Issue 597 | January 2013 - Association of Clinical Biochemists

ACB News
The Association for Clinical Biochemistry
|
Issue 597
|
January 2013
In this issue
Ian Barnes
Heads Up
DofH QA
Review of
Pathology
Southend
& Basildon
Not Happy at Losing Out in East of
England
College
Launches
50 Objects
Haemoglobin is Harmonising
ACB
Application
Form for
New Trainees in this Issue
About ACB News
The editor is responsible for the final content. Views expressed are not necessarily those of the ACB.
Editor
Dr Jonathan Berg
Department of Clinical Biochemistry
City Hospital
Dudley Road
Birmingham B18 7QH
Tel: 07973-379050/0121-507-5353
Fax: 0121-507-5290
Email: jon@bergfamily.co.uk
Associate Editors
Mrs Sophie Barnes
Department of Clinical Biochemistry
12th Floor, Lab Block
Charing Cross Hospital
Fulham Palace Road
London W6 8RF
Email: sophie.barnes@imperial.nhs.uk
Mr Ian Hanning
Department of Clinical Biochemistry
Hull Royal Infirmary
Anlaby Road
Hull HU3 2JZ
Email: ian.hanning@hey.nhs.uk
Dr Derren Ready
Microbial Diseases
Eastman Dental Hospital
University College London Hospitals (UCLH)
256 Gray's Inn Road
London WC1X 8LD
Email: d.ready@eastman.ucl.ac.uk
Mrs Louise Tilbrook
Department of Clinical Biochemistry
Broomfield Hospital
Chelmsford
Essex CM1 5ET
Email: louise.tilbrook@meht.nhs.uk
Situations Vacant Advertising
Please contact the ACB Office:
Tel: 0207-403-8001
Fax: 0207-403-8006
Email: admin@acb.org.uk
Display Advertising & Inserts
PRC Associates
Sundial Court, Unit 4 - Ground Floor
Barnsbury Lane
Tolworth
Surrey KT5 9RN
Tel: 0208-337-3749 Fax: 0208-337-7346
Email: mail@prcassoc.co.uk
ACB Administrative Office
Association for Clinical Biochemistry
130-132 Tooley Street
London SE1 2TU
Tel: 0207-403-8001
Fax: 0207-403-8006
Email: admin@acb.org.uk
ACB President
Dr Michael Thomas
Department of Clinical Biochemistry
Royal Free Hospital
Pond Street
London NW3 2QG
Email: president@acb.org.uk
ACB Home Page http://www.acb.org.uk
Printed by Swan Print Ltd, Bedford
ISSN 1461 0337
© Association for Clinical Biochemistry 2013
ACB News
The monthly magazine for clinical science
Issue 597 • January 2013
General News
Council Matters
A Personal View
Practice FRCPath Style Calculations
Current Topics
Meeting Reports
Council Nomination Form
ACB News Crossword
Application for Election to
Membership Form page 4 page 12 page 13 page 14 page 16 page 18 page 24 page 25 page 26
Front cover: Participants in the recent ACB Spotlight meeting on demand management
Issue 597 | January 2013 | ACB News
4 |
General News
College’s Fifty Pathology Objects Launched
A new book, A History of Pathology in 50
Objects, has been launched by the Royal
College of Pathologists. The book was commissioned to commemorate the College’s
50th Anniversary, describing the objects chosen to celebrate the contribution that pathology has made to modern healthcare.
The objects are an eclectic mix including the light microscope, the frog, Lister’s Donkey
Engine and the organ donor card.
Dr Suzy Lishman, Vice-President of the
College and author of the book said that she was “grateful to College members and staff for nominating the objects they felt had made the greatest difference to patient care.
The final 50 were chosen to reflect the most important advances in pathology and the huge impact the specialty has had on the prevention, diagnosis and treatment of disease. Some of the objects will come as no surprise to the reader – the microscope, post-mortem instruments, the discovery of penicillin and ABO blood groups are all commonly associated with pathology. Some are less obvious – the book explains why the pea plant, paraffin wax, Blossom the cow and pigeon are also important.”
Dr Archie Prentice, President of The Royal
College of Pathologists explained that
“Pathology is a relatively young science.
The first pathologists dealt with all areas of the subject, but advances quickly meant that pathologists too became specialists. The Royal
College of Pathologists was established in 1962 to co-ordinate this development and maintain the internationally renowned standards and reputation of British pathology.” All Fellows of the College will receive a copy of the book with the January edition of the College
Bulletin. A limited number of copies are also available in return for a donation to the
College. Contact amaka.nwagbara@rcpath.org
for more details.
Sudoku
This month’s puzzle
Last month’s solution
ACB News | Issue 597 | January 2013
General News
| 5
Encourage Your New Trainees to Join the ACB
The Association continues to thrive only with the injection of new scientific blood into the organisation. If you are supervising newer Clinical
Scientists then it is you that is most likely to point to all the advantages of belonging to the ACB. These of course include all the local and national scientific meetings as well as our regular publications. On top of that is the important role of the
Federation in helping with workplace issues.
To help in this we have reproduced the ACB application form and guidance notes on page 26 of this ACB News.
Aberdeen Public Awareness Recognised
Helen Turner, Principal Clinical Scientist in
Aberdeen Royal Infirmary, was recently presented with the Royal College of
Pathologists Furness Prize for Science
Communication. Helen was awarded the prize in recognition of her ongoing work in raising public awareness of the importance of the contributions made by the pathology specialties to patient care. Her work has included annual public events at Satrosphere
Science Centre, Aberdeen, at which members of the public have the opportunity to carry out hands-on experiments, events for senior school pupils considering a career in healthcare science or medicine, and organising a series of public talks by prominent local scientists including a forensic pathologist, microbiologist and an expert on drug use in sport.
Speaking after being presented with her award Helen said, “It is an honour to win the
Furness Prize but thanks must also be given to all the staff within Laboratory Medicine who have helped make the National Pathology
Year events successful”. Dr Bernie Croal,
Vice President of the Royal College of
Pathologists, added, “2012 is the 50th
Anniversary of the founding of the College, and in addition has also been designated
National Pathology Year. As such, to win this communication prize against a strong competitive background of over 800 public engagement events taking place around the
UK is a particularly significant achievement.”
