = Ideal, 20 = General Anesthesia Routes of Drug Administration Oral Inhalation I.V. I.M. Transmucosal/Transdermal Other Each has unique positives and negatives Most states regulate dentist’s ability to perform sedation by route of drug administration, but depth of sedation is really the bottom line. Any route of drug administration may render the patient into planes where respiration is depressed, and most self-administered drug overdoses (suicides) are given via the oral route. Someday, all states will assess didactic and psychomotor competency via standardized exams on patient simulators, analogous to passing a BLS exam Oral + Acceptance No special skills Low side effects No extra equipment Pt. Can take night before No extra state permit? Variable absorption First pass effect Need compliance ~ 1 hour to peak, therefore can’t easily titrate May actually reach maximum sedation after discharge! Inhalational + Rapid onset/peak effect Can titrate Quick elimination (Pt. can often drive self home) No extra state permit? Special equipment Special skills Need compliance Waste gas Hypothesis: The risk of sedating an anxious patient with nitrous oxide/oxygen alone is less than not sedating that same person States should consider dropping any requirements for nitrous oxide permits and instead issue them to dentists who fail to recognize and treat (or refer) anxious patients I.M. + Least cooperation of all techniques No special skills Useful in emergencies Bypasses gut Titration Difficult Hurts Parenteral route, need advanced monitoring and possible ―extra‖ state permit I.V. + - Fastest onset Can titrate Most predictable (safest to go deep) Best route for emergency drugs Predictable Amnesia Special skills Need cooperation Special equipment/Permit Adverse drug reactions most rapid and intense Malpractice $ A Priori logic would suggest that the IV route should be the safest. Sedation of the Future? “PatientControlled IV Sedation” Milk of amnesia How Deep is the Patient? Monitor CNS Respiration/Ventilation Cardiovascular Temperature CNS Sedative drugs effect the CNS first, sensory nerves before motor For conscious sedation, the patient should be able to talk and respond appropriately to command University of Michigan Sedation Scale (UMSS) 0 Awake and alert 1 Minimally sedated: tired/sleepy, appropriate response to verbal conversation and/or sound 2 Moderately sedated: somnolent/sleeping, easily aroused with light tactile stimulation or a simple verbal command 3 Deeply sedated: deep sleep, arousable only with significant physical stimulation 4 Unarousable Responsiveness Scores of the Modified Observer’s Assessment of Alertness/Sedation Scale (OAA/S) 5 Responds readily to name spoken in normal tone (alert) 4 Responds lethargically to name spoken in normal tone 3 Responds only after name is called loudly and/or repeatedly 2 Responds only after mild prodding or shaking 1 Responds only after painful trapezius squeeze 0 Does not respond to painful trapezius squeeze The American Academy of Pediatric Dentistry and American Academy of Pediatrics have stressed the importance of monitoring vital signs and level of consciousness during sedation to ensure patient safety. At present, there is no objective, universally accepted measure for level of sedation. Bispectral analysis (BIS) monitoring is a relatively new, noninvasive technology used clinically to evaluate level of sedation. This technology is based on the principle that electroencephalogram wave forms change with the level of alertness. In general, when an individual is awake, electroencephalogram waveforms are high frequency and low amplitude. When the individual is deeply sedated, the frequency decreases and amplitude increases, and there are changes in relationships among different frequencies Using these principles, an algorithm for digital signal processing was developed that produces a numeric value known as the BIS index, ranging from 0 to 100. The manufacturer’s guidelines are as follows: a BIS index of 70 to 90 represents light to moderate sedation, 60 to 70 deep sedation, 40 to 60 general anesthesia, and less than 40 a deep hypnotic state. A BIS score of 0 represents no brain activity and is seen in coma and death Anesth Analg. 