PHYSICAL THERAPY CARE PLAN
advertisement

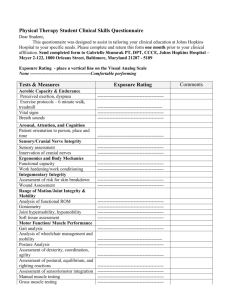
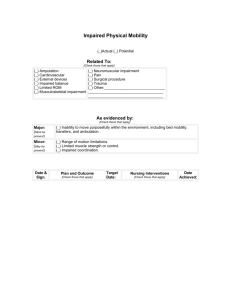
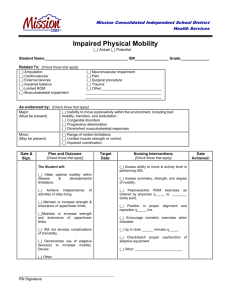
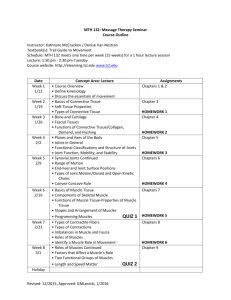
INITIAL UPDATED PHYSICAL THERAPY CARE PLAN Diagnosis/ Reason for PT: Frequency and Duration: ONSET: If applicable, portion of Plan of Care assigned to a PTA was discussed, explained to the PTA: Yes INTERVENTIONS No N/A Locator #21 Evaluation Balance training /activities Teach hip safety precautions Establish/ upgrade home exercise program Pulmonary Physical Therapy Copy given to patient Ultrasound to _____ at _____ x _____ min Teach safe/effective use of adaptive/assist device (specify) Copy attached to chart Electrotherapy to _____ for _____ min Teach safe stair climbing skills Patient/Family education Prosthetic training Teach fall safety Therapeutic exercise TENS to _____ for _____ min Pulse oximetry PRN Transfer training with/without assistance Functional mobility training Heat/Cold to _____ for _____ min Gait training with/without assistance Teach bed mobility skills Therapeutic massage to _____ x _____ min OTHER INTERVENTION/TREATMENT: Note: Each modality specify frequency, duration, amount and specify location: LONG TERM GOALS SHORT TERM GOALS Locator #22 .p n SA sy M ste PL m E .co m GENERAL GENERAL Gait will increase tinetti gait score to _____ / 12 within ______ weeks. Gait will increase tinetti gait score to _____ / 12 within ______ weeks. Will improve gait requiring ____ to _____ from _____ to ______ within ____ weeks. Will improve gait requiring ____ to _____ from _____ to ______ within ____ weeks. BED MOBILITY BED MOBILITY Pt. will be able to turn side (facing up) to lateral (left/right) within ____ weeks. Pt. will be able to turn side (facing up) to lateral (left/right) within ____ weeks. Pt. will be able to lie back down within _____ weeks. Pt. will be able to butt scoot within _____ weeks. Pt. will be able to sit up independently _______ within ______ weeks. Pt. will be able to sit up with/without assistance _______ within ______ weeks. Pt. will be able to self reposition within ______ weeks. BALANCE BALANCE Will increase tinetti balance score to _____/16 within _____ weeks. Will increase tinetti balance score to _____/16 within _____ weeks. Pt. will be able to reach steady static/dynamic sitting/standing balance Pt. will be able to reach steady static/dynamic sitting/standing balance with/without assistance ______ within ______ weeks with/without assistance ______ within ______ weeks TRANSFER TRANSFER Pt. will be able to transfer from _________ to _________ with/without assistance Pt. will be able to transfer from _________ to _________ with/without assistance _____ within ____ weeks. _____ within ____ weeks. STAIR/UNEVEN SURFACE STAIR/UNEVEN SURFACE Pt. will be able to climb stair/uneven surface with/without assistance _____ steps # Pt. will be able to climb stair/uneven surface with/without assistance _____ steps # _______ within ________ weeks. _______ within ________ weeks. MUSCLE STRENGTH MUSCLE STRENGTH Pt. will be able to hold weigh _______ lb within ________ weeks. Pt. will be able to hold weigh _______ lb within ________ weeks. Pt. will be able to oppose flexion or extension force over _____ within ______ weeks. Pt. will be able to oppose flexion or extension force over _____ within ______ weeks. PAIN PAIN Pain will decrease from ____/10 to ____ /10 within _______ weeks. Pain will decrease from ____/10 to ____ /10 