Helen Turner being presented with the Furness Prize by Dr Archie Prentice, College President
Lay Representative Neil Formstone
It is with great sadness that we announce the death of the Association’s Lay Representative,
Neil Formstone. Neil was a valued member of both Council and Executive and his contribution will be sadly missed.
Issue 597 | January 2013 | ACB News
6 |
General News
Haemoglobin is Harmonising to g/L
At their recent meeting in Birmingham the Department of Health’s Pathology Harmony group considered the implementation of the new units for haemoglobin and MCHC. The deadline for all clinical laboratories to report in g/L is set as 31st March 2013.
This important change harmonises an area of current clinical risk as presently UK Pathology reports in two different units which give results differing by a factor of 10 with a risk of misinterpreting results, especially those given urgently over the telephone. The Pathology
Harmony recommendation of moving to g/L has been agreed by the pathology professional groups working on the Pathology Harmony project.
Pathology Harmony is aiming to ensure all laboratories and their users are aware of this harmonisation. Key things that need to be considered locally by every laboratory still reporting in g/dL include:
Date at which you will change to the new units locally.
Putting in place the required IT changes to your laboratory computer and any links to your user’s computers. It is suggested that a standard comment is attached to all full blood count results for a 12 month period stating simply “Please note new units for haemoglobin and
MCHC”.
Laboratories are encouraged to seek any help they require from their IT suppliers and haematology analyser providers.
Point of Care Testing analysers that report haemoglobin, for example, blood gas analysers also need to be considered. Sometimes, these are not controlled by the Pathology
Department. Where this is the case it is important that those in charge of these analysers are made aware of the changes required.
Clinical Governance areas such as the clinical risk coordinators need to be involved with this change.
Speaking about this Dr Mike Galloway said, “It is vitally important that labs act locally to ensure that they have a plan to implement and communicate this important change”. The Pathology
Harmony website www.pathologyharmony.co.uk
includes a page of helpful information.
ACB News | Issue 597 | January 2013
General News
| 7
ACB Republic of Ireland Region Scientific Meeting
Education & Research Center
St Vincent’s University Hospital, Dublin
Friday 25th January 2013
09:30 Registration (Tea and Coffee)
09:50 Welcome by Myra O’Keane, Chair of ACB ROI Region
Chairperson: Ruth O’Kelly, Coombe Women’s and Infants University Hospital, Dublin
10:00 Update on High Sensitive Troponin
Dr Sean Cunningham, St Vincent’s University Hospital, Dublin
10:45 Cardiovascular Disease (TIA and Strokes) in the Elderly
Dr Diarmuid O’Shea, St Vincent’s University Hospital, Dublin
11:30 Demand Management
Dr Michael Ryan, Northern Health & Social Care Trust, Ballymena, Co Antrim and
Ms Ger Collier, Beaumont Hospital
12:45 Lunch: sponsored by Roche Diagnostics
14:00 INAB Accreditation – An Overview
Marie O’Mahony, Irish National Accreditation Board
14:45 INAB Accreditation – Laboratory Perspective
Ms Alison Bransfield, Bon Secours Hospital, Cork, Co Cork
15:30 Meeting Closes
16:00 Annual General Meeting (Members only)
CPD points are available for the meeting.
Registration is free for ACB Members,
€
10 for non-Members. Please register with m.okeane@svuh.ie or mstapleton@coombe.ie before 16th January 2013 for lunch numbers
Issue 597 | January 2013 | ACB News
8 |
General News
ACB & RCPath
Conference
Biochemical Endocrinology
Tuesday 5th March 2013
2 Carlton House Terrace, London
Aimed at those with an interest in Biochemical Endocrinology providing an update on a range of current analytical and clinical issues.
Chair: Miss Sarah Jarvis, Lanarkshire
09.30
Thyroid Hormone Standardisation – Are We Nearly There Yet?
Dr Graham Beastall, Glasgow and Dr Julian Barth, Leeds
10.30
Clinical Management of Acromegaly
Dr Claire Higham, Manchester
11.00
Refreshments
11.30
The Knows and Don’t Knows of Vitamin D
Professor Naveed Sattar, Glasgow
12.30
Lunch
13.15
Appropriate Investigation of Female Hyperandrogenism and an Update on PCOS
Dr Danielle Freedman, Luton
12.45
Clinical Uses of AMH
Professor Richard Anderson, Edinburgh
14.15
Interactive Case(s) from the Endocrine Clinic
Dr Danielle Freedman, Luton and Dr Kevin Deans, Aberdeen
14.45
Break
15.15
Debate: This House Believes that the Future of Hormone Measurements Lies with
Tandem Mass Spectrometry, not Immunoassay?
Speaking in favour of the Motion:
Dr Sandra Rainbow, London
Speaking against the Motion:
Dr Richard Chapman, London
Facilitator: Dr Kevin Deans
16.15
Close
Book online at: http://www.rcpath.org/meetings/book-now
Early bookings and online: RCPath/ACB Members/Fellows £205,
Concessions £102 (Trainees, Nurses, Retired, Students), Non-Members £255
Regular bookings: RCPath/ACB Members/Fellows £225,
Concessions £144, Non-Members £275
ACB News | Issue 597 | January 2013
General News
| 9
Waters LC-MS Source
Heaters Problems
MHRA Medical Alert -
MDA/2012083 Issued:
12th December 2012
The problem identified is that the ion block source heater can fail, potentially leading to inaccurate results which may not be picked up by quality control or internal standard monitoring. Assays with shorter dwell times are most affected, including neonatal screening for phenylketonuria, medium chain acyl CoA dehydrogenase deficiency and maple syrup urine disease.
