Leg discomfort
advertisement

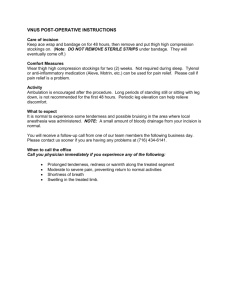
Clinical practice 55 Leg discomfort Leg discomfort is a common presentation among the elderly and can be a manifestation of many different disease processes. One key issue is how to differentiate between the benign and the more serious causes. Tis article will explore the main differential diagnoses including the most common causes and management of these, and the recognition of potentially life or limb threatening causes with an overview of red flag signs and symptoms. Dr Louise Powter, Specialty Registrar, Acute Medicine, Gloucestershire Royal Hospital, Great Western Road, Gloucester Dr Pippa Medcalf, Consultant Geriatric Medicine, Gloucestershire Royal Hospital, Great Western Road, Gloucester Email louisepowter@nhs.net Leg discomfort can be caused by problems in the skin, muscles, vasculature or nerves of the leg itself, be due to more distant disease for instance in the spine, or be the presentation of systemic disease. A useful way to think of the differential diagnosis is to differentiate between unilateral and bilateral causes (see box 1). History and examination The information gained from the history of patients with leg discomfort will guide subsequent examination and investigations. Are the symptoms unilateral or bilateral? Is there a history of trauma? Determine the type and site of any pain, the presence of any neurological or vascular symptoms; including symptoms outside the affected leg for instance back pain, urinary incontinence or retention. Are there any systemic symptoms to indicate an infective or inflammatory cause? A thorough review of the past medical history will elicit risk factors for venous thromboembolism, peripheral vascular disease, and www.gerimed.co.uk infections (such as diabetes or immunosuppression). The appearance of the affected leg will give clues as to the diagnosis. Erythema may indicate cellulitis or DVT, chronic discolouration is seen in venous insufficiency and venous eczema, pallor or levido reticularis is seen in ischaemia, and in chronic ischaemia the skin may be shiny and atrophic with loss of hair. Muscle wasting and fasiculations indicate a lower motor neurone neurological condition. Look for generalised leg oedema, unilateral or bilateral, or more specific swelling for instance a joint effusion or a baker’s cyst. Assess the power and sensation of both legs and perform a full nervous system examination including anal tone and perianal sensation if a neurological condition is suspected. If a vascular cause is likely check the pulse rate and rhythm and perform an ECG, examine the heart, palpate the abdomen for an aortic aneurysm, listen for carotid and femoral bruits and check for the presence of peripheral pulses. In suspected trauma assess all joints for range of movement and check ability to weight bear. Vascular causes Deep vein thrombosis DVT has an incidence of around 1 in 1000. It can present with pain, swelling and erythema, although can be clinically silent. Clinical assessment combined with a validated pre-test probability score such as the Wells score1 can be used for risk stratification. British committee for standards in haematology guidelines suggest that a D-dimer assay should be sent in low risk patients. A negative D-dimer can safely exclude DVT in these patients. Low risk patients with a positive D-dimer and all moderate or high risk patients should have a compression ultrasound scan of the affected leg, and if negative this should be repeated in one week.2 If a DVT is found the patient should be anticoagulated for a period of six weeks to six months depending on the clinical context and local guidelines. Most trusts offer an ambulatory service for the March 2012 | Midlife and Beyond | GM 56 Clinical practice Box 1: Differential diagnosis Vascular DVT Superficial thrombophlebitis Chronic venous insufficiency Chronic peripheral vascular disease Acute ischaemia Neurological Spinal cord/cauda equina Radiculopathy Mononeuritis multiplex Peripheral polyneuropathy Restless legs Musculoskeletal Trauma Cramp Bone tumours Inflammatory Myositis Arthropathies Infection Cellulitis Necrotising fasciitis Osteomyelitis assessment and management of patients with suspected DVT. Te cause for the DVT is ofen obvious, for example recent immobility or surgery, but DVT may be the presenting feature of underlying diseases such as malignancy. DVT should be identified and treated to prevent fatal pulmonary embolism. Superficial thrombophlebitis Superficial thrombophlebitis presents with localised pain and erythema along a superficial vein. It GM | Midlife and Beyond |March 2012 Usually unilateral Usually unilateral Usually bilateral Usually bilateral Unilateral Usually bilateral Usually unilateral Unilateral Bilateral Bilateral Unilateral Bilateral Unilateral Bilateral Unilateral or bilateral Usually unilateral Usually unilateral Usually unilateral can be spontaneous or result from trauma or intra-venous cannulae. Risk factors include varicose veins, immobility and hypercoagulable states such as pregnancy and hormone therapy. If it is migratory, ofen travelling from