Pulmonary HT in the cath lab – practical and ideal
advertisement

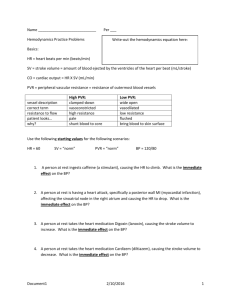
Pulmonary HT in the cath lab – practical and ideal Antoinette Cilliers Paediatric Cardiology C.H. Baragwanath Academic Hospital University of the Witwatersrand Johannesburg Pulmonary Hypertension • mPA pressure ≥ 25 mmHg (n = 14 ± 3mmHg). • or 30 mmHg with exercise. Pulmonary Vascular Disease • • • • mPA pressure ≥ 25 mmHg. PCWP (estimate of LAmp) ≤ 15 mmHg. PVR ≥ 3 Wood Units. Transpulmonary pressure gradient (TPG) ≥ 12 mmHg. Classification of PHT 5th World Symposium on PH, Nice, France, Feb 2013 • Pulmonary arterial hypertension - CHD. • Pulmonary hypertension due to left heart disease. • Pulmonary hypertension due to lung disease and or hypoxia. • Chronic thromboembolic pulmonary hypertension (CTEPH). • Pulmonary hypertension with unclear multifactorial mechanisms. JACC 2013;62(25), Suppl D: D34-41 Levels of PHT Right Heart Pre-Capillary PCWP normal (6-12 mmHg) High PVR > 3 WU Left Heart Post-Capillary PCWP > 15 mmHg Normal PVR High LAp, High LVEDP PHT and CHD D’Alto M. Eur Respir Rev 2012;21:328 • PHT is a frequent complication L > R shunts. • Increased PBF and pressure may result in vascular remodelling & endothelin dysfunction. • Leads to increased PVR and eventually reversal of the shunt or Eisenmengers syndrome (most advanced form of PHT due to CHD). • Definition of Eisenmengers syndrome (1897) PHT at systemic levels due to high PVR (> 800dynes sec/cm2 = Dr Wood) with reversed or bidirectional blood flow through a septal defect. PHT & CHD • PHT starts at birth, progression depends on type and size of defect. • Some children do not develop severe PHT – genetic predisposition ? • Usually reversible < 1-2 years. • Cyanotic Lesions develop PVD earlier < 6 mo, hypoxia is a trigger for pulmonary vasoconstriction, saturations > 85% indicate operability in infants < 1yr of age. Saxena A. PHT in CHD. PVRI 2009;2:101 Cyanosis in patient with large ASD • Not necessarily due to irreversible PVD. • May occur with normal pulmonary artery pressures due to: * Unroofed coronary sinus * Very large defect e.g. common atrium * Streaming of IVC blood to LA Saxena A. PHT in CHD. PVRI 2009;2:101 Patients at high risk of PHT Lopes AA et al. Pulm Circ 2014;4(2):330 • Age > 1-2 years. • Cardiac anomaly viz: * Truncus arteriosus * AVSD * TGV + VSD (see next slide) • Large defects. • Bidirectional shunts + periods of desaturation e.g with exertion or feeding. • Absence of heart failure. • Downs Syndrome – recurrent LRTI, decreased alveolar density and macroglossia causing chronic UAO, & endothelin dysfunction. Prevalence of PHT in patients with CHD D’Alto M. Eur Respir Rev 2012;21:328 No technique is perfect for assessment of operability in a borderline case … • Comprehensive evaluation is necessary … * Clinical evaluation(cyanosis, clubbing, presence of murmur) * CXR * ECG * ECHO * Catheterization data • It is possible to make the right decision in the majority of cases. Saxena A. PHT in CHD. PVRI 2009;2:101 Large VSD with PHT OPERABLE Cardiomegaly, prominent PA segment, increased pulmonary vasculature, pruning may occur. Eisenmenger Syndrome INOPERABLE Smaller heart, prominent PA segment, pruning. Saxena A. PHT in CHD. PVRI 2009;2:101 ECG – operable VSD + PHT Q wave present in V6, right axis, RVH ECG – inoperable