first aid manual
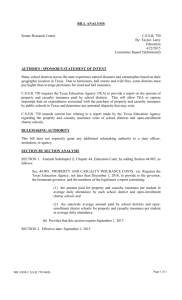
advertisement

First Aid Every Emergency. 4 First Aid Manual ©4Life Pty Ltd This work including illustrations is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the copyright holders. Requests and inquiries concerning reproduction and rights should be addressed to Suite 9, 311 Glen Osmond Road, Glenunga SA 5064. www.4lifetraining.com.au First published 2006 4 th Edition 2011 4Life First Aid Manual 4 th Edition. Authors – Bruce Cameron and Melinda Asquith Subject – First Aid Training I Contents FIRST AID OVERVIEW Introduction 2 What is First Aid? 3 Legal Considerations in First Aid 4 First Aid Kits 6 First Aid Hygiene 7 Immediate Action 8 Getting Help (Calling Emergency Services) 8 Medical Alert Devices 9 Reassuring the Casualty 10 Human Anatomy 11 The Nervous System 11 The Cardiovascular System 12 The Respiratory System 13 The Musculoskeletal System 13 The Digestive System 14 The Urinary System 14 The Endocrine System 14 The Lymphatic System 14 The Reproductive System 15 The Skin 15 WHERE TO BEGIN II 1 17 Emergency Action Plan: DRSABCD 18 Basic Life Support Flow Chart 21 Unconscious Casualty 22 24 Breathing 27 Rescue Breathing 29 Compressions – Adult, Child, Infant 32 Defibrillation 33 Automated External Defibrillation (AED) 34 Cardiopulmonary Resuscitation 36 CPR – Adult, Child, Infant 37 Cardiac Arrest 40 The Chain of Survival 41 Assessing an Accident Scene 42 Primary Assessment 42 Secondary Assessment 43 Reassuring the Casualty 46 TRAUMA Contents Airway Management 47 Bleeding and Shock 48 Nose Bleed 51 Internal Bleeding 52 Shock 53 Burns 55 Airway Burns 57 Head Injuries 58 Ear Injuries 59 Eye Injuries 61 Tooth Injuries 62 Spinal Injuries 63 Helmet Removal 64 III Chest Injuries 65 Abdominal Injuries 67 Crush Injuries 68 Fractures 69 Slings 71 Soft Tissue Injuries 73 MEDICAL Syncope (Fainting) 76 Anaphylaxis 77 Asthma 79 Hyperventilation 81 Stroke 82 Choking 83 Febrile Convulsion 86 Diabetes 87 Seizure (Fitting) 89 Heart Conditions 90 Chest Pain 90 Angina and Heart Attack 91 Poisoning 92 Drug Overdose 94 Heat Exhaustion 96 Heatstroke 97 Hypothermia 98 Drowning IV 75 100 101 Snakes 102 Spiders 103 Bee, Wasp and Ant Stings 105 Marine Creatures 106 ADVANCED FIRST AID 111 Triage – Prioritisation of Casualty Treatment 112 Road/Machine Accidents 113 Diving Emergencies 115 Behavioural Emergencies 118 Oxygen Administration 119 Back Care (Care of the Spine) 123 Emergency Childbirth 125 TECHNIQUES Techniques Contents BITES AND STINGS – ENVENOMATION 129 130 WORKBOOK 137 INDEX 149 V VI First Aid Overview FIRST AID OVERVIEW 1 Introduction Being confronted with an emergency situation can be very frightening. Knowing what to do to help the casualty in this setting is a wonderful skill. Imagine knowing that you are able to change or even save the life of your family member, friend or workmate in an emergency. The 4Life First Aid Manual is designed to assist a First Aider by providing comprehensive but accessible information and strategies for many emergency situations. The skills required to perform emergency First Aid are essentially simple but it is important to understand how to perform them appropriately and effectively. Prompt, confident application of First Aid can save lives. This manual will assist with First Aid training, as well as being a useful resource. It will also enable the retention of practical skills and knowledge received during the training sessions. The 4Life First Aid Manual adheres to all current Australian Resuscitation Council (ARC) guidelines. 2 First Aid is the initial care and treatment of the sick or injured person. It is care initiated as soon as possible after an accident or onset of illness. Prompt assistance and care in the period prior to the ambulance arrival can significantly alter the outcome for the person involved. It may mean the difference between a full or partial recovery, or even the difference between life and death. The main aims of First Aid are to: • preserve life • protect from further harm • relieve pain • promote recovery. First Aid Overview What is First Aid? Cardiopulmonary ­Resuscitation (CPR) consists of: • r escue breathing, which is also commonly known as mouth-to-mouth •e xternal Chest Compression (ECC). CPR allows oxygenated blood to circulate to vital organs such as the brain and heart. Even if rescue breathing is not possible by the First Aider, it is important to remember to apply external chest compression (ECC) as this will maintain oxygen to the person’s brain until more advanced help arrives. In order to preserve life the First Aider may be involved in providing a number of simple life-saving treatments, including Cardiopulmonary Resuscitation. 3 Legal Considerations in First Aid First Aiders should be aware of the potential legal consequences of becoming involved in an incident. However, State Acts (one of which is the ‘Good Samaritan Act’) exist to protect volunteers and First Aiders who are not accepting financial gain in a formal setting. There are four main legal considerations which relate to First Aid. 1. Duty Of Care Common Law does not impose an automatic duty on First Aiders to render aid to a casualty. However, if you choose to provide First Aid assistance you have a duty to use your knowledge and skills in a responsible way, to exercise reasonable care and to act in accordance with your level of training. You should continue to provide First Aid until: • s omeone with more qualifications than you (e.g., paramedic, doctor, nurse) relieves you • another First Aider relieves you 4 • t he casualty no longer requires First Aid • y ou become incapable of continuing. A nominated workplace First Aider has a duty of care imposed on them by law to assist another person in the workplace. A duty of care can be imposed by legislation. 2. Negligence It is an unlikely possibility that a First Aider may be sued in connection with providing First Aid. If it did occur, the likelihood is that the Australian courts would find liability only if the First Aider’s behaviour was grossly negligent. 3. Consent Under Australian law, you should ask for and receive the casualty’s consent to your treatment before you start. If the casualty is unconscious, or unable to give consent due to his or her injuries, consent may be assumed. 4. Recording If possible, a First Aider should immediately document the incident, no matter how minor. This documentation may later be used as a form of evidence. If you have a role as a First Aider at your workplace, you may have obligations under Occupational Health and Safety legislation. First Aid Overview For casualties under the age of 18, consent from a parent or guardian will be required. If a parent or guardian is not present you may proceed. When preparing a report, some general guidelines are recommended: • use pen only • do not use correction fluid • sign and date the record •e nsure your notes are accurate, factual and are based on observations rather than opinions. The information must be kept confidential. Any disclosure of personal information, particularly in the work setting, requires the written consent of the person involved. 5 First Aid Kits Possession of an appropriate, well-stocked First Aid Kit is vital in order to provide emergency assistance. Keep a kit in your car, at home and at work. Workplaces must provide a First Aid Kit under State and Territory legislation. Check with local authorities before purchasing a “workplace” First Aid Kit, as there are specific requirements. It is recommended that a personal First Aid Kit should have the following contents: 6 • • • • • • • • • • • • • • • • • • resuscitation face shield bandaids hand towels/cloths tape non-adhesive dressing alcohol swabs safety pins large combine dressings small plastic rubbish bags crepe bandages scissors 2 eye pads splinter probes – tweezers gloves (disposable) saline eye wash solution wound dressings triangular bandages bite and sting cream. Infectious diseases are those diseases which cause infections to the human body. In some cases they are transmitted by contact or cross infection. A First Aider can do little to cure an infection but can do a great deal to limit the risk of infection by: •a voiding direct contact with an infection •a voiding transmitting an infection. The following simple steps are sufficient to prevent both the First Aider and casualty from infection: •w ash hands with soap and water or rinse with antiseptic solution •w ear gloves if available. This places a barrier between the First Aider and the casualty’s body fluids. It is recommended that gloves are worn at all times but remember intact skin will still provide a good barrier for protection First Aid Overview First Aid Hygiene •u se a face shield or resuscitation mask if available when doing active Rescue breathing or Cardiopulmonary Resuscitation (CPR) – techniques which you will learn in this manual •u se clean bandages and dressings •w ash hands and change gloves between casualties •c lean up after treatment – dispose of used dressings, sharps, gloves and soiled clothing safely and correctly. Place used materials inside a plastic bag, then inside a second plastic bag, and tie securely. Do not place the bag in a rubbish bin. Dispose of it at the local council or hospital. Alternatively, give it to paramedics to dispose of. Wash hands again with soap and water, even if you used gloves. 7 Immediate Action Quick action is vital. Remember the following: • remain calm, do not panic • careful and deliberate action is of most benefit to the casualty • take control and be confident • deliver appropriate treatment. Getting Help (Calling Emergency Services) To get expert medical assistance, call an ambulance on 000 or 112: •0 00 can be dialled from any fixed or mobile telephone •1 12 is an alternative number to use when dialling from a mobile phone. It can be used when the phone is out of signal range, or even without having a sim card or pin number for the phone. In the workplace, there may be an internal number to call in emergency. This should be displayed on or near the telephone. 8 When calling for help, there are three things to remember: 1. state which service you need – ambulance, police, fire 2. s tay on the line until connected to the service requested 3. g ive as much information as you can about the emergency, including: •e xact location/address •c ity or town •n earest cross road or street • landmarks, distance from town or landmarks • your name •p hone number from where the call is being made •w hat has happened • t he number and condition of the casualties. Some individuals may wear or carry a medical alert device (e.g., bracelet, necklace, wallet card) to alert others as to the nature of their specific medical condition or illness (e.g., diabetes, allergies, asthma, epilepsy, heart conditions). First Aid Overview Medical Alert Devices Check to see if a medical alert device is evident as the information may be vital to the casualty’s treatment. A number may appear on the back of the device. This number will link to the casualty’s file which will provide further information. 9 Reassuring the Casualty Reassurance is a very important aspect of First Aid treatment. The First Aider should: •c omfort and reassure the casualty. Keep him/ her informed of what is happening. This constant reassurance is of great psychological value • r emember that others involved in the emergency (e.g., workmates, relatives, bystanders) may also need reassurance. After the incident has ended, take time to gather everyone together. Praise their efforts and let them know how important their contribution was. Some common responses include: •c rying “for no apparent reason” •d ifficulty in sleeping • inability to think clearly or to make decisions • f eeling of disbelief, shock, anger •c onstant apathy, tiredness • f eeling emotionally drained •e xcessive drinking and/or drug use • lack of appetite or extreme hunger •a nxiety, feelings of powerlessness • f ear, sadness, depression Emotional Responses • flashbacks An emergency can cause unusual stress in those who have been involved or affected by it, including First Aiders. •h eadaches, stomach problems, feeling sick. Emotional responses can appear immediately or months/years later. They are normal and expected. Every person reacts differently. 10 Understanding what you are feeling and taking positive steps such as contacting a person for counselling can help you to cope. If the feelings persist, seek professional help. A basic understanding of the human body’s anatomy and physiology assists a First Aider to recognise: •w hat is occurring within the body and why • t he potential outcomes of the initial injury or event •h ow to best care for the casualty. The human body is composed of several systems which allow the body to function effectively. An injury to one system can ultimately affect many systems or areas of the body. First Aid Overview Human Anatomy The Nervous System The Central Nervous System is made up of the brain and spinal cord. It is the control centre of the body and is extremely complex. The brain regulates most of the body’s functions, including the respiratory system. Damage to the Central Nervous System can therefore have significant and long lasting effects on the rest of the body. The Peripheral Nervous System is made up of the nerves which conduct messages from the brain and spinal cord to other parts of the body. These messages relate to movement and other sensations (taste, touch, smell etc). ©4-Life 11 The Cardiovascular System This system involves the heart, blood vessels and blood. The heart acts as a pump, pushing the blood through the blood vessels to the body’s organs and tissues. Arteries carry the oxygen-rich blood from the heart to the cells of the body. Veins carry the blood back to the heart, from where it is transported to the lungs and re-oxygenated before starting the process again. As well as oxygen, the blood carries many sugars, proteins, chemicals and other substances to support the various systems of the body. Each time the heart pumps, a pulse beat can be felt at various locations around the body. The easiest pulse points to feel are the carotid (neck) and radial (wrist) arteries. The resting heart rate of the average adult is between 60-100 beats per minute. This is dependent on age, general fitness and other medical conditions. 12 ©4-Life This system comprises the: •a irway (mouth, nose) and air passages to the lungs • lungs, including alveoli (the small air sacs within the lungs). The functions of the respiratory system are to: •p rovide oxygen to the blood • r emove the waste products (carbon dioxide). ©4-Life First Aid Overview The Respiratory System This process occurs at the alveoli in the lungs. The oxygen in the airways passes through the membranes of the alveoli and into the bloodstream, while the carbon dioxide moves the other way. The Musculoskeletal System This system comprises the bones, muscles, ligaments and tendons which support the body, protect the internal organs and provide movement. ©4-Life 13 The Digestive System This system includes the oesophagus (food pipe), stomach and intestines. Food and drink travel to the stomach via the oesophagus. In the stomach the process of digestion commences. The food is then absorbed into the body via the intestines. Other organs (liver, pancreas) also assist digestion by helping to process the food into the necessary chemical substances the body requires. The Urinary System This system includes the kidneys and bladder. The function of this important system is to flush out waste products from the body, thereby maintaining a healthy state. The Endocrine System This system involves several glands and organs which secrete hormones to activate bodily functions. An example of this is the pancreas which releases insulin necessary in the control of blood glucose (sugar) levels. The Lymphatic System This system provides a draining mechanism for the body. Lymphatic fluid is drained from the body’s tissue, is strained in the lymph nodes (in armpits, neck and groin) and then drains into the blood stream. Most toxins (e.g., snake venom) or infections absorbed 14 into the tissues are collected by the lymphatic system, which is slow moving. It is possible to reduce the movement of toxins into the circulation by applying pressure and immobilisation, as this slows the lymphatic drainage. The female reproductive system consists of the: The male reproductive system consists of the: •o varies (which produce the human egg) • testes (which produce sperm) •u terus (where the fertilised egg attaches and grows) • v agina (the birth canal). • penis. The ovaries and testes are also known as the sex glands and are therefore linked with the body’s endocrine system. First Aid Overview The Reproductive System The Skin This system includes skin, hair and nails. The skin is the body’s largest organ and its function is to protect the body from infection. The skin’s fibres are elastic and tough, so the skin can therefore stretch without easily tearing. 