The following products are affected:
Product Part number
Acquity TQD
Acquity TQD IVD
Quattro Micro
Acquity SQD
186003875
186003875IVD
VB-QMICRO
186003762
Quattro Premier XE 186003250
Quattro Premier M946430DC1
Xevo TQ
Xevo TQ IVD 1
Xevo G2 Tof
186004490
186004490IVD
186005597
The action plan with the company includes the replacement of affected parts by 14th January
2013. The duty of the laboratory is to determine if you have affected parts and if so to ensure it is replaced. If you determine you have been using a faulty heater then patient result review should be considered. See the
MHRA website for further details.
ACB Election of
Directors
Nominations are called for the following elected Directors. This notice updates the one published in the December ACB News.
Director of Finance
Director of Publications and
Communications (Company Secretary)
Director of Education, Training and
Workforce
Director of Scientific Affairs
Director of Clinical Practice
Director of Regulatory Affairs
These posts are for a maximum term of five years commencing at the AGM in 2013.
All the current Directors, with the exception of the Director of Publications &
Communications and the Director of
Regulatory Affairs, are eligible and willing to continue for a further term of office.
Nominations for these positions, duly countersigned should be made on the nomination form included on page 24 of this issue of ACB News and sent to:
ACB Administrative Office
130-132 Tooley Street
London
SE1 2TU.
Closing date: Friday 8th February 2013.
Coming Next Month . . .
Pathology Team Building on the Piste
Next month we will look at ways of fostering a team approach in pathology. From beekeeping, badminton and 5-aside football, to ski lessons followed by a lab ski trip to the Alps. If you have an idea for an article or some local news about your pathology environment you want to share, please contact the Editor.
Issue 597 | January 2013 | ACB News
10 |
General News
Pathology QA Review
A review of quality assurance arrangements for NHS pathology services has been announced by
NHS Medical Director
Professor Sir Bruce Keogh.
The review is led by National Clinical Director for Pathology Dr Ian Barnes. It will scrutinise
NHS arrangements for the oversight and safeguards of laboratory testing. The review will bring together experts in the field to explore how QA systems can be strengthened and how organisations can be more confident about the monitoring of the quality of care they offer the public. The review will report to the NHS Commissioning Board by the end of
2013.
Professor Sir Bruce Keogh commented that
“Around two million pathology tests are carried out by the NHS every day, and serious incidents are rare. However, concerns were raised at Sherwood Forest NHS Foundation
Trust in October about pathology testing of breast cancers, used to choose the best treatment for each patient, where the care of a small number of women was disadvantaged.”
Ian Barnes commented “This important work which will help to assure that the processes that govern laboratory testing are as strong as they can be”.
East of England Announces
Winners**
The successful bidders in the intra-NHS tendering process for GP Pathology have now been announced.
The winning organisations are now tasked with more detailed discussions with clinical commissioning groups to finalise requirements by a deadline of 31st March 2013.
So, four of five bids were successful.
Southend and Basildon Hospitals is not part of the new provider organisations.
Southend Echo Launches
Pathology e-Petition
Following the announcement of the four preferred providers of GP pathology testing in East of England the Southend Echo has launched a major campaign against the decision. A straw poll on their website showed 25,000 hits with 97% voting to keep
GP Pathology local. The newspaper has now launched an HM Government e-petition as follows:
East of England Winners**
Organisation
Consolidated Pathology Services
Eastern Pathology Alliance
Transforming Pathology Partnership
Includes
Luton & Dunstable, Bedford Hospital,
Princess Alexandra Hospital,
West Hertfordshire Hospital
James Paget – Great Yarmouth,
Queen Elizabeth Hospital – Kings Lynn,
Norfolk & Norwich
Cambridge, Colchester, East & North
Hertfordshire, HItchinbrooke, Ipswich,
Mid Essex, West Suffolk
Not a consortium Peterborough & Stamford Hospitals
ACB News | Issue 597 | January 2013
e-Petition Proposal
“The Echo newspaper is campaigning for blood testing to be kept in south
Essex. Regional Health Authority NHS
Midlands and East has decided Bedford is the best place to carry out analysis of pathology samples requested by GPs.
They will be sent by road from
Southend, Basildon and Castle Point to
Harlow first and then on to Bedford for screening. Results will then go to GPs.
You can now get blood tests back in a hour using the in house system at
Southend and Basildon Hospitals but under the new scheme it could take days, wasting valuable time. The Echo campaign asks for the pathology testing to remain within south Essex to provide the best service to patients. Sign to show your support for our campaign.”
The petition, requiring a verified email and address check, had nearly 1,000 signatures over the Christmas period. If it reaches
100,000 signatures then it will be considered for debate in the House of Commons.
General News
| 11
Issue 597 | January 2013 | ACB News
12 |
Council Matters
A Report from the ACB Council
Meeting, November 2012
Ruth Lapworth, ACB Secretary
National School of
Healthcare Science
Boards in areas such as curricula, training the trainers, assessment and quality assessments of training departments to ensure that our current standards are maintained.
The first topic of the day was the National
School of Healthcare Science. Val Davison gave an update on progress made during the year.
She described the governance arrangements and structure of the School including the seven themed boards. The aim is for all funding to be top sliced and training commissioned nationally. A great deal has been done on working with trainees including focused workshops, leadership training, national trainee events, formal introduction to the School, general information about
Modernising Scientific Careers (MSC), the assessment strategy and QA of training environments. The aim is to standardise training and work based assessments to ensure consistency across healthcare sciences with an outcome of excellent educational standards, a competent and capable workforce of adaptable and flexible staff. It is therefore important for organisations such as the ACB to work with the School by engaging with the
Labs are Vital
The second topic was devoted to Labs are Vital and the role of the pathology Champions.
The role of a pathology champion who can influence decision making at a local level was devised under the LRV initiative. The need for this role with the advent of pathology commissioning and other initiatives is thought to be of increasing importance. Everyone needs to interact with colleagues outside the four walls of the laboratory and the Trust so that the importance of laboratory medicine is appreciated in delivering effective integrated patient care. It was agreed that the work the
ACB is doing in connection with this initiative should continue under the LRV banner.