PDA + PHT Q wave present in V1, right axis, poor LV forces in V6. ECHO Important for diagnosis of lesion * Direction of shunting can be seen * Severity of PHT can be assessed using TR and PR velocities Cardiac catheterization – Gold Standard ? BUT………………………… Need for cardiac catheterization? • Unnecessary in presence of overt pulmonary congestion associated with left to right shunts especially < 6 mo? • Unnecessary in patients with Truncus arteriosus, TGV + VSD, AVSD < 3 mo? • Necessary in select patients > 6mo when there is concern about irreversible PHT ? • Univentricular hearts for Glenn, Fontan surgery. • Children at high altitude < 3-6 mo ? Lopes AA, Leary PW. Cardiol Young 2009;19(E-Suppl.1):8-12 Criteria for Closing Cardiac Shunts WSPH of the WHO, Nice, France, Feb 2013 JACC 2013;62 (25), Suppl D:D34-41 PVR index ≥ 6 WU and PVR/SVR ratio ≥ 0.33 are at risk of developing PAH late after shunt closure. D’Alto et al. Int J Cardiol 2013;168:3797 Assessment of PVR & SVR several sources of error ! • Inappropriate haemodynamic and respiratory conditions. • Inadequate blood sampling and processing. • Inappropriate assumptions and approximations. Resistance is the pressure drop across the pulmonary or systemic circulation per unit of flow in a specified time period = mmHg/L/min or Wood units (u.m2) Lopes AA, Leary PW. Cardiol Young 2009;19(E-Suppl.1):8-12 Shunt measurement FICK PRINCIPLE Wilkinson JL. Heart 2001;85:113 VO2 • Direct measurement is preferable, but not practical in most institutions. • Indirect prediction (tables, nomograms, regression models) are unreliable. • If assumption is used then more than one value should be obtained – LaFarge, Lindhal, Lundell etc. • If difficulty with flow calculations use PVR/SVR ratios ? Lopes AA, Leary PW. Cardiol Young 2009;19(E-Suppl.1):8-12 Predicted VO2 calculated from regression equations published by Lindhal, Wessel et al, Lundel et al. Laitenen PO et al. Heart 1998;80:601 • LINDAHL (sedated, spontaneous breathing) < 10 kg > 10 kg VO2 = (ml/min) = 6.8 x wt (kg) + 8 VO2 = (ml/min) = 4.0 x wt (kg) + 35.8 • WESSEL et al (sedated, spontaneous breathing) VO2 = 144.8 x BSA (m2) + 5.6 • LUNDELL et al (sedated, spontaneous breathing) < 3 years VO2 = 0.4 x wt (kg) + 1.91 x ht (cm) + 0.17 x H/R (beats/min) – 91.0 BOYS > 3 years = VO2 (ml/min) = 157.9 x BSA (m2) + 0.79x H/R (beats/min) – 61.8 GIRLS > 3 years = VO2 (ml/min) = 159.0 x BSA (m2) + 0.77 x H/R (beats/min) – 61.6 LaFarge & Mietten Higher levels in younger children > lower PVR Cardiovascular Research 1970;4:23-30 Patient Cath date (day/mo/yr) Give 1 for Age<3 Sex: give 0 for yr 1 minus D female Age (yr) Weight (kg) 1 minus F Give 0 for W<10 A.N.P. 21/11/2007 3,1 0 1 1 0 14,5 1 Saturation E-mail pO2 address Saturation pO2excel based Sat programme pO2 Saturation Saturation for access to Hb(g/dL) Pulm venous Pulm venous Pulm artery Pulm artery Aorta Aorta Sup v cava Inf v cava 11,8 0,96 75 0,65 42,3 0,88 64,2 0,66 0,7 Venous-art O2 Arterio-venous O2 Mean pressure Mean pressure Mean pressure Mean difference difference (mmHg) (mmHg) (mmHg) press(mmHg) Pulmonary Systemic Pulm artery Left atrium Aorta Right atrium 5,07298 3,42468 63 12 90 10 aablopes@usp.br LaFarge & Miettinen VO2 (ml/min) 105,976506 Lindal LaFarge & Miettinen VO2 (ml/min)/m2 Lindal Bergstra VO2 (ml/min) 170,4601897 Lundell Bergstra VO2 (ml/min)/m2 100,7149853 Lundell Wessel 161,9971837 Wessel VO2 (ml/min) VO2 (ml/min)/m2 VO2 (ml/min) VO2 (ml/min)/m2 VO2 (ml/min) VO2 (ml/min)/m2 93,8 150,8746268 131,1677325 210,9795595 95,6233544 153,8074404 RESULTS Qpi Qpi Qpi Qpi Qpi 3,360159 3,193334 2,974083 4,158888 3,031895 PVRi 15,17785 PVRi 15,97077 PVRi 17,14814 PVRi 12,26289 PVRi 16,82116 Qsi Qsi Qsi Qsi Qsi 4,9774049 4,7302867 4,4055102 6,1605627 4,491148 SVRi 16,07263 SVRi 16,91229 SVRi 18,15908 SVRi 12,98583 SVRi 17,81282 Qp/Qs Qp/Qs Qp/Qs Qp/Qs Qp/Qs 0,675082 0,675082 0,675082 0,675082 0,675082 PVR/SVR 0,944329 PVR/SVR 0,944329 PVR/SVR 0,944329 PVR/SVR 0,944329 PVR/SVR 0,944329 Computer-based matrix for rapid calculation of pulmonary haemodynamics in CHD Lopes AA et al. Annals of Thoracic Medicine 2009;4:124 * * Failure to calculate dissolved O2 will result in an overestimated PBF and lower PVR than is the case. Wilkinson JL. Heart 2001;85:113 * * Some patients may achieve a substantial increase in PBF associated with a large drop in PVR despite little change in PAP. Wilkinson JL. Heart 2001;85:113 Assumed VO2 – mostly adequate ? Wilkinson JL. Heart 2001;85:113 • Young children 2-5 yrs 150 – 200ml/min/m2 • Infants younger than 3 months 130mls/min/m2 • Older infants 170mls/min/m2 • Children 1-2 years 200mls/min/m2 • Children 2-3 years 180mls/min/m2 • Adolescents 150ml/min/m2 • Adult women 100mls/min/m2 Males have a higher VO2 by 10-20% than females A tachycardia above 150 beats/min associated with a 10% increase compared with heart rates 120/min or lower Ventilation • Mechanically ventilated patients and degree of anaesthetic depth and neuro-muscular blockade – can decrease VO2 by 20-30% (Rutledge et al. Am H J 2010;160:109) Vasoreactivity test & operability ? • Precise selection of patients is not possible. • Operability is the likelihood of a favourable vs unfavourable outcome using clinical, echo and sometimes haemodynamic information. • Best outcome PVRi < 6 WUm2 & PVR/SVR ratio < 0.3. • Vasodilator challenge if PVR 6-9 WU, PVR/SVR ratio 0.3 -0.5? Lopes AA, Leary PW. Cardiol Young 2009;19(E-Suppl.1):8-12 Vasodilator test • 80-100% O2 x 10 min (Wilkinson JL. Heart 2001;85:113) • OTHER PROTOCOLS WITH NO (expensive, not always available): Maximal stimulation ≥ 90% O2 + 80ppm NO Less than maximal adequate: 20 ppm NO + any amount of O2 Intermediate protocols: 21-30% O2 + 80ppm NO or 100% O2 + 40 ppm NO Lopes AA, Leary PW. Cardiol Young 2009;19(E-Suppl.1):8-12 Magnitude of response • ≥ 20% decrease in PVRi (positive response, does not imply operability !)* • ≥ 20% decrease in PVR/SVR ratio* • PVR < 6 WUi* • PVR/SVR ratio < 0.3* • Some patients with PVR ≥ 8-9 WUi and resistance ratio ≥ 0.5 may be considered especially if large PBF, but have high operative risk. • NB - Response to pulmonary vasodilators suggests that vasculopathy is not advanced but does not predict favourable outcome. (Lopes A. Annals Thorac Med 2014;9:S21) Lopes AA, Leary PW. Cardiol Young 2009;19(E-Suppl.1):8-12 Transpulmonary gradient Index of PVR • If elevated indicates increased PVR or anatomic obstruction (e.g. pulmonary vein obstruction). • Increases following vasoconstriction of the pulmonary arteries or veins or both. Transpulmonary Gradient < 12mmHg Independent of Flow Gorlitzer et al. Transplant International 2005;18: 390 MPAP can be in excess of 40 mmHg with PVR