within _______ weeks. ROM Pt. will increase ROM of ________ by ______ degrees flexion/extension within _____ weeks. w w w ROM Pt. will increase ROM of ________ by ______ degrees flexion/extension within _____ weeks. SAFETY SAFETY Pt. will be able to use _____ independently to _____ feet within ______ weeks. Pt. will be able to use _____ with/without assistance to _____ feet within ______ weeks. Pt. will be able to self propel wheel chair _____ feet within _______ weeks. Pt. will be able to propel wheel chair _____ feet within _______ weeks. HEP will be established and initiated. Pt will be able to finalize and demonstrated to follow up HEP. Locator #22 ADDITIONAL SPECIFIC THERAPY GOALS Note: Each modality specify location, frequency, duration, and amount. Patient Expectation SHORT TERM Time Frame LONG TERM DISCHARGE PLANS DISCUSSED WITH: Patient/Family Physician Other (specify) Care Manager CARE COORDINATION: MSW Aide PTA REHAB POTENTIAL: Physician Other (specify) Poor Fair OT Good Equipment needed: Patient/Caregiver aware and agreeable to POC: Plan developed by: Physician signature: SN Time Frame APPROXIMATE NEXT VISIT DATE: PLAN FOR NEXT VISIT ST Excellent Yes No (explain): Date Therapist Name/Signature/title Date Please sign and return promptly, if applicable Original - Patient Chart Copy - Patient's Home Chart PATIENT NAME - Last, First, Middle Initial ID# PHYSICAL THERAPY Cruz & Sanz Health Services, Inc. EVALUATION TIME IN HOMEBOUND REASON: Needs assistance for all activities Residual weakness Requires assistance to ambulate Confusion, unable to go out of home alone Unable to safely leave home unassisted Severe SOB, SOB upon exertion Medical restrictions Dependent upon adaptive device(s) Other (specify) Evaluation Ultrasound Therapeutic Exercise Electrotherapy Transfer Training Prosthetic Training Muscle Re-education / DATE OF SERVICE OBJECTIVE DATA TESTS AND SCALES PRINTED ON OTHER PAGE. PT ORDERS: RE-EVALUATION OUT TYPE OF EVALUATION Initial Interim SOC DATE / / Final / (if Initial Evaluation, complete Physical Therapy Care Plan) Home Program Instruction Other: Gait Training Chest PT PERTINENT BACKGROUND INFORMATION TREATMENT DIAGNOSIS/ PROBLEM ONSET / / MEDICAL PRECAUTIONS: Fractures Cardiac Cancer Diabetes Infection Assistive Device: Needs: Respiratory Immunosuppressed Osteoporosis Open wound Other (specify) PRIOR/CURRENT LEVEL OF FUNCTION Prior level of function (ADL/IADL) Specify: (ADL/IADL On Problematic Areas) .p n SA sy M ste PL m E .co Hypertension I m MEDICAL HISTORY Has: Current level of function (ADL/IADL) Specify: (ADL/IADL On Problematic Areas) LIVING SITUATION Capable Able Willing caregiver available Limited caregiver support (ability/willingness) No caregiver available HOME SAFETY BARRIERS: PERTINENT MEDICAL/SOCIAL HISTORY AND/OR PREVIOUS THERAPY RECEIVED AND OUTCOMES Throw rugs Needs railings Steps (number/condition) Other (specify) w Needs grab bars w Clutter Alert w BEHAVIOR/MENTAL STATUS Oriented Conf used Cooperative Impaired Judgement Memory deficits Other (specify) PAIN INTENSITY: 0 1 2 3 4 5 6 7 8 9 10 LOCATION: AGGRAVATING /RELIEVING FACTORS: PAIN TYPE (dull, aching, etc): PATTERN (Irradiation): VITAL SIGNS/CURRENT STATUS BP: Edema: Sensation: Skin Condition: Communication- T.P.R.: Muscle Tone: Posture: Vision: Hearing: Endurance: Orthotic/ Prosthetic Devices: PART 1 - Clinical Record PATIENT/CLIENT NAME - Last First, Middle Initial PART 2 - Therapist ID# PHYSICAL THERAPY EVALUATION PHYSICAL THERAPY (Cont'd.) Cruz & Sanz Health Services, Inc. EVALUATION MUSCLE STRENGTH/FUNCTIONAL ROM EVAL Shoulder ACTION Flex/Extend Abd./Add. Int. rot./Ext. rot. ASSIST SCORE TASK ASSISTIVE DEVICES/COMMENTS Roll/Turn Sit/Supine Scoot/Bridge Flex/Extend Forearm Sup./Pron. Wrist Flex/Extend Fingers Flex/Extend Hip Flex/Extend Int. rot./Ext. rot. Ankle Plant/Dors Foot Inver/Ever Floor Static Sitting Dynamic Sitting Static Standing Dynamic Standing Propulsion W/C SKILLS .p n SA sy M ste PL m E .co Flex/Extend Toilet Auto Abd./Add. Knee Bed/Wheelchair m Elbow TRANSFERS Sit/Stand BALANCE LOWER EXTREMITIES UPPER EXTREMITIES AREA FUNCTIONAL INDEPENDENCE/BALANCE EVAL ROM Right Left BED MOBILITY STRENGTH Right Left RE-EVALUATION Pressure Reliefs Foot Rests Locks OBJECTIVE DATA TESTS AND SCALES MANUAL MUSCLE TEST (MMT) MUSCLE STRENGTH FUNCTIONAL RANGE OF MOTION (ROM) SCALE GRADE 5 4 3 2 1 0 DESCRIPTION Normal functional strength - against gravity - full resistance. Good strength - against gravity with some resistance. Fair strength - against gravity - no resistance - safety compromise. Poor strength - unable to move against gravity. Trace strength - slight muscle contraction - no motion. Zero - no active muscle contraction. GRADE 5 4 3 2 1 5 4 3 2 1 0 NORMATIVE DATA FOR JOINT MOTION (ROM) w Elbow Forearm Wrist Fingers BALANCE SCALE (sitting - standing) DESCRIPTION GRADE 106% active functional motion. 75% active functional motion. 50% active functional motion. 25% active functional motion. Less than 25%. AREA Shoulder DESCRIPTION Physically able and does task independently. Verbal cue (VC) only needed. Stand-by assist (SBA)-100% patient/client effort. Minimum assist (Min A)-75% patient/client effort. Maximum assist (Max A)-25% - 50% patient/client effort. Totally dependent-total care/support w 1 0 w FUNCTIONAL INDEPENDENCE SCALE (bed mobility, transfers, W/C skills) GRADE 5 4 3 2 DESCRIPTION Hip Independent Verbal cue (VC) only needed. Stand-by assist (SBA)-100% patient/client effort. Minimum assist (Min A)-75% patient/client effort. Maximum assist (Max A)-25% patient/client effort. Totally dependent for support. Knee Ankle Foot ACTION/MOVEMENT o 158 Extend Flex o 170 Abd. o Add. 70 Int. rot. Ext. rot. 145 o Ext. Flex o 85 Pron. Sup. o 73 Ext. Flex o 90 Flex all Ext. o 901-115 Ext. Flex o 45 Add. Abd. o 45 Ext. rot. Int. rot. o Flex 135 Ext. o Plant. 50 Dors. Inv. 30 o Ever. o 55 o 50 o 90 0o o 70 o 70 o 0 25 o o 30 45o 10o o 20 o 20 GAIT ASSISTANCE: SBA Min. assist Mod.assist Max. assist Unable Stairs (number/condition) DISTANCE: PWB WBAT TDWB NWB WEIGHT BEARING STATUS: FWB ASSISTIVE DEVICE(S): Cane Quad cane Crutches Hemi-walker Wheeled walker Walker Other (specify) SURFACES: Independent Level Uneven FOR RE-EVALUATION USE ONLY: IF A PREVIOUS PLAN OF CARE WAS ESTABLISHED, THEN IT WILL: CHANGE NOT CHANGE QUALITY/DEVIATIONS: PATIENT INFORMATION PATIENT'S NAME: THERAPIST'S SIGNATURE/TITLE MED. RECORD #: DATE / / PHYSICIAN'S DATE SIGNATURE * If no changes made to Initial Plan of care, MD signature no required. / / Cruz & Sanz Health Services, Inc. PHYSICAL THERAPY WEEKLY SUMMARY REPORT Bedrest/BRP Transfer Bed/ Chair Up as Tolerated ACTIVITIES PERMITTED: Complete Bedrest No Weightbearing Independent at Home No Restrictions Full Weightbearing Partial Weightbearing Hoyer Lift Stair Climbing Cane Crutches Walker Wheel Chair Other Disoriented Agitated Comatose Depressed Lethargic MENTALSTATUS: Oriented Forgetful Other Subjective Comments: Specific Safety Issues Addressed: Ambulates with Assist