15 16 Where to begin WHERE TO BEGIN 17 Emergency Action Plan: DRSABCD The Emergency Action Plan to be followed during the treatment and care of a casualty comprises seven steps: • DANGER • RESPONSE • SEND FOR HELP • AIRWAY • BREATHING • CPR • DEFIBRILLATION Refer to Basic Life Support Chart on page 21. DANGER The ongoing safety of everyone at the scene must be ensured. Think of the safety of the following: • yourself • bystanders • casualties. Take time to look for potential dangers or hazards before you enter an emergency situation. Some examples of hazards are: • fire • smoke • flammable materials • gases/fumes 18 • • • • • • • • electricity fallen power lines risk of explosion chemicals unstable structures sharp objects/metal slippery surfaces oncoming traffic. Never enter an emergency situation if it is unsafe. Do not risk your own safety. Leave dangerous situations to the appropriate emergency service personnel who have the necessary equipment and training to manage the hazard. At times, some hazards may be able to be removed (e.g., turning off the electricity, removing broken glass at a motor vehicle accident). Only move a casualty if there is a hazard which cannot be safely removed, such as fire or poisonous fumes. Remember your personal protection and hygiene to maintain your safety. Dangers can include infectious diseases. The three levels of consciousness are: • f ully conscious – alert, awake, orientated to time and place • s emi-conscious – drowsy, confused •u nconscious – unresponsive. If the person responds to the Touch and Talk Technique: •c heck his/her condition •a sk if assistance is required • r ender assistance as required • call an ambulance 000 if the person appears disorientated or incoherent. RESPONSE To check for a response from a person use the Touch and Talk technique: •g ently put your hand on the person’s shoulder and talk loudly to them: “Are you alright?”, “Can you hear me?” Where to begin The Touch and Talk Technique is an effective method to wake a sleepy person or to get a reaction from a sick or inebriated person. If there is no response, the person is considered to be unconscious. •d o not shake the person to gain a response. SEND FOR HELP Call an ambulance 000. AIRWAY A clear airway is essential. To check if an airway is clear: •o pen mouth and inspect that it is clear. If visible material such as vomit and/or blood is in the airway it must be removed by the First Aider: • t urn the casualty onto his/her side to assist with the removal of the obstruction. If the person does not respond: •c all an ambulance 000 • shout for help • check the airway. 19 CPR •g ive 30 chest compressions followed by 2 rescue breaths (100 compressions in a minute). DEFIBRILLATION •a n AED (Automated External Defibrillator) is a device that adminsters an electric shock through the chest wall to the heart • If an AED is available apply now. BREATHING LOOKto see if the chest and upper abdomen rises LISTENfor the sound of breathing from nose and mouth FEELfor movement of air against your cheek and place hand on the chest and upper abdomen to check for the rise and fall. If casualty is not breathing normally. Start CPR. If casualty is breathing and unconscious consider recovery position. Refer to page 22. 20 REMEMBER! Any resuscitation is better than none at all. Where to begin Basic Life Support Flow Chart* AED = Automated External Defibrillator *Source: ARC Basic Life Support Flow Chart (2011) 21 Unconscious Casualty An unconscious casualty is unable to safely control his/her own airway due to relaxation of his/her muscles. The tongue has the potential to fall backwards across the airway, and cause an obstruction. Food, blood or vomit may also obstruct the airway. It is important that such material be removed as soon as possible. The risk of airway obstruction is increased if a breathing but unconscious casualty remains on his/her back. The most effective way of eliminating this problem is to place the casualty into the recovery position, on his/her side. This will allow for drainage of fluid from the casualty’s airway and for the tongue to fall away from the airway opening. Recovery position 22 Recovery Position Technique The First Aider should: •o ffer reassurance and an explanation to a casualty, even if he/she is unconscious • r emove any objects from casualty’s pockets such as keys/mobile phone •k neel next to the casualty, align both legs straight •p lace the casualty’s arm furthest from you at right angles to his/her body •p lace the casualty’s nearest arm to you across the chest and place the back of his/her hand against the cheek All unconscious casualties must be handled gently and every effort made to avoid any twisting or forward movement of the head and spine. •k eep the casualty’s hand pressed against the cheek and place pressure on the upper leg to roll him/her away from you (and onto his/her side) •a lign the casualty’s upper leg so that both the hip and knee are bent at right angles • t ilt the casualty’s head back to maintain an open airway •m aintain close observation of the casualty (airway, breathing, circulation). Where to begin • t ake hold of the nearest leg just above the knee, pull it up, keeping the foot flat on the ground A pregnant woman should be placed on her left side if not restricted by injury. This will prevent distress to the foetus. 23 Airway Management It is important to clear an airway in an unconscious casualty to prevent obstruction. An obstruction is often caused by the tongue falling backwards and blocking the airway. It can also be caused by foreign material (such as food, blood or vomit) obstructing the airway. Abnormal sounds in airway obstruction include: Obstruction may occur at any point within the airway, from the upper airways (windpipe and voice box) to the bronchi deep within the chest. • a complete airway obstruction makes no noise as no air is moving. Signs and Symptoms Recognition of airway obstruction To determine whether or not the casualty is breathing normally, do the following: •L OOK for chest/abdominal movement •L ISTEN at the casualty’s mouth and nose for breath sounds and abnormal noises • FEEL at the casualty’s mouth and nose for expired air. 24 • s noring – due to obstruction of upper airway by the tongue •g urgling – due to obstruction of upper airway by liquids (blood, vomit) •w heezing – due to narrowing of the airways deep in the chest The First Aider must maintain the airway for an unconscious casualty. Airway maintenance takes priority over any other injury or illness. Treatment To maintain and clear the airway of foreign material such as vomit or blood, the following is advised: • r oll the casualty onto his/her side •c arefully extend the head backwards with your hands • t o open airway, lift the chin forward by placing your fingers under bony part of the casualty’s chin • if the casualty has loose fitting dentures, remove to prevent airway obstruction. Head Tilt The Head Tilt Technique is used for a casualty who is placed on his/her side or managed on his/her back to perform CPR. To perform this technique: •p lace one hand on the casualty’s forehead •p lace fingers of opposite hand under bony part of chin • lift the chin forward and support the jaw, helping to tilt the head back. Jaw Thrust The casualty’s airway may be difficult to open. The jaw thrust technique can be applied in these circumstances. Where to begin • support the jaw and lift forward to open the casualty’s mouth To perform this technique: •g rasp the curve in the casualty’s lower jaw with both hands • lift with both hands – this should displace the jaw forward • if the lower lip closes, open with thumbs. Assess Severity* Ineffective Cough Effective Cough Severe airway obstruction Mild airway obstruction Unconscious Call ambulance 000 Commence CPR Conscious Call ambulance 000 Give up to 5 back blows if not effective Give up to 5 chest thrusts Encourage coughing Continue to check victim until recovery or deterioration Call ambulance 000 *Source: ARC Airway obstruction flow chart (2006). 25 AIRWAY (Adult) A clear airway is essential to breathe. To check that the person’s airway is open and clear, do the following: • t ilt head back gently (placing your hand on the person’s forehead) • s upport and lift the chin to open airway • t ilt the jaw forward to open the mouth. If a neck injury is suspected, tilt only enough to open airway. If the casualty’s airway is obstructed: • t urn the casualty onto his/her side • remove any visible obstruction from the casualty’s mouth, such as vomit or broken or dislodged false teeth (but leave well-fitting dentures in place). Once the airway is clear: • check the casualty’s breathing. AGE GROUPS • Infant – Under 1 year • Child – Between 1 year and 8 years • Adult – 9 years + 26 AIRWAY (Child) To check that a child’s airway is open and clear, do the following: • s upport the child’s head in horizontal position (the child is on his/her back) •o pen mouth • look inside •c lear the airway of foreign materials •d o not bend the head back – this will block the airway. Instead, place the child on his/her back and with careful movement slightly tilt back the head. AIRWAY (Infant) To check that an infant’s airway is open and clear, do the following: • s upport head in horizontal position (the infant is on his/her back) •o pen mouth • look inside •c lear the airway of foreign materials • do not bend the head back – this will occlude (block) the airway. Instead, place the infant in the neutral position (that is, how the infant would normally lie on his/her back). BREATHING (Adult) BREATHING (Child) Keep the airway open and check for normal, effective breathing by using the Look, Listen and Feel method, as follows: Keep the airway open and check for normal, effective breathing by using the Look, Listen and Feel method, as follows: •L OOK to see if the chest and upper abdomen rises and falls •L OOK to see if the chest and upper abdomen rises and falls •L ISTEN for the sound of breathing from nose and mouth • LISTEN for the sound of breathing from nose and mouth •F EEL for the rise of the chest and upper abdomen under your hand and for air against your cheek. •F EEL for the rise of the chest and upper abdomen under your hand and for air against your cheek. If breathing normally: • t urn the casualty to the Recovery Position (on his/her side) •c all an ambulance 000 •c ontinue to monitor the casualty’s condition. If breathing normally: • t urn the child to the Recovery Position (on his/her side) •c all an ambulance 000 •c ontinue to monitor the child’s condition. If not breathing normally: •c all an ambulance 000 • s tart CPR (Refer to page 36 for details of CPR). If not breathing normally: •c all an ambulance 000 • s tart CPR (Refer to page 36 for details of CPR). Where to begin Breathing 27 BREATHING (Infant) Keep the airway open and check for normal, effective breathing by using the Look, Listen and Feel method, as follows: •L OOK to see if the chest and upper abdomen rises and falls •L ISTEN for the sound of breathing from nose and mouth •F EEL for the rise of the chest and upper abdomen under your hand and for air against your cheek. 28 If breathing normally: • t urn the infant to the Recovery Position (on his/her side) •c all an ambulance 000 •c ontinue to monitor the casualty’s condition. If not breathing normally: •c all an ambulance 000 • s tart CPR (Refer to page 36 for details of CPR). When you are performing rescue breathing you are actually breathing oxygen into the casualty’s lungs. Your exhaled breath contains 16% oxygen which is close to the 20% contained in the air you breathe in. Rescue breathing is essential to provide oxygenation of the casualty’s brain, which will hopefully prevent brain damage and eventual death. Mouth-to-Mouth To perform mouth-to-mouth resuscitation: •g ently tilt head back •p inch the nostrils closed with thumb and index finger or seal nose with your cheek •p lace your mouth tightly over the casualty’s mouth •b low 2 quick breaths and observe for rise and fall of the casualty’s chest. Mouth-to-Nose If the casualty has suffered an injury to the mouth, or there is some other reason why mouth-to-mouth resuscitation is impossible, you may need to ventilate through the nose: Where to begin Rescue Breathing • gently tilt head back •c over the casualty’s mouth firmly and close your mouth around the nose, forming a tight seal •b low 2 breaths gently into casualty’s nose •o pen the casualty’s mouth to allow air to escape as the chest falls. Cover again to blow into the nose, just enough to make the chest rise. Mouth-to-Mouth-and-Nose When an infant or small child is unconscious and not breathing normally, rescue breathing can be done through the nose and mouth: •m aintain the infant’s head in a neutral position (avoid excessive head tilt) and ensure the airway is clear 29 • s eal your lips around the infant’s mouth and nose and breathe until the chest rises • r emove your mouth and, as the chest falls, allow the infant to exhale. Slow gentle breaths are required for a young child or infant. The preferred technique is to puff breath from the First Aider’s mouth. This will prevent over-inflation of the infant’s lungs. Mouth-to-Mask Mouth-to-Stoma • gently tilt head back In some instances, a casualty may breathe through an opening in the front of his/her neck called a stoma. This is due to surgery and having part of his/her trachea removed. To perform mouth to stoma resuscitation: • fi t mask firmly over casualty’s mouth and nose •p lace mouth over stoma and tightly seal (there is no need to cover mouth and nose) •d o not tilt head back too far as this may block the airway •b reathe as for mouthto-mouth 30 • if the casualty’s chest does not rise, you should cover his or her mouth and nose and continue breathing through the stoma. The most desirable form of rescue breathing is by mouthto-mask. It will help reduce the risk of cross infection and protect the First Aider from exposure to casualty’s body fluids. To perform: •d eliver rescue breaths via a valve or tube at top of mask •b low 2 gentle breaths and observe for rise and fall of the casualty’s chest. • t he casualty is not breathing normally • t he casualty’s skin is blue in colour. How to Perform Rescue Breathing AIRWAY •o pen the casualty’s airway by tilting his/her head back with one hand while lifting up his/her chin with your other hand. Check that it is clear Where to begin When to Perform Rescue Breathing • if the airway is obstructed, roll the casualty onto his/ her side and clear the obstruction. DANGER •e nsure the safety of yourself and others; check for potential dangers and hazards. RESPONSE BREATHING •c heck breathing – Look, Listen and Feel for breathing • if the casualty is not breathing normally, start CPR. •p lace the casualty flat on his/ her back on a hard surface • t ouch the casualty on the shoulder. Ask in a loud voice, “Are you okay?” • if no response, call an ambulance 000. SEND FOR HELP Call an ambulance 000. 31 Compressions – Adult, Child, Infant EXTERNAL CHEST COMPRESSIONS (Adult) •p lace heel of one hand on centre of casualty’s chest. With your other hand directly on top of first hand, depress sternum 1/3 depth of the chest •p erform 30 compressions to every 2 breaths (rate: 100 per minute). EXTERNAL CHEST COMPRESSIONS (Child) •p lace heel of one hand on centre of casualty’s chest. With your other hand directly on top of first hand, depress sternum 1/3 depth of the chest •p erform 30 compressions to every 2 breaths (rate: 100 per minute). EXTERNAL CHEST COMPRESSIONS (Infant) •p lace 2 fingers of one hand on centre of infant’s chest •c ompress chest 1/3 depth of the chest •p erform 30 compressions to every 2 breaths (rate: 100 per minute). REMEMBER! Any resuscitation is better than none at all. 32 An AED (Automated External Defibrillator) is a device that administers an electric shock through the chest wall to the heart: • if an AED is available apply now. Where to begin Defibrillation If you see this sign, this is where a defibrillator is located. 33 Defibrillation Automated External Defibrillation (AED) A Heart Attack can interfere with the heart’s rhythm and ability to pump. Instead of the heart beating normally, the rhythm can be chaotic (ventricular fibrillation) or stop the heart altogether. When this happens it is known as a cardiac arrest. When a person experiences cardiac arrest, CPR will help keep oxygen flowing to the brain, but the electric shock from an AED vastly improves the chances of restarting the heart. 34 What is An AED? An AED is a device that administers an electric shock through the chest wall to the heart. The AED assesses the person’s heart rhythm. It determines whether defibrillation is required and then administers the necessary level of shock by the user pressing the appropriate buttons. Audible and/or visual prompts will step the user through the process. The following is the process which is undertaken when using an AED: If Shock is Indicated •e nsure that everybody is clear of the casualty • in a loud voice say, “stand clear” Where to begin First Aiders can be trained to use an AED. Most AEDs are designed to be used by people without medical backgrounds. AEDs are most effective when appropriate training programs are in place. •w hen directed by AED push shock button • r epeat or “shock” as directed by AED. • s witch on defibrillator •a ttach the electrode pads to casualty as directed by diagram on pad • f ollow spoken/visual directions •e nsure that nobody touches the person whilst the AED is analysing the rhythm. Caution When using an AED remember the following: • always turn off and remove oxygen that the casualty may be using • make sure the area is dry around the casualty • the AED should be used by trained personnel • maintain safety standards • never connect the AED to anyone who is conscious • never use near explosive materials. 