Ò
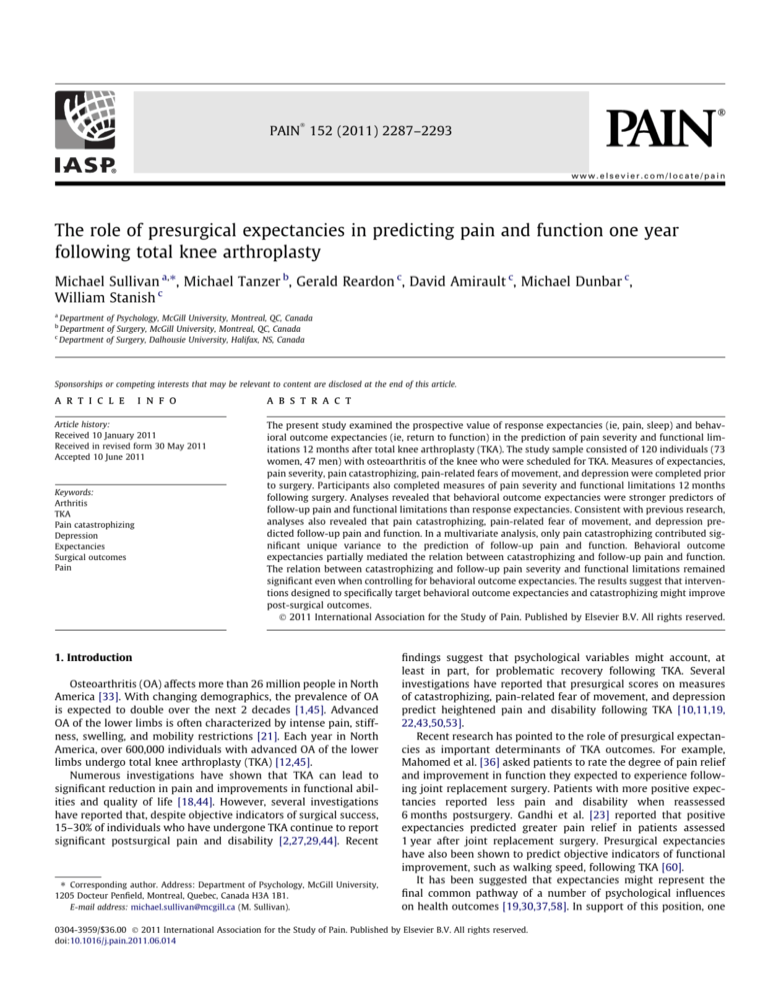
PAIN 152 (2011) 2287–2293
www.elsevier.com/locate/pain
The role of presurgical expectancies in predicting pain and function one year
following total knee arthroplasty
Michael Sullivan a,⇑, Michael Tanzer b, Gerald Reardon c, David Amirault c, Michael Dunbar c,
William Stanish c
a
b
c
Department of Psychology, McGill University, Montreal, QC, Canada
Department of Surgery, McGill University, Montreal, QC, Canada
Department of Surgery, Dalhousie University, Halifax, NS, Canada
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
a r t i c l e
i n f o
Article history:
Received 10 January 2011
Received in revised form 30 May 2011
Accepted 10 June 2011
Keywords:
Arthritis
TKA
Pain catastrophizing
Depression
Expectancies
Surgical outcomes
Pain
a b s t r a c t
The present study examined the prospective value of response expectancies (ie, pain, sleep) and behavioral outcome expectancies (ie, return to function) in the prediction of pain severity and functional limitations 12 months after total knee arthroplasty (TKA). The study sample consisted of 120 individuals (73
women, 47 men) with osteoarthritis of the knee who were scheduled for TKA. Measures of expectancies,
pain severity, pain catastrophizing, pain-related fears of movement, and depression were completed prior
to surgery. Participants also completed measures of pain severity and functional limitations 12 months
following surgery. Analyses revealed that behavioral outcome expectancies were stronger predictors of
follow-up pain and functional limitations than response expectancies. Consistent with previous research,
analyses also revealed that pain catastrophizing, pain-related fear of movement, and depression predicted follow-up pain and function. In a multivariate analysis, only pain catastrophizing contributed significant unique variance to the prediction of follow-up pain and function. Behavioral outcome
expectancies partially mediated the relation between catastrophizing and follow-up pain and function.
The relation between catastrophizing and follow-up pain severity and functional limitations remained
significant even when controlling for behavioral outcome expectancies. The results suggest that interventions designed to specifically target behavioral outcome expectancies and catastrophizing might improve
post-surgical outcomes.
Ó 2011 International Association for the Study of Pain. Published by Elsevier B.V. All rights reserved.
1. Introduction
Osteoarthritis (OA) affects more than 26 million people in North
America [33]. With changing demographics, the prevalence of OA
is expected to double over the next 2 decades [1,45]. Advanced
OA of the lower limbs is often characterized by intense pain, stiffness, swelling, and mobility restrictions [21]. Each year in North
America, over 600,000 individuals with advanced OA of the lower
limbs undergo total knee arthroplasty (TKA) [12,45].
Numerous investigations have shown that TKA can lead to
significant reduction in pain and improvements in functional abilities and quality of life [18,44]. However, several investigations
have reported that, despite objective indicators of surgical success,
15–30% of individuals who have undergone TKA continue to report
significant postsurgical pain and disability [2,27,29,44]. Recent
⇑ Corresponding author. Address: Department of Psychology, McGill University,
1205 Docteur Penfield, Montreal, Quebec, Canada H3A 1B1.
E-mail address: michael.sullivan@mcgill.ca (M. Sullivan).
findings suggest that psychological variables might account, at
least in part, for problematic recovery following TKA. Several
investigations have reported that presurgical scores on measures
of catastrophizing, pain-related fear of movement, and depression
predict heightened pain and disability following TKA [10,11,19,
22,43,50,53].