Uses W/C, Walker, Cane Severe Weakness Paralysis Unable to walk Other m Severe SOB Bed bound Up in Chair with max assist Balance/Gait - Unsteady .p n SA sy M ste PL m E .co HOMEBOUND STATUS DUE TO: INSTRUCTED: Pt. C.G w TREATMENT RENDERED (If Pt/CG. instructed. see response below) Assessment Therapeutic Exercises Adaptive Equipment Transfer Training Gait Training EMS, Ultrasound, Massages, Hot/Cold Pack w w Energy Conservation Other PLAN OF CARE: PROBLEM - ACTION/PROGRESS TOWARD GOALS - PT'S/CG's RESPONSE TO TREATMENT/INSTRUCTION Interdisciplinary Communication: Date/Describe: Next Scheduled Visit Date: Additions to Plan of Care Patient Name Therapist Name/Signature/Title R.N. P.T./P.T.A. O.T./OTA S.L.P. Plan for Next Visit: Date: M.S.W. H.H.A. M.D. PHYSICAL THERAPY REVISIT NOTE TRINITY HEALTH SERVICES, INC. DATE OF SERVICE: PT ID PERFORMED VIA NAME, DOB, AND ADDRESS VITAL SIGNS: Temperature: Pulse: / Blood Pressure: Right PAIN: None Same Regular / Left Improved Worse Lying OUT Irregular Respirations: Standing Sitting Regular Irregular O2 saturation ____ % (when ordered) Location(s) Origin Intensity 0- 10 Duration TIME IN Relief measures Other TYPE OF VISIT: Revisit SOC DATE: Revisit and Supervisory Visit Other (specify) HOMEBOUND REASON: Needs assistance for all activities Residual weakness Requires assistance to ambulate Confusion, unable to go out of home alone Severe SOB, SOB upon exertion Unable to safely leave home unassisted Dependent upon adaptive device(s) Medical restrictions Other (specify) TREATMENT DIAGNOSIS/PROBLEM AND EXPECTED OUTCOMES: SIGNS/SYMPTOMS THAT SHOULD BE PRESENT TO WARRANT ADMINISTRATION OF THE TREATMENT: PHYSICAL THERAPY INTERVENTION/INSTRUCTIONS (Mark all applicable with an ''X''.) Balance training/activities TENS Ultrasound (B7) Electrotherapy (B8) Prosthetic training (B9) Preprosthetic training Fabrication of orthotic device (B10) Muscle re-education (B11) Modality used Location Frequency Duration Intensity Other Modality used Location Frequency Duration Intensity Other ROM: STRENGTH: BALANCE: MOBILITY/TRANSFER/AMBULATION: ASSESSMENT/PATIENT'S PROGRESS: SKILLED INTERVENTION (OUTCOME): Teach safe stair climbing skills Teach safe/effective use of adaptive/assist device (specify) Other: Cardiopulmonary PT Pain Management CPM (specify) Functional mobility training Teach bed mobility skills Teach hip safety precautions .p n SA sy M ste PL m E .co Copy given to patient Copy attached to chart Patient/Family education Therapeutic exercise (B2) Transfer training (B3) Gait training (B5) Management and evaluation of care plan (B12) Pulmonary Physical Therapy (B6) m Evaluation (B1) Establish/Upgrade home exercise program Modality used Location Frequency Duration Intensity Other SAFETY ISSUES w w w Obstructed pathways Home environment Stairs Unsteady gait Verbal cues required Equipment in poor condition Bathroom Commode Others: TEACHING, TRAINING, RESPONSE TO INSTRUCTIONS: Reviewed/Revised with patient involvement. CARE PLAN: If revised, specify To CG Family To Patient INSTRUCTION ABOUT: Treatment, Equipment Need for referral (specify) Other: ______________________ Other: ______________________ TEACHING/TRAINING OF PLAN FOR NEXT VISIT: PATIENT/FAMILY RESPONSE TO INSTRUCTIONS: (specify) DISCHARGE PLANS DISCUSSED WITH: Patient/Family Physician Other (specify) Care Manager BILLABLE SUPPLIES RECORDED? N/A Yes (specify) CARE COORDINATION: HHA MSW SN Physician PT/PTA Other (specify) OT CARE PLAN UPDATED? SLP No Yes (specify, complete