35 Cardiopulmonary Resuscitation Cardiopulmonary Resuscitation (CPR) consists of external chest compression (ECC) and rescue breathing. CPR allows oxygenated blood to circulate to vital organs such as the brain and heart. CPR can maintain oxygen to the person’s brain until more advanced help arrives. •a llow the chest to rise after each compression. When to Start CPR Hand Positioning for Infants A First Aider should commence CPR when a casualty: The First Aider should: • is not breathing normally. •u se 2 fingers to perform chest compressions • fi nd the centre of the chest Hand Positioning for Adults and Children •p ush down approximately 1/3 the depth of the chest The First Aider should: •k eep hand and fingers clear of the abdomen •k neel at the casualty’s side •p lace heel of one hand on the centre of the chest •p lace other hand on top interlock the fingers of both hands • with elbows straight push down to a depth of 1/3 of chest •c ompress at a rate of 100 times per minute 36 •c ompress at a rate of 100 times per minute •a llow the chest to rise after each compression. DANGER AIRWAY •e nsure the safety of yourself and others; check for potential dangers and hazards. •o pen the casualty’s airway by tilting his/her head back with one hand while lifting up his/ her chin with other hand •c heck that it is clear •p lace the casualty flat on his/ her back on a hard surface • if the airway is obstructed, roll the casualty onto side and clear. • t ouch the casualty and ask in a loud voice, “Are you okay?” BREATHING SEND FOR HELP •c heck breathing – Look, Listen and Feel for breathing RESPONSE Call an ambulance 000. Where to begin CPR – Adult, Child, Infant • if casualty is not breathing normally, start CPR. 37 CPR (Adult and Child) CPR (Infant up to 1 year old) Give 30 chest compressions followed by 2 rescue breaths (100 compressions in a minute). Give 30 chest compressions followed by 2 rescue breaths (100 compressions in a minute). • stop compressions if casualty commences breathing normally. •p lace two fingers in the centre of the chest •p ush down 1/3 the depth of the chest • perform 30 compressions to every 2 breaths (rate: 100 times per minute) • stop compressions if casualty commences breathing normally. 38 DEFIBRILLATION Whether performing 1 or 2 person CPR, you should stop: An AED (Automated External Defibrillator) is a device that administers an electric shock through the chest wall to the heart: • if the scene becomes unsafe •o n arrival of qualified help •a nother First Aider takes over • if an AED is available apply now. Where to begin When to Stop CPR • y ou are physically unable to continue • casualty commences breathing normally. 39 Cardiac Arrest Instead of the heart beating normally, the rhythm can be chaotic (ventricular fibrillation) or the heart can stop altogether. When either of the above happens it is known as a cardiac arrest. Signs and Symptoms • t he casualty is unconscious • t he casualty has no normal breaths but may appear to gasp on occasions • t he casualty has a short period of jerky body movement. 40 Treatment This is an extreme medical emergency. Without immediate help the person will die. The First Aider should proceed as follows: • DRSABCD • call an ambulance 000 • commence immediate CPR. Chain Of Survival is a term used to describe the fourstage approach for a response to an emergency situation such as cardiac arrest. The survival Call of a casualty from cardiac arrest can significantly improve when all four links of the Chain of Survival are strong. CPR The four Links in the Chain of Survival are: 1st Link – Early Access Call fast (000). Get emergency medical help quickly to the cardiac arrest casualty. 2nd Link – Early CPR Early CPR helps circulate blood that contains oxygen to the vital organs. This buys time, which can be life-saving. Where to begin The Chain Of Survival Defib Ambulance 3rd Link – Early Defibrillation Most victims of sudden cardiac arrest need an electric shock called defibrillation to restore the heart to a regular rhythm. 4th Link – Early ACLS (Early Advanced Care Life Support) This is given by trained medical personnel such as Paramedics who provide further care. 41 Assessing an Accident Scene Approaching a scene On approaching a scene the first priority is your own safety. Before approaching, make sure the scene is safe for yourself, bystanders and the casualty. Once the scene is safe you should note the following: • t he number of casualties • t he possibility for assistance from bystanders •w hat has actually occurred (e.g., car accident, house fire or heart attack). Primary Assessment 42 The aim of the primary assessment is to detect serious and immediate lifethreatening injuries. The primary assessment is a systematic approach of assessing and treating a casualty. It can be applied to both medical and traumarelated emergencies. Unconscious Once you have gained access to the casualty, check to see if he/she is conscious or unconscious. • call an ambulance 000. If the casualty is unconscious: •c heck that the airway is clear (If not, clear the airway) •c heck for normal breathing •c heck for any haemorrhage. If present, control with direct pressure over wound • “Can you take a deep breath?” Do not delay urgent treatment in order to gain a detailed history from the casualty. This history can be obtained later or, if possible, have a bystander speak to witnesses or relatives to gain vital information. • “ Can you cough?” Start with open ended questions, such as: • “ Can you describe what happened?” • “ Where is the pain?” Simple questions will enable the First Aider to gather important information quickly. It will also give a good indication of what the casualty may be suffering from. The information gained by the First Aider is also very important once the casualty has been transferred to hospital. Your history-taking and observations may be crucial in the treatment of the casualty. Where to begin Conscious Secondary Assessment A secondary assessment is conducted following the primary assessment. The secondary assessment involves: • make sure you are able to see the skin when examining the casualty. Take special care when checking the body and limbs: •h istory-gathering, to determine any medical and/or trauma-related problems that a casualty may be suffering • ask the casualty if you may look under or remove clothing •a systematic head to toe examination of a casualty. • if possible, have another person present The head-to-toe examination should be systematic and thorough so that no injuries are missed: •b e careful not to unnecessarily move the casualty while performing the secondary survey as movement may cause further injury. •e xplain to the casualty why this is necessary 43 HEAD SHOULDERS AND CHEST Look at and feel the casualty’s head and face. Look for the following: Look at and feel the casualty’s shoulders, collarbone and chest for the following: • abrasions • tenderness when touching ribs • bruising • bruising • fluids in the nose or ears • swelling • damage to the eyes. •c heck for unequal rise and fall of chest during respirations. NECK Look at and feel the casualty’s neck for the following: • tenderness • bruising • deformity • bleeding. Check for Medical Alert necklace/bracelet. ABDOMEN AND PELVIS Look at and feel the casualty’s abdomen and pelvis for the following: • tenderness • bruising • swelling • rigidity • wounds • press on both of the protruding bones in the pelvis and note if there is any pain or deformity. 44 BACK AND SPINE Look at and feel the casualty’s arms and legs for the following: Look at and feel the casualty’s back and spine for the following: • bruising • bruising • deformity • deformity • haemorrhage • haemorrhage • pain and tenderness • pain and tenderness. • sensation in all limbs To perform an examination of the back and spine, slide your hand carefully under the casualty. • check the pulse in both wrists •c heck the pulse at the top of each foot Where to begin ARMS AND LEGS •c heck for full range of movement. Check for Medical Alert bracelet/necklace 45 Reassuring the Casualty Reassurance is a very important aspect of First Aid treatment. The First Aider should: •c omfort and reassure the casualty •k eep him/her informed of what is happening • t his constant reassurance is of great psychological value • r emember that others involved in the emergency (e.g., workmates, relatives, bystanders) may also need reassurance •a fter the incident has ended, take time to gather everyone together •p raise everybody’s efforts and let them know how important their contribution was. Emotional Responses An emergency can cause unusual stress in those who have been involved or affected by it, including First Aiders. Emotional responses can appear immediately or months/ 46 years later. They are normal and expected. Every person reacts differently. Some common responses include: •c rying for no apparent reason •d ifficulty sleeping • inability to think clearly or to make decisions • f eeling of disbelief, shock, anger •c onstant apathy, tiredness • feeling emotionally drained •e xcessive drinking and/or drug use • lack of appetite or extreme hunger •a nxiety, feelings of powerlessness • f ear, sadness, depression • flashbacks •h eadaches, stomach problems, feeling sick. Understanding what you are feeling and taking positive steps can help you to cope. If the feelings persist, seek professional help. Trauma TRAUMA 47 Bleeding and Shock The average adult body contains between five and seven litres of blood, which circulates around the body in order to keep the organs supplied with oxygen. Blood is composed of: • r ed blood cells, which carry oxygen and waste products •w hite blood cells, which fight infection •p latelets, which assist in the clotting process •p lasma, the liquid which supports all these cells. Some indicators of external bleeding include: • it is obvious and apparent • it is caused by cutting, perforating or tearing of the skin • s erious wounds involve damage to blood vessels • t he severity depends on the type of wound and which blood vessels are damaged. Arteries Blood moves around the body under pressure through the heart and blood vessels. If either the blood volume or pressure is inadequate the body’s functions soon begin to fail. Arteries carry blood rich with oxygen away from the heart. The blood can spurt with each heart beat and is bright red in colour. Bleeding or haemorrhage causes both the volume and the pressure to decrease through loss of blood through the system, and therefore poses a great threat to survival. It is one of the most common causes of death in accidents. Veins There are two types of bleeding: external and internal. 48 External Bleeding Blood from veins is dark red and flows from the wound. Capillaries Blood from capillaries is dark red in colour and oozes from the wound which is usually close to the skin. No Embedded Object Types of wounds which can cause external bleeding include: •a pply direct pressure with sterile or clean pad •g raze – abrasion of skin • incision – a wound made by slicing (e.g., sharp knife/ piece of metal) which can bleed extensively • laceration – deep wound with tissue loss •a mputation – severed body part (e.g., a limb) •p uncture/embedded object (e.g., bullet/knife wound). Trauma Types of Wounds • lie the casualty down •e levate and support the injured part (if possible, above the level of the heart) •a pply firm bandage to hold pad in place • If bleeding does not stop, remove bandage and apply firm pressure to the wound • t reat for shock if required (Refer to page 53) •c heck circulation regularly. Management of External Bleeding When treating life-threatening bleeding, the First Aider should do the following: • DRSABCD •c all an ambulance 000 as soon as possible •e xpose the wound and check for visible embedded object (do not remove the embedded object). 49 Embedded Object/Puncture Wound: Incisions/Lacerations: • DRSABCD •c all an ambulance 000 •c all an ambulance 000 •c heck wound for foreign matters •c heck wound but do not remove any embedded object •a pply indirect pressure around the wound • s tabilise with ring pad and non-stick dressing • DRSABCD •a pply pressure – bring sides of wound together •a pply a non-stick dressing and bandage • immobilise and elevate. •a pply a firm bandage •e levate the injured limb and immobilise. Amputation: • DRSABCD •c all an ambulance 000 Treatment Abrasions/Grazes: •a pply direct pressure to reduce the bleeding • DRSABCD • check wound •a pply large pad or dressing to wound • s wab with antiseptic solution or sterile water • t reat for shock (Refer to page 53) • apply non-stick dressing. • if possible, immobilise and elevate injured limb •c ollect amputated body part and seal in a plastic bag. Do not wash or clean it •p lace amputated body part in iced water • f reezing will kill tissue so do not allow the body part to directly contact ice. 50 Treatment Treat a nose bleed in the following way: Trauma Nose Bleed •h ave the casualty lean slightly forward and pinch the fleshy part of the nose just below the bone •m aintain this position for at least 10 minutes. Warm weather or exercise may mean that up to 20 minutes or more may be required to cease the bleeding. However: • if bleeding persists, obtain medical assistance •a dvise the casualty not to blow or pick nose for several hours. 51 Internal Bleeding Internal bleeding is often difficult to detect, as there may be no direct evidence of the bleeding. A thorough history of the incident or illness is vital to give the First Aider the necessary clue as to whether internal bleeding is a possibility Treatment and Care Some visible indicators of internal bleeding include: • if the casualty is unconscious, place him/her in recovery position • obvious blood loss • s igns of shock (pale, cool, clammy skin). 52 • DRSABCD •c all an ambulance 000 • rest and reassurance • if the casualty is conscious, position him/her supine (face up) with legs raised •g ive nothing by mouth. Shock is a life-threatening condition. It occurs when the body’s blood circulation is inadequate to meet the oxygen demands of the major organs of the body. Shock is a deteriorating condition which requires active treatment, as the casualty may rapidly progress to a state of total body shutdown. A delay of even a few minutes may lead to death, so prompt care is vital. Normal Common Causes of Shock • loss of blood Trauma Shock • loss of body fluids (e.g., due to extensive burns, dehydration, severe vomiting and diarrhoea) •h eart attack •a naphylaxis (severe allergic reaction) • s epsis (severe infection). Signs of Shock Skin Pink, Warm and Dry Pale, Cold and Clammy Conscious Level Alert and Orientated Confused, drowsy, aggressive 53 Signs and Symptoms Treatment and Care A casualty suffering from shock may display the following symptoms: • DRSABCD •pale, cool, clammy skin • r apid, shallow breathing • r apid, weak pulse •c asualty is irritable or confused • nausea/vomiting •c asualty is collapsed/ unconscious. 54 •c all an ambulance 000 •c ontrol any bleeding • r est and reassurance •m aintain the casualty’s body temperature by covering with a blanket • if the casualty is conscious, position him/her supine (face up) with legs elevated • if the casualty is unconscious, place him/her in recovery position. Burns can be a minor problem or a life-threatening emergency. Distinguishing a minor burn from a more serious burn may be difficult and involves determining the degree of damage to the casualty’s skin and tissues. Causes The causes of burns are various and can include the following: • fire • sun • chemicals Partial thickness (second-degree) burns: Trauma Burns • t he first and second layers of the casualty’s skin are affected • t he skin is red and blistered • s evere pain and swelling may occur. Full thickness (third-degree) burns: •a ll layers of the casualty’s skin are affected • t here is charring or whitening of the skin •d ue to nerve damage, the casualty may feel no pain at all. • heated objects • fluids • electricity. Treatment When treating a burn the First Aider should do the following: Signs and Symptoms • DRSABCD Superficial (first-degree) burns: •c all an ambulance 000 •o nly the outer layer of the casualty’s skin is affected • if the casualty’s skin is not broken, run cool water over the burn for 20 minutes. Do not use ice • t he skin is usually red • s evere pain and swelling may occur. •c over the burn with a sterile bandage or non stick clean cloth 55 •p lastic wrap is a commonly used dressing for burns •d o not apply lotions, creams or powder • r emove clothing that has not adhered to casualty’s skin • r emove any constrictive clothing and jewellery •d o not break blisters • fl ush skin of any chemicals that may cause burning. Note: if a chemical gets into the casualty’s eyes, flush them with water immediately. Continue to flush the eyes with running water for at least 20 to 30 minutes. All infants or children with burns should be medically assessed. 56 This can be due to smoke and heat from a fire, which can cause swelling. This swelling can lead to a life-threatening condition due to airway obstruction. Treatment • DRSABCD Trauma Airway Burns • call an Ambulance 000. Signs and Symptoms A casualty suffering from an airway burn may display the following symptoms: • f acial hair loss • s oot around nose and mouth •c oughing, hoarse voice/ casualty unable to talk •d ifficulty breathing. Serious burns that need immediate emergency attention include those which affect the airways and cause breathing difficulty. 57 Head Injuries The main concern with a head injury is that there may be bleeding or swelling inside the skull. This can occur even if the skull does not appear damaged. Blood and/or swelling that collects within the skull may eventually put pressure on the brain and cause serious brain damage. Head injuries may be classified as: 1. O pen Head Injury – head injury accompanied by an open head wound. 