However, the likely emergence of the
Pathology Alliance as a common voice for pathology may mean that this work sensibly transfers and continues under this banner in future.
Council Executive at their December meeting
ACB News | Issue 597 | January 2013
A Personal View
| 13
East of England Moves on to Middle England
A Personal View from Three Senior Staff in the East of England
We read the article on Middle England GP
Pathology in the October edition of ACB News with interest. We would like to expand upon the article on the East of England Pathology
Transformation Project in the November issue as the East of England experience foreshadows what is about to happen in the East and West
Midlands.
The EoE SHA was never renowned for an interest in pathology matters until it decided to transform pathology along the lines of the
DoH’s interpretation of the Carter Report about three years ago. Naturally the SHA avoided contact with anyone from NHS pathology at that stage and came up with a three laboratory plan for Bedfordshire,
Cambridgeshire, Essex, Hertfordshire, Norfolk and Suffolk. The three hubs were yet to be determined, but at the first meeting open to pathologists and before the open PQQ phase we were told they would be, “Norwich,
Cambridge and one other”. This set the tone and at meetings with the SHA ‘experts’ you could guarantee that the one person in the room who knew least about the subject was from the SHA. This even extended to KPMG who were facilitating the process, but who got the geography of the region wrong. Deadlines were always fixed for the labs but flexible for the SHA mainly due to reality checks.
service at the Lister’s sister hospital, the QEII in
Welwyn, despite the presence of an A&E and
ITU on site.
Is this then an exemplar for the East and
West Midlands to follow? EoE has seen three years in which some trusts have vainly committed themselves to long-term leases on equipment to prevent being reduced to spoke status. Three years in which consultant posts have been left unfilled and then abolished, including posts at Addenbrooke’s,
Hinchingbrooke, West Suffolk, Norwich, Great
Yarmouth and Chelmsford. This has left several hospitals with only occasional consultant cover; a situation that CPA appears content with. The human impact on senior staff has been tangible with evidence of stress-related sickness during the past year. As for the Royal
College of Pathologists, they have said little during the process. As a result several of the remaining Consultant Chemical Pathologists in the region have left the Royal College of
Pathologists in protest.
These are our personal reflections on what we have been through. Importantly to others this is the background to the ‘commissioning toolkit’ developed by the Cambridge SHA office, with money from the Pathology
Director at the Department of Health. Now several of the key EoE SHA players move on to reprise their roles on a grander stage in cities such as Nottingham, Leicester, Stoke and
Birmingham.
Staff Moving On
If the current plan goes ahead, GP pathology from Stevenage will go to Serco at Bedford while the non-urgent work will go to
Addenbrooke’s Hospital, leaving only a hot lab at the Lister Hospital. Will this mean three different reference intervals? Will all the results get onto one database? Laboratory staff are not waiting to find out and staff shortages mean that from 1st December 2012 there will be no out of hours laboratory
Articles in ACB News are never published unless authorship accompanies articles when submitted. This article has been written by senior staff from three hospitals in the East of England. The Editor has received other comments about the EoE tender process anonymously which he has felt unable to publish.
Issue 597 | January 2013 | ACB News
14 |
Practice FRCPath Style Calculations
Deacon’s Challenge
No 140 - Answer
You have been asked to check the calibration of your laboratory’s spectrophotometer. Using a solution of potassium dichromate (50.0 mg/L) in dilute sulphuric acid, you obtain absorption values of 0.523, 0.521, 0.524 and 0.523 at 350 nm. The absorptivity index of potassium dichromate at this wavelength is 10.7 ± 0.11 Lg -1 cm -1 . Given you have used cuvettes with a pathlength of 1 cm, calculate the probability that the spectrophotometer is correctly calibrated.
FRCPath, Autumn 2011
First calculate the expected absorbance ( A ):
A = e x c x l
Where e = absorptivity index = 10.7 L.g
-1 cm -1 c = concentration in g/L l = pathlength = 1 cm
Since the concentration is given in mg/L it must first be converted to g/L to be compatible with e :
Therefore
Concentration (g/L) = 50 mg/L = 0.05 g/L
1000
A = 10.7 x 0.05 x 1 = 0.535
Next calculate the mean and standard deviation ( s ) for the set of absorbance readings ( x ): x x 2
SUM: 2.091
1.093075
Mean =
Σ x = 2.091
= 0.523 (to 3 sig figs) n 4 s 2 = x 2 – (
Σ x ) 2 / n = 1.093075 – (2.091
2 )/4 n - 1 4 - 1
=
0.523
0.521
0.524
0.523
0.273529
0.271441
0.274576
0.273529
s =
1.093075 – 1.0930703
= 0.0000047
= 0.000001567
3 3
√
0.000001567
= 0.00125 (to 3 sig figs)
ACB News | Issue 597 | January 2013
Practice FRCPath Style Calculations
| 15
Calculate t , with n -1 degrees of freedom, to compare the observed mean with the target value of
0.535: t = Target mean – measured mean = (Target mean – Measured mean) x
√ n s /
√ n s
= (0.535 – 0.523) x
√
4 = 0.012 x 2 = 19.2
0.00125
0.00125
From tables, when t = 19.2 with n -1 (i.e. 3) degrees of freedom, the probability that the difference in mean absorbances arose purely by chance is less than 0.001.
Therefore the probability that the instrument is correctly calibrated is less than 0.001.
Ideally an alternative t -test should be used which allows for the imprecision of the absoptivity index. However, this is not practicable since it is not clear if the quoted figure of ±0.11g
-1 cm -1 is a variance, standard deviation or standard error. Furthermore, the number of observations on which it is based ( n ) is not given.
Question 141
The symptoms of ovarian cancer are non-specific. The prevalence of ovarian cancer in symptomatic women who present in general practice is 0.23%. If the sensitivity and specificity of CA 125 for detecting ovarian cancer are both 78%, calculate the post-test probability of disease given a positive result.
If the prevalence of ovarian cancer in women who carry the brca1 oncogene is approximately
15%, what would be the post-test probability of disease?
FRCPath, Autumn 2011
Issue 597 | January 2013 | ACB News
16 |
Current Topics
From Biomarker to Medical
Test
Dr Phillip Monaghan, The Christie Hospital, Manchester
Meeting of the European
Federation of Clinical
Medicine and Laboratory
Medicine (EFLM) Working
Group on Test Evaluation
(WG-TE), 15th-16th
October 2012, Dubrovnik
The venue on the Adriatic provided a stimulating atmosphere in which to exchange ideas and develop new strategies for the evaluation of medical tests. In this time of austerity, justification of costs associated with the introduction of new laboratory tests should ideally be based on demonstration of proportional benefits to patients. New laboratory tests are often released to market with limited supporting evidence regarding their value or impact in clinical practice.
Test evaluation should be performed with informed and carefully devised study design, yet evidence-based methodology is often lacking in the scientific literature, and when available is often poorly understood. As a consequence, inadequately designed evaluation studies may lead to erroneous clinical decision making that threatens patient safety. The Science Committee of the EFLM has established the test evaluation working group with the aim of developing a framework of guidance for the appropriate evaluation of new laboratory tests. They aim to develop practical tools to support the design and conduct of test evaluation studies and to aid training and education.
The Working Group
The Group is a joint collaboration between the
EFLM and AACB (Australasian Association of
Clinical Biochemistry). Membership represents collaboration between experts in evidencebased laboratory medicine, evidence-based diagnosis and epidemiology, and R&D of IVD industrial partners. However, until recently, the involvement of young scientists in the activities of the EFLM has been limited.
In order to boost the role of young scientists the executive board invited nominations for young scientist appointments on each of their working groups and after nomination by the
ACB, I was successfully appointed to the
Group. My first meeting was this two-day conference. Day one was devoted to discussing the key principles and components of the test evaluation process, and day two comprised brainstorming sessions on the development of new guidance for critical elements of the devised test evaluation framework.
Key Principles
We launched into the finalisation of the
Scoping Paper which aims to set out how exactly test evaluation should be done when a new biomarker is discovered. This is taking the form of a test evaluation framework to provide an evidence-based approach to study design, thus setting standards for test evaluation in the research and clinical setting, forming guidance for researchers, clinicians
ACB News | Issue 597 | January 2013
Current Topics
| 17 and laboratory professionals. The Group came to consensus on a number of key definitions and additionally finalised a figure for the scoping paper to clearly illustrate the key components of the test evaluation framework and how each element interacts in the cyclical test evaluation process. We concluded this session by agreeing on a set of example laboratory tests with different purposes
(e.g. screening, diagnosis and monitoring) for which we could generate and apply key questions and criteria for identifying unmet clinical needs in current clinical pathways.
Critical Elements
An 8 am start signified a busy day ahead and the group continued on the theme of developing and testing questions and criteria for identifying unmet clinical needs and addressing ways of analysing how a new test would fit into an existing clinical pathway.
As the “youngest” I was delegated the task of scribe for the ensuing brainstorming session. With my flip-chart at the ready we began to draft key questions, using the test examples agreed the day before, for the identification of unmet clinical needs. By defining the source of limitations in current practice we were able to establish opportunities for process improvement. This strategy was applicable to tests with different purposes and the group concluded that this principal phase of test evaluation was to be an immediate focus of attention for the group in elaborating the proposed test evaluation framework.
The afternoon session looked at establishing clinical performance criteria for medical tests, an aspect of test evaluation for which there is a paucity of methodological criteria in the literature. The group discussed novel ideas on grading clinical performance, including how to express clinical performance criteria through a hierarchical approach with proxy outcome levels. With clinical performance in mind, we looked at the aim of various test roles
(e.g. triage, add-on tests) and addressed the clinical performance criteria in each particular scenario whilst contemplating the various modifiers that may impact overall clinical performance and what study design application to best evaluate a particular testing scenario. We rounded off the meeting by approaching the difficult question of setting predefined values for quantifying clinical performance standards for new medical tests analogous to criteria available for analytical specifications. This final session generated some interesting novel ideas which the WG-TE will now develop and refine as part of the test evaluation framework.
I found my first meeting a highly enjoyable and educational experience. This appointment has given me the opportunity to collaborate with colleagues from Europe and beyond and I came away from this meeting filled with enthusiasm and excitement at what the
WG-TE will achieve and contribute to the field of test evaluation.
For more information on the EFLM’s WG-TE please visit: http://efcclm.eu/science/wg-testevaluation
Issue 597 | January 2013 | ACB News
18 |
Meeting Reports
Laboratory Medicine at the
Clinical Interface
Dr Sarah Glover, Bradford
Following the successful inaugural European
Federation of Clinical Chemistry and
Laboratory Medicine (EFLM) and the European
Union of Medical Specialists Board of Medical
Biopathology (UEMS) Meeting in Lisbon in
2010, the city of Dubrovnik was chosen to host the second meeting Laboratory Medicine at the Clinical Interface in collaboration with the
Croatian Society of Medical Biochemistry.
Dubrovnik with its Old City, a UNESCO World
Heritage Centre, is certainly one of the most beautiful cities in Europe, whilst the conference venue itself, Hotel Rixos, provided a stunning backdrop with spectacular views over the Adriatic.
The major focus of the meeting was the link between the clinician, GPs and the laboratory.
The meeting included classic plenary lectures, parallel symposia, posters and interactive pro-contra sessions with plenty of lively debate.
Predicting Outcomes in the
Critically Ill
The opening ceremony included a Key Note
Lecture by Velimir Sri (Professor of
Management, University of Zagreb) on the management of change. We were reminded of how technological changes in the last 20 years have drastically altered the way we live and work. Whilst change in laboratory medicine is certain, the exact nature of these changes may be unknown. However, the responsibility for implementing change for patient benefit lies with us all. The opening ceremony concluded with the Croatian Music Society St Cecilia performing a Moreška, a knightly sword dance originating from around the 12th century.