2006 Aug;103(2):385-9. Bispectral index does not correlate with observer assessment of alertness and sedation scores during 0.5% bupivacaine epidural anesthesia with nitrous oxide sedation. Park KS, Hur EJ, Han KW, Kil HY, Han TH. Anesthesiologists should be aware that the BIS monitor may not be sensitive enough to provide an adequate measure of the depth of sedation and hypnosis when using N2O alone for sedation. It may be better to monitor sedation clinically (e.g., with the OAA/S scale) to determine the dose requirement and the adequacy of depth of sedation and hypnosis. Respiration Morbidity/Mortality from outpatient sedations most often are due to respiratory arrest. Sedative drugs depress respiratory rate and tidal volume before the cardiovascular system. Pulse oximetry is the standard of care for assessing respiration and thus oxygenation. Also assess color of blood, breath sounds and respiratory rate Capnography (CO2 monitoring) useful for GA Pulse Oximetry Non-invasively, measures percent oxygenation of hemoglobin in capillary blood Also measures heart rate Should maintain above 90% Cardiovascular Blood Pressure EKG Heart Rate Type and Frequency of Monitoring Depends on Depth of Sedation Local Anesthesia: Pre-op B.P. and pulse Nitrous Oxide and Conscious Sedation via oral route: Continuous talking to patient, and Pre, Intra and Post-op B.P. and Resp. rate. If patient driving self home (Nitrous Only), then Pre/Post-op Trieger Test Parenteral Conscious/Deep Sedation: Continuous pulse oximetry, q5 min. B.P. G.A.: Continuous pulse oximetry, Capnography, EKG, Temperature, q5 min B.P., BIS monitor? Patient Name NITROUS OXIDE/SEDATION RECORD Student Nam e Date Faculty Name Assistant MED History (circle): Pregnancy URI Recent Retinal Surgery Psych Drug Allergies (List) _______________ PreOP Vitals: BP Pulse Oral Sedation Time Drug Resp Consent Prior to Sedation? _______________________ Dose PreOP Trieger Test IntraOP volumes: Nitrous IntraOP vitals: BP LPM Pulse O2 LPM Resp Nitrous Initiated (Time) PostOP 100% O2: minutes PostOP vitals: BP Pulse Resp PostOP Trieger Test PT Discharge Condition Discharged to (circle): Other Self PT Discharge Time Spouse Parent Other Yes No B.P./O2 Sat. + Printer E.K.G. Emergency Equipment (Crash Cart) B.L.S. most important, with the ability to breath for someone who isn’t… mouth-to-mouth, mouth-tomask, bag/valve /mask, intubation Reversal Drugs Supplemental O2 AED Automatic External Defibrillator The Ideal Anxiolytic Not antigenic Cheap Effective via any route Rapidly absorbed if given P.O. Tastes good (like chicken) Reversible --- has an antidote Makes patient happy, motionless, possibly amnesic The Ideal Anxiolytic Favorable Therapeutic Index (safe)… The perfect anxiolytic acts only on the emotion center of the CNS, not influencing the respiratory or cardiovascular systems Quickly and completely metabolized (no active by-products) without help form the patient’s kidneys, liver, etc. Non-addicting Oral Agents ETOH Barbiturates Benzodiazepines Antihistamines Narcotics Others Benzodiazepines Less respiratory depression and hangover effects compared to barbiturates., work on limbic system in ―GABAnergic‖ way, favorable T.I., schedule 4 agents, older agents cheap, antidote (Romazicon) Teratogenic, paradoxical excitement in some kids, psychologically addicting, newer agents $ Differences between drugs in this class are mostly due to their duration of action…..short being good for dentistry. Benzodiazepines: The Big 3 Diazepam (Valium) long half-life (~24 hr.) with active metabolite, cheap Triazolam (Halcion) popular sleeping pill, short half-life (~3 hours) Midazolam elixir (Versed) ―Approved‖ for use in children. New and relatively expensive, rapid absorption via oral route, PDR urges caution RE respiratory depression. Other Benzodiazepines Lorazepam (Ativan) Alprazolam (Xanax) Oxazepam (Serax) Temazepam (Restoril) Flurazepam (Dalmane) Triazolam U.S. Brand Names: Halcion Generic Available: Yes Children <18 years: Dosage not established. Adults maximum dose: 0.5 mg/day Sedation for dental procedure: 0.25 mg taken the evening before oral surgery; and/or 0.25 mg 1 hour before procedure (Sublingual administration results in a 28 percent greater bioavailability compared with oral administration, in turn resulting in higher plasma concentrations at one to two hours after the drug is administered Sublingual administration of triazolam should produce a faster onset and enhance titration ability by reducing some of the variables associated with oral administration) Metabolic Subplots CYP3A enzymes in the intestines and the liver metabolize triazolam. Antiretroviral agents inhibit CYP3A, resulting in a two-fold increase in plasma concentrations. Other CYP3A4 inhibitors include azole antifungals, ciprofloxacin, clarithromycin, diclofenac, doxycycline, erythromycin, imatinib, isoniazid, nefazodone, nicardipine, propofol, protease inhibitors, quinidine, and verapamil. Midazolam U.S. Brand Names: Versed Dosage needs to be individualized based on the patient’s age, underlying diseases, and concurrent medications. Decrease dose (by ~30%) if narcotics or other CNS depressants are administered concomitantly. Children <6 years may require higher doses and closer monitoring than older children; calculate dose on ideal body weight. Personnel and equipment needed for standard respiratory resuscitation should be immediately available during administration. Children: Conscious sedation for procedures or preoperative sedation: Oral: 0.25-0.5 mg/kg as a single dose preprocedure, up to a maximum of 20 mg; administer 30-45 minutes prior to procedure. Children <6 years and uncooperative patients may require as much as 1 mg/kg as a single dose; 0.25 mg/kg may suffice for children 6-16 years of age. Reversal Agent (Antidote) ROMAZICON is indicated for the complete or partial reversal of the sedative effects of benzodiazepines in cases where general anesthesia has been induced and/or maintained with benzodiazepines, where sedation has been produced with benzodiazepines for diagnostic and therapeutic procedures, and for the management of benzodiazepine overdose. ROMAZICON® (flumazenil) INJECTION The use of Romazicon has been associated with the occurrence of seizures. These are most frequent in patients who have been on benzodiazepines for long-term sedation or in overdose cases where patients are showing signs of serious cyclic antidepressant overdose. Practitioners should individualize the dosage of Romazicon and be prepared to manage seizures. For the reversal of the sedative effects of benzodiazepines administered for conscious sedation, the recommended initial dose of ROMAZICON is 0.2 mg (2 mL) administered intravenously over 15 seconds. If the desired level of consciousness is not obtained after waiting an additional 45 seconds, a second dose of 0.2 mg (2 mL) can be injected and repeated at 60-second intervals where necessary (up to a maximum of 4 additional times) to a maximum total dose of 1 mg (10 mL). The intramuscular, subcutaneous and sublingual routes of flumazenil injection have been studied in dogs. Although reversal of midazolam-induced respiratory depression was successful with all injection methods, the mean reversal time was significantly shorter with intravenous administration (120 versus 262 seconds with sublingual administration). Gen Dent. 2005 Jan-Feb;53(1):22-6. Rehabilitation of a fearful dental patient with oral sedation: utilizing the incremental oral administration technique. Feck AS, Goodchild JH. The treatment of fearful or anxious patients presents a myriad of problems for the dentist. In-office sedation using oral (enteral) medications is an effective means of increasing patient tolerance of invasive dental procedures. The incremental oral administration technique is a protocol that can be utilized to treat fearful or anxious patients. A case is presented in which this technique was used as an adjunct to the rehabilitation of a debilitated mouth. ADA/AAOMS Position: 2003 Titration of oral medications for the purpose of sedation is unpredictable Can produce alteration in the state of consciousness beyond the intent of the provider. Combination inhalational – enteral sedation raise the risk of oversedation Should not exceed manufacturer’s recommended dosage Balancing efficacy and safety in the use of oral sedation in dental