Modify Order) If PT assistant/aide not present, specify date he/she was / / contacted regarding updated care plan: SIGNATURES/DATES x Patient/Caregiver (if applicable, optional if weekly is used) / Date / PART 1 - Clinical Record PATIENT NAME - Last, First, Middle Initial Complete TIME OUT prior to signing below. Therapist (signature/title) PART 2 - Therapist ID# / Date / PHYSICAL THERAPY IN DEPTH ASSESSMENT REAL BEST HOME HEALTH SERVICES, INC. *This In Depth Assessment is to be completed in its entirety. No revisit note required! HOMEBOUND REASON: Needs assistance for all activities Residual weakness Requires assistance to ambulate Confusion, unable to go out of home alone Unable to safely leave home unassisted Severe SOB, SOB upon exertion Dependent upon adaptive device(s) Medical restrictions Other (specify)____________________________________________________________ TYPE OF EVALUATION 13TH VISIT Supervisory 19TH VISIT 30 day visit Other visit: Indicate # ______ SOC Date____/____/_____ TREATMENT DIAGNOSIS(ES) / PROBLEMS IDENTIFIED AT START OF CARE .p n SA sy M ste PL m E .co m ________________________________________________________________________________________________________ ________________________________________________________________________________________________________ PRIOR LEVEL OF FUNCTION/ AT THE START OF CARE ADLs Independent Needed assistance Unable Equipment used &/or assistance needed: __________________ _______________________________________________________________________________________________________ In-Home Mobility (gait/wheelchair/scooter): Independent Needed assistance Unable Equipment used &/or assistance needed:_________________________________________________________________________________________ Community Mobility (gait/wheelchair/scooter): Independent Needed assistance Unable Equipment used &/or assistance needed:_________________________________________________________________________________________ CURRENT LEVEL OF FUNCTION ADLs Independent Needed assistance Unable Equipment used &/or assistance needed: __________________ ________________________________________________________________________________________________________ In-Home Mobility (gait/wheelchair/scooter): Independent Needed assistance Unable Equipment used &/or assistance needed:_________________________________________________________________________________________ Community Mobility (gait/wheelchair/scooter): Independent Needed assistance Unable Equipment used: _____ ________________________________________________________________________________________________________ LIVING SITUATION Capable Able Willing Caregiver available Limited caregiver support (ability/willingness) No caregiver available Home Safety Barriers: Clutter Throw rugs Needs Grab Bars Needs railings Steps (number/condition)_______________ Other(specify)__________________________________________________ BEHAVIOR/MENTAL STATUS Alert Oriented Cooperative Confused Memory deficits Impaired judgment Other (specify)__________ ________________________________________________________________________________________________________ CCURRENT PAIN Location(s) ________________________________________________________________ Pain (describe) ______________________________________________________________ Impact on Function_____________________________________________________________________ 1 2 3 4 5 6 7 8 9 10 Previous Pain Level ____________________________________________________________ CURRENT ADL/IADLs Shoulder LEFT RIGHT LEFT w RIGHT w w CURRENT MUSCLE STRENGTH/FUNCTIONAL ROM EVAL AREA STRENGTH ACTION ROM (degrees) Flex/Extend Abd. /Add. Int.rot/Ext rot. Elbow Forearm Wrist Fingers Flex/Extend Sup./Pron Flex/Extend Flex/Extend CURRENT FUNCTIONAL INDEPENDENCE/BALANCE EVAL ASSISTIVE TASK LEVEL DEVICES/ OF COMMENTS ASSIST Bed Roll/Turn Mobility Sit/Supine Scoot /Bridge Transfers Sit/Stand Bed/Wheelchair Toilet Floor Auto Flex/Extend Hip Abd. /Add. Balance Int.rot/Ext rot Knee Ankle Foot Flex/Extend Plants. /Dors. Inver/Ever PATIENT/CLIENT NAME - Last, First, Middle Initial Wheel Chair Skills ID# Static Sitting Static Standing Dynamic Sitting Dynamic Standing Propulsion Pressure Reliefs Foot Rests Locks Wheel Chair Mobility GRADE 5 4 3 2 1 MANUAL MUSCLE TEST (MMT) MUSCLE STRENGTH GRADE Normal functional strength – against gravity - full resistance. Good strength - against gravity with some resistance Fair strength - against gravity - no resistance – safety compromise. Poor strength - unable to move against gravity. Trace strength - slight muscle contraction - no motion. Noted Deviations from previous assessments GAIT: Braces/prosthesis:_________________________________________________________ Assistance: Independent SBA Min Assist Mod Assist Max Assist Unable Distance: _________________ Surfaces: Level Uneven Stairs (number/condition) ______________________________________ Weight Bearing Status: FWB WBAT PWB TDWB NWB Other:_________ Patient Has Assistive Device(s): Standard Cane Quad Cane Crutches Wheel Chair Walker(specify type) ________________ Other (specify) ___________________________________________________ Patient Needs Assistive Device(s): Standard Cane Quad Cane Crutches Wheel Chair Walker(specify type) ________________ Other (specify) Noted Gait Deviations: _________________________________ _______________________________________________________________________________________________________ Balance: TUG (On a scale of 1-4) 1 Less than 10 seconds - High mobility 2 10-19 seconds -Typical mobility 3 20-29 seconds - Slower mobility 4 30+ seconds - Diminished mobility: Interventions: __________________ Sensation (describe & include impact on function if appropriate): m BERG or Tinnetti Forms can be attached if appropriate for evaluation .p n SA sy M ste PL m E .co REHAB POTENTIAL/ DISCHARGE PLANS Rehab Potential Fair: Pt will develop functional mobility within the home care setting Rehab Potential: Good with PT able to return to previous level of activity and improvement in functional status in accordance with pt's endurance level. Discharge Plan: Pt will be d/c when Pt is able to function independently w/in current limitations @ home Current Goals that pertain to current illness Rehab Potential: Guarded with minimal improvement in functional status expected and decline is possible. Rehab Potential: Good for PT to be able to follow the plan of care/treatment regimen, and be able to self manage her/his condition. Other Discharge Plan: Pt will be discharged when Pt is able to function with assistance of caregiver within current limitations at home Other Progress Toward Goals/ Lack of Progress Toward Goals w w w Pt. will ______ assist with bed mobility within_____ weeks visits. Pt. to demonstrate increased strength of ________ (include specific joint, muscle, and indicate left, right or bilat.) to _______ within ______ weeks visits Pt. &/or cg will demonstrate comprehension of home exercise program within____ weeks