Geoffrey Baird (USA) kicked off the session on predicting the outcome in critically ill patients, with a discussion on the use of ionized and pH corrected calcium in ICU patients. Members of the audience were thankful for the technological advances which have been made since the first measurements of ionized calcium, made using an isolated frog heart! A lack of guidelines for the routine monitoring of calcium in critically ill patients frequently results in over requesting. Dr Baird highlighted the need for responsible requesting and demonstrated no adverse outcome of reduced calcium testing and reduced calcium gluconate treatment in certain ICU patients. Jack Ligtenberg
(The Netherlands) covered glucose regulation in ICU patients, describing how tight glycaemic control, although difficult to achieve, effectively reduces morbidity and mortality, with little evidence of any severe adverse effects of hypoglycaemia. Georg-
Christian Funk (Austria) covered the use of lactate guided therapy. Lactate is an excellent prognostic marker in ICU patients and is superior to cardiac output in predicting outcome in patients with haemorrhagic shock.
A lunchtime workshop looked at the role of newer biomarkers for preventing and monitoring of renal disease. Stefan
Herget-Rosental (Germany) discussed the use of Cystatin C in detecting and monitoring of early stage diabetic nephropathy. Olaf Stanger highlighted the value of NGAL in the detection of kidney injury following cardiac surgery. NGAL reflects acute epithelial damage and peaks within hours of surgery, so can be used as an early marker for the identification of patients who will require dialysis.
Presentations by Ron van Schaik (The
Netherlands) and Philip Quirke (UK) guided the audience through the pros and cons of pharmacogenetics in predicting anti-cancer therapy response. A healthy debate led to the conclusion that whilst pharmacogenetics currently has a limited impact upon treatment decisions, it holds great potential. Further research, specifically, random controlled trials,
ACB News | Issue 597 | January 2013
Meeting Reports
| 19 is needed before pharmacogenetics becomes routine practice.
Esa Sioni (Finland) looked ahead at the use of mobile technology within laboratory medicine. The audience was guided through the use of wirelessly connected devices in each step of the total testing process, from specimen collection in tubes with radiofrequency identification tags to issuing of reports directly to clinicians and/or patients on mobile devices.
Laboratory Genetics in Practice
An interesting session on laboratory genetics was given by Sian Ellard (UK), Kate Thomson
(UK) and Joep Defesche (The Netherlands).
Dr Ellard described the use of targeted next generation sequence analysis in patients with neonatal diabetes or maturity onset diabetes of the young, in whom the cause is unknown.
The benefits and challenges of molecular genetic testing in the setting of inherited cardiomyopathy were discussed by
Dr Thomson. Dr Defeche completed the session describing how genetic testing for familial hypercholesterolaemia fits alongside family history, clinical presentation and routine laboratory findings.
Stephen Halloran (UK) and Wendy Atkin
(UK) led a pro-contra session on screening for bowel cancer but rather than providing opposing views, the presenters discussed how laboratory and endoscopic screening both have an important role to play. Professor
Halloran detailed the success and experience gained from setting up and running the NHS
Bowel Cancer Screening Southern Programme
Hub. The use of faecal immunochemical tests
(FIT) was also discussed. Dr Atkin summarised the pros and cons of colonoscopy and flexible sigmoidoscopy in bowel cancer detection and treatment.
The final morning included a session covering pre- and post-analytical aspects, which proved very popular. Aasne Aarsand
(Norway) presented some examples of how
EQA can be used to help assess the total testing process, for diseases with complex diagnostic testing e.g. porphyrias.
Such schemes can be used to highlight where improvements can be made in the pre-analytical, analytical and post-analytical phases. Ana-Maria Šimundi discussed how laboratories need to take greater responsibility for assessing quality indicators for the pre-analytical phase, to ensure the service we provide is continually improved and meeting the needs of our users. Quality indicators are important tools but data collection without corrective actions does not lead to service improvement.
The meeting was rounded off with a session on approaching malnutrition from the laboratory point of view. Walter Nützenadel
(Germany) described how laboratory tests are used in failure to thrive (FTT) in childhood.
Dr Nützenadel discussed how routine biochemical tests can give clues to support a clinical suspicion of FTT, whereas specific tests may be useful in making a diagnosis e.g.
coeliac disease, cystic fibrosis. Alastair Forbes
(UK) discussed malnutrition from an adult perspective. Professor Forbes highlighted the importance of nutrition screening tools, although these rarely include biochemical data. The role of the laboratory is primarily in monitoring patients during refeeding or whilst on long term parenteral nutrition.
Sarah was able to attend the meeting using the bursary from winning last year’s
Geoffrey Walker Award.
Issue 597 | January 2013 | ACB News
20 |
Meeting Reports
Showcasing Demand
Control Initiatives
Emma Connell, Croydon University Hospital and Laura Tooth, St George’s
Healthcare NHS Trust
The ACB Spotlight Meeting held at the Royal
Colleges of Pathologists in October focused on the topical problem of managing increasing demand for laboratory testing in the lean post-Carter era. Demand management strategies have become a priority for many
Trusts in order to cut costs in the face of increasing workloads, with the 2008 Carter review of UK pathology services reporting that up to £500 million could be saved per year.
The meeting was convened by Dr Stuart
Smellie and Professor Tony Fryer, on behalf of the Clinical Practice Section of the ACB.
Both organisers are active locally and nationally in pathology benchmarking exercises and in promoting appropriate test requesting. The challenges of demand management and successful initiatives for overcoming them were discussed, and the audience were kept ‘on their toes’ with a series of interactive votes!
Dr Smellie started the day with an overview of demand management. The options discussed included changing the content of test profiles (e.g. removing GGT from the liver function test panel), management at the point of electronic requesting, targeted knowledge initiatives and using benchmarking as a facilitator. Many managers, however, have unrealistic expectations as to how much can be saved, which will be dependent on how efficient the laboratory is to begin with.
Under-requesting is also a problem in some areas e.g. measurement of CK pre-statin treatment and screening for chlamydia in the under 25s. It is therefore important not just to reduce the number of tests requested but to ensure there is an evidence-based approach to testing.
Tony Fryer spoke next about developing a demand management strategy and assessing its effectiveness. He started by expressing his
ACB News | Issue 597 | January 2013
Meeting Reports
| 21 concern over the lack of current publications on this topic and urged the audience to share their experiences and knowledge.
Benchmarking data show an inconsistent picture across laboratories, but these data has also driven standardisation. Questioning of the audience showed that 71% agreed that all laboratories should develop a demand management strategy, although interestingly
29% disagreed. Four phases of strategy development were discussed: defining the scale of the problem, changing behaviour through GP master classes, spreading the news through publications and regional demand management forums and finally structuring the approach and formulating an over-arching strategy. A demand management toolkit written by Tony Fryer and Stuart Smellie will be published later this year.
Over Diagnosis from Over Testing
After a short break Danielle Freedman posed a series of questions to the audience. The major reasons for test over-utilisation were thought by those present to be junior clinicians’ lack of knowledge and training, duplicate requesting, a ‘tick-box’ culture, pressure from the patient and even fear of litigation. Danielle estimated that around 30% of tests carried out are unnecessary, with a risk of over-diagnosis in healthy people and an increase in further invasive investigations or hospital referrals, anxiety and hospital length-of-stay. She highlighted data from the NHS Atlas of
Variation showing significant variation in GP test requesting nationwide. Work carried out at the Luton and Dunstable Hospital using the
OrderComms system as a two-way process to manage demand was presented, with medical and surgical clinical test profiles, duplicate request rules, hyperlinks to resources such as bettertesting.org.uk, test costs and diagnostic algorithms all available to the requesting clinicians.
The last speaker before lunch was Dr Tim
Lang. Dr Lang spearheaded the national minimum re-testing intervals (MRIs) project with the ACB Clinical Practice Group, the consensus results of which are soon to be published. He discussed how these guidelines were assembled and emphasised the importance of keeping your clinicians on-board with implementation of duplicate request rules. An audience poll showed that
68% of labs represented at the meeting have duplicate rules, with 95% being prepared to implement them if they haven’t done so already.
Borthwick’s Approaches
After an excellent lunch on the sunny balcony at the College we returned to Hazel
Borthwick’s demand management approaches at her hospital, where currently inpatient and outpatient testing is requested on paper forms. She highlighted what is possible with paper requesting, with condition-led test profiles and a re-design of the A&E request form to hopefully vanquish the ‘tick-box’ culture. This process was led by a small team, including consultant A&E staff. Jenna Waldron from the Royal Wolverhampton then discussed the local approach pre-, within- and postlaboratory, again emphasising the importance of face-to-face discussions with clinicians and
GPs in development of condition-based test profiles and diagnostic algorithms. The work of the ACB West Midlands Demand
Management Forum in beginning to standardise test requesting practices across the region was mentioned.
Next there was an opportunity for general discussion, with the panel of speakers taking questions from the audience. There was concern about focusing purely on driving down test requesting and losing sight of the
‘bigger picture’ – for example, it was mentioned that adding magnesium to bone profiles will pick up many cases of clinically significant hypomagnesaemia. The difficulties in quantifying certain savings were also discussed e.g. avoiding admissions to A&E or referral to outpatients by doing the correct tests in primary care. Another difficulty in the estimation of savings occurs when increased laboratory costs lead to significant cost reductions in other hospital departments. For example, faecal calprotectin testing costs the lab more money but can prevent unnecessary endoscopies.
Issue 597 | January 2013 | ACB News
22 |
Meeting Reports
GP Test Standardisation
The final session of the day consisted of case presentations from Gethin Roberts and Soha
Zouwail, both from the Welsh region. Gethin spoke about establishing a national strategy for MRIs using the All Wales LIMS and Welsh
Clinical portal. This is currently being implemented and involved reviewing the existing MRIs across 4 hospital laboratories and agreeing consensus MRIs for 25 assays. These rules were then configured in LIMS to trap duplicates when tests were requested on paper. For electronic requests, the previous result was shown to the requester who was then asked if they still wished to continue.
Soha went on to showcase her work on standardising test requesting from GP practices served by her laboratory. This involved monthly summarising of GP testing, together with cost information. The GP practices were named and outliers have now expressed an interest in changing their requesting patterns. The laboratory has been involved in this process, and the ACB Venture publication ‘Primary Care and Laboratory
Medicine’ was also used. After interactive voting, Dr Zouwail’s presentation was voted the most useful of the session, although both speakers received prizes.
Tony Fryer then closed the day with some more audience questions to identify which demand management strategies were currently used in laboratories Only 34% of the laboratories represented in the audience had made changes to routine test profiles during the last year, but 84% of the laboratories represented had been involved in developing local guidelines on appropriate testing. The meeting was highly insightful and gave people lots to think about for improving demand management in their own laboratories. This topic is likely to become the subject of a Royal
College KPI in the future and will need to be prioritised by clinical scientists and medical staff managing laboratories.
Advertisement
Serum Fructosamine Report
Hull and East Yorkshire Hospitals
NHS Trust
Glycaemic Assessment Service
This service has been established to provide a referral and interpretative service for samples from patients where there is concern regarding a possible inconsistency between their markers of glycaemia, such as HbA1c and either their clinical picture or other assessments of glucose control.
Currently, part of the service includes measuring HbA1c by affinity chromatography, which is a method more able to take account of abnormal haemoglobins than traditional HPLC means of analysis.
The service can also measure serum Fructosamine by a novel enzymatic method. An individualised report is issued giving the range of HbA1c values which would be expected from the
Fructosamine result in order to help establish if the measured
HbA1c is consistent with this independent measure of glycaemia or not.
Users of the service also have access to further advice regarding the interpretation of difficult cases through the service team headed by Professor Eric Kilpatrick.
Further details of cost and specimen requirements can be found at: www.assayfinder.com
under the relevant test name.