outpatients. J Am Dent Assoc, Vol 137, No 4, 502-513. April 2006. Raymond A. Dionne, DDS, PhD; John A. Yagiela, DDS, PhD; Charles J. Coté, MD; Mark Donaldson, PharmD; Michael Edwards, DMD; David J. Greenblatt, MD; Daniel Haas, DDS, PhD; Shobha Malviya, MD; Peter Milgrom, DDS; Paul A. Moore, DMD, PhD, MPH; Guy Shampaine, DDS; Michael Silverman, DMD; Roger L. Williams, MD; and Stephen Wilson, DMD, MA, PhD. Overview. There is a strong need and demand for adult and pediatric sedation services. Using oral medication to achieve anxiolysis in adults appears to have a wide margin of safety. Mortality and serious morbidity, however, have been reported with oral conscious sedation, especially in young children. Most serious adverse events are related to potentially avoidable respiratory complications. Conclusions. Clinical trials are needed to evaluate oral sedative drugs and combinations, as well as to develop discharge criteria with objective quantifiable measures of home readiness. Courses devoted to airway management should be developed for dentists who provide conscious sedation services. State regulation of enteral administration of sedatives to achieve conscious sedation is needed to ensure safety. Aldrete Score: Maximum 10 Activity: Able to move four extremities voluntarily on command 2 Able to move two extremities voluntarily on command 1 Able to move no extremities voluntarily on command 0 Respiration: Able to breath deeply and cough freely Dyspnea or limited breathing Apnea 2 1 0 Circulation: BP +/- 20 of preanesthetic level BP +/- 21-49 of preanesthetic level BP +/- 50 of preanesthetic level 2 1 0 Consciousness: Fully awake Arousable on calling Not responding 2 1 0 O2 Saturation: 2 1 0 Able to maintain O2 saturation > 92% on room air Needs O2 inhalation to maintain O2 saturation > 90% O2 saturation < 90% even with O2 supplement What’s new in Nitrous Oxide? Absolute contraindication? More data on chronic effects More emphasis on waste gas hygiene Int J Neurosci. 2006 Jul;116(7):847-57. Psychotropic analgesic nitrous oxide for acute cocaine withdrawal in man. Gillman MA, Lichtigfeld FJ, Harker N. This article reports the first single-blind study using psychotropic analgesic nitrous oxide (PAN) for treating acute withdrawal states following cocaine abuse. Nitrous Oxide Nitrous oxide Online. Shop Target.com. Waste Gas… What’s the Problem? Early data suggested possible link between chronic, low level exposure and fertility problems Best study to date: NEJM Rowland, Oct. 1992 Specifically looked at relationship between amount of N2O exposure and the ability of dental assistants to become pregnant NEJM: Results 459 pregnant D.A. participated in study Those exposed to more than 5 hours per week of non-scavenged N2O had greater problems conceiving that was statistically significant Higher rate of spontaneous abortion D.A.s in offices that used N2O > than 5 hours per week but scavenged - no different success than offices that didn’t use N2O at all Reducing Waste Gas Can measure N2O in operatory (infrared detectors, N2O badges) Levels around DDS/D.A. can reach 1000 ppm With upgrades, can reduce this to < 50 ppm No State*/Federal laws yet, but NIOSH recommends < 50 ppm *Nitrous Oxide CDA 2007 Safe Use of Nitrous Oxide For nitrous oxide, an employer needs to monitor the work environment if the employer or any staff member believes individual staff may be exposed to concentrations in excess of 50 ppm, which is a timeweighted average permissible exposure limit (PEL) for an eight-hour day. Effective scavenging equipment and periodic inspection of equipment should keep nitrous oxide exposures to within acceptable limits. Reducing Waste Gas: How Scavenging Masks (patient must exhale through nose) Increased room ventilation (fans, open windows, open operatories) Auxiliary suction devices Frequent checks for leaks National Institute for Occupational Safety and Health http://www.cdc.gov/niosh/nitoxide.html http://www.cdc.gov/niosh/noxidalr.html Scavenging Masks Scavenging Masks Exhaled air is sucked away, out HVE line (Where does your waste gas go?) Suction set @ 45 lpm: too much, patient doesn’t get N2O , too little gas into room Mask must fit tight, otherwise