2. C losed Head Injury – there is no obvious sign of injury present. Signs and Symptoms • unconsciousness •p ain at the site of injury •d eformity of the skull •blood or straw-coloured fluid draining from the ears or nose •c hange in the level of consciousness (the person gets progressively sleepier) •a gitation and combativeness •n ausea and vomiting •b ruising around the eyes and ears after the injury •p oor memory. 58 Treatment • DRSABCD •c all an ambulance 000 • treat and control haemorrhage •c over wound with dressing • r est the casualty and watch closely • if the casualty has an altered level of consciousness and you are concerned about airway obstruction, place in the recovery position making sure the head and neck are kept in alignment •c over ear with sterile pad. If you suspect a head injury in a person, or he/she has been knocked unconscious, seek medical advice immediately. Occasionally foreign bodies or insects lodge in the ear canal. This may lead to an ear infection or a far more serious injury such as a ruptured ear drum. Signs and Symptoms A casualty suffering from an ear injury may display the following symptoms: •h olding the affected ear lower than the non-affected side • r edness visible in the ear canal Treatment Object in Ear Trauma Ear Injuries •c alm and reassure the casualty • if the object is sticking out gently remove it by hand or with a pair of tweezers • if you think a small object may be lodged within the ear but you cannot see it, do not reach into the ear canal with tweezers. You may do more harm than good • t ry using gravity to remove object • t ilt head to affected side • t he First Aider can see a possible foreign body in the casualty’s ear • s hake it gently towards the direction of the ground to hopefully dislodge the object • s mell or discharge from ear. • if the object does not come out, seek medical help. 59 Insect in Ear Ruptured Ear Drum • do not let the casualty place finger in the ear as may cause the insect to go further in If the casualty has a ruptured ear drum he/she will experience severe pain. The First Aider should: • t urn the casualty’s head so the affected side is facing up • t he insect may then crawl to the top of the ear •p ouring a small amount of olive oil or baby oil into the ear may float the insect out • seek medical advice. 60 •p lace sterile pad over ear • if casualty has drainage from ear then lie the casualty with the affected ear down to allow drainage to occur • s eek medical help. An eye injury can be serious and difficult to manage. It may lead to permanent damage. Seek medical help if concerned. Signs and Symptoms • s quinting and/or spasm of the eyelids • rubbing of the eye Foreign Bodies • flush the eye with disposable eyewash or clean running water for a short period of time • if flushing does not remove the object it may be possible to remove it from the eye with a well-moistened surgical spear on an applicator stick • redness of the eye. • if the foreign body cannot be removed, pad the eye and seek medical assistance. Treatment Embedded Objects Chemical Injuries •c all an ambulance 000 •c all an ambulance 000 •d o not attempt to remove the object • discharge, watery eye • fl ush the eye for at least 20 minutes, including under the eyelids. It may be necessary to hold the eyelids apart Trauma Eye Injuries • r eassure the casualty • assist the casualty to rest in the most comfortable position. • lightly pad the injured eye. Chemical Burn to Eye •c all an ambulance 000 • fl ush with cold water for 20 minutes • lightly pad the affected eye. 61 Tooth Injuries A permanent tooth can often be saved if prompt action is taken and the tooth is handled carefully. A permanent tooth has the best chance of survival if replaced within 30 minutes. Treatment If a casualty loses a tooth the First Aider should do the following: •h old the tooth by the crown (the top) not the root 62 • r inse the tooth immediately •d o not scrub the tooth • t he best place to preserve the tooth is back in the socket • r eplace it gently then have the casualty bite down on a gauze pad to keep it in place • if replacing the tooth is not possible, place the tooth in milk • s ee a dentist immediately. The spinal cord, along with the brain, makes up the central nervous system. It is vital to be very cautious when handling a casualty you suspect has a spinal injury in order to avoid cord damage. The spine is made up of the vertebrae, the spinal cord, the intervertebral discs and the tendons, muscles and ligaments that hold all of this together. When the spine is injured, vertebrae may fracture or a disc may rupture and the spinal cord can be severely damaged. Sometimes, however, the cord is uninjured. Therefore, how you manage the casualty is very important. Signs and Symptoms •h istory of trauma (e.g., diving, fall) Trauma Spinal Injuries •u nnatural positioning of the body •c omplaint of tingling in fingers •n o feeling in limbs •u nable to move arms and or legs. ©4-Life 63 Treatment other life-threatening injury • DRSABCD • t reat the casualty for shock •c all an ambulance 000 •m aintain the casualty’s head in alignment with his/her shoulders •p erform examination of the casualty with extreme caution • r estrict any movement of the casualty to a minimum to avoid further injury • t reat haemorrhage or any • if the casualty requires to be placed in the recovery position, obtain help and do so with the Log Roll Technique as pictured. Log Roll Helmet Removal Leaving the helmet in place keeps the neck from bending back too far. Helmets also fit snugly and cradle the head, minimising head and neck motion. Thus, if an injured casualty is breathing and does not require airway management, the helmet should be left on to help support the head and neck. 64 However, if a casualty requires airway intervention, immediately remove the helmet. In most situations, the First Aider should not remove the helmet unless they cannot establish an airway which allows for effective breathing or unless the helmet is not adequately stabilising the casualty’s head. Injuries to the chest can range from mild (with minimal discomfort) to life-threatening. Major injuries to the chest may lead to collapse of breathing or circulation due to damage to the heart or lungs. The First Aider must be aware for the signs of shock. Penetrating Chest Wound A chest injury may involve the ribs and/or lungs. • t here is a stick or other foreign object protruding from the chest area. Signs and Symptoms • pale, cool, clammy skin • rapid weak pulse • rapid shallow breathing A penetrating chest wound can be rapidly life-threatening. A First Aider should suspect a penetrating chest wound if: Trauma Chest Injuries • t here is a wound on the chest and the casualty is in respiratory distress Do not remove foreign object protruding from chest wall. If the object is too large to move the casualty, call for emergency help. Do not cut the object yourself. • increased pain • pain on touching affected area Signs and Symptoms •g uarding of the affected area •p ale, cool, clammy skin • bruising, swelling. • r apid weak pulse • r apid shallow breathing Treatment •p ain at site of injury • DRSABCD • v isible open chest wound •c all an ambulance 000 • v isible object still in place. •w atch closely for breathing difficulties •g ive oxygen if available. 65 Treatment • DRSABCD •c all an ambulance 000 • if foreign object still in place, support object with padding around wound and tape in position • if the chest wound is open, apply a non-adherent dressing to site. Tape on 3 sides only to allow for air or fluid to escape •p lace casualty in a position of comfort •w atch closely for breathing difficulties. 66 Injuries to the abdomen can damage the internal organs such as the liver, spleen, kidneys or intestinal tract. The majority of abdominal injuries are caused by blunt trauma through motor vehicle accidents. Penetrating trauma is caused by such events as stab wounds or gunshot. Bleeding can be profuse and life-threatening. The First Aider must be aware for the signs of shock. Signs and Symptoms •p ale, cool, clammy skin • r apid weak pulse • r apid shallow breathing •p ain on touching abdominal area •g uarding of the abdomen • r igid abdominal area • v omiting of blood •b ruising, swelling. Treatment • DRSABCD Trauma Abdominal Injuries •c all an ambulance 000 •g ive nothing to drink or eat • if the object is embedded, do not remove but stabilise by applying padding • if possible, and if the casualty is conscious, carefully place the casualty onto his/her back • r aise the casualty’s legs to help with shock process If abdominal contents are on view this is known as evisceration. If you suspect evisceration: •d o not attempt to place abdominal contents back into abdominal cavity •a pply a non-stick dressing (or, if unavailable, a moist pad or plastic wrap) over the casualty’s organs • t he non-stick dressing may then be covered by a loose bandage. 67 Crush Injuries A crush injury is caused by a substantial weight on top of a casualty. This may lead to a life-threatening situation. Signs and Symptoms A casualty suffering a crush injury may display the following range of signs and symptoms: • large area of the casualty’s body is involved •n o detectable pulse in limb below crush injury •p ale, cool, clammy skin • r apid, weak pulse. 68 Treatment For the treatment of a crush injury do the following: • DRSABCD •c all an ambulance 000 • r eassure the casualty •a ll crushing forces should be removed as soon as possible • t reat any other injuries •k eep the casualty warm. A fracture is any break in the continuity of a bone. Fractures can cause total disability or in some cases death due to the severing of vital organs and/ or arteries. First Aid includes immobilising the fractured part in addition to applying lifesaving measures when necessary. The basic splinting principle is to immobilise the joints above and below the fracture. Fracture Classification: Signs and Symptoms • deformity Trauma Fractures • tenderness • swelling • pain • inability to move the injured part • haemorrhage •b ruising of skin at the injury site • crepitus (a grating noise made when the ends of fractured bones rub together). •A closed fracture is a broken bone that does not break the overlying skin. The tissue beneath the skin may be damaged. •A n open fracture is a broken bone that breaks (pierces) the overlying skin. The broken bone may come through the skin. •A complicated fracture involves damage to internal organs or blood vessels that are located in the vicinity of the fracture. ©4-Life Treatment Fractures often occur along with other injuries. Assess which injury takes priority. For example, heavy bleeding is more urgent – and requires higher priority care – than a fracture. 69 Purposes of Immobilising Fractures Immobilise the fracture area on both sides of the fracture site (above and below) by using splints wherever available. A fracture is immobilised to prevent the sharp edges of the bone from moving and cutting tissue, muscle, blood vessels, and nerves. This reduces pain and helps prevent or control shock. In a closed fracture, immobilisation keeps bone fragments from causing an open wound, which can become contaminated and lead to a risk of infection. Fracture Management (forearm, upper arm, leg) • DRSABCD •c all an ambulance 000 • r eassure the casualty •c heck for a pulse at the base of limb • if pulse not present, you may need to apply gentle traction to assist with return of circulation • t reat any wounds •a pply an appropriate splint. Fractured Pelvis • DRSABCD •c all an ambulance 000 • r eassure the casualty •b end casualty’s legs at knees, gently bring them together and support with bandages •p lace folded blanket either side of the casualty’s hips for support. Fractured Jaw • DRSABCD •c all an ambulance 000 • r eassure the casualty • s upport jaw with pad • lean the casualty forward to help with drainage of fluid from mouth • if the casualty is unconscious, place in the recovery position. Splints Splints may be improvised from such items as boards, poles, sticks, newspaper, or cardboard. 70 A sling is a bandage suspended from the neck to support an upper extremity. The triangular bandage is ideal for this purpose. The casualty’s hand should be higher than his/her elbow, and the fingers should be showing at all times. The sling should be applied so that the sling is tied on the unaffected side. Triangular Bandage Sling To apply this type of sling: • insert the triangular bandage under the injured arm so the arm is in the centre, the apex of the sling is beyond the elbow, and the top corner of the material is over the shoulder of the injured side •p osition the forearm with the hand slightly raised Trauma Slings • bring the lower portion of the triangular bandage over the injured arm and over the shoulder of the uninjured side • t ie the two corners in a nonslip knot on the side of the neck on the uninjured side • t wist the apex of the sling and tuck it in at the elbow. Collar and Cuff This sling can be used for a fractured upper arm: • t he elbow on the injured side must hang naturally at the side of the casualty • t he hand on the injured side must be extended towards the shoulder on the noninjured side • t he triangular bandage is used as a clove hitch: form two loops, one towards you, one away from you •p lace the loops together by folding both towards each other 71 •g ently place the clove hitch over the hand and pull firmly to secure on the casualty’s wrist •p lace ends of bandage on either side of neck • t ie off on the unaffected side • t he casualty’s arm should hang comfortably • if further support is required, place another triangular bandage around the upper arm and body to maintain support of arm against body of casualty • t his will help restrict movement. 72 Muscles, tendons and ligaments all surround bones and joints and are known as soft tissues. Tendons attach muscle to the bone and cross over at the joint. Ligaments join bone to bone at the joint. Dislocation can also be included in soft tissue injuries. Causes Many soft tissue injuries are related to sporting accidents and may be caused by the following: •o verstretching of a ligament at the joint, causing a sprain •p artial tearing of a muscle or tendon, causing a strain •c omplete tearing of a muscle or tendon, causing a rupture •d eep bruising, causing a large amount of bleeding into the muscle. Signs and Symptoms •b ruising and swelling at or near the injury •d ifficulty or reluctance in moving the affected part Treatment The treatment for soft tissue injury is R.I.C.E: Trauma Soft Tissue Injuries REST to reduce the pain r cold compress to ICE o affected area COMPRESSION compression bandage for support ELEVATE the injury to reduce swelling. Rest: ensure that the casualty is in a comfortable position. This will also include resting and carefully steadying and supporting the injured body part. Ice: cool the area with a cold compress (e.g. an ice pack wrapped in a cloth). Cool for 10 minutes every 2 hours. This treatment should be continued for up to 24 hours after the injury. Compression: apply a compression bandage to the affected area. This will provide gentle and even support to the injury. •p ain and tenderness at or near the injury. 73 Elevation: gently raise and support the injury in order to reduce bleeding and therefore reduce swelling and pain. 74 If pain is severe or the casualty cannot use the injured part, further medical assessment can determine if a fracture is present. Medical MEDICAL 75 Syncope (Fainting) Syncope (fainting) is defined as sudden loss of consciousness due to a decline in blood flow to the brain. Syncope usually lasts for less than one minute and the person makes a full recovery. • s udden stress • s evere pain •p rolonged standing •q uickly standing upright, especially after bed rest. Treatment Signs and Symptoms Signs of syncope can include the following: • t he person may complain of feeling light-headed and/or nausea • t he person’s heart rate slows • t he person’s skin is clammy and pale in colour. Causes Syncope may be caused by lack of blood supply to the brain due to the following: 76 •a ssist the person to lie down flat •e levate the person’s legs by placing on a chair •e ncourage the person to take deep breaths. If the person remains unconscious: • DRSABCD •c all an ambulance 000. If a person complains of feeling faint, then assist him/her to sit or lie down immediately to prevent syncope. Anaphylaxis is an immediate and rapid response following exposure to an irritant that a casualty is sensitive to. It is the most severe form of allergic reaction. If not treated immediately, it has the potential to be life-threatening. Signs and Symptoms A casualty suffering from anaphylaxis may demonstrate signs and symptoms within minutes of exposure to the allergen. Such signs and symptoms could include: • t he casualty may complain of a lump in the throat • wheezing • t ightness of the chest Causes Common causes of anaphylaxis may include everyday stimuli such as: •d rug reactions • f ood reactions • insect stings. Treatment If the casualty is conscious and able to respond to verbal commands, the following treatment should be instigated: • r eassure the casualty and remain calm •h elp the casualty to sit upright to help casualty’s breathing • t he forming of a rash over most of the casualty’s body • if the casualty cannot sit upright then assist him/her to lie down •g eneralised swelling •c all an ambulance 000 • hives • if the casualty is prescribed medication (EpiPen®) assist with administration. Administration technique is described on the EpiPen®. • increased heart rate • t he casualty could collapse and/or become unconscious. Medical Anaphylaxis Death may occur within minutes due to respiratory failure. 