one leg to the other, there is a strong association with adenocarcinoma of the pancreas or lung (Trousseau’s sign) and a search for an underlying malignancy should be undertaken. Patients with superficial thrombophlebitis may have an associated deep vein thrombosis, in one case series rates of DVT were 21.6% and PE 28.3%.3 Tis study did not identify any risk factors that were associated with underlying thromboembolic disease however other studies suggest risk factors include male sex, unprovoked thrombophlebitis and factor V leiden.4 Management of superficial thrombophlebitis includes nonsteroidal anti-inflammatory drugs, topical treatment and compression stockings. Te role of anticoagulants is controversial. Chronic venous insufficiency Chronic venous insufficiency is common in the elderly and presents with aching, pressure, burning, itching or heaviness in the legs, associated with leg oedema and reddish brown haemosiderin deposits in the skin and venous eczema. It results from venous hypertension and valve incompetence and is common afer DVTs (the post thrombotic syndrome). Management consists of leg elevation at rest and compression stockings. Surgery is reserved for severe cases. Peripheral vascular disease Peripheral vascular disease is very common and increases with age, affecting 20% of over 75s5. Presentation is often with intermittent claudication, where patients complain of leg pain or weakness on walking, which is relieved with rest. Symptoms may reduce as a collateral circulation develops. Rest pain that is relieved by hanging the leg down indicates critical limb ischaemia. Management www.gerimed.co.uk 58 Clinical practice Box 2: Red flag signs and symptoms Signs and symptoms Pain, pallor, pulselessness, parasthaesia, paralysis, perishingly cold Back pain, numbness, weakness, bladder or bowel symptoms, saddle anaesthesia Very painful, pale, tense leg following trauma Hot swollen joint Septic patient with rapidly spreading rash or pain out of proportion to skin signs of peripheral vascular disease includes lifestyle measures such as stopping smoking and control of cardiovascular risk factors. Antiplatelet therapy is recommended for patients with symptomatic peripheral artery disease6. Drugs licensed for treatment include cilostazol (Pletal), a phosphodiesterase III inhibitor, which has antiplatelet and vasodilator effects, and naftidrofuryl, which has vasodilator effects. Vascular intervention includes angioplasty, stenting, and bypass surgery. Referral to a vascular specialist should be made if the diagnosis is in doubt, if risk factors are unable to be managed to appropriate targets, or if the patient has symptoms, which limit their lifestyle. Young and otherwise healthy adults should also be referred to rule out entrapment syndromes. 6 Beta-blockers are ofen indicated for coronary artery GM | Midlife and Beyond | March 2012 Diagnosis Acute ischaemia Spinal cord compression or cauda equina compression Compartment syndrome Septic arthritis until proven otherwise Necrotising fasciitis disease in patients with peripheral vascular disease and this has previously caused concern, however a recent Cochrane review found no evidence that beta blockers adversely affect walking distance in people with intermittent claudication.7 Acute ischaemia may develop due to thrombus formation or emboli. This presents classically with the six Ps; pallor, pulselessness, pain, perishingly cold, parasthesia and paralysis. An acutely ischaemic limb needs urgent assessment for revascularisation. Neurological causes Spinal cord syndromes Spinal cord compression usually presents with back pain but can be associated with radicular pain and leg discomfort. Weakness and sensory loss are usually later features. Cauda equina syndrome ofen presents with non-specific symptoms, low back pain is usually a feature and leg pain, usually bilateral, and/or weakness can be the presenting complaint. Other symptoms include bladder and bowel dysfunction, sexual dysfunction and saddle anaesthesia. The most common cause of cord compression is malignancy and should be considered in any patient with known malignancy that presents with back pain or neurological symptoms. Central disc prolapse is a common cause of cauda equina syndrome; other causes include spinal stenosis secondary to osteoarthritis, trauma, or inflammatory conditions such as ankylosing spondylitis. In suspected metastatic cord compression an MRI of the whole spine should be performed within 24 hours. Te care of these patients should be determined by oncologists and spinal surgeons and will include high dose steroids, radiotherapy or surgery.8 Radiculopathy Radiculopathy can be caused by spinal cord compression or cauda equina syndrome, or can result from compression of the dorsal nerve root alone. Sciatica is the most common radiculopathy and presents as pain in the back or buttock radiating down the leg, and can be associated with numbness, tingling and weakness. The usual causes are disc herniation or degenerative disease. Peripheral neuropathy Peripheral neuropathy can be a mononeuropathy, mononeuritis multiplex or a polyneuropathy. All of these may present as leg www.gerimed.co.uk Clinical practice 59 discomfort. The most common cause of a mononeuropathy is compression neuropathy. Mononeuritis multiplex is normally caused by a systemic disease such as diabetes or vasculitidies. Symmetrical polyneuropathy is the most common form of peripheral neuropathy. It presents in a stocking distribution and can present with a whole array of sensory symptoms including burning, stinging, itching, tingling or numbness. If motor nerves are involved there may be weakness, cramps and spasms. The most common cause is diabetes mellitus. Other causes include alcohol, B12 deficiency, drugs such as isoniazid, chronic renal failure, hypothyroidism, malignancy and hereditary motor and sensory neuropathies (Charcot-Marie-Tooth). Patients with painful diabetic neuropathy should be offered duloxetine, and those with other neuropathic pain conditions should be offered amitriptyline or pregabalin.9 Restless legs Restless leg syndrome is very common. The pathophysiology is not fully understood but it is likely that there is involvement of the dopaminergic system and a possible depletion of iron stores. Te International Restless Leg Syndrome Study Group has developed standardised criteria for the diagnosis. 10 These are: an overwhelming urge to move the legs, onset of symptoms occurring or worsening with rest or inactivity, symptoms relieved by movement, and symptoms worse in the evening or at night. Te severity of symptoms can be assessed using a rating scale.10. www.gerimed.co.uk Box 3: Possible investigations or inflammatory cause is suspected underlying disease necessary crystals neuropathy or myopathy suspected Serum ferritin levels should be checked to rule out iron deficiency. Treatment for mild disease includes advice on good sleep hygiene, stretching and relaxation exercises. Patients with frequent symptoms can be prescribed a dopamine agonist.11 Musculoskeletal causes Trauma Trauma can cause fractures or damage to other tissues and is usually obvious, however sometimes elderly patients who are confused or have dementia will present with leg pain and decreased mobility and will not give a history of trauma. These patients may have hip or pelvis fractures that can be missed. Tibial fractures or other lower limb trauma can lead to compartment syndrome which should be suspected if there is pain out of proportion to the injury, or other signs such as pallor and parasthesia. Compartment syndrome is an emergency and the patient may require a fasciotomy to prevent tissue necrosis. Cramp Leg cramps are common especially in the elderly and at night. Tey are ofen idiopathic but may be secondary to uraemia, liver disease, thyroid disorders, volume loss such as diarrhoea or extreme heat, medication especially diuretics, radiculopathies or neuropathies. Idiopathic leg cramps can be diagnosed once underlying causes have been ruled out. Stretching exercises may help although there is limited evidence. 12 There is conflicting evidence for the use of quinine but it can be used if cramps are causing a significant March 2012 | Midlife and Beyond | GM 60 Clinical practice Arthropathies. Arthropathies of the knees, hips, ankles or foot joints typically presents as joint pain but may present as leg discomfort. Joint aspiration is mandatory if septic arthritis is suspected and will help in the diagnosis of a non-septic joint for example differentiating between gout, pseudogout and reactive arthritis. Infective causes disruption to sleep. 13 Quinine should be stopped after a four week trial if there is no benefit.14 Bone tumours Bone tumours are rare and usually present with gradually increasing pain, sometimes a mass or a pathological fracture. In the elderly bony metastases are more common than primary bone tumours and should prompt a search for a primary malignancy, ofen breast, lung or prostate. Inflammatory causes Myositis Leg discomfort and weakness may indicate an inflammatory GM | Midlife and Beyond | March 2012 myopathy. This group of disorders are characterised by muscle cell infiltrations causing inflammation. The main variants are polymyositis, dermatomyositis and inclusion body myositis. Polymyositis typically presents insidiously with a proximal myopathy, in dermatomyositis cutaneous features such as a heliotrope rash and gottron’s papules can precede the muscle symptoms by several years. Inclusion body myositis typically affects more distal muscles and onset is usually afer the age of 50. If an inflammatory myopathy is suspected specialist referral should be made. Some patients may respond to immunosuppression.15 Cellulitis Cellulitis is common in the elderly population. Te patient normally presents with a hot, erythematous, tender leg. Portals of entry can include any broken skin from trauma, scratching and fungal foot infections. Many patients will have underlying diabetes mellitus which may be a known diagnosis or the cellulitis may be the first presentation of diabetes, so blood sugar should be checked in these patients. Grading systems such as the Eron/Dall classification system can be used to assess whether a patient needs oral or intravenous antibiotics, and if they can be managed in the community or if they need hospital admission. 16 Intravenous antibiotics can be safely and effectively administered at home or in an ambulatory setting17 and many trusts offer an ambulatory service for once daily outpatient intravenous antibiotics. Necrotising fasciitis Necrotising fasciitis is a severe, rapidly progressing soft tissue infection that often presents on the lower limbs. It carries a high mortality. It can be differentiated from simple cellulitis as patients ofen complain of pain, which seems www.gerimed.co.uk Clinical practice 61 excessive compared to the physical appearance, as the infection spreads along deep tissue layers leaving the overlying skin intact. Te patient will appear toxic and deteriorate rapidly. There may be rapidly advancing erythema and a purpuric blistering rash with subsequent necrosis. If necrotising fasciitis is suspected the patient needs urgent surgical review and debridement. 2008; 4. Art. No. CD005508. cord compression, acute ischaemia 8. NICE Clinical Guideline and necrotising fasciitis. Look for 75. ‘Metastatic spinal cord “red flag” signs and symptoms and compression. Diagnosis and refer patients for urgent opinion and management of adults at risk of investigations if any of these serious and with metastatic spinal cord compression. November 2008 conditions are suspected. Conflict of interest: Dr Powter has none. Dr Medcalf has been sponsored to attend educational courses by pharmaceutical companies. Osteomyelitis Osteomyelitis may co-exist with References cellulitis and should be suspected if there is bone pain or a deep ulcer 1. Wells P, Owen C, Doucette S et al. Does this patient have deep vein acting as a portal for entry. Plain thrombosis? JAMA 2006; 295(2): radiographs may show lucent areas 199–207 or a periosteal reaction, but may 2. British committee for standards in be normal. Tese patients require haematology. The diagnosis of deep vein thrombosis in symptomatic prolonged intravenous antibiotics outpatients and the potential for and occasionally surgical treatment. Investigations 3. Possible investigations depend on the likely diagnosis as listed in box 3. Red flags Any red flag symptoms as described in box 2 should prompt 4. urgent further investigation. Conclusion 5. There are many causes of leg discomfort in the elderly. A thorough history and focused examination will guide the differential diagnosis 6. and subsequent investigation. Many cases are benign for instance leg cramps and restless legs; some are more serious but common, for 7. example deep vein thrombosis, and some are less common but life or limb threatening, for example spinal www.gerimed.co.uk clinical assessment and D-dimer assays to reduce the need for diagnostic imaging. British Journal of Haematology 2004; 124: 15–25 Lima Sobreira M, Humberto De Abreu Maffei F, Bonetti Yoshida W, et al. Prevalence of deep vein thrombosis and pulmonary embolism in superficial thrombophlebitis of the lower limbs: prospective study of 60 cases. International Angiology 2009; 28(5): 400-409 Hirmerova J, Seidlerova J, Subrt I. Superficial thrombophlebitis which cases are more risky? Journal of Thrombosis and Haemostasis 2009; 7/S2 (724): 1538-7933 Fowkes F, Housley E, Cawood E, et al. Edinburgh Artery Study: prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol 1991; 20(2): 384–92 Scottish Intercollegiate Guidelines Network. Diagnosis and management of peripheral arterial disease. A national clinical guideline. October 2006 Paravastu S, Mendonca D, Da Silva A. Beta blockers for peripheral arterial disease’. Cochrane Database of Systematic Reviews 9. N I C E Clinical Guideline 96. Neuropathic pain. The pharmacological management of neuropathic pain in adults in nonspecialist settings. March 2010 www.nice.org.uk/guidance/CG96 Accessed 12/2/12 10. Allen P, Picchietti D, Hening WA, et al. International Restless Legs Syndrome Study Group. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med 2003; 4(2): 101–9 11. Vignatelli L, Billiard M, Clarenbach P, et al. EFNS Task Force. EFNS guidelines on management of restless legs syndrome and periodic limb movement disorder in sleep. Eur J Neurol 2006; 13(10): 1049–65 12. Butler J, Mulkerrin E, O’Keeffe S. Nocturnal leg cramps in older people. Postgrad Med J 2002; 78: 596–98 13. El-Tawil S, Al Musa T, Valli H, et al. Quinine for muscle cramps. Cochrane Database of Systematic Reviews 2010; 12. Art. No.: CD005044 14. Medicines and Healthcare Products Regulatory Agency. Quinine: Not to be used routinely for nocturnal leg cramps. Drug Safety Update June 2010; 3(11): 3. 15. Mantegazza R, Bernasconi P. Dermatomyositis, Polymyositis and Inclusion Body Myositis. Madame Curie Bioscience Database. Landes Bioscience; 2000 16. Dall L, Peddicord T, Peterson S, et al. Hospitalist treatment of CAP and Cellulitis Using Objective Criteria to Select Patients.’ Infect Med 2003; 20(8): 379–90 17. Corwin P, Toop L, McGeoch G, et al. Randomised controlled trial of intravenous antibiotic treatment for cellulitis at home compared with hospital. BMJ 2005; 330: 129 March 2012 | Midlife and Beyond | GM