visits. Pt will verbalize pain relief from ___/10 to ____/10 within ____________ weeks visits. Pt. will demonstrate increased ___ ROM of ______ to ______ degrees within ______ weeks visits Pt/cg will demonstrate __________transfers with ______ level of assist within____ weeks visits. Pt will ambulate _____ feet with ____________assistance with without ___________________assistive device within __________ weeks visits Increase ______ sitting balance to _______ within ______ weeks visits Increase ______ standing balance to _______ within _____ weeks visits Additional Current Goals Rehab Potential: good for stated goals Progress Toward Goals/ Lack of Progress Toward Goals Other: Other: Other: PATIENT/CLIENT NAME - Last, First, Middle Initial ID# New Goals: Functional Reassessment Expectation of Progress Toward Goals If lack of progress to goals: therapist and physician determination of need for continuation Supportable statement to continue therapy and why goals attainable: m Safety (PT to document noted safety concerns and the training needed to address them): .p n SA sy M ste PL m E .co Treatment Provided This Visit: Plan for next visit: w Patient/Caregiver response to Plan of Care: w w Care coordination/ interdisciplinary communication ( to address findings and plans to continue) with: Physician SN Case Manager PTA OT ST MSW Other (specify)______________________________________________ Changes to the POC: Patient/Client Signature___________________________ Therapist Signature/Title _________________________________ Date ____/____ / _____Time In ________ Time Out_______ Date_____/_____/_______ QI Review Yes Frequency Verified Yes PATIENT/CLIENT NAME - Last, First, Middle Initial ID# PHYSICAL THERAPY VISIT NOTE VISIT DATE: VITAL SIGNS: Pulse: Blood Pressure: Right PAIN: None Regular Left / Improved Same Location(s) Constant Frequency: Relief Measures Irregular / Respiration: Lying Standing Regular Sitting / / Irregular Worse NO HURT Occasional Intensity 1 - 1 0 Intermittent HURTS HURTS HURTS HURTS HURTS LITTLE BIT LITTLE MORE EVEN MORE WHOLE LOT WORSE . 0 2 N o Pain 4 6 8 Moderate Pain TYPE OF VISIT: Needs assistance for all activities Residual weakness HOMEBOUND REASON: Requires assistance to ambulate Confusion, unable to go out of home alone Requires assistance to transfer Severe SOB, SOB upon exertion Medical restrictions Unable to safely leave home unassisted Other (specify) Dependant upon adaptive device(s) Evaluation Visit Visit and supervisory visit Discharge Other (specify) INTERVENTIONS Gait training m TREATMENT DIAGNOSIS/PROBLEM Home exercise program upgrade .p n SA sy M ste PL m E .co Evaluation Establish rehab. program Establish home exercise program Copy given to patient Copy attached to chart Patient/Client/Family education Therapeutic/Isometric/Isotonic Exercises Muscle Strengthening Passive/Active/Resistive exercises Stretching exercises Transfer Training Pulmonary Physical Therapy Disease Process and Management Energy Conservation Techniques Prosthetic Training Preprosthetic Training Pain Management CPM (Specify) Functionality Mobility Training Teach safe/effective use of adaptive/ assist device (specify) Teach safe stair climbing skills Teach Bed mobility skills Teach hip safety precautions Falls Prevention Body Mechanics/Posture Training Pulse Ox Management and Evaluation of Care Plan Other: Muscle/Neuro Re-Education Breathing/CP Conditioning Exercises Balance training/activities Note: Specify location, amount, frequency and