77 If the casualty is unconscious: • DRSABCD •c all an ambulance 000 • if the casualty is not breathing normally, start CPR. The casualty who is known to have a severe allergy may have an EpiPen® prescribed by his or her doctor. An EpiPen® is a pre-loaded dose of adrenaline that can be injected into the casualty. Adrenaline can help reverse the effects of anaphylaxis. 78 EpiPen® use People with Asthma have extra sensitive airways. The airways react by narrowing when they become irritated. This makes it difficult for air to move in and out. The narrowing or obstruction is caused by: Causes •a irway inflammation, meaning that the airways in the lungs become swollen and narrow • strong fumes • bronchoconstriction, meaning that the muscles that encircle the airways tighten or go into spasm. • inhaled irritants Signs and Symptoms Asthma attacks can range from mild to very severe and how a person’s symptoms appear will depend on how severe the attack is. An attack can be recognised by some or all of the following: • wheezing • coughing • distress • difficulty with speaking • s hortness of breath or difficulty breathing Common causes of broncho­ constriction can include everyday stimuli such as: Medical Asthma • cold air • dust • exercise • smoke • pollen • animals • house dust mite. Treatment If the casualty has an Asthma Action Plan, this plan should be followed. If the person is conscious and able to respond to verbal commands the following treatment should be initiated: • r eassure the person and remain calm • help the person to sit upright • skin is pale/blue in colour. 79 •g ive 4 separate puffs of a blue/grey reliever, one puff at a time •e ncourage the person to breathe in 4 times after each puff • if there is no improvement after 4 minutes, call an ambulance 000 •c ontinue to give 4 separate puffs with 4 breaths in between •w ait 4 minutes between each set of 4 If the person is unconscious: • DRSABCD •c all an ambulance 000 • if the person is in cardiac arrest, start CPR. A person with severe Asthma is exhausted through the fight to breathe and can appear quite calm. This is often a dangerous stage. Even if medication appears to be effective, medical advice should be sought. Call an ambulance 000. •c ontinue until ambulance arrives • if available, use a spacer. Asthmatic using inhaler with spacer device 80 Hyperventilation means breathing faster than normal. Both adults and children can find hyperventilation very frightening. Always remember there are many people who hyperventilate – this may be due to a serious illness and must be treated as such. Anxiety Related Hyperventilation Medical Hyperventilation Causes Hyperventilation is likely to occur due to the following: • anxiety • fear • emotional stress. Signs and Symptoms A person suffering from hyperventilation may display signs and symptoms as follows: • r apid breathing/shortness of breath • rapid heart rate • anxiety • visual disturbance Treatment The best way to prevent Hyperventilation is to avoid situations and activities that may cause anxiety but if an attack occurs the following treatment should be initiated: • r eassure the person and remain calm • tingling in fingers • r emove the person from the cause if possible • s ometimes loss of consciousness. •e ncourage the person to slow their breathing The symptoms usually last 20-30 minutes but it may seem like hours to the person. Although frightening, hyperventilation is not usually dangerous. •d o not use a bag for the person to breathe into • if the person shows no improvement call an ambulance 000. 81 Stroke Stroke occurs when the arteries that lead to the brain become either blocked or ruptured. When this happens the brain does not receive the oxygen that is required and so brain cell death occurs. THINK FAST! Facial weakness Arm weakness Speech difficulty Time to act fast Causes Signs and Symptoms A person suffering from a stroke may show signs and symptoms as follows: • t otal or partial weakness on one side of the body • inability to talk • inability to understand or remember certain things • t rouble swallowing • pain • numbness •p roblems with sight. The two most common causes of stroke are as follows: • a blood clot forms and blocks blood flow in an artery leading to the brain • a cerebral haemorrhage occurs when a defective artery in the brain bursts. Treatment If the person is conscious and able to respond to verbal commands, the following treatment should be initiated: • r eassure the person and remain calm • loosen tight clothing •p rotect the person’s airway and place the person on his/ her non-paralysed side •k eep the person warm ©4-Life 82 •c all an ambulance 000. • DRSABCD •c all an ambulance 000 • if the person is non-breathing, start CPR • if the person is in cardiac arrest, start CPR. While a person suffering from a Stroke may not be able to communicate he/she may be able to understand what is going on about them. Therefore, it is important to explain all procedures and to offer constant reassurance to the casualty. Medical If the person is unconscious: Choking Choking in a conscious casualty may occur when the upper airway, usually the throat or trachea, is blocked by an object. The blockage may be partial or complete. When the airway is blocked the casualty is deprived of oxygen. Rapid First Aid for choking can save a life. Signs and Symptoms The casualty suffering from partial obstruction may display signs and symptoms as follows: • s hortness of breath •b lue/pale/cold skin The casualty suffering from Complete Obstruction may display signs and symptoms as follows: •u nable to breathe, cough and/or speak •c lutching the throat or chest • f ace and extremities turning blue. Causes Choking is more likely to occur due to the following: • s wallowing large, poorlychewed food • wheezing •c onsumption of large amounts of alcohol • coughing •w earing poor-fitting dentures •n oisy breathing. • t alking or laughing while eating. 83 Treatment (Adult, Child) Ineffective Cough If the casualty is conscious and able to respond to verbal commands and can also cough effectively, the following treatment should be initiated: •g ive up to 5 back blows between the shoulder blades using the heel of your hand. Effective Cough • r eassure the casualty and remain calm •c all an ambulance 000 •h elp the casualty to sit upright and encourage coughing •m aintain continuous checking of casualty until recovery or deterioration (deterioration is recognised if the casualty turns blue or becomes limp). If the casualty is conscious but has an ineffective cough, the following treatment should be instigated: If back blows unsuccessful: •g ive up to 5 chest thrusts. Chest Thrusts Chest thrusts are similar to chest compressions in CPR but sharper and delivered at a slower rate: •p lace dominant hand in centre of the chest, place other hand on top and interlock fingers of both hands •p ush down approximately 1/3 depth of the chest, up to 5 times. Unconscious casualty •c all an ambulance 000 •c ommence CPR •C PR refer page 36. 84 Ineffective Cough Effective Cough •p lace infant in downward position across your knees with head lower • r eassure the casualty and remain calm •c all an ambulance 000 •h elp the casualty to sit upright and encourage coughing •m aintain continuous checking of casualty until recovery or deterioration (deterioration is recognised if the casualty turns blue or becomes limp). Medical Treatment (Infant) •g ive up to 5 back blows between the shoulder blades using the heel of your hand. If back blows unsuccessful: •g ive up to 5 chest thrusts. Chest Thrusts •p lace 2 fingers in centre of the chest •p ush down approximately 1/3 depth of the chest, up to 5 times (Chest thrust similar to chest compressions in CPR but sharper and delivered at a slower rate) Unconscious casualty •c all an ambulance 000 •c ommence CPR. • CPR refer page 36. 85 Febrile Convulsion Febrile Convulsion can affect infants and children less than 5 years of age and is caused by a high temperature (above 38.5 Celsius). The condition is generally not life-threatening. Signs and Symptoms A child suffering from febrile convulsion may display the following signs and symptoms: •p ossible high temperature •c old-like symptoms •e yes roll back • t he child may first become unconscious, followed by a stiffening of the legs, arms and body • t he head is flung backwards and the arms and legs commence jerking • t he child’s skin colour may become pale or even turn blue • t he convulsion ends after a few minutes and normal colour and conscious state returns. 86 Causes Common causes of febrile convulsion include the following: • t he child is genetically predisposed to the condition • t he child suffers frequent illness, which includes high temperature. Treatment The following treatment should be initiated: •p osition the child on his/her side • r emove the child’s clothing •d o not place the child in cold water •d o not over-cool the child •c all an ambulance 000. A child who has suffered a febrile convulsion must be transported by ambulance to hospital to determine the cause of the convulsion. Diabetes is a disorder of the body’s ability to use glucose (sugar), the body’s main source of energy. Two conditions suffered by a diabetic which may be encountered by a First Aider are hypoglycaemia (low blood sugar) and hyperglycaemia (High blood sugar) Treatment The following treatment should be initiated: •c all an ambulance 000 • if the person remains conscious and able to swallow give a sweet drink (remember not diet drink). Alternatively, administer 8-10 jelly beans to the casualty Hypoglycaemia • r epeat the treatment if the person responds Hypoglycaemia is also called low blood sugar. This condition occurs when a person’s blood sugar level drops too low to provide enough energy for the body’s activities. •w hen the person recovers and is able to swallow, help with the administration of food such as a biscuit, piece of fruit or sandwich. Signs and Symptoms A person suffering from hypoglycaemia may display signs and symptoms as follows: • hunger • sweating • dizziness • drowsiness • confusion • difficulty speaking. Medical Diabetes If the person is unconscious, place them into the recovery position and call an ambulance to provide additional treatment. Do not administer insulin to a person suffering from a hypoglycaemic attack. ©4-Life 87 Hyperglycaemia Treatment Hyperglycaemia is an increase in glucose (sugar) circulating in the blood. The following treatment should be initiated: Signs and Symptoms Hyperglycaemia has a slower onset compared to hypoglycaemia and is also less common. Signs and symptoms include: • excess urine production • increased thirst • increase in hunger • hot dry skin • t he person may experience visual disturbance • tiredness • t he person may become unconscious. •h igh blood sugar reading on glucometer. 88 • call an ambulance 000 • if the person is unconscious, place him/her into the recovery position. Never place anything in an unconscious person’s mouth •o ffer reassurance, even to an unconscious casualty. A seizure is a sudden change or disturbance in the way the cells of the brain function caused by chaotic electrical signals. Signs and Symptoms The signs and symptoms may present in different ways depending on the severity. • blank staring • chewing • wandering • confused speech. If the seizure is severe, signs and symptoms may include: • collapse Treatment The following treatment should be initiated: Medical Seizure (Fitting) •c ushion the person’s head and remove eye glasses •c all an ambulance 000 • loosen tight clothing •p rotect person from harm • do not restrain •d o not place anything in the person’s mouth •o nce the seizure activity has finished, place the person on his/her side •w hen the person gains consciousness, reassure him/her. • loss of consciousness •u ncontrolled jerky movements of the person’s arms/legs/body. 89 Heart Conditions The heart is a muscle that is located a little to the left of the middle of the chest, and generally it is about the size of your fist. The heart is like a pump and it sends blood around the body. The blood Chest Pain Chest pain is usually a sign of lack of oxygen to the heart muscle. •c all an ambulance 000 to provide emergency care. 90 provides the body with the oxygen and nutrients it needs. The heart is a pump that should beat regularly. Certain heart conditions can create an irregular pulse. Heart Attack and angina can present in a very similar way and it can be difficult to determine between the two. Signs and Symptoms •c hest pain or discomfort •p ain or heaviness in the arms, shoulders, throat and/or jaw • sweating • breathlessness • collapse. If the person is unconscious: • DRSABCD Medical Angina and Heart Attack •c all an ambulance 000 • if the person is in cardiac arrest, start CPR. A person who has been diagnosed with angina may also be prescribed a medication by their doctor. This medication is taken as a spray or tablet beneath the tongue. If the person has this medication it must be administered by the person not by the First Aider. Treatment If the person is conscious and able to respond to verbal commands the following treatment should be initiated: • DRSABCD •c all an ambulance 000 • r eassure the person and remain calm • loosen tight clothing • r estrict activity and ensure that the person rests. 91 Poisoning Poisoning can be defined as substances entering the body either through inhalation, absorption, injection, or skin contact which cause injury, illness or death. Causes Causes of poisoning can include the following: • inhalation of substance • absorption • injection of substance Signs and Symptoms • s kin contact. Look for these signs and symptoms if you suspect poisoning: Treatment •b urns or redness around the mouth and lips, which can result from drinking certain poisons • breath that smells like chemicals, such as petrol, insecticide or other chemicals • burns, stains and odours on the casualty or his/her surrounds • vomiting Swallowed Poisons Note that some poisons may not cause immediate symptoms in a casualty. In some instances, it may be several hours before symptoms show. However, damage may still be occurring during this time. If you suspect a casualty has swallowed poison you should do the following: •d ifficulty breathing • t ake the container with you to the telephone •a ltered conscious state/ confusion. •C ALL POISON INFORMATION CENTRE 13 11 26 •c all an ambulance 000 •D O NOT make the patient vomit. 92 Poison Safety If a casualty has absorbed poison through the skin: Remember the following key points relating to poison safety in the home and workplace: • t horoughly flush the area immediately with copious amounts of water •C ALL POISON INFORMATION CENTRE 13 11 26 •c all an ambulance 000 •c ontinue to flush with running water until ambulance personnel arrive •e nsure no-one else on scene is affected. Inhaled Poisons If inhalation of poison is a possibility, the First Aider should suspect an inhalation injury even if there are no apparent signs and symptoms. In such an instance: •m ove the casualty to fresh air quickly without putting yourself in danger • if safe to do so, open windows and doors wide •C ALL POISON INFORMATION CENTRE 13 11 26 •c all an ambulance 000. Medical Absorbed Poisons •k eep medicines and chemicals out of sight and out of reach in a locked or child-resistant cupboard •d o not leave chemicals unattended whilst in use • r ead directions for use carefully •d o not decant chemicals •a lways purchase household products with child-resistant packaging •a void taking medication in front of small children. POISON INFORMATION CENTRE 13 11 26 24 HOURS A DAY ANYWHERE IN AUSTRALIA 93 Drug Overdose A drug is usually a substance used to treat an illness, relieve a symptom or prevent disease in the body. It comes in many forms such as capsules, tablets, powders, liquids, aerosols and pastes. A doctor’s prescription is generally required for the purchase of most drugs. However, the use of illegal drugs in our communities is very common and can lead to major health problems or even death. Prescription and Non-Prescription Drugs Prescription drugs require a doctor’s prescription to be written prior to purchase. Less dangerous non-prescription drugs can be purchased over the counter from pharmacists or supermarkets. Natural and Synthetic Drugs A natural drug is made from a plant or animal. Most medicines prescribed by a doctor are synthetic as they are made from chemicals. 94 Legal and Illegal Drugs Legal drugs, whether prescription or nonprescription, can be bought in pharmacies and shops. Illegal drugs are those that are imported, grown or manufactured illegally. Often, illegal drugs are dangerous and cause the user to become addicted. Some examples of illegal drugs include cocaine, heroin, ecstasy and marijuana. Overdose A drug overdose occurs when you consume more drugs than your body can tolerate. Drugs affect how the body works. When taken incorrectly or as an overdose they may be very toxic to the body and cause serious injury or death. Care and Treatment A drug overdose may be a life-threatening situation depending on the type of drug and the amount taken. If a person is suffering from a drug overdose you should do the following: A person suffering from a drug overdose may display the following signs and symptoms: •a ltered level of conscious state • unconsciousness Medical Signs and Symptoms • DRSABCD • call an ambulance 000 • if unconscious place in recovery position • if the casualty is in cardiac arrest, start CPR. • blurred vision • slurring of speech • pinpoint pupils • slow shallow respiration POISON INFORMATION CENTRE • s low pulse or, alternatively, rapid weak pulse 13 11 26 •e vidence of needle injection marks 24 HOURS A DAY • respiratory arrest • cardiac arrest •e mpty medication containers/packets. ANYWHERE IN AUSTRALIA 95 Heat Exhaustion Heat Exhaustion is a common condition seen by First Aiders and occurs when people exercise (work or play) in a hot, humid place and their body fluids are lost through sweating, causing the body to overheat. Signs and Symptoms The following are the most common symptoms of heat exhaustion although each individual may experience symptoms differently: • profuse sweating • pale skin • t he person may feel faint or may collapse • nausea • t he person complains of a headache. 96 Treatment For the treatment of heat exhaustion, initiate the following care: •c all an ambulance 000 • r eassure the casualty and remain calm • r elocate the casualty to a cool place • r emove enough clothing to cool the casualty without chilling him/her • lightly fan the casualty’s skin •a pply/wrap ice packs to casualty’s groin and armpits •a dminister oral fluids (water), small frequent amounts. Heatstroke is a life-threatening condition. It is due to the body’s elevated temperature. Heatstroke can be caused by many different situations such as: Treatment •e xcessive exercise and excessive heat. •c all an ambulance 000 Signs and Symptoms • r elocate the casualty to a cool place The following are the most common symptoms of heatstroke although each individual may experience symptoms differently: • headache • dizziness •d isorientation, agitation or confusion •h ot dry skin that is flushed but not sweaty • high body temperature • altered conscious state • rapid shallow breathing • increased pulse rate and breathing. For the treatment of heatstroke implement the following care: Medical Heatstroke • DRSABCD • r eassure the casualty and remain calm • r emove enough clothing to cool the casualty • lightly fan the casualty’s skin •a pply/wrap ice packs to casualty’s groin and armpits •g radually cool the body with tepid sponging or wet cloths. If the casualty is unconscious: • DRSABCD •c all an ambulance 000 •p lace the casualty on his/her side • if the casualty is in cardiac arrest, start CPR. 97 Hypothermia Hypothermia is a condition in which the person’s core body temperature has dropped to significantly below normal (35 degrees Celsius). Causes The main causes of hypo­ thermia are: • immersion in cold water •e xposure to a cold environment. Signs and Symptoms The following are the most common symptoms of hypothermia although each individual may experience symptoms differently: • shivering • confusion •c hange in conscious state/ unconsciousness •d ry cold skin. 98 Treatment For the treatment of Hypothermia initiate the following care: • DRSABCD •c all an ambulance 000 •h andle the casualty gently and remove him/her from cold environment • if clothing is wet, carefully remove. If casualty is conscious and shivering: • r e-warm the casualty slowly (e.g., wrap in warm blankets or clothing) • t reat for shock. If the casualty is unconscious: • DRSABCD •c all an ambulance 000 •p lace the casualty on his/her side • if the casualty is in cardiac arrest, start CPR. Medical CAUTION •d o not rub or massage the casualty •d o not give alcohol •d o not use hot water bottles or place the casualty in hot water. Mild hypothermia casualty conscious and shivering 99 Drowning Drowning is second only to motor vehicle accidents as a cause of accidental death in Australia. Signs and Symptoms The casualty who has been rescued may display: • s hortness of breath • DRSABCD •c all an ambulance 000 •d ue to drowning, a large amount of water may be in the mouth. This can be drained by turning the casualty on to their side •b lue/pale/cold skin • if the casualty shows no signs of life, start CPR • unconsciousness •C PR refer to page 36. • non-breathing. Treatment If the casualty is conscious and able to respond to verbal commands the following treatment should be initiated: • r eassure the casualty and remain calm • help the casualty to sit upright and take regular deep breaths •c all an ambulance 000 • if the casualty is cold, warm with blanket. 100 If the casualty is unconscious: Never cancel an ambulance even if the casualty appears to have made a full recovery. It is imperative that the casualty is seen at a hospital as his/her condition may deteriorate. Bites and Stings BITES AND STINGS – ENVENOMATION 101 Snakes Approximately 70% of Australian snakes are venomous. Venom can be a lethal substance and may cause a diverse array of reactions in a casualty. Not everyone that is bitten by a snake is poisoned. Treatment •w here possible, apply an immobilisation splint. (Do not remove once in place) •d o not wash the bite site as this may be used for venom detection The main goal of treatment is to restrict the transport of venom through the body: •d o not apply a tourniquet or constrictive bandage. •c all an ambulance 000 Pressure Immobilisation Bandage Technique •m ake a thorough physical assessment and, where possible, identify the snake •o ffer the casualty reassurance and try to relax him/her both physically and psychologically •a pply a firm pressure immobilisation bandage technique (see below) to the affected area/limb Anyone suspected of being bitten should be treated. 102 • apply a second roller bandage, starting at the toes or fingers and continuing up the limb Apply a wide bandage over the bite site. This bandage should be firm but still allow blood flow to the limb. If the casualty is unconscious: • DRSABCD •c all an ambulance 000 • if the casualty is in cardiac arrest, start CPR. Red-Back The venom takes a long period of time to act, causing complications up to three hours later. The venom is rarely life-threatening in adults. ©4-Life Bites and Stings Spiders Signs and Symptoms A casualty suffering from a red-back spider bite may display the following signs and symptoms: • immediate pain at the bite site, and pain to increase with time • s kin may appear red •p rofuse sweating at the bite site • s kin may be hot to touch at the bite site • local swelling at bite site • nausea/vomiting •a bdominal pain Treatment Treatment should proceed as follows: •o ffer the casualty reassurance and try to relax him/her both physically and psychologically •m ake a thorough physical assessment •a pply ice to the bite site and elevate. (Do not apply a pressure bandage as this will increase the pain) •u ndertake constant assessment of the casualty •c all an ambulance 000. •b lurred vision. 103 Funnel Web Treatment The funnel web is more commonly found in the eastern states and a person is more likely to be bitten at night. Deaths are rare due to availability of appropriate treatment. The main goal of treatment is to restrict the transport of venom through the body. The male is highly aggressive when disturbed or cornered and is able to inflict multiple strikes with its hardened fangs. Signs and Symptoms A casualty suffering from a funnel web spider bite may display the following signs and symptoms: •p rofuse sweating and salivation from the mouth • s kin may be cold and the casualty may shiver • local swelling at bite site • nausea/vomiting •a bdominal pain •b lurred vision. • DRSABCD •c all an ambulance 000 •m ake a thorough physical assessment • offer the casualty reassurance and try to relax him/her both physically and psychologically •a pply a firm pressure immobilisation bandage technique to the affected area/limb (Refer to page 102) • apply a second roller bandage, starting at the toes or fingers and continuing up the limb •w here possible, apply an immobilisation splint. (Do not remove once in place) •d o not wash the bite site as this may be used for venom identification •d o not apply a tourniquet or constrictive bandage. Anyone suspected of being bitten should be treated. 104 Bee, wasp and ant stings are painful but are generally not life threatening unless the casualty is allergic. (Refer to anaphylaxis page 77). Treatment The main goal of treatment depends on the presentation of symptoms: • DRSABCD •c all an ambulance 000 Bites and Stings Bee, Wasp and Ant Stings •m ake a thorough physical assessment •o ffer the casualty reassurance and try to relax him/her both physically and psychologically ©4-Life Signs and Symptoms A casualty suffering from an insect sting or bite may experience: • itchy skin • rash • swelling of the area • nausea/vomiting •a ltered state of consciousness/collapse • s hortness of breath. • r emove the sting by scraping but do not squeeze the sting as this will release more venom •a pply an ice pack or cold compress to the site for relief of pain • if the casualty has an allergic reaction, call an ambulance 000 and apply pressure immobilisation bandage technique (Refer to page 102). If the casualty is unconscious: • DRSABCD •c all an ambulance 000 • if the casualty is in cardiac arrest, start CPR. 105 Marine Creatures Blue-Ringed Octopus Treatment The blue-ringed octopus is a common octopus species which can be found in crevices and under rocks at the seashore. It can be found in most states of Australia. The Blue Ringed Octopus is not normally aggressive and attacks only if provoked. It is the most venomous octopus in the world. The main goal of treatment is to restrict the transport of venom through the body: Although bites are infrequent they are known to be harmful due to the effect on breathing. Signs and Symptoms A casualty suffering from a blue-ringed octopus sting may present the following symptoms: •p ainless bite site with a visible spot of blood •n umbness in the lips, tongue, face and neck within minutes •c all an ambulance 000 •m ake a thorough physical assessment •o ffer the casualty reassurance and try to relax him/her both physically and psychologically •a pply a firm pressure immobilisation bandage technique to the affected area/limb (Refer to page 102) •w here possible, apply an immobilisation splint. (Do not remove once in place) •d o not wash the site as this may be used for venom identification •d o not apply a tourniquet or constrictive bandage If the casualty is unconscious: • v isual disturbances • DRSABCD •d ifficulty speaking •c all an ambulance 000 •g eneralised weakness • if the casualty is in cardiac arrest, start CPR. • t he casualty may collapse requiring resuscitation. 106 • DRSABCD Treatment The cone-shell has venom glands and can inject venom when handled or stepped on. The venom can cause progressive muscle weakness that can lead to sudden death. The main goal of treatment is to restrict the transport of venom through the body: Although bites are infrequent they are known to be harmful due to the effects on breathing. •m ake a thorough physical assessment Signs and Symptoms •p ainless bite site with a visible spot of blood •n umbness in the lips, tongue, face and neck within minutes. • v isual disturbances •d ifficulty speaking •g eneralised weakness •p aralysis of respiratory muscles leading to difficult breathing • r espiratory arrest • t he casualty may collapse requiring resuscitation. • DRSABCD •c all an ambulance 000 Bites and Stings Cone-Shell • offer the casualty reassurance and try to relax him/her both physically and psychologically •a pply a firm pressure immobilisation bandage technique to the affected area/limb (Refer to page 102) •w here possible, apply an immobilisation splint. (Do not remove once in place) •d o not wash the site as this may be used for venom identification •d o not apply a tourniquet or constrictive bandage. If the casualty is unconscious: • DRSABCD •c all an ambulance 000 • if the casualty is in cardiac arrest, start CPR. 107 Box Jellyfish Treatment Box jellyfish are pale blue and transparent. They are cubeshaped with four distinct sides, hence their name. The main goal of treatment is to restrict the transport of venom through the body: They are usually found in tropical regions. Signs and Symptoms A casualty suffering a sting from a box jellyfish may display the following symptoms: • s evere pain of the affected area •b listering and red marking on skin • altered state of consciousness • DRSABCD •c all an ambulance 000 •m ake a thorough physical assessment •o ffer the casualty reassurance and try to relax him/her both physically and psychologically • r emove any tentacles from the patient. This can be done by washing the area with large amounts of vinegar (first wash then try to remove) • s hortness of breath •a pply cold packs or wrapped ice to relieve pain. • r espiratory arrest If the casualty is unconscious: •h eart irregularities. • DRSABCD •c all an ambulance 000 • If the casualty is in cardiac arrest, start CPR. 108 Treatment Stonefish and Bullrouts have many spines that inject venom deeply under the casualty’s skin. This causes severe pain. The main goal of treatment is to restrict the transport of venom through the body: Signs and Symptoms •o ffer the casualty reassurance and try to relax him/her both physically and psychologically A casualty suffering from stone fish or bullrout venom may display the following signs and symptoms: • intense pain at the site of injury • s welling at the site •a n open wound may be present at the site •b arbs may still be visible • t he casualty may be very anxious •a local grey/blue discolouration and/or bleeding. •m ake a thorough physical assessment Bites and Stings Fish Stings • s ubmerge the affected area in hot water (as hot as can be tolerated by the casualty) •d o not restrict movement of the limb •c all an ambulance 000. If the casualty is unconscious: • DRSABCD •c all an ambulance 000 • if the casualty is in cardiac arrest, start CPR. 109 Tick Bite Treatment The tick is very small and may attach anywhere to the body such as hairy areas and in body crevices. It can cause paralysis and allergic reactions. Prompt removal of the tick is essential. Signs and Symptoms • local skin irritation • tiredness • muscle weakness • double vision • breathing/difficulty swallowing. 110 • r emove tick with forceps by pressing down skin around tick’s mouth part •w ith forceps, grip mouth part firmly but slowly and gently remove • avoid squeezing tick • seek medical help. Advanced First Aid ADVANCED FIRST AID 111 Triage – Prioritisation of Casualty Treatment The word triage comes from the French word trier, which means ‘to sort’. It is a system of rapidly identifying casualties who have life threatening injuries and who have the best chance of survival. This system is generally used in a mass casualty situation. Only commence a triage system when there are two or more injured people. For a single casualty, always implement First Aid. As a First Aider at a mass casualty scene you may have to choose patients who require immediate transport to the hospital to save their lives as opposed to patients who can wait for help later. This can be a very difficult and traumatic task. In most situations you will be relieved of this task by an ambulance paramedic. 112 To triage effectively you will need to be objective and consider the following: •d o not treat the deceased •g ive CPR to a casualty in cardiac arrest ONLY if there are NO other seriously injured casualties who require urgent treatment • r emove those casualties who can be helped by immediate transportation •d elay transportation of casualties whose condition will not be affected by delay • t reat casualties with minor injuries and the walkingwounded who need help less urgently last •a llocate your limited first aid assistance and resources to those who are most likely to survive. Trauma from road accidents is one of the leading causes of accidental death and serious injury in Australia, despite the develop­ments in manufacturing of motor vehicles such as air bags, crumple zones and seat belts. The First Aider is often first at the scene of an accident and may dramatically influence the outcome for the casualties involved. First Aiders need to remain calm and provide systematic assistance. If you are involved in attending a road accident, the following approach should be applied: • other road traffic • stability of the vehicle • sharp objects • potential for fire. Remember do not enter the scene unless everything is secured and safe. Advanced First Aid Road/Machine Accidents Manage the Scene A road accident scene may become chaotic. Remain calm and give good clear directions to bystanders so they can help you manage the situation. Make sure an ambulance has been called 000. Approaching the Incident – Hazards Safety is your first priority. Be aware for hazards to yourself, bystanders and the casualty, which can include: • power lines • fuel ©4-Life 113 Assess the Scene • DANGER It is important to gather relevant information about the scene and what has happened. Relay this information to Emergency Services on placing the initial phone call. Important information includes: • RESPONSE • t he number of casualties involved Treat the casualties for shock, keep them warm and reassure them about their situation. • the number of fatalities • t he number of unconscious casualties •w hether any casualties are trapped. Treatment Approach the management of the casualties requiring treat­ment as per the primary assessment (Refer to page 42). Remember that the Emergency Action Plan (DRSABCD) to be followed during the treatment and care of a casualty comprises six steps: 114 • SEND FOR HELP • AIRWAY • BREATHING • COMPRESSIONS • DEFIBRILLATION Removal of the casualties from the vehicle should only be performed if they cannot be managed due to the following: • fire (rare event) • t he First Aider is unable to manage the casualty’s airway • t he First Aider is unable to manage severe bleeding • t he First Aider needs to perform CPR. When the ambulance crew arrives give an accurate handover of what has happened, including the condition and treatment of casualties. The details you provide are very important as it will assist in the manage­ment of the casualties by ambulance personnel and later by medical staff at the hospital. A diving emergency could be any casualty who has suffered an emergency underwater regardless of depth which has affected their state of health. Scuba divers breathe air from a tank via a regulator. This ensures the correct amount of air is delivered to the diver. If a diver suffers from an emergency condition whilst diving, it is very important that medical treatment is initiated as soon as possible. The rapid ascent causes nitrogen gas to become trapped in the tissues of the body. This trapped gas may find its way into the diver’s bloodstream. Signs and Symptoms Advanced First Aid Diving Emergencies A casualty suffering from DCS may display a range of symptoms including: • fatigue •d eep pain to muscle and joints • itchy skin DECOMPRESSION SICKNESS (The Bends) •p ins and needles A serious diving emergency is decompression sickness (DCS), otherwise known as The Bends. This happens when the diver ascends too quickly to the water’s surface. •c hoking or coughing • paralysis • r apid breathing • unsteadiness/staggering when walking •c hest pain • unconsciousness. ©4-Life 115 Treatment Ruptured Lung For treatment of DCS do the following: A diver can suffer a ruptured lung. • DRSABCD •c all an ambulance 000 Treatment • call Divers 24-hour Emergency Service 1800 088 200 To treat a ruptured lung do the following: • r eassure and calm the casualty • DRSABCD • lie flat • if the casualty is in an altered conscious state or is unconscious, place in a recovery position • if oxygen therapy is available, administer 100% high flow oxygen • if the casualty is experiencing difficulty with breathing the First Aider may have to support into an upright position •k eep the casualty warm. •c all an ambulance 000 • call Divers 24-hour Emergency Service 1800 088 200 • r eassure and calm the casualty • if the casualty is in an altered conscious state or is unconscious, place in recovery position • if oxygen therapy is available, administer 100% high flow oxygen • if the casualty is experiencing difficulty with breathing the First Aider may have to support into an upright position •k eep the casualty warm. 116 Treatment The eardrum is a thin membrane that separates the inner ear from the outer ear. A Ruptured Eardrum means that it has a tear or hole in it. This may be caused by a change in pressure whilst diving. To treat a Ruptured Eardrum do the following: •p lace a clean sterile pad over the affected ear • s eek medical advice. Do not place any fluid or drops in ear unless prescribed by a doctor. Advanced First Aid Ruptured Eardrum Signs and Symptoms A casualty suffering from a ruptured ear drum may display the following symptoms: • s udden, sharp ear pain •b leeding or discharge from the ear •h earing loss • r inging in the ear • dizziness. 117 Behavioural Emergencies Abnormal behaviour may be due to many medical factors. A casualty suffering from abnormal behaviour should be approached with safety as your main priority. Treatment and Approach •c all an ambulance 000 •a ssume the same eye contact level in order to reduce the feeling of being stood-over (which may distress the person) • s peak in a non-judgmental manner in order to minimise any feelings of guilt the person may be experiencing •a llow the person time to respond to your questions. If you rush to get answers to your questions you may agitate the person and cause further distress 118 •a void sudden movements, as the person may see these as a threat •d o not touch the person without his/her permission, as the person may see this as a threat and believe that you are going to harm them •a pproach the person with caution: never place yourself in danger •n ever turn your back to the person •p osition yourself so you have the ability to exit quickly if necessary. Assessing the situation is always the main priority to ensure your personal safety and that of others. The First Aider must take precautions to avoid confrontation at all times. Remember that support and understanding of a person with an abnormal behaviour is very important. Oxygen is a colourless, odourless gas. The body requires oxygen for normal cell function and obtains it through the respiratory and circulatory systems. The atmosphere contains approximately 21% oxygen, of which 4-5% is used by the body while at rest. If the body is under stress or has a disorder of the respiratory or circulatory system, oxygen demands are increased. That demand can exceed the body’s ability to deliver adequate oxygen to the tissues. At these times, providing a supplementary external source of oxygen can be of great benefit to the casualty. Oxygen should be used in the following situations: •c ardiac and respiratory arrest • altered state of consciousness • shock • s hortness of breath, whatever the cause •c hest pain • s evere injury or trauma •b lood loss Oxygen Therapy Delivery Systems Oxygen can be delivered to a casualty by the following devices: •F ace Mask (Hudson) •N ebuliser Mask Advanced First Aid Oxygen Administration •S oft Bag and Mask Device. Face Mask (Hudson) Features of the Hudson Face Mask are: • it has a series of holes to allow air to mix with oxygen on inspiration; these holes allow exhaled air to escape and prevent the build up of carbon dioxide • t he percentage of oxygen inspired depends on flow rate, and rate and depth of the person’s respirations • t hat it is used at a flow rate of at least 8 lpm in an emergency setting. • seizures. 119 Nebuliser Mask Medical Oxygen This is the same as a face mask except that: Medical oxygen is supplied in the following ways: • it has an attachment that enables reliever medication to be administered •a luminium cylinders •o xygen and reliever medication are administered at the same time. Soft Bag and Mask The primary use of the soft bag and mask device is to ventilate non-breathing patients. This device: • should be used to deliver high concentrations of oxygen to critically ill breathing casualties. A bag valve mask on a breathing patient has a nonrebreathing valve to permit the escape of exhaled air •m ust use supplemental oxygen of at least 8 lpm • is more effective at flow rate of 14 lpm •c an deliver 80 to 95% concentration of oxygen. 120 •m etal cylinders •c arbon fibre/fibre glass wrap cylinders. Oxygen is stored at a pressure of approx 15,000 kPA or 200 PSI. Oxygen is delivered from the cylinder via a regulator which reduces the pressure to a safe working pressure of 414 kPA. The valve on medical oxygen cylinders is a yoke type with holes on the valve stem. These holes and the pins on the regulator ensure that only medical grade oxygen can be used with medical oxygen delivery devices. The pin fittings also prevent the fitting of an incorrect regulator. Cylinders are available in the following sizes (when full): •B – 200 litres •C – 400 litres •D – 1500 litres •G – 7600 litres. • inlet connections comply with national standards to prevent connection to incorrect gas cylinders • t he system is protected from dust and grit by 3 filters •c ontents gauge is fitted with a safety back to relieve pressure in event of gas leakage Storage and handling points to consider: •c ylinders should always be placed on side •h andle cylinders with care – avoid knocking or dropping • do not lift by valve or regulator •c ombustible materials such as OIL or GREASE must not come into contact with the cylinder, regulator, fittings, valves, or hoses Flow Meters •d o not seal outlets with adhesive tape, because most are petroleum-based – static spark can be generated on removal use acetate bags and rubber bands •F low meters allow for variable rates of oxygen to be delivered depending on the needs of the casualty. • s tore below temperature of 50 degrees • r egulator is also protected from delivery of excessive pressure by safety valves. Storage and Handling of Cylinders The storage of oxygen must meet the requirements of each State or Territory. Contact relevant government officials to determine the correct procedures relevant to your situation. Advanced First Aid Medical Oxygen Regulators •n ever smoke in any area where oxygen is used or stored •e nsure the cylinder is within 5 years of last test date before refilling •o xygen cylinders must be secured during transport •o nly use with correct, current checked regulator (never modify equipment) • do not use damaged cylinders – tag and send for inspection. 121 Daily Checks Oral Airway Sizing To maintain good safety standards with the use of oxygen it is important to perform daily checks with oxygen equipment. Ensure the following: To select the correct airway in an unresponsive casualty: • t he bottle is medical oxygen (black and white bottle) •p lace the airway against the side of the casualty’s face • it should extend from the corner of the mouth to the angle of the jaw. • t he bottle is clean and free of grease and oil Oral Airway Insertion • t here is no damage to oxygen bottle To insert the oral airway into an unresponsive casualty: • t he bottle is full of oxygen. •o pen the casualty’s mouth Oropharyngeal Airway • insert the oral airway with tip pointing up to avoid pushing the tongue backwards Oral airways are designed to keep the tongue from falling back and blocking the upper airway. This plastic device has a rigid flange and a hollow curved tube. Oral airways are only used in unresponsive casualties who do not have a gag reflex. The airway must be inspected prior to inserting an airway device to remove any potential obstruction. • r otate the oral airway tip slowly 180 degrees downward until the curve of the oral airway matches the curve of the tongue • t he flange of the oral airway should rest against the casualty’s lips. Oral airway insertion 122 A large percentage of the population at some point during their lives will suffer from a back injury. The spine is a very complex structure, with a delicate spinal cord protected by the vertebrae. Between the vertebrae are discs, which have a tough outer casing and a jelly-like centre. Many back problems are caused by the ligaments and muscles in the lower back becoming weakened which in turn leads to the discs becoming weakened. In certain types of back injury the outer covering of the disc can split, allowing the jelly-like contents to squeeze out. If this occurs it may lead to severe pain and a chronic debilitating injury. Another frequent cause of back injury is the lifting of heavy objects whilst not maintaining correct posture and lifting techniques. Being overweight and not exercising enough can also increase your risk of a back injury. Avoiding Back Injuries • t ake frequent small breaks and rest between lifts if you are lifting a number of objects •m ake sure you do not strain to lift. If you have to strain to carry the load, it is too heavy Advanced First Aid Back Care (Care of the Spine) •m ake sure you have enough room to lift safely. Clear a space around the object before lifting it • look around before you lift, and look around whilst you carry. Make sure you can see where you are walking. Know where you are going to put down the load •a void walking on slippery, uneven surfaces while carrying a load •g et help before you try to lift a heavy load. Use a mechanical appliance to move the load •m aintain the normal curves of the spine when standing, sitting or lifting a load (See next section). This will provide support for ligaments, joints and discs underneath. 123 Lifting or Moving a Load •u se slow and controlled movements •h urried, uncontrolled movements can strain the muscles in your back Remember the management of your back and the prevention of injury is in your hands. A chronic back injury will affect your quality of life significantly. •k eep your body facing the load whilst lifting. Twisting while lifting can cause a serious injury •k eep the load close to your body. Having to reach out to lift and carry a load may cause a back injury • t ry to carry the load in the space between your shoulder and your waist. This puts less strain on your back muscles • lift with your legs not your back; bend your knees and not your back • t o pick up the load, keep your back straight, balance feet on floor, bend from the hips and knees and avoid twisting the body •w here possible, slide instead of carrying. 124 Acute Management of a Painful Back • s top the aggravating activity • r est, preferably in a lying position on a firm surface •u se icepacks to reduce inflammation and pain • s eek medical advice for a thorough assessment even if pain subsides. Emergency childbirth may be due to a woman’s labour proceeding so fast (especially if she is having her second or subsequent baby) that there is not enough time for medical help to arrive before the baby is born. If you are the only person present at such a birth, remember that birth is a natural process and that you are there to provide support and assistance to the mother as required. The majority of births are not life-threatening emergencies. Preparing for Birth In you are present during emergency childbirth: •c all for an ambulance 000 •m ake the room warm and the mother comfortable with pillows •p lace a clean sheet beneath the mother and, if possible, a plastic sheet beneath the clean sheet • r eassure the mother and remain calm •d o not be alarmed if there is a lot of fluid, some of it bloodstained: this is normal. The Three Stages of Labour Stage One • t he mother experiences regular contractions. The strength and frequency of contractions will increase over a period of time Advanced First Aid Emergency Childbirth •d uring pregnancy a mucus plug has formed a barrier between the mother’s uterus and vagina. This will be expelled as a bloodstained discharge • t here may be a slow trickle or a sudden gush of fluid from the vagina, which is the fluid from around the baby being released from the membranes. This is known as the breaking of the waters. Stage Two •c ontractions become much stronger and are usually accompanied by an urge to push 125 • t he baby may place pressure on the rectum and may cause the mother to use her bowels •a dvise the mother to push only when she is a having a contraction, so that the two forces combine to expel the baby • once the cervix is fully dilated, the baby proceeds down the birth canal and the head rotates and appears at the opening •a s the head emerges, it rotates again to help the shoulder out. Do not pull on the baby; it will deliver naturally without force After the baby has been born, the mother’s uterus continues to contract to expel the placenta, or afterbirth. The contraction also prevents excess bleeding from the wall of the uterus as the placenta is pulled away. This completes the third and final stage of labour. At this time: •d o not place pressure or pull on cord • r etain placenta for examination at hospital •b reast feeding a baby directly after birth will help with uterine contraction • if the umbilical cord is around the baby’s neck, place two fingers beneath the cord and slide it over the baby’s head. The second stage of labour ends when the baby emerges completely from the mother’s birth canal. Stage Three • t he umbilical cord can be left uncut until help arrives or until mother and baby reach hospital. It may appear to pulsate for a few minutes • if the umbilical cord has to be cut, tie in two places 25cm and 30cm from the baby. Cut between these ties ©4-Life 126 • t he placenta (afterbirth) will come out of the vagina between 10 to 40 minutes following birth. Care of Newborn Infant Once the baby is born the First Aider should: •w ipe mucus from both nose and mouth while holding the baby Care of Mother Following the birth the First Aider should: •o bserve the mother for any further bleeding •p lace a clean combine or sanitary pad in place Advanced First Aid •d o not remove ties once cord has been cut. Observe closely for haemorrhage at the cut sites and control if present •e nsure all pads or products from birth are retained and sent with the mother to hospital •h elp with clean clothing and/ or hygiene for the mother •k eep warm. • s timulate breathing by rubbing the baby’s back • if no signs of life after 1 minute start CPR •w rap the baby in a blanket and maintain body warmth immediately •n ote time of delivery. 127 128 Techniques TECHNIQUES 129 Techniques Hand Washing Hand washing is a very important technique and is one of the most basic ways to prevent the spread of disease. Good hand washing technique is easy to learn and essential when performing aseptic dressing procedures: •h ave access to appropriate hand washing facilities • r emove any items of jewellery worn on hands or wrists • t urn on water and regulate to appropriate temperature •w et your hands with warm running water •a pply liquid soap from dispenser (bar soap should be avoided whenever possible due to potential of cross infection) • r ub hands together, making a soapy lather, wash the front and back of hands, as well as between your fingers and under your nails. Work lather over hands and wrists all the way up to elbows. This must be done for at least 1 minute 130 • if nail brush to be used it must be single use brush only and discarded after use • r inse soap off thoroughly using a single use disposable hand towel • t urn off tap by using hand towel or back of elbow. Do not turn off with bare hands •d iscard hand towel into foot pedal operated bin. Temperature A temperature can be taken with a thermometer. There are several types of thermometers available to take a temperature with: • digital •g lass with a bulb containing mercury. Taking a Temperature •w ash hands prior to procedure •e xplain to casualty the procedure you are about to perform • if using glass thermometer shake mercury into base of thermometer • if using digital press “on” button. Underarm Method •m ake sure under arm is dry •p oint the thermometer upward and place the tip well into the casualty’s underarm Techniques •w ipe the thermometer with an alcohol wipe prior to use. Digital thermometers also come with a plastic probe cover for hygiene purposes. • f old casualty’s arm over chest to hold in place and keep air away from underarm •k eep in place for 4 minutes • if using digital listen for beep Oral Method •p lace thermometer bulb (glass) or probe (digital) under tongue, hold in place with mouth closed •k eep in place for 2 minutes • if using digital a beep will be heard when ready • r emove thermometer, read temperature on display and record result •c lean thermometer with alcohol wipe and place back into storage container. • r emove thermometer, read temperature on display and record result •c lean thermometer with alcohol wipe and place back into storage container. Eye Irrigation The purpose of eye irrigation is to dilute or remove chemicals from the eye. It can also help to relieve pain and burning that can be associated with a foreign body: •e xplain and reassure the casualty •w ash your hands • if possible, put on gloves 131 •p osition the casualty for comfort and easy access to perform the procedure. Ensure adequate lighting •p repare equipment required (eye irrigation solution, towel to protect casualty and surrounds, bowl to catch fluid from irrigation) Aseptic dressing technique is an important procedure performed for the management of chronic, acute and infected wounds. It is important that the procedure is undertaken in the correct way to promote wound healing and prevent infection: •a sk casualty to open both eyes • check for a care plan regarding the wound and its treatment • t aking care not to apply direct pressure to the eyeball, hold the lids open on affected eye •p repare and protect the appropriate working surfaces with disinfectant solution before commencing procedure •d irect a gentle and steady flow of eye wash solution from the inner aspect of eye to outer aspect of eye. Catch excess fluid in bowl •a ssemble necessary equipment for procedure – antiseptic soltuion, new dressing and dressing pack •e ncourage the casualty to move eye in all directions • r e-examine eye after irrigation procedure • r epeat if unsuccessful •e nsure casualty is clean, dry and comfortable after procedure •a n eye patch may need to be applied for further protection. 132 Dressing Technique •p lace disposable waste bag within easy access of working surface to discard used dressing material in. • prepare the wound for dressing. Loosen dressing for easy removal •w ash hands •o pen the outer cover of dressing pack and remove inner pack placing onto prepared surface •w ith forceps used for arranging items, remove loosened dressing and discard dressing and forceps into rubbish bag •o pen appropriate dressings required and place on sterile dressing surface or pour solutions that are required into sterile dressing container •w ash hands using appropriate technique •p ut on sterile gloves if available • if no gloves are available, use the non touch technique • s terile dressing towel should now be placed between wound and person performing dressing to maintain sterile dressing field •u sing dressing forceps pick up and moisten swab with solution in container •c lean wound by using one swab at a time, swab from outside of wound to within. One swab for each stroke Techniques •w ith the forceps which can be viewed on outer surface of pack open inner pack and arrange contents •o nce wound has been cleansed, dry wound and cover with new sterile dressing. Secure with tape •a ll used dressing items to be placed onto used dressing tray and wrapped up •p lace wrapped items into waste bag. Waste bag is then disposed of into medical waste •d isinfect working surface •w ash hands thoroughly •c omplete any paper work regarding procedure. 133 Taking a Pulse A pulse represents the beating of the heart. Radial Pulse This is the pulse that is taken at your wrist. The radial pulse may not be present if the person is in shock. To take the radial pulse: • move your fingers along until you can feel a slight pulsation – this is the carotid pulse. The pulse rate is the amount of beats counted over one minute. For example, a pulse may be recorded as 70 beats per minute. Blood Pressure •u se 2 fingers, preferably the 2nd and 3rd finger •p lace them in the groove in the wrist that lies below the thumb •m ove your fingers along until you can feel a slight pulsation, this is the radial pulse. Carotid Pulse This is the pulse felt in your neck. The carotid pulse can be more easily felt and is sometimes stronger than the radial pulse. A Carotid pulse should be the preferred pulse check site: •u se 2 fingers, preferably the 2nd and 3rd finger • place them along side the outer edge of the trachea (windpipe) 134 There are several types of blood pressure machines available to take a blood pressure with: •m ercury sphygmomanometer •a neroid sphygmomanometer • electronic device. Preparing to take a Blood Pressure • the casualty should not smoke, drink alcohol or coffee approximately 15 minutes prior to procedure •a rm should be supported with a pillow • r est before the procedure •d on’t talk during measurement • r emove any thick clothing covering arm. Blood Pressure by Palpation •p lace the cuff around the arm leaving the cuff’s lower edge about 2cm above the bend of the elbow •c lose the cuff around the arm using the velcro to secure in place •w ith one hand locate the brachial or radial pulse by using 2 fingers (palpation) •w ith the other hand tighten the screw at the side of the rubber bulb •b y squeezing the bulb air is pumped into the cuff which causes it to expand • inflate the cuff 30mmHg. above the point where the brachial or radial pulse disappears Techniques •m ake sure the casualty is sitting in a comfortable position with back supported •o pen the screw slowly whilst feeling for the return of the brachial or radial pulse • look at sphygmomanometer and note reading when pulse returns •c ompletely deflate the cuff and write down the reading e.g., 120/P (P=Palpation). Blood Pressure by Stethoscope A stethoscope is a device used to listen for sound at various locations around the body. The part which comes in contact with the body is known as the bell. There are two ear pieces connected by tubing at the other end of the stethoscope. •w ith one hand place the bell of the stethoscope over the brachial artery •w ith the other hand tighten the screw at the side of the rubber bulb 135 •by squeezing the bulb air is pumped into the cuff which causes it to expand • inflate the cuff 30mm Hg above the point of the brachial pulse sound disappearing •p lace the cuff around the arm leaving the cuff’s lower edge about 2cm above the bend of the elbow •o pen the screw slowly whilst listening for the return of the brachial pulse •c lose the cuff around the arm using the velcro to secure in place • look at sphygmomanometer and note reading when the sound of the pulse returns. This is known as the systolic pressure • s witch on the machine •c ontinue to look at the sphygmomanometer, note reading when the sound of the pulse disappears. This is known as the diastolic pressure •c ompletely deflate the cuff and write down the reading: e.g., 120/80. 136 Blood Pressure by Electronic Devices •n umbers will display on screen, once this has occurred press the start button • t he machine will automatically inflate and deflate the cuff • t he machine will display results when complete •R ecord the reading: e.g., 120/80. Workbook WORKBOOK 137 Workbook Questions Introduction 1. What are the 4 aims of First Aid? 1. 2. 3. 4. 2. List 4 situations in which you may need to assist with First Aid? 1. 2. 3. 4. 3. You should provide First Aid until: 1. 2. 3. 4. 4.Does a conscious casualty need to give consent for a First Aider to initiate care? Yes No 5.Do you need consent to initiate First Aid treatment to an unconscious casualty? Yes No Explain your answer 6.What are 2 recommended guidelines when preparing a First Aid treatment report? 1. 2. 7. Why is it important for a First Aider to possess a First Aid kit? 138 9. H ow should you dispose of used bandages? Workbook 8.How can First Aiders protect themselves against exposure to a casualty’s body fluids? Human Anatomy 10. What is the heart’s role in the body? 11. What are the main parts of the respiratory system? 12. What is the function of the respiratory system? 13.What are 2 functions of the musculoskeletal system? 1. 2. 14. What is the function of the lymphatic system? 15. What is one of the main functions of the skin? Emergency Action Plan 16. What does DRSABCD stand for? 17. Complete this sentence: Safety to you, bystanders and 18. List 2 reasons why you would move a casualty: 1. 2. 139 19.What is one of the main causes of an airway obstruction in an unconscious casualty? 20. What is rescue breathing? 21.When performing CPR on an adult how many compressions are recommended per minute? 22. Only stop CPR when: 23.What 2 numbers can be dialled to call emergency assistance from a mobile telephone? 24.What information needs to be provided to emergency services when calling for help? 25.What are 2 reasons why somebody would wear a ‘MedicAlert® bracelet and or necklace’? 1. 2. Airway Management 26. What are 2 techniques used to open an airway? 1. 2. 27.What are 3 actions to be taken when assessing whether or not a casualty is breathing? 1. 2. 3. 140 29.What is the risk of leaving an unconscious casualty lying on his/her back? Workbook 28. If the casualty is not breathing normally, what should you do? 30.When placing an unconscious pregnant woman in a recovery position, on which side should she be placed and why? Cardiopulmonary Resuscitation 31. What are the 4 links of the ‘Chain Of Survival’? 1. 2. 3. 4. 32.When performing CPR on an adult, how many compressions are needed for every 2 breaths? 33. List 3 reasons when CRP can be stopped: 1. 2. 3. Assessing a casualty 34.The secondary assessment should only be performed on an unconscious casualty? True False 35. Where on the body does the secondary assessment begin? 36.When performing a secondary assessment on a casualty what are you looking for when examining limbs? 141 Bleeding and Shock 37. What are the 2 types of haemorrhage? 38.What is involved in the management of an external haemorrhage after the First Aider has checked DRSABCD? 39. A First Aider should remove an embedded object: True False 40. Should an amputated body part be placed directly in ice? True False 41.When pinching the nose to stop a nose bleed how long should you apply pressure? 42.What are 5 signs and symptoms of Shock? 1. 2. 3. 4. 5. Burns 43. What are the 3 classifications of burns? 1. 2. 3. 44. How long should you cool a burn with cool running water? 45. Should you remove a casualty’s clothing if it is adhered to the skin? True False 46.If chemicals enter an eye, how long should you irrigate the eye and what type of fluid can be used to irrigate? 142 47.If an unconscious casualty has discharge from the left ear, which ear should be closer to the ground once placed in the recovery position? 48. Give one reason a helmet can be removed in an emergency. Workbook Trauma 49.List 5 signs and symptoms that may be evident when a casualty fractures a rib. 1. 2. 3. 4. 5. 50.If there is a protruding object embedded in the chest, how should you bandage the area? 51.What sort of dressing should be placed over an injury where abdominal contents are exposed? 52.List 5 signs and symptoms of a fracture. 1. 2. 3. 4. 5. 53. Explain the difference between an open and closed fracture. 54.A fracture is _____________________________ to prevent the sharp edges of the ___________________________________ from moving and cutting tissue, muscle, blood vessels, and nerves. 55. W hat is meant by the term ‘soft tissue’? 143 56. What is the treatment for a soft tissue injury? R I C E Medical 57. Explain Syncope. 58. What are 3 common causes of Anaphylaxis? 1. 2. 3. 59.List 5 signs and symptoms that may indicate a person suffering from Anaphylaxis. 1. 2. 3. 4. 5. 60.What is the device called that a person suffering from Anaphylaxis may carry with them? 61. What colour is the Ventolin container? 62.What are 3 signs and symptoms of a person suffering from Hyperventilation? 1. 2. 3. 63. Explain the term stroke. 144 65.What is the treatment for a conscious person who is pale and sweaty and who is known to have diabetes? Workbook 64. What are 2 signs of stroke? 1. 2. 66.Should the First Aider place something in the mouth of a person who is having a seizure? Yes No 67. Why do Febrile Convulsions occur in some children? 68. List 5 signs and symptoms of a Heart Attack. 1. 2. 3. 4. 5. 69.In a choking person who is coughing effectively, is the treatment to apply firm blows to the back? Yes No 70. What is the Poison Information Centre phone number? 71. Does a person who is suffering from heat stroke sweat? Yes No Bites and Stings Envenomation 72. What is the main goal when treating a casualty for snake bite? 73.What is the treatment for a Red-Back Spider bite? 74.How is the barb removed from a bee sting? 75. What is the treatment for a tick bite? 145 146 Index INDEX 147 A abdominal injuries 67 adrenaline 78 AED 34 airway management 24 airway management (adult) 26 airway management (child) 26 airway management (infant) 26 airway obstruction 24 anaphylaxis 77 angina 91 ant sting 105 aseptic dressing technique132 assessing an accident scene 42 assessment, primary 42 assessment, secondary 43 asthma 79 Automated External Defibrillation See AED B back care See spine care bee stings 105 basic life support flow chart (DRSABCD) 21 bends, the See DCS behavioural emergencies118 bleeding 48 bleeding (external) 48 bleeding (internal) 52 blood pressure, taking 134 blue-ringed octopus sting 106 box jellyfish sting 108 148 breathing (adult) breathing (child) breathing (infant) burns burns (airway) 27 27 28 55 57 C cardiac arrest 40 cardiopulmonary resuscitation See CPR cardiovascular system 12 Chain of Survival 41 chest injuries 65 chest pain 90 chest wound, penetrating 65 childbirth, emergency 125 choking 83 choking (adult, child) 84 choking (infant) 85 compressions, chest (adult, child) 32 compressions, chest (infant) 32 cone-shell sting 107 CPR 36 crush injuries 68 D DCS decompression sickness See DCS defibrillation diabetes digestive system diving emergencies DRSABCD 115 33 87 14 115 18 E ear, object in ear, insect in eardrum, ruptured ECC emergency action plan See DRSABCD endocrine system EpiPen® external chest compression See ECC eye injuries eye irrigation F fainting See syncope febrile convulsion first aid kits first aid, definition fish stings fitting See seizure fractures funnel web spider bite 21 100 94 59 60 60 32 14 77 61 131 86 6 3 109 69 104 G getting help (emergency services) 8 H haemorrhage See bleeding hand washing technique 130 head injuries 58 head tilt technique 25 heart attack 91 heat exhaustion 96 heatstroke 97 helmet removal 64 Hudson face mask 119 hygiene, first aid 7 hyperglycaemia 88 hyperventilation 81 hypoglycaemia 87 hypothermia98 I insect stings J jaw, fractured jaw thrust technique Index DRSABCD, flow chart drowning drug overdose 105 70 25 L labour (stages of) 125 legal considerations in first aid 4 limb, fractured 70 lung, ruptured 116 lymphatic system 14 M machine accidents medical alert devices medical oxygen medical oxygen regulators mouth-to-mask 113 9 119 121 30 149 mouth-to-mouth 29 mouth-to-mouth-and-nose29 mouth-to-nose 29 mouth-to-stoma 30 musculoskeletal system 13 N nebuliser mask device nervous system nose bleed O oral airways oropharyngeal airways See oral airways oxygen administration P pelvis, fractured pressure immobilisation technique poisoning primary assessment See assessment, primary pulse, taking 120 11 51 secondary assessment See assessment, secondary shock 53 seizure (fitting) 89 skin, the 15 slings, types of 71 snake bites 102 soft bag and mask device120 soft tissue injuries spider bites 122 119 73 103 spinal injuries 63 spine care 123 splints (fractures) 70 stroke 82 syncope (fainting) 76 70 T temperature, 102 92 techniques of taking 130 the bends See DCS 134 R reassuring the casualty 10 recovery position 22 red-back spider bite 103 reproductive system 15 rescue breathing 29 respiratory system 13 R.I.C.E. (soft tissue injury) 73 road accidents 113 150 S tick bite tooth injuries 110 62 touch and talk technique 19 triage 112 U unconscious casualty 22 urinary system 14 W wasp stings 105 IN AN EMERGENCY CALL: 000 Remember: Any resuscitation is better than none at all. AED = Automated External Defibrillator Source: ARC Basic Life Support Flow Chart (2011) Poisons Information Centre: 13 11 26 Registered Training Organisation National – Provider Code 40185 – CRICOS No. 03222F Associate Member of the Australian Resuscitation Council (ARC) 300 2 4LIFE 4Life Phone: 1 1300 2 45433 Email: info@4lifetraining.com.au Website: www.4lifetraining.com.au