remaining within an acceptable range, therefore PAP alone provides an incomplete picture. TPG vs PVR mPAP vs PVR Bell A et al. JACC 2009;3(11):1285 Effect of Viscosity on PVR ! TA1B (AM) Post Glenn, pre-op Fontan mPAP = 9 mmHg (<15) TPG = PAm-LAm = 9-5mmHg = 4mmHg (< 8) PBF 1L/min/m2 PVR = 9 Wood Units (<2.5) Hct = 74 % Hb 23g/dL Relative Viscosity pre-op = 2 with Hct at 70% and PVR 9 WU pre-op and 9/2 = 4.5 WU post op Viscosity • Calculations of PVR should consider effects of blood viscosity. • Resistance to flow through a tube is a function of tube geometry (length & radius) x viscosity !!! • To assess the geometric factor, resistance is divided by viscosity to derive “hindrance”. • For constant hindrance, halving the viscosity halves the resistance, and doubling the viscosity doubles the resistance. • Hence in patients with polycythemia and Ht 70% the viscosity is almost doubled !! Hoffman J. Cardiac cath and angio VISCOSITY ! Ht 74% wth hindrance of 2 Hoffman J. Cardiac cath and angio Effect of Viscosity on Rp Hoffman J. Cardiac cath and angio Effect of Viscosity on PVR TA1B (AM) Post Glenn, pre-op Fontan mPAP = 9 mmHg (<15) TPG = PAm-LAm = 9-5mmHg = 4mmHg (< 8) PBF 1L/min/m2 PVR = 9 Wood Units (<2.5) Hct = 74 % Hb 23g/dL Relative Viscosity pre-op = 2 with Hct at 70% and PVR 9 WU pre-op and 9/2 = 4.5 WU post op Clear case of irreversible PHT ? CM, 2yrs 8 mo, 9kg, LARGE PDA Mild clubbing, cyanosis in RA Conscious sedation – ivi Ketamine Room air: PCWP 7mmHg 87/47/65 PVR = 32 WU TPG = 58mmHg Qp/Qs 0.39:1 70% oxygen: Rp/Rs PCWP 1.7:1 6mmHg 90/59/76 87/47/65 PCWP 6mmHg 79/46/64 PVR = 15 WU TPG = 58mmHg 62% 83% 60% 89/0/8 85/0/8 72% 99% CM - echo CM - ECG No Q wave in V6 CM - angiography Inoperable Pulmonary Vasodilators ? Balloon Occlusion can help with decision making PDA : Pre-balloon occlusion –balanced pressures Balloon occlusion Operable Saxena A. PHT in CHD. PVRI 2009;2:101 Decisions based on calculations ! Balanced pressures in room air 115/52/83, 78% KN, 6yrs, male: From another Province Palpitations Pink, no clubbing ECHO VSD 16 mm Qp/Qs = 4.6:1 Rp/Rs = 0.27:1 PWP 11 mmHg PVR 8 WU mPAP = 83mmHg TPG = 72mmHg In 100% O2: PWP 11 mmHg PVR 2.8 WU mPAP 58mmHg 114/78/97, 87% Prominent PA segment, plethora, pruning RVH Large LA on venous return Large VSD Sudden tapering of peripheral PA vasculature No Q waves in V1 Q waves in V6 Treatment Surgical Repair of VSD • Stopped anti-failure medications 4 mo after surgery. • ECHO showed mild TR, PIG 46 mmHg (3.4m/s). • Has returned to Province of origin. • Asymptomatic. • PULMONARY VASODILATOR ?? Timing of surgery • Persistently increased PAP can become progressive with endothelial dysfunction resulting in vasoconstriction and remodelling of the pulmonary vascular bed. • Changes can reverse if defect is repaired early. • If delayed beyond 2 years of age PVR may fall but does not reach normal levels. • There may be a point of “no return” where progression continues despite correction. Beware effects of Anaesthetic agents ! Effect of Anaesthetic agents at cath • PROPOFOL: Continuous infusion 100-200 ug/kg/min * decrease SVR * increase SBF * increase R > L shunting * reduced Qp:Qs * No change in PVR and PBF • KETAMINE: Continuous infusion 50-75 ug/kg/min * increase systemic BP * No change in mPAP, SVR and PVR Oklu E et al. J of Cardiothoracic and Vascular Anaesthesia 2003:17:686 KETOFOL Pediatric Emergency Care 2012;28(12) RG, T21, 3yrs, AVSD, small VSD PDA 6 mm, ligated 1 yr before * Mild Clubbing * NPO2 * Propofol infusion PCWP 2mmHg PVR 18 WU Qp/Qs 0.5:1 Rp/Rs 16:1 mPAP 54 mmHg TPG 52mmHg 81/32/57 58% 40% 85/-15/5 100/-10/10 58% 47% Propofol infusion 54% 80/48/62 BP varied between 100/60 & 90/55 July 2013 RG, T21, 3yrs Post PDA ligation 1 yr before * Ketofol induction * Sevoflurane maintenance * Intubated * O2 30% 61% PCWP 4 mmHg PVR 10 WU Qp/Qs 0.87:1 Rp/Rs 0.9:1 mPAP 44mmHg TPG 40 mmHg 65/17/40 72% 75/0/10 66/0/10 84% 69% October 2013 RG RG Pruning, Small left atrium RG Bidirectional shunting across large ASD primum Inoperable, progressive PVD Histology • Not recommended routinely. • Useful in selected cases. • Interpretation depends on quality of tissue and expertise of pathologist. Heath Edwards. Circulation 1958;18:533 6 Grades of pathological changes in PA of pts with CHD & PHT 2 3 1 Reversible up to grade 3 - Changes do not exceed grade 3 in PHT secondary to pulmonary venous HT e.g MS. Histological changes may be distributed unequally and may be missed in a given specimen! 1 2 Grade 6 Fibrinoid necrosis is associated with severe PVR > 8 WU = refractory to O2, prostacyclin or NO 3 4 5 Rabinovitch, M. J of Clin Invest 2008 118;2372 Progression of PVD and effect on RV function Champion HC et al. Circulation 2009;120:992 PHT due to left heart Disease Right Heart Pre-Capillary PAWP normal High PVR > 3 WU Left Heart Post-Capillary PAWP > 15 mmHg Normal PVR High LAp, High LVEDP Pulmonary vein stenosis 12yrs old Haemoptysis PCWP = 40 mmHg Winter tree appearance angiographically Ideopathic Pulmonary HT Vasoreactivity Testing Guidelines for diagnosis & Rx of PHT, EHJ, 2009 Positive Vasodilator response Barst Criteria, Circulation 1999 Rashid A, Ivy D. Arch Dis Child 2005 Algorithm of Treatment Ideopathic Pulmonary HT Rashid A, Ivy D. Arch Dis Child 2005 Other less invasive diagnostic modalities Right heart catheterization and Doppler echocardiographic measurements in 152 pts D’Alto M. Int J of Cardio 2013;168:4058 Good correlation between right heart catheterization measurements and echocardiographic estimates Doppler ECHO indices for evaluation of PHT Bossone E et al. J Am Soc Echocardiography 2013;26:1-14 PVR = (TRVmax/RVOTTVI) x 10 + 0.16 e.g. 2.78/11 x 10 + 0.16 = 2.68 The ratio TRV/TVI is normally ≤ 0.15 >2.8m/s > 31 mmHg PVR distinguishes high PAP due to high flow versus pulmonary vascular disease. Not accurate with PVR > 8 Wood units. Normal PVR < 1.5 WU. Significant PH > 3 WU. Echo Guidelines. Rudski LG et al. J Am Echo 2010;23:685 TDI & the RV RV S’ or systolic excursion velocity has had population validation studies for the RV S’ < 10 cm/s should raise suspicion for abnormal RV function especially in the younger patient S’ > 10 cm/s E/E’ ratio ≥ 4 has high S & S for predicting RA pressure ≥ 10 mmHg Echo Guidelines. Rudski LG et al. J Am Echo 2010;23:685 Tissue doppler S’ lateral TVa < 7.62cm/s = PVRCATH > 6 WU/m2 TRV >3.96m/s = PVRCATH > 6WU/m2 TRV/TVIRVOT >0.149 = PVRCATH > 6WU/m2 ECHO Doppler Roushdy et al. J Saudi Heart Assoc 2012;24:233 MRI the future ? Op/Qs > 2.5:1 have a PVR ≤3.5WU Bell A et al. JACC 2009;3(11):1285 (Lopes A. Annals Thorac Med 2014;9:S21) History Examination Chest X ray Transthoracic echocardiography Catheterization END