Fructosamine : 420
µmol/L (reference interval* 122-236)
Fructosamine** of 420 µmol/L predicts an HbA1c*** of 77-92 mmol/mol (9.2-10.6%)
* 466 non-diabetic, non-pregnant 20-60 year olds
** using a platform-independent enzymatic assay (Randox)
*** using a Menarini/Arkray HA-B160 HPLC assay
USER
Your patient shown in a distribution of 269 non-pregnant patients with diabetes
ACB News | Issue 597 | January 2013
Meeting Reports
| 23
Outbreak Sessions in
Liverpool
Marc Niebel, Trainee Clinical Scientist, Glasgow
The joint Federation for Infection Societies and
Healthcare Infection Society conference in
Liverpool took place last November. The conference was attended by over 800 delegates covering a wide variety of areas which included infection prevention and control, infectious diseases, surveillance and epidemiology. Sessions were structured as lectures for all, parallel sessions and debates with poster walks organised in the evening to see some of the approximately 350 posters being presented at this conference.
The conference started with a session on multi-drug resistant gram negative infections which included an interesting and succinct overview given by Professor Rossolini into the epidemiology of MDR gram negative organisms, for example the rise of carbapenem resistant Klebsiella pneumoniae.
A lecture looking at faecal transplantation in patients with recurrent CDI showed that this could be a viable option with a reported success rate of
92-93%, although cost could be inhibitory.
Contaminated Privacy Curtains
A debate on antimicrobial prophylaxis for infective endocarditis focused on contrasting views towards prophylaxis in accordance with the NICE Guidelines published in 2008.
A session on the optimal use and value of antibiotics included a fascinating lecture on the economics behind antibiotic management with strategies to improve antibiotic therapy.
This included switching from intravenous to oral treatment and the use of outpatient parenteral antimicrobial therapy which showed in a recent evaluation to lead to significant reduction in treatment costs.
On the final day I attended the outbreak sessions which discussed numerous topics, including an interesting case of group A streptococcus from an index case with necrotising fasciitis being transmitted to another patient via contaminated privacy curtains.
New Vaccines
A session on future vaccine development included the evaluations of numerous
Neisseria meningitidis serogroup B vaccines which recently has led to the first vaccine,
4CMenB to be recommended for approval by the European Medicines Agency. This is currently being considered by the Joint
Committee on Vaccination and Immunisation for implementation into the routine childhood immunisation schedule. A free papers session on infection control and clinical microbiology included a presentation of particular interest where a dry mist hydrogen peroxide system was used instead of a chlorine-based cleaning agent to decontaminate healthcare environments following norovirus outbreaks.
Issue 597 | January 2013 | ACB News
24 |
Council Nomination Form
Association for Clinical Biochemistry
Council Nomination Form 2013
Election of Directors of the Association for Clinical Biochemistry
We, the undersigned, being Members* of the Association nominate
Name ………………………………………...........................................…………………………………….
Address ………………………………………...........................................…………………………………….
………………………………………...........................................…………………………………….
for election as **
Director of Finance
Director of Publications and
Communications (Company Secretary)
Director of Education, Training and
Workforce
Director of Scientific Affairs
Director of Clinical Practice
Director of Regulatory Affairs according to Articles 11 and 14 as outlined in Bye-Law 6, subsections 6.2 and 6.3 of the Articles of the Association.
Name 1. ……………………………
Capitals
………………………………………….
Signature
Name 2. ……………………………
Capitals
Name 3. ……………………………
Capitals
………………………………………….
Signature
………………………………………….
Signature
I am willing to undertake the duties and responsibilities of this office if elected.
……………………………
Signature
………………………………………….
Date
* Every Member other than a Corporate, Retired, Temporary Retired, Temporary, Federation,
Affiliate or Student Member shall have one vote and is therefore entitled to support a nomination. Federation Members can nominate and vote for the election of the Director of
Regulatory Affairs. Only Ordinary Members are eligible to hold office.
** Please clearly circle the post you are nominating.
This form, duly countersigned, to be returned to
The Administrative Office, Association for Clinical Biochemistry,
130-132 Tooley Street, London SE1 2TU, before 8th February 2013
ACB News | Issue 597 | January 2013
Crossword
| 25
ACB News Crossword
Set by Rugosa
Well done to everyone who has submitted a winning entry for the Townsend Christmas
Crossword. Pots of fine English honey are on the way to you. If you would like a pot as well then why not try your hand at this puzzle set by Rugosa.
Last month’s solution
Across
8 Generally dissipated, all lacking get-up-and-go (6)
9 User's software sorted index for supplement (8)
10 Metal press (4)
11 Immunity potentially increases with time (10)
12 In opposition in Santiago (4)
13 A 19 that contributes to 11 (5,5)
17 Web medical thesaurus (4)
18 Musical tonic (5)
19 Rejection of French computer terminal (4)
21 Incorrect initiation of cooking alters fats (5,5)
23 Smooth uniform (4)
24 Uriah consumed a meat pie, developed renal tract problem
(10)
28 Pelt shelter (4)
29 Synthesis of first stable enteric hormone (8)
30 Clinic ignored unusually inconclusive blood type (6)
Down
1 Transport access (8)
2 Ostentatiously displays meals for constipation? (10)
3 Power plant destruction degradative chemical process (10)
4 Grammar school boxing scars (4)
5 Copies some tapestry (4)
6 Christian name within? (4)
7 Nutrient from hopeless
Phoenician cook (6)
14 Toast the singer (5)
15 Have incorporated travel arrangement for circulation director (5,5)
16 Lash out with anger and name
German pathologist (10)
20 Terrible doctor deaf about upstart trainee (8)
22 Surprised at promotion about two-dimensional puzzle (6)
25 Further traditional customs without point (4)
26 Carry course calculator (4)
27 Closed chain gang (4)
Issue 597 | January 2013 | ACB News
26 |
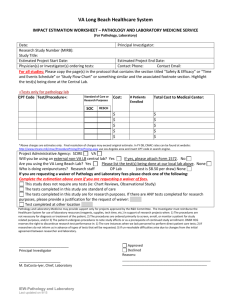
Application for Election to Membership
ACB News | Issue 597 | January 2013