Recent research has pointed to the role of presurgical expectancies as important determinants of TKA outcomes. For example,
Mahomed et al. [36] asked patients to rate the degree of pain relief
and improvement in function they expected to experience following joint replacement surgery. Patients with more positive expectancies reported less pain and disability when reassessed
6 months postsurgery. Gandhi et al. [23] reported that positive
expectancies predicted greater pain relief in patients assessed
1 year after joint replacement surgery. Presurgical expectancies
have also been shown to predict objective indicators of functional
improvement, such as walking speed, following TKA [60].
It has been suggested that expectancies might represent the
final common pathway of a number of psychological influences
on health outcomes [19,30,37,58]. In support of this position, one
0304-3959/$36.00 Ó 2011 International Association for the Study of Pain. Published by Elsevier B.V. All rights reserved.
doi:10.1016/j.pain.2011.06.014
2288
Ò
M. Sullivan et al. / PAIN 152 (2011) 2287–2293
recent study has reported that self-efficacy expectations mediated
the relation between catastrophizing and pain in individuals with
osteoarthritic knee pain [49]. It is possible that catastrophizing,
pain-related fears, and depression might impact on health
outcomes following TKA indirectly through their influence on
expectancies.
There are important clinical implications to mediational
relations among psychological predictors of TKA outcomes. The realities of clinical practice place limits on the number of questionnaires
that can be included in assessment protocols. Identification of the
key processes by which psychological factors impact on TKA outcomes would permit streamlining assessment protocols to focus
on variables with the highest predictive values. Research examining
the processes by which psychological variables impact on TKA outcomes might also help identify key targets for psychosocial interventions designed to improve health outcomes following TKA.
In the present study, patients scheduled for TKA were assessed
1 week prior to surgery and then again 12 months postsurgery.
Multivariate analyses were conducted to assess the role of presurgical expectancies (ie, response expectancies, behavioral outcome
expectancies) as mediators of the relations between pain-related
psychological variables (ie, catastrophizing, fear of pain, depression) and postsurgical pain severity and physical function.
2. Methods
2.1. Participants
The study sample consisted of 120 individuals (73 women, 47
men) who had been scheduled for TKA at 1 of 3 hospitals in Eastern
Canada. The mean age of the sample was 67 years, with a range of
50–85 years. The mean preoperative body mass index (BMI) was
31, with a range of 20–45. The majority of the sample was married
(87%) and had completed at least 12 years of education (92%).
Sixty-seven patients had a TKA of the right knee and 54 had a
TKA of the left knee.
2.2. Measures
2.2.1. Pain and function
The Western Ontario and McMaster Universities Osteoarthritis
Index (WOMAC) was used as a measure of health status relevant to
TKA outcomes [7]. The WOMAC is a self-administered instrument
that yields a total score and subscale scores for (1) Pain, (2) Stiffness,
and (3) Physical Function. For the purposes of the present article,
only scores in WOMAC subscales for pain severity and physical function were analyzed. Higher scores reflect worse pain and function.
The WOMAC has been shown to be a valid and reliable measure of
health functioning associated with OA, and has been shown to be
sensitive to changes in function subsequent to TKA [6–8].
2.2.2. Comorbidities
Common comorbid conditions that can influence TKA outcomes
include hypertension, osteoarthrosis of other joints, diabetes mellitus, chronic obstructive pulmonary disease, and history of tobacco use. Comorbidity was assessed with the Charlson Comorbidity
Index [15]. On this measure, respondents are asked to indicate
the presence and severity of 13 different health conditions. The
number of different health conditions endorsed by the respondent
are summed to yield a total score [15].
2.2.3. Pain catastrophizing
The Pain Catastrophizing Scale (PCS; [57]) was used as a measure of catastrophic thinking related to pain. The PCS consists of
13 items describing different thoughts and feelings that individuals
may experience when they are in pain. The PCS has been shown to
have high internal consistency (Cronbach alpha = .87) [17], and to
be associated with heightened pain and disability in patients with
OA [22,53].
2.2.4. Pain-related fear of movement
The Tampa Scale for Kinesiophobia (TSK; [34]) is a 17-item
questionnaire that assesses pain-related fear of movement. The
TSK has been shown to be internally reliable (coefficient
alpha = .77) [32,63]. The TSK has been associated with various indices of behavioral avoidance and disability in patients with a variety
of health conditions, including OA [16,40,54].
2.2.5. Depressive symptoms
The Patient Health Questionnaire – 9 (PHQ-9) was used as a
measure of depressive symptom severity. The PHQ-9 is a 9-item
questionnaire that asks respondents to indicate the frequency with
which they experience each of the 9 symptoms considered in the
diagnostic criteria for Major Depression [51]. The PHQ-9 has been
shown to be a valid and reliable measure of depressive symptoms
in patients with a variety of medical conditions [24,26,35].
2.2.6. Expectancies
Patients responded to 4 questions concerning their expectancies for recovery following TKA. Two items addressed expectancies
for pain and sleep (‘‘How likely is it that one month following surgery; your pain will have decreased?; your sleep will have returned
to normal?’’). Two items addressed expectancies for return to function (‘‘How likely is it that one month following surgery; you will
have resumed your household responsibilities?; you will have
resumed your social and recreational activities?’’). For each item,
patients were asked to rate the probability of each occurrence on
a scale from 0% to 100% with the endpoints ‘‘not at all likely’’ and
‘‘extremely likely.’’ Cronbach alpha for the 4 expectancy items
was .82.
The expectancy items were chosen to reflect the distinction
between ‘‘response expectancies’’ and ‘‘behavioral outcome expectancies.’’ Predictions about nonvolitional responses (eg, pain, sleep,
emotional arousal) are referred to as ‘‘response expectancies’’ [30].
Behavioral outcome expectancies refer to individuals’ estimates of
the probability of occurrence of a given behavioral outcome that is
under volitional control [4]. In the context of recovery following
TKA, a distinguishing factor between response expectancies and
behavioral outcome expectancies is that individuals do not have
direct control over whether they will experience pain reduction
following surgery, but they do have control over the degree to
which they resume household or social activities. It has been
suggested that the processes linking response expectancies to
symptom outcomes are essentially automatic and unmediated,
while behavioral outcome expectancies are likely mediated by
motivational factors [4,30].