duration with any modality SAFETY ISSUES Obstructive pathways Home environment Stairs Unsteady gait Verbal cues required Equipment in poor condition Bathroom Impaired judgement/safety Other (specify) w ASSESSMENT/PROGRESS TOWARDS GOALS: AMBULATION: w STRENGTH: BALANCE: w ROM: TRANSFERS/BED MOBILITY: PATIENT/CAREGIVER RESPONSE: SUPERVISORY VISIT (Complete if applicable) PLAN FOR NEXT VISIT: PT Assistant Aide Supervisory Visit: DISCHARGE PLANS DISCUSSED WITH: Patient/Family/Caregiver Not present N/A Unscheduled Observation of Care Manager Physician Teaching/Training of Other (specify) CARE COORDINATION: MSW OT SLP Other (specify) Present Scheduled None SN Physician PT/PTA HHA Case Manager MEDICATION CHANGE. Since last visit Patient/Family Feedback on Services/Care (specify) Care Plan Updated? Yes No Yes (specify) No SIGNATURE/DATE: / x PATIENT NAME - Last, First, Middle Initial / Date Therapist (signature/title) ID# 10 Worst Possible Pain PHYSICAL THERAPY EVALUATION OBJECTIVE DATA TESTS AND SCALES PRINTED ON NEXT PAGE DATE OF SERVICE / / / / SOC DATE HOMEBOUND REASON: Needs assistance for all activities Residual weakness (If Initial Evaluation, Complete Physical Requires assistance to ambulate Confusion, unable to go out of home alone Therapy Care Plan) Unable to safely leave home unassisted Severe SOB, SOB upon exertion OTHER DISCIPLINES PROVIDING CARE: Dependent upon adaptive device(s) Medical restrictions SN OT ST Aide MSW Other (specify) Requires assistance to transfer PERTINENT BACKGROUND INFORMATION Chest Pt. PT ORDERS: Evaluation Gait Training Therapeutic Exercise Home Program Instruction Transfer Training Electrotherapy Ultrasound Prosthetic Training Other: Muscle Re-education TREATMENT/DIAGNOSIS/PROBLEM: MEDICAL HISTORY Cancer Immunosuppressed Arthritis Other (specify) REASON FOR EVALUATION (Diagnosis/Problem/History) .p n SA sy M ste PL m E .co m Hypertension Cardiac Diabetes Respiratory Osteoporosis Fractures LIVING SITUATION w Capable Able Willing caregiver available ALF Limited caregiver support (ability/willingness) No caregiver available HOME SAFETY BARRIERS: None Clutter Throw rugs Bath bench/equipment Needs grab bar Needs railings Steps (number/condition) Other (specify) BEHAVIOR/MENTAL STATUS w w Alert Oriented ___x1___ x2___ x3 Cooperative Confused Memory deficits Impaired judgement Other (specify) PAIN NO HURT 0 HURTS LITTLE BIT HURTS LITTLE MORE HURTS EVEN MORE HURTS WHOLE LOT 2 4 6 8 HURTS WORSE 10 LOCATION: FREQUENCY: Occasional AGGRAVATING/RELIEVING FACTORS: PATIENT NAME - Last, First, Middle Initial Intermittent Continuous PRIOR LEVEL OF FUNCTION ADLs: Independent Unable Level of assistance _________ Equipment Used: Other: IN-HOME MOBILITY (gait or wheelchair/scooter): Independent Level of assistance ________________ Unable Equipment Used: No AD Cane/QC Walker/RW WC/Scooter Other: TRANSFER MOBILITY: Independent Level of assistance ________________ Unable Equipment Used: No AD Cane/QC Walker/RW WC/Scooter Other: COMMUNITY MOBILITY (gait or wheelchair/scooter): Independent Level of assistance ____________ Unable Equipment Used: No AD Cane/QC Walker/RW WC/Scooter Other: VITAL SIGNS/CURRENT STATUS Blood Pressure: Pulse: Respirations: Skin Condition: Edema: Vision: Sensation: Communication: Hearing: Posture: Activity Tolerance: Muscle Tone: Orthotic/Prosthetic devices: ID# Continued on Next Page UPPER EXTREM. MUSCLE STRENGTH / FUNCTIONAL ROM EVAL AREA ROM STRENGTH AREA BED MOBILITY PHYSICAL THERAPY EVALUATION (Cont'd) FUNCTIONAL INