White blood / Weisses Blut
advertisement
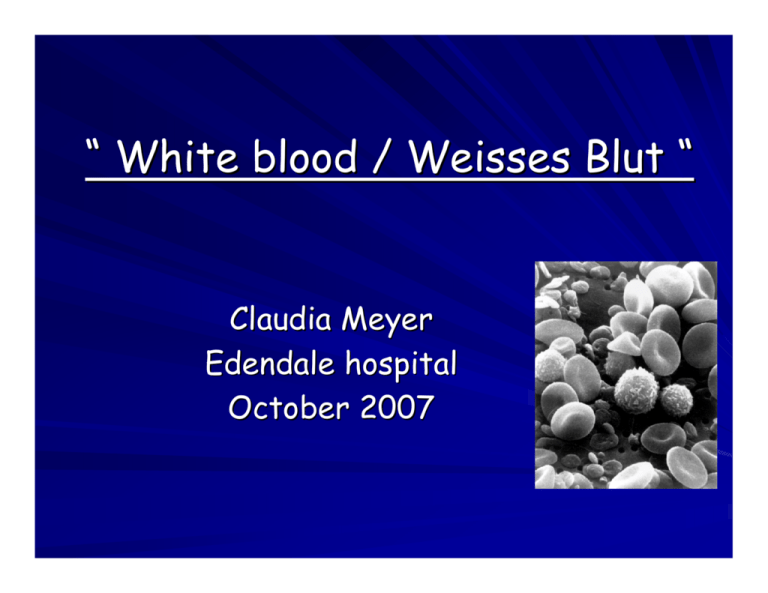
“ White blood / Weisses Blut “ Claudia Meyer Edendale hospital October 2007 Index patient: Main complaint 21 year old gentleman from Edendale Main complaint: Gingival bleeding and fatigue for 7 months Epistaxis and dizziness for 2 weeks No haematuria, no haematemesis, no melaena, no haemoptysis PMH: HIV positive, CD 4 unknown, not on HAART. No previous opportunistic infections, no previous malignancy Drugs: Nil. Not on Co-trimoxazole History cont. Allergies: Nil known Social: Non-smoker. No ethanol use. Salesman. One sister from same parents, 8 half-siblings. No occupational exposure to radiation, pesticides, benzene. Family History: Nil of note. Travel History: Nil. Systemic enquiry: No LOW, no night sweats or fever. Decreased exercise tolerance. No other resp or cvs S. No ecchymosis or jaundice. No polyarthralgia, no photosensitivity. Clinical examination General : Pallor, anicteric, acyanotic, small mobile LN submandibular, no oedema, no oral candidiasis No ecchymosis, no skin nodules, no lesions suggestive of Kaposi’s sarcoma Vital signs: Apyrexial, BP 99/48 mmHg, HR 112bpm, weight 57kg CVS: APPE, JVP →, tachycardia, regular, good volume, apex undisplaced, hyperdynamic, heart sounds normal, 2/6 ESM at LSB Clinical examination Resp: RR 14, resonant, clear, bilat b/s Abdomen: soft, non-tender, no organomegaly Neuro: alert, orientated, no focal signs, no retinal haemorrhages ENT: no gingival hypertrophy, enlarged tonsils bilaterally, but not inflamed. Urine: No macroscopic or microscopic haematuria. No proteinuria. No urobilinogen. Ward Hb: 2 g/dl Clinical assessment 21 year old salesman presents with symptoms suggestive of a qualitative or quantitative platelets defect and severe anaemia, in the absence of palapable organomegaly. The patient is HIV positive, without prior opportunistic infections. Differentials: Aplastic anaemia Malignancies: ALL, AML, lymphoma Myelodysplasia Opportunistic infections Investigations FBC: HB 3.2 g/dl; MCV 87 fl; MCH 32.2 pg; WCC 1.25; abs neutr 0.43, abs lymph 0.58; mono 0.02; PLT 20, MPL 7.8 fl Corrected Reticulocyte count : 0.77% U&E, CMP: normal, LDH: 275 iu/l, Uric acid: 0,29 mmol/l LFT: TP 95 g/l, alb 21 g/l, rest normal Coagulation: 1.22; APTT 23.7 secs, control 28,9 secs, D-Dimer 1000 ng/ml, Fibrinogen 2,0 g/l CD4 count: 268 cells/ul Investigations cont. Smear: pancytopenia, anisocytosis 2+, occasional promyelocytes noted Urgent BMAT and Trephine: Acute promyelocytic leukemia, trephine demonstrates neoplastic infiltration. PCR, cytogenetic tests and flow cytometry pending. Ultrasound abdomen: no organomegaly, no lymphadenopathy, normal CXR: normal Blood culture, u-MCS: no growth Acute myelocytic leukemia Acute myelocytic leukemia Heterogeneous group of diseases Clonal disorder of haematopoietic progenitor cells which lose the ability to differentiate normally and to respond to normal regulators of proliferation. Incidence of AML 3,6 per 100 000 per year, increases with age. Median age at presentation at 70 years. Acute promyelocytic leukemia is a subtype of AML, median age of presentation 25 years. Etiology Heredity: Somatic cell aneuploidy eg. Trisomy21; Excessive chromosome fragility eg Bloom S Ionising radiation: ↑ Incidence AML 5-7 yrs after atomic bomb explosion. Chemicals: Benzene, smoking, petroleum products, paint, ethylene oxide, pesticides. Drugs: 1. Alkylating agent-associated leukemias 4-6 yrs after exposure (chr 5; 7); 2. Topoisomerase II inhibitor-associated leukemias occur 1-3 yrs after exposure (chr 11; t 15:17; t 8:21); 3. Chloramphenicol, chloroquine → BM failure that may evolve into AML Haematopoiesis Neutrophil development Multipotent stem cell ↓ Common myeloid progenitor cell ↓ GM Commited precursor cell ↓ Granulocytic progenitor cell ( lineage committed cells ) ↓ Myeloblast → ↓ ← Promyelocyte ↓ Myelocyte ↓ Metamyelocyte ↓ Band form → ↓ Neutrophil Classification French-American-British Classification (1985) 8 major subtypes according to morphology & cytochemisty. Required > 30% myeloblasts in BM for diagnosis. M0 M1 M2 M3 M4 M5 M6 M7 Minimally differentiated leukemia Myeloblastic leukemia without maturation Myeloblastic leukemia with maturation Hypergranular promyelocytic leukemia Myelomonocytic leukemia Monocytic leukemia Erythroleukemia Megakaryoblastic leukemia WHO Classification Requires presence of > 20% myeloblasts in blood and/or BM. Incorporates molecular & cytogenetic, morphologic (multi-lineage dysplasia ), clinical features ( prior haematologic disorder ). - Recurrent translocations: t(8;21)(q22;q22), t(15;17)(q22;q22), t(16;16)(p13;q22). t(v:11q23) - Multi-lineage dysplasia - Therapy related AML & myelodysplastic S - Not otherwise categorised - Acute myelomonocytic L - Acute leukemia of ambiguous lineage - Bilineal acute L Leukemogenesis of AML Two-hit model: Class 1 genetic damage: results in constitutive activation of cell surface receptors ( eg RAS ), or receptor tyrosine kinases ( eg FLT 3, c-KIT ) → clonal expansion Class 2 genetic damage: results in formation of fusion genes that block myeloid differentiation. FAB Classification & associated genetic abnormalities Leukemogenesis of M3 RARs are nuclear receptors that act as ligand-dependent transciption factors ↓ t ( 15;17) ( q22;q12) ↓ PML-RARα fusion protein binds retinoid acid response elements ↓ suppresses gene transcription and blocks differentiation of the cell ↓ differentiation at promyelocyte stage arrested Clinical presentation Symptoms related to pancytopaenia: easy fatigue, infections, hemorrhagic findings Constitutional Sx: LOA, LOW, fever Pallor, fever, infection, hemorrhage including retinal hemorrhages Hepatosplenomegaly, lymphadenopathy Infiltration of gingivae, skin, soft tissues or meninges ( monocytic subtype M4 and M5) Granulocytic sarcoma ( chloroma ): mass consisting of leukemic cells in soft tissues, breast, uterus , ovary, GIT, lung or other organs → associated with t(8;21) Clinical presentation: M3 APL can be complicated by DIC ( at diagnosis or initiation of chemotherapy). Mechanism: 1. Tissue factor → forms a complex with F VII to activate F X and IX 2. Cancer procoagulant, which activates F X 3. ↑ Annexin R expression on surface of leukemic promyelocyes→ annexin II R binds plasminogen & tissue plasminogen activator → this results in increased plasmin formation Thrombocytopenia as well as platelet dysfunction Diagnosis BM aspirate & trephine biopsy Cytogenetic: RT-PCR for AML 1ETO and CBFB-MYH 11 in nonAPL and PML-RARA in suspected APL, FISH in selected cases Cytochemistry ( MPO or Sudan Black, combined esterase ) Immunophenotyping for specific intracellular & surface antigens Treatment of AML: Overview Induction Rx : age younger > 60 – 65 yrs ↓ ↓ “3+7“ Standard Rx or ↓ investigational Rx Postremission Rx: or supportive Rx risk stratify ↓ ↓ ↓ favourable intermed averse risk (good) (standard) (poor) ↓ ↓ ↓ cytarabine cytarabine allogenic tplt or new drugs Treatment of AML Induction therapy: Aim is complete remission: BM < 5% blasts, neutrophils > 1000, PLT > 100 000 3 + 7 combination “→ daunorubicin IVI 3 days, cytarabin IVI for 7 - 10 days Postremission therapy: Risk stratify ! Cytogenetic abnormalities Elderly AML patients Associated with: 1. more adverse cytogenetics 2. overexpression of MDR 1 gene encoding a drug efflux pump p-glycoprotein 3. ↑ incidence of prior myelodysplasia 4. generally do not tolerate chemotherapy as well as younger patients Options: A) Standard treatment B) Palliative chemoR: low-dose cytarabine C ) investigational treatment (clinical trial ) D ) supportive care ( very poor performance status, abn organ Function, > 80 yrs old ) General measure & supportive care Hyperleukocytosis: leucopheresis if Sx ( but not in PML) Tumour lysis S: hydration, allopurinol, monitor I + O, recombinant urate oxidase (rasburicase) Platelet transfusion Packed cell transfusion Anti-infective Rx Use of prophylactic AB controversial Haematopoietic growth factors G-CSF given after completion of chemotherapy → reduce duration of neutropenia and decrease AB use, but no effect on rates of remission or overall survival. “ Priming effect “: G-CSF could stimulate leukaemic cells to proliferate, which could increase their susceptibility to chemotherapy→ reduction in relapse and improved survival for patients with standardrisk AML. Treatment M3: ATRA ATRA as soon as Dx of APL suspected and given for prolonged time ( 21-60days) Treatment M3 Retinoic acid syndrome: ATRA → diff. of APL cells → cytokine release & surface adhesion molecule modulation → capillary leak & fluid retention as well as organ infiltration by leukaemic cells. Sx/Tx: cough, dyspnoea, fever, pulm infiltrates, pleural & pericardial effusion, oedema, Lab: ↑ WBC Management: stop ATRA temporarily, dexamehtasone 10mg bd IVI; prophylactic steroids with induction Rx – benefit uncertain. Treatment M3 Induction: - ATRA - daunorubicin & cytarabin IVI Consolidation: 2-3 anthracycline- based courses, ATRA Maintenance therapy: ATRA Coagulopathy: 1. Keep PLT > 50 until remission. 2. Keep coagulation times normal with FFPs 3. Anti-fibrinolytic agents if life threatening hemorrhage Patient progress Initial resuscitation with packed cells, developed massive epistaxis 4 days later, hence received a total of 8 units packed cells and 1 pool of platelets over the next 10 days Cyclokapron, H2 receptor antagonist, Piperacillin-Tazobactam and Gentamycin No isolation facilities were available at EDH Patient progress Whilst awaiting transfer to IALCH: ATRA 40mg bd, Prednisone 30mg dly, Omeprazole 20mg dly, Cyclokapron The patient is currently undergoing induction therapy at IALCH with ATRA, daunorubicin & cytarabin. References Estey E. AML. Lancet 2006; 368:1894 - 90 Lowenberg G. AML. NEJM 1999; 341: 1051 - 1059 British Committee for Standards in Haematology. British Journal of Haematology 2006; 135: 450 - 474 UpToDate Schiffer C. Hematopoietic Growth factors and AML. NEJM 2003; 349: 727 - 729 Lowenberg B. Effecy of Priming with G-CSF on the outcome of chemotherapy for AML. NEJM 2003; 349: 743 - 52 Menell J. Annexin II and Bleeding in acute promyelocytic leukemia,. NEJM 1999; 340: 994 – 1004 References cont. Pedersen-Bjergaard. Insights into leukemogenesis from therapy-related leukemia. NEJM 2005. 352: 1591-1594 McPhee S. Pathophysiology of disease. Lange. Fifth edition p 116 Kaushansky K. Lineage-Specific Hematopoietic Growth Factors. NEJM 2006;354:2034-45 Thank you ! Molecular monitoring : RT-PCR assay to detect minimal residual disease and relapse. Relapse: ATRA + chemoRx followed by rescue using allogenic stem cells Mechanism of chemotherapy ATRA: All-trans retinoic acid ( tretinoin): discussed previously Cytarabine: inhibition of DNA polymerase Daunorubicin: Anthracycline AB 1. inhibits topoisomerase II 2. High affinity binding to DNA through intercallation → results in blockade of DNA & RNA synthesis 3. Alteration in cell membrane transport 4 Generation of oxygen free radicals that cause DNA strands to break Topoisomerase II