2.3. Procedure
Patients were recruited from 3 collaborating hospitals in eastern Canada. Ethical approval was received from the Research Ethics
Boards of the McGill University Health Centre, the Hôpital Maisonneuve-Rosemont, and the Capital Health Authority of Nova Scotia.
Participants received $25 as compensation for completing the
questionnaires. Participants completed questionnaires at the time
of their presurgical evaluation and at the time of their 12-month
postsurgical follow-up. Findings from analyses on a subsample of
these data assessed at 6 weeks post-TKA have been reported in a
previous article [53].
Criteria for inclusion in the present study included a diagnosis
of primary OA of the knee, age between 50 and 85 years, and being
Ò
2289
M. Sullivan et al. / PAIN 152 (2011) 2287–2293
scheduled for TKA at one of the 3 collaborating sites. Exclusion
criteria included: (1) diagnosis of rheumatoid arthritis; (2)
previous arthroplasty of the knee; (3) previous patellectomy; (4)
preoperative BMI >45; (5) evidence of substance abuse; (6) major
bone loss requiring structural bone graft; (7) functionally limiting
peripheral vascular disease; (8) previous fracture of the patella,
femoral condyle, or tibial plateau; and (9) requiring bilateral TKA
within 1 year of the index procedure.
Surgeries were performed by 1 of 7 surgeons. At 12-month
follow-up, radiographic analysis indicated that all prostheses were
in good mechanical alignment (2–7° of femoral-tibial valgus) with
satisfactory implant placement. Examination of radiographs
revealed no evidence of implant migration, implant breakage,
cement breakage, or progressive radiolucent lines. There was no
evidence of implant loosening and no implants were revised. None
of the study patients had evidence of ligament instability on
follow-up examination. By clinical standards, all patients in the
study sample were considered surgical successes.
2.4. Data analytic approach
Since prospective analyses were being conducted, the sample
consisted only of patients for whom complete data were available
on baseline and follow-up variables. Means and SDs were computed on sample characteristics and questionnaire scores. T-tests
for independent samples were used to compare women and men
on study measures. Pearson correlations were used to assess the
cross-sectional and prospective relations among study variables.
Multiple regression analyses were used to assess the mediating
role of expectancies for TKA outcomes at 12-month follow-up. In
the regression results reported, all tolerance coefficients were
>.60 such that no problem of multicollinearity was indicated.
Mediation analyses were conducted according to procedures outlined by Baron and Kenny [5].
3. Results
3.1. Sample characteristics
As shown in Table 1, women and men did not differ significantly
with respect to age, BMI, duration of surgery, and presurgical WOMAC pain and function scores. WOMAC pain and function scores
were similar to those reported in previous research on patients
undergoing TKA [9,38]. Women obtained significantly higher scores
than men on the comorbidity index, t (118) = 2.2, P < 0.01. Examination of individual items on the comorbidity index revealed trends
where women were somewhat more likely than men to report
depression and back pain. Men were more positive than women
about the likelihood that their sleep would return to normal within
1 month of surgery, t (188) = 2.0, P < 0.05. Men and women did not
differ significantly on any other presurgical variable.
As expected, there were significant decreases in pain, t (119) =
18.1, P < 0.001, and functional difficulties, t (74) = 17.7, P < 0.001,
from the presurgical assessment to 12-month follow-up. WOMAC
pain scores decreased from 10.6 (SD = 3.5) at presurgical evaluation to 3.5 (SD = 3.7) at 12-month follow-up. WOMAC function
scores decreased from 38.2 (SD = 12.7) at presurgical evaluation
to 14.4 (SD = 12.2) at postsurgical evaluation.
3.2. Correlations among variables
Table 2 presents the correlations among study variables assessed presurgically. Consistent with previous research, measures
of pain catastrophizing (PCS), pain-related fear of movement
(TSK), and depression (PHQ-9) were significantly intercorrelated.
Table 1
Sample characteristics on presurgical variables.
Age
BMI
Comorbid
Surgery duration (min)
WOMAC pain pre
WOMAC function pre
PCS
TSK
PHQ-9
Exp pain
Exp sleep
Exp household
Exp social-rec
Women n = 73
Men n = 47
P value
67.3 (8.4)
31.0 (5.8)
3.1 (1.4)
99.0 (26.0)
10.8 (3.5)
39.0 (12.1)
13.9 (12.6)
29.6 (13.9)
7.0 (6.6)
75.7 (19.9)
69.4 (24.4)
65.1 (26.7)
66.7 (25.7)
66.6 (7.6)
30.6 (4.0)
2.3 (1.4)
112.6 (11.8)
10.2 (3.7)
38.1 (13.6)
11.4 (9.1)
28.9 (8.3)
6.3 (7.5)
79.2 (20.5)
78.8 (23.7)
68.0 (27.9)
66.7 (27.3)
ns
ns
0.05
ns
ns
ns
ns
ns
ns
ns
0.05
ns
ns
Note: N = 120.
BMI, body mass index; Comorbid, number of comorbid health conditions; WOMAC
pain pre, Western Ontario and McMaster Universities Osteoarthritis Index
(WOMAC) Pain Score, presurgery; Function pre, WOMAC Physical Function Score,
presurgery; PCS, Pain Catastrophizing Scale; TSK, Tampa Scale for Kinesiophobia;
PHQ-9, Patient Health Questionnaire – 9; Exp pain, expectancies for pain reduction;
Exp sleep, expectancies for improved sleep; Exp household, expectancies for
resumption of household responsibilities; Exp social-rec, expectancies for
resumption of social and recreational activities.
The PCS and PHQ-9 were also significantly correlated with the
WOMAC pain and function scales. The TSK was correlated with
the WOMAC function scale but not the WOMAC pain scale. The
PCS and the PHQ-9 were significantly (inversely) correlated with
expectancies for the resumption of household and social/recreational activities, but not with expectancies for improvement in
pain sleep. The TSK was significantly (inversely) correlated with
expectancies for resumption of household responsibilities. All 4
expectancy variables were significantly intercorrelated.
Table 3 shows the prospective partial correlations (controlling
for presurgical pain severity and physical function) between presurgical variables and pain severity and self-reported disability
assessed at 1-year follow-up. Analyses revealed that behavioral outcome expectancies were more strongly correlated with follow-up
pain severity and functional limitations than response expectancies.
The PCS, TSK, and PHQ-9 were also significantly correlated with
follow-up pain severity and functional limitations. Age, BMI, comorbidities, and surgery duration were not significantly correlated with
follow-up pain severity and functional limitations.
As shown in Table 4, 2 multiple regression analyses were conducted to examine the degree to which the PCS, TSK, and PHQ-9
contributed shared or unique variance to the prediction of follow-up pain severity and physical function. For both regressions,
presurgical pain severity and physical function were entered in
the first step of the analysis, and age, sex, BMI, comorbidities,
and surgery duration were entered in the second step of the equation. Surgeons were dummy-coded as ‘‘0’’ or ‘‘1’’ and entered as a
block in the third step of the regression analysis. The PCS, TSK,
and PHQ-9 were entered in the final step of the analysis. Examination of the beta weights for the final regression equation revealed
that only the PCS contributed significant unique variance to the
prediction of follow-up pain severity (b = .27, P < 0.05) and physical
function (b = .34, P < 0.01). Given the shared variance among
psychological variables, and the unique contributions of the PCS,
mediation analyses were conducted only for the PCS.
3.3. The mediating role of expectancies in the prediction of follow-up
pain severity
As proposed by Baron and Kenny [5], 4 conditions must be met
to confirm a mediated relation: (a) the independent variable (eg,
catastrophizing) must be significantly associated with the
Ò
2290
M. Sullivan et al. / PAIN 152 (2011) 2287–2293
Table 2
Correlations among presurgical variables.
1
1. Age
2. Comorbid
3. Surg dur
4. Pain
5. Function
6. PCS
7. TSK
8. PHQ-9
9. Xpain
10. Xsleep
11. Xhous
12. Xsoc
2
.17
.01
.27**
.18*
.11
.01
.13
.02
.04
.05
.02
3
.08
.17
.16
.31**
.01
.29**
.23**
.10
.28**
.23**
4
.12
.13
.11
.09
.12
.12
.10
.03
.08
5
.75**
.40**
.15
.34**
.13
.11
.11
.08
6
.43**
.20*
.42**
.13
.07
.16
.12
7
.34**
.53**
.07
.13
.25**
.30**
8
.31**
.06
.09
.17*
.08
.01
.06
.21*
.21*
9
10
11
.46**
.46**
.46**
.49**
.56**
.80**
Note: N = 120.
Surg dur, Surgery duration; Pain, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Pain Score; Function, WOMAC Physical Function Score; PCS, Pain
Catastrophizing Scale; TSK, Tampa Scale for Kinesiophobia; PHQ-9, Patient Health Questionnaire – 9; XPain, expectancies for pain reduction; XSleep, expectancies for
improved sleep; Xhous, expectancies for resumption of household responsibilities; Xsoc, expectancies for resumption of social and recreational activities.
*
P < 0.05.
**
P < 0.01.
dependent variable (eg, follow-up pain severity); (b) the independent variable (eg, catastrophizing) must be significantly associated
with the hypothesized mediator (eg, expectancies); (c) the hypothesized mediator (eg, expectancies) must be significantly associated
with the dependent variable (eg, follow-up pain severity); and (d)
the contribution of the independent variable to the prediction of
the dependent variable must significantly decrease after controlling for the effect of the hypothesized mediator [25]. As shown in
Table 3, partial correlations indicate condition ‘‘a’’ is met for catastrophizing. In Table 2, zero-order correlations show that condition
‘‘b’’ is also met for catastrophizing. Although response expectancies
were correlated with follow-up pain and function, they were not
correlated with catastrophizing. As such, only behavioral outcome
expectancies met criteria for testing mediation. Since expectancies
for the resumption of household and social activities were highly
correlated (r = .80), scores on the variables were combined
(averaged) for the purposes of the mediation analyses.
Table 5 shows the results of 2 hierarchical regressions testing
the mediating role of expectancies in the relation between catastrophizing and follow-up pain severity (Regressions 1a and 1b).
In the first regression analysis, catastrophizing accounted for 8%
of the variance in follow-up pain after controlling for presurgical
pain severity and functional limitations. In the second regression,
behavioral outcome expectancies were entered in the second step
of the equation and accounted for 12% of the variance in follow-up
pain severity. After controlling for behavioral outcome expectancies, the contribution of pain catastrophizing to the prediction of
follow-up pain severity decreased to 4%, but remained significant.
Sobels’ test indicated significant mediation, 2.7, P < 0.01.
3.4. The mediating role of expectancies in the prediction of follow-up
physical function
Table 3
Partial correlations between presurgical variables and 1-year follow-up pain and
function.
WOMAC pain F/U
#
Pain pre
Function pre#
Age
BMI
Comorbidities
Surgery duration (mins)
PCS
TSK
PHQ-9
Xpain
Xsleep
Xhouse
Xsocial
**
.30
.29**
.02
.08
.03
.17
.31**
.23**
.24**
.06
.19*
.36**
.36**
WOMAC function F/U
.29**
.32**
.02
.05
.12
.13
.38**
.22**
.27**
.10
.27**
.45**
.42**
Note: N = 120.
F/U, follow-up; Pain pre, Western Ontario and McMaster Universities Osteoarthritis
Index (WOMAC) Pain Score, presurgery; Function pre, WOMAC Physical Function
Score, presurgery; Pain post, WOMAC Pain Score, postsurgery; Function post,
WOMAC Physical Function Score, postsurgery; PCS, Pain Catastrophizing Scale; TSK,
Tampa Scale for Kinesiophobia; PHQ-9, Patient Health Questionnaire – 9; XPain,
expectancies for pain reduction; XSleep, expectancies for improved sleep; Xhouse,
expectancies for resumption of household responsibilities; Xsocial, expectancies for
resumption of social and recreational activities.
For correlations with WOMAC pain F/U, WOMAC presurgical pain score is controlled; for correlations with WOMAC function F/U, WOMAC presurgical function
score is controlled.
#
Zero order correlations.
*
P < 0.05.
**
P < 0.01.
Table 6 shows the results of 2 hierarchical regressions examining the mediating role of behavioral outcome expectancies in the
relation between catastrophizing and follow-up physical function.
Regression 1a shows that presurgical catastrophizing accounted
for 13% of the variance in follow-up physical function. In Regression 1b, behavioral outcome expectancies were entered in the second step of the equation and accounted for 19% of the variance in
follow-up physical function, beyond the variance accounted for by
presurgical pain severity and physical function. The contribution of
catastrophizing to the prediction of follow-up physical function decreased to 6% after controlling for behavioral outcome expectancies, but remained significant. Sobel’s test revealed significant
mediation, 2.99, P < 0.001.
4. Discussion
The results of the present study join a growing literature
indicating that psychological factors have significant prognostic
value in the prediction of post-TKA pain severity and physical function [19,22,43]. The results are consistent with previous research
showing that presurgical pain catastrophizing predicts poorer
recovery from TKA. Pain-related fear of movement and depression
also predicted poorer recovery from TKA but were significant only
in univariate analyses. The findings of the present study extend
previous research in showing that behavioral outcome expectancies partially mediate the effects of pain catastrophizing on recovery outcomes following TKA.
Ò
2291
M. Sullivan et al. / PAIN 152 (2011) 2287–2293
Table 4
Regression analyses examining the role of catastrophizing, pain-related fear and depression in the prediction of follow-up pain severity and physical function.
Dependent variable
Follow-up pain severity
b
Follow-up physical function
R2change
Fchange
.10
6.4 (2, 117)
R2change
Fchange
.02
.09
.10
6.9 (2, 117)
.02
.52 (5, 112)
b
Step 1
Pain pre
Function pre
.08
.07
Step 2
Age
Sex
BMI
Comorbidities
Surgery duration
.08
.05
.12
.01
.12
.02
.61 (5, 112)
.03
.07
.08
.01
.05
Step 3
Surgeon
.04
.02
.27 (7, 105)
.03
.02
.44 (7, 105)
Step 4
PCS
TSK
PHQ-9
.27*
.10
.07
4.3 (3, 102)**
.34**
.06
.11
.13
6.2 (3, 102)**
.10
**
**
Note: Beta coefficients are from the final regression equation. For the variable ‘‘surgeon,’’ the mean beta weight for 7 surgeons is included in the table.
*
P < 0.05.
**
P < 0.01.
To our knowledge, the present study is the first to examine the
differential predictive value of response expectancies and behavioral outcome expectancies in patients undergoing TKA. Response
expectancies refer to predictions about the probability of occurrence of nonvolitional responses [30]. Examples of nonvolitional
responses include pain, sleep, and emotional reactions. Although
nonvolitional responses are considered to occur automatically,
the expectation of their occurrence can have a significant impact
on experience [30,31]. Response expectancies for pain have been
studied primarily in the context of placebo manipulations in pharmaceutical trials [41]. Behavioral outcome expectancies are distinguished from response expectancies in that they involve responses
that are under volitional control. Under conditions where individuals possess the necessary skills for execution of a particular
behavior, and when adequate incentives are in place, behavioral
Table 5
Regression analyses examining the mediating role of expectancies in the prediction of
follow-up pain severity.
outcome expectancies are said to be a major determinant of individuals’ activity choices and the effort they will expend to attain
desired outcomes [4]. In the present study, patients’ predictions
about their future resumption of household and social/recreational
activities were used as indices of behavioral outcome expectancies.
Behavioral outcome expectancies were stronger predictors of
pain severity and physical function at 1-year follow-up than
response expectancies. The results of regression analyses revealed
that behavioral outcome expectancies accounted for 12% of the
variance in follow-up pain severity and 19% of the variance in follow-up physical function. Although the relation between expectancies for pain relief and follow-up pain severity was in the expected
direction, the correlation was not significant. In the present study,
expectancies for pain relief were very high. It is possible that
Table 6
Regression analyses examining the mediating role of expectancies in the prediction of
follow-up physical function.
R2change
b
R2change
b
Fchange
Fchange
Regression 1a: the relation between catastrophizing and follow-up pain severity
Step 1
Pain pre
.12
Function pre
.06
.10
6.4 (2, 117)**
Regression 1a: the relation between catastrophizing and follow-up physical
function
Step 1
Pain pre
.04
Function pre
.11
.11
6.9 (2, 117)**
Step 2
PCS
Step 2
PCS
.31**
.08
11.1 (1, 116)***
.40***
.13
19.8 (1, 116)***
Regression 1b: catastrophizing – controlling for outcome expectancies
Step 1
Pain pre
.14
Function pre
.04
.10
6.4 (2, 117)**
Regression 1b: catastrophizing – controlling for outcome expectancies
Step 1
Pain pre
.06
Function pre
.09
.11
6.9 (2, 117)**
Step 2
OutExp
.30***
.12
18.4 (1, 116)***
Step 2
OutExp
.37***
.19
31.7 (1, 116)***
Step 3
PCS
.22**
.04
5.8 (1, 115)**
Step 3
PCS
.30**
.06
11.6 (1, 115)**
Note: N = 75.
Pain pre, Western Ontario and McMaster Universities Osteoarthritis Index
(WOMAC) Pain Score, presurgery; PCS, Pain Catastrophizing Scale; TSK, Tampa Scale
for Kinesiophobia; PHQ-9, Patient Health Questionnaire – 9; OutExp, outcome
expectancies.
Values in parentheses are degrees of freedom. Beta weights are from the final
regression equation.
**
P < 0.01.
***
P < 0.001.
Note: N = 75.
Pain pre, Western Ontario and McMaster Universities Osteoarthritis Index
(WOMAC) Pain Score, presurgery; PCS, Pain Catastrophizing Scale; TSK, Tampa Scale
for Kinesiophobia; PHQ-9, Patient Health Questionnaire – 9; OutExp, outcome
expectancies.
Values in parentheses are degrees of freedom. Beta weights are from the final
regression equation.
**
P < 0.01.
***
P < 0.001.
2292
Ò
M. Sullivan et al. / PAIN 152 (2011) 2287–2293
restricted range on participants’ responses might have reduced the
power required to demonstrate a relation between pain relief
expectancies and follow-up pain severity ratings.
In other domains of research, behavioral outcome expectancies
have also been shown to have significant prospective value. For
example, behavioral outcome expectancies have been studied
extensively in individuals recovering from work-related musculoskeletal injuries [20]. In numerous investigations, injured individuals’ expectancies about the likelihood of return to work have
emerged as one of the strongest psychological predictors of actual
return to work [20,46,47].
It has been suggested that negative outcome expectancies have
a detrimental impact on behavior or performance by compromising the effort or motivational resources that will be required to
achieve certain outcomes [3,48]. In the case of individuals who undergo TKA, low expectancies for the resumption of household, social, or recreational activities might reduce the likelihood that
individuals will choose or initiate behaviors necessary to resume
these activities, or might negatively influence individuals’ persistence in the face of challenges or obstacles in their goal pursuits.
In turn, low levels of activity might lead to deconditioning, more
rapid advance of arthritic degeneration, medical comorbidities,
demoralization, and depression.
Little is currently known about how behavioral outcomes
expectancies develop in individuals undergoing TKA or how expectancies can be manipulated for therapeutic benefit. It is possible
that communication from health care professionals might play a
significant role in the development of patients’ behavioral outcome
expectancies. It is also possible that medical information obtained
through media, the Internet, or significant others might play a role
in the development of behavioral outcome expectancies. There are
indications that individual difference variables such as catastrophizing or optimism might influence behavioral outcome expectancies [39].
Previous research has shown that catastrophizing impacts negatively on health and mental health outcomes following TKA
[10,53]. The findings of the present study suggest that behavioral
outcome expectancies represent one of the vehicles through which
catastrophizing exerts its negative impact on post-TKA pain
severity and physical function. The mediating role of behavioral
outcome expectancies as a possible determinant of the adverse
influence of catastrophizing calls for greater attention to the therapeutic management of expectancies in individuals scheduled for
TKA.
Even when controlling for behavioral outcome expectancies,
catastrophizing still contributed significant variance to the prediction of post-TKA pain and physical function. These results suggest
that catastrophizing also impacts on post-TKA pain severity and
physical function through mechanisms that are independent of
expectancies. Such mechanisms might include attentional focus
or attentional disengagement deficits [59], rumination, ineffective
coping or problem-solving [42,52], and activity avoidance [61,62].
Interpersonal processes related to social support, support entitlement, or solicitousness might also be expectancy-independent
mechanisms by which catastrophizing might impact on post-TKA
pain severity and physical function [13,14]. The role of these variables as potential mediators of relations between psychological
variables and TKA outcomes will need to be addressed in future
research.
The findings of the present study suggest that presurgical
assessment of psychological factors might help identify individuals
at risk for problematic outcomes following TKA. In addition to
catastrophizing and expectancies, pain-related fear of movement
and depression also emerged as significant predictors of followup pain and function. However, in multivariate analyses, painrelated fear of movement and depression were no longer
significant. Catastrophizing has been discussed as the cognitive
precursor to both fear and depression, which likely accounts for
the lack of unique variance contributed by fear and depression in
the prospective multivariate analyses [55,64]. Coupled with the results of previous investigations, the results of the present research
suggest that measures of catastrophizing, and expectancies should
be considered as part of standard screening of individuals being
considered for TKA [43,53,65].
At present, interventions specifically designed to target psychological risk factors for problematic outcomes following TKA have
yet to be developed and evaluated. Nevertheless, psychological risk
factors for problematic pain outcomes are considered to be
modifiable, and have been shown to be amenable to change
through targeted interventions in osteoarthritis pain, individuals’
chronic low back pain, and whiplash [28,56]. Given the magnitude
of the relation between psychosocial variables and post-TKA pain
severity and physical function, the development and evaluation
of interventions specifically designed to target psychosocial risk
in individuals scheduled for TKA would appear warranted.
Caution must be exercised in the interpretation of the study
findings. A number of exclusion criteria were used to maximize
the homogeneity of the study sample. The exclusion criteria used
in the study necessarily impact on the generalizability of the findings. The modest sample size also limits the generalizability of
findings and can be associated with increased Type II error. In addition, follow-up measures of physical function were based only on
self-report. Although self-report measures of physical function
such as the WOMAC are considered valid, the degree to which
scores reflect actual limitations in function remains unclear.
In spite of these limitations, the findings of the present study
highlight the important role of expectancies as predictors of
post-TKA outcomes. The results of the present research support
the use of measures of behavioral outcome expectancies as part
of the standard assessment of individuals scheduled for TKA. The
findings also suggest that measures of catastrophic thinking should
be considered as part of standard assessment of individuals scheduled for TKA. Psychosocial interventions might be required to foster more positive recovery in individuals who present with a
psychosocial risk profile. Future research will need to address
questions concerning the effectiveness and cost-efficacy of different approaches to targeting psychosocial risk factors in individuals
undergoing TKA.
Conflict of interest statement
None of the authors has any financial interests in the findings of
the present study.
Acknowledgements
This research was supported by a grant from the Canadian Institutes of Health Research (CIHR). The authors thank Heather Adams,
who worked as project coordinator. The authors also thank Karen
Smith, Donalda Dickey, Allan Hennigar, Kory Arsenault, and
Anne-Marie Laliberté for their assistance in participant recruitment and data collection.
References
[1] Arden N, Nevitt MC. Osteoarthritis: epidemiology. Best Pract Res Clin
Rheumatol 2006;20:3–25.
[2] Baker PN, Van der Meulen JH, Lewsey J, Gregg PJ. The role of pain and function
in determining patient satisfaction after total knee replacement. Data from the
National Joint Registry for England and Wales. J Bone Joint Surg Br
2007;89:893–900.
[3] Bandura A. Reflections on self-efficacy. Adv Behav Res Ther 1983;1:237–69.
[4] Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1977.
Ò
M. Sullivan et al. / PAIN 152 (2011) 2287–2293
[5] Baron RM, Kenny DA. The moderator-mediator variable distinction in social
psychological research: conceptual strategic, and statistical considerations. J
Pers Soc Psychol 1986;51:1173–82.
[6] Bellamy N. Pain assessment in osteoarthritis: experience with the WOMAC
osteoarthritis index. Semin Arthritis Rheum 1989;18:14–7.
[7] Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation
study of WOMAC: a health status instrument for measuring clinically
important patient relevant outcomes to antirheumatic drug therapy in
patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:
1833–40.
[8] Bellamy N, Kean WF, Buchanan WW, Gerecz-Simon E, Campbell J. Double blind
randomized controlled trial of sodium meclofenamate (Meclomen) and
diclofenac sodium (Voltaren): post validation reapplication of the WOMAC
Osteoarthritis Index. J Rheumatol 1992;19:153–9.
[9] Boonstra MC, De Waal Malefijt MC, Verdonschot N. How to quantify knee
function after total knee arthroplasty. Knee 2008;15:390–5.
[10] Brander V, Gondek S, Martin E, Stulberg SD. Pain and depression influence
outcome 5 years after knee replacement surgery. Clin Orthop Relat Res
2007;464:21–6.
[11] Brander VA, Stulberg SD, Adams AD, Harden RN, Bruehl S, Stanos SP, Houle T.
Predicting total knee replacement pain: a prospective, observational study.
Clin Orthop Relat Res 2003;416:27–36.
[12] Canadian Joint Replacement Registry. CJRR report: total hip and total knee
replacements in Canada 2004. Ottawa, ON: Canadian Institute of Health
Information; 2004.
[13] Cano A. Pain catastrophizing and social support in married individuals with
chronic pain: the moderating role of pain duration. Pain 2004;110:656–64.
[14] Cano A, Leong L, Heller JB, Lutz JR. Perceived entitlement to pain-related
support and pain catastrophizing: associations with perceived and observed
support. Pain 2009;147:249–54.
[15] Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying
prognostic comorbidity in longitudinal studies: development and validation. J
Chronic Dis 1987;40:373–83.
[16] Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling
than pain itself: evidence on the role of pain-related fear in chronic back pain
disability. Pain 1999;80:329–39.
[17] Cronbach LJ. Coefficient alpha and the internal structure of tests.
Psychometrika 1951;16:297–334.
[18] Dunbar MJ. Subjective outcomes after knee arthroplasty. Acta Orthop Scand
Suppl 2001;72:1–63.
[19] Edwards RR, Haythornthwaite JA, Smith MT, Klick B, Katz JN. Catastrophizing
and depressive symptoms as prospective predictors of outcomes following
total knee replacement. Pain Res Manag 2009;14:307–11.
[20] Fadyl J, McPherson K. Return to work after injury: a review of evidence
regarding expectations and injury perceptions, and their influence on
outcome. J Occup Rehabil 2008;18:362–74.
[21] Felson DT. An update on the pathogenesis and epidemiology of osteoarthritis.
Radiol Clin North Am 2004;42:1–9. v.
[22] Forsythe ME, Dunbar MJ, Hennigar AW, Sullivan MJ, Gross M. Prospective
relation between catastrophizing and residual pain following knee
arthroplasty: two-year follow-up. Pain Res Manag 2008;13:335–41.
[23] Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain
relief with joint arthroplasty. J Arthroplasty 2009;24:716–21.
[24] Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical
settings with the Patient Health Questionnaire (PHQ): a diagnostic metaanalysis. J Gen Intern Med 2007;22:1596–602.
[25] Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the
study of mediators and moderators: examples from the child-clinical and
pediatric psychology literatures. J Consult Clin Psychol 1997;65:599–610.
[26] Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient
Health Questionnaire-9 to measure depression among racially and ethnically
diverse primary care patients. J Gen Intern Med 2006;21:547–52.
[27] Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. Health related
quality of life outcomes after total hip and knee arthroplasties in a community
based population. J Rheumatol 2000;27:1745–52.
[28] Keefe FJ, Abernethy AP, Campbell LC. Psychological approaches to
understanding and treating disease-related pain. Annu Rev Psychol
2005;56:601–30.
[29] Kennedy DM, Hanna SE, Stratford PW, Wessel J, Gollish JD. Preoperative
function and gender predict pattern of functional recovery after hip and knee
arthroplasty. J Arthroplasty 2006;21:559–66.
[30] Kirsch I. Response expectancy as a determinant of experience and behavior.
Am Psychol 1985;40:1189–202.
[31] Kirsch I. Expectancy and conditioning in placebo analgesia: related or
independent mechanisms? Pain Forum 1997;6:59–61.
[32] Klenerman L, Slade PD, Stanley IM, Pennie B, Reilly JP, Atchison LE, Troup JD,
Rose MJ. The prediction of chronicity in patients with an acute attack of low
back pain in a general practice setting. Spine (Phila Pa 1976) 1995;20:478–84.
[33] Kopec JA, Rahman MM, Berthelot JM, Le Petit C, Aghajanian J, Sayre EC, Cibere J,
Anis AH, Badley EM. Descriptive epidemiology of osteoarthritis in British
Columbia, Canada. J Rheumatol 2007;34:386–93.
[34] Kori SH, Miller RP, Todd DD. Kinesiophobia: a new view of chronic pain
behavior. Pain Manag 1990;1:35–43.
[35] Li C, Friedman B, Conwell Y, Fiscella K. Validity of the Patient Health
Questionnaire 2 (PHQ-2) in identifying major depression in older people. J
Am Geriatr Soc 2007;55:596–602.
2293
[36] Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, Katz JN.
The importance of patient expectations in predicting functional outcomes
after total joint arthroplasty. J Rheumatol 2002;29:1273–9.
[37] Milling LS, Reardon JM, Carosella GM. Mediation and moderation of
psychological pain treatments: response expectancies and hypnotic
suggestibility. J Consult Clin Psychol 2006;74:253–62.
[38] Nunez M, Nunez E, del Val JL, Ortega R, Segur JM, Hernandez MV, Lozano L,
Sastre S, Macule F. Health-related quality of life in patients with osteoarthritis
after total knee replacement: factors influencing outcomes at 36 months of
follow-up. Osteoarthritis Cartilage 2007;15:1001–7.
[39] Peters ML, Sommer M, de Rijke JM, Kessels F, Heineman E, Patijn J, Marcus MA,
Vlaeyen JW, van Kleef M. Somatic and psychologic predictors of long-term
unfavorable outcome after surgical intervention. Ann Surg 2007;245:487–94.
[40] Picavet HS, Vlaeyen JW, Schouten JS. Pain catastrophizing and kinesiophobia:
predictors of chronic low back pain. Am J Epidemiol 2002;156:1028–34.
[41] Pollo A, Amanzio M, Arslanian A, Casadio C, Maggi G, Benedetti F. Response
expectancies in placebo analgesia and their clinical relevance. Pain
2001;93:77–84.
[42] Quartana PJ, Burns JW, Lofland KR. Attentional strategy moderates effects of
pain catastrophizing on symptom-specific physiological responses in chronic
low back pain patients. J Behav Med 2007;30:221–31.
[43] Riddle DL, Wade JB, Jiranek WA, Kong X. Preoperative pain catastrophizing
predicts pain outcome after knee arthroplasty. Clin Orthop Relat Res
2010;468:798–806.
[44] Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction
after knee arthroplasty: a report on 27,372 knees operated on between 1981
and 1995 in Sweden. Acta Orthop Scand 2000;71:262–7.
[45] Robertsson O, Dunbar MJ, Knutson K, Lidgren L. Past incidence and future
demand for knee arthroplasty in Sweden: a report from the Swedish Knee
Arthroplasty Register regarding the effect of past and future population
changes on the number of arthroplasties performed. Acta Orthop Scand
2000;71:376–80.
[46] Schultz IZ, Crook J, Berkowitz J, Milner R, Meloche GR. Predicting return to
work after low back injury using the Psychosocial Risk for Occupational
Disability Instrument: a validation study. J Occup Rehabil 2005;15:365–76.
[47] Schultz IZ, Crook JM, Berkowitz J, Meloche GR, Milner R, Zuberbier OA,
Meloche W. Biopsychosocial multivariate predictive model of occupational
low back disability. Spine (Phila Pa 1976) 2002;27:2720–5.
[48] Seligman MEP. Depression and learned helplessness in man. J Abnorm Psychol
1975;84:228–38.
[49] Shelby RA, Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Blumenthal JA. Domain
specific self-efficacy mediates the impact of pain catastrophizing on pain and
disability in overweight and obese osteoarthritis patients. J Pain
2008;9:912–9.
[50] Singh JA, Lewallen D. Age, gender, obesity, and depression are associated with
patient-related pain and function outcome after revision total hip
arthroplasty. Clin Rheumatol 2009;28:1419–30.
[51] Spitzer RL, Williams JBW, Kroenke K, et al. Patient Health Questionnaire – 9.
Prime MD Today. New York: Pfizer Inc; 1999.
[52] Sullivan M, Bishop S, Pivik J. The Pain Catastrophizing Scale: development and
validation. Psychol Assess 1995;7:524–32.
[53] Sullivan M, Tanzer M, Stanish W, Fallaha M, Keefe FJ, Simmonds M, Dunbar M.
Psychological determinants of problematic outcomes following Total Knee
Arthroplasty. Pain 2009;143:123–9.
[54] Sullivan MJ, Stanish WD. Psychologically based occupational rehabilitation:
the Pain-Disability Prevention Program. Clin J Pain 2003;19:97–104.
[55] Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA,
Lefebvre JC. Theoretical perspectives on the relation between catastrophizing
and pain. Clin J Pain 2001;17:52–64.
[56] Sullivan MJL, Adams H, Rhodenizer T, Stanish WD. A psychosocial risk factor –
targeted intervention for the prevention of chronic pain and disability
following whiplash injury. Phys Ther 2006;86:8–18.
[57] Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development
and validation. Psychol Assess 1995;7:524–32.
[58] Sullivan MJL, Rodgers WM, Kirsch I. Catastrophizing, depression and
expectancies for pain and emotional distress. Pain 2001;91:147–54.
[59] Van Damme S, Crombez G, Eccleston C. Retarded disengagement from pain
cues: the effects of pain catastrophizing and pain expectancy. Pain
2002;100:111–8.
[60] van den Akker-Scheek I, Stevens M, Groothoff JW, Bulstra SK, Zijlstra W.
Preoperative or postoperative self-efficacy: which is a better predictor of
outcome after total hip or knee arthroplasty? Patient Educ Couns
2007;66:92–9.
[61] Verbunt JA, Sieben J, Vlaeyen JW, Portegijs P, Andre Knottnerus J. A new
episode of low back pain: who relies on bed rest? Eur J Pain 2008;12:508–16.
[62] Verbunt JA, Sieben JM, Seelen HAM, Vlaeyen JW, Bousema EJ, van der Heijden
GJ, Knottnerus JA. Decline in physical activity, disability and pain-related fear
in sub-acute low back pain. Eur J Pain 2005;9:417–25.
[63] Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/
(re)injury in chronic low back pain and its relation to behavioral performance.
Pain 1995;62:363–72.
[64] Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic
musculoskeletal pain: a state of the art. Pain 2000;85:317–32.
[65] Wade JB, Riddle DL, Price DD, Dumenci L. Role of pain catastrophizing during
pain processing in a cohort of patients with chronic and severe arthritic knee
pain. Pain 2011;152:314–9.