gas escapes Patient exhales through mouth? — gas escapes Patient talks? — gas escapes BMJ 2002;325:532-533 (7 September) Nitrous oxide anaesthesia in the presence of intraocular gas can cause irreversible blindness. Y F Yang, a, L Herbert, a, H Rüschen, a. Retinal detachment arising from a retinal break occurs in about 1 person per 10 000 per year. Spontaneous retinal reattachment is rare, and retinal reattachment surgery is required to prevent irreversible total loss of vision. Modern vitreoretinal techniques often use intraocular gases as tamponading agents. These gases may persist in the eye for up to three months after surgery. During this period further anaesthesia using nitrous oxide will cause the intraocular gas bubble to expand, which can result in sight threatening increases in intraocular pressure. We present a case in which this occurred with devastating consequences. What’s New and Groovy in Local New Drugs Compounded Topicals Novel Delivery Methods Reversal Agent Phentolamine History W. Halsted injected cocaine for dental procedures 1884 Procaine (Novocain) synthesized 1905 Lidocaine, the first amide, released 1948 Long acting Bupivacaine became available in USA in 1983 Articaine available in Germany, 1976 and in the USA, 2000 New Drugs Articaine Ropivacaine Levobupivacaine Articaine Why do some patients not require any local anesthesia? J Hypertens. 1999 Dec;17(12 Pt 2):1799-804. Relationship between dental pain perception and 24 hour ambulatory blood pressure: a study on 181 subjects. Guasti L, Zanotta D, Petrozzino MR. OBJECTIVE: To investigate dental pain perception in a large group of essential hypertensive subjects. METHODS: A total of 130 hypertensive patients together with 51 normotensive subjects were submitted to tooth-electrical stimulation to determine the dental pain threshold (occurrence of pulp sensation) . CONCLUSIONS: The correlation between both baseline and 24 h blood pressure and pain perception has been confirmed in a large group study of normotensive and hypertensive subjects. Moreover, even among the hypertensive range of blood pressure, the higher the blood pressure is, the lower the sensitivity to pain is. Articaine In use in other countries since 1976 Marketed in US as a 4% solution under brand names Septocaine or Zorcaine with epinephrine @ 1:100,000, or 1:200,000 Has thiophene (Sulfur containing) ring Similar to Lidocaine in duration Articaine What’s Hot Better diffusion through bone-possible elimination of need for palatal injections (and mandibular blocks?) Faster onset Shorter systemic half-life (20 min. vs. 90 min. for Lidocaine) What’s Not ~1.5 X the cost Avoid in Sulfa allergic patients? Improved efficacy not universally believed For 70kg patient, can ―only‖ give ~7 cartridges (7mg/kg, 68mg/cartridge) ―Non-Surgical‖ Parasthesias? Articaine…..Bottom Line Don’t Use for Mandibular or Lingual Nerve Blocks Caution if anesthetizing ―entire mouth‖ all at once Better Diffusion through Bone Do use if anesthetizing ―entire mouth‖ over 2 3 hours (dental school full mouth extractions) Ropivacaine Levo Bupivacaine Not ―approved‖ yet for dentistry in USA Long acting like Bupivacaine Less neuro and cardio toxic Ropivacaine a mild vasoconstrictor Levo Bupivacaine, is actually the ―S‖ enantiomer of ―regular‖ Marcaine Local Anesthesia..…Some patients don’t like that persistent swollen/numb feeling* Why not ―reverse‖ the local? *Often beneficial following surgery October 2006 NOVALAR Announces Positive Phase 3 Results For Novel Dental Anesthesia Reversal Agent Novalar Pharmaceuticals, Inc. today announced that NV-101, a local dental anesthetic reversal agent, was well tolerated and met its primary endpoints in two pivotal Phase 3 studies. In both trials, NV-101 treated patients reported the return of sensation in less than half the amount of time it normally took after receiving local dental anesthesia. Novalar Raises $30 Million in Series D Financing Nov. 1 2007 - Novalar Pharmaceuticals, Inc., a specialty pharmaceutical company focused on developing and in-licensing novel oral healthcare solutions, announced today that it has closed a $30 million Series D financing. The proceeds will be used to support the U.S. launch of NV-101, a first-in-class, local dental anesthetic reversal agent, and the development of other innovative dental pharmaceuticals in Novalar's pipeline. If approved by the FDA, NV-101 will be the only local anesthetic reversal agent that accelerates the return to normal sensation and function following restorative and periodontal maintenance procedures. The product has been tested in pediatric, adolescent and adult patients. Phentolamine mesylate (a vasodilator), the active ingredient in the investigational agent NV-101, has been approved and in use in specific medical indications significantly higher doses for over 50 years. It’s the first FDA approved needlefree subgingival anesthetic agent providing patients an option in anesthesia for SRP procedures. International Academy of Compounding Pharmacists Pharmacy Compounding is... – the long-established tradition in pharmacy practice that enables physicians to prescribe and patients to take medicines that are specially prepared by pharmacists to meet patients’ individual needs. FOR IMMEDIATE RELEASE December 5, 2006 FDA Warns Five Firms To Stop Compounding Topical Anesthetic Creams The Food and Drug Administration (FDA) is warning five firms, Triangle Compounding Pharmacy, University Pharmacy, Custom Scripts Pharmacy, Hal’s Compounding Pharmacy, and New England Compounding Center, to stop compounding and distributing standardized versions of topical anesthetic creams, which are marketed for general distribution rather than responding to the unique medical needs of individual patients. FDA is concerned about the serious public health risks related to compounded topical anesthetic creams. Exposure to high concentrations of local anesthetics, like those in compounded topical anesthetic creams, can cause grave reactions including seizures and irregular heartbeats. Two deaths have been connected to compounded topical anesthetic creams J Am Dent Assoc. 2007 Oct;138(10):1333-9. The use of compound topical anesthetics: A review. Kravitz ND. Clinical Implications. Compound topical anesthetics may be an effective alternative to local infiltration for some minimally invasive dental procedures; however, legitimate concerns exist in regard to their safety. Until they become federally regulated, compound topical anesthetics remain unapproved drug products whose benefits may not outweigh their risks for dental patients. Topicals…Bottom Line Use compounded agents with great care Use esters with great care Recall some trans-mucosal systemic absorption with all drugs Alternate Delivery Methods Computer delivered Intra osseous Advantages of Intraosseous LA Improved LA efficacy (Getting the hot tooth numb) Reduce LA volume Anesthetizing only the tooth…..no more numb lips/tongue No palatal injections Disadvantages of Intraosseous Rapid absorption, possible tachycardia depending on epi concentration Drilling into roots Drilling into IAN Increased cost No Transitional Dentition Can’t use through thick bone (2nd Molars) Computer controlled injections What’s Hot What’s Not Less pain during injections….less intra and post- op too? Improved tactile sense Fun to use Cost Results may be no better if operator injects slowly Hassle to use Up your nose with a local anesthetic? ―The procedure was explained to the patient including its risks benefits and alternatives and all questions were answered.‖ Consent for local anesthesia too? Other LA Controversies…. Data is equivocal Large needles (25 gauge) hurt more than small needles ―Warming‖ the local anesthetics reduce pain during the injection Defense wins Super-Bowls Conclusions Don’t forget to diagnose anxiety; consider it a disease that can be treated For general dentistry, most patients do well with local anesthesia and iatrosedation Nitrous and/or oral sedation improves outcomes on the nervous patient Avoid using Articaine for mandibular blocks? Employ appropriate modifications, so all below answers are yes Will they get numb and sit still? Will we prevent a medical emergency? Will they stop bleeding? Will they resist infection? Will they heal? Will the operation ―work‖? Will they have a positive experience, and want to come back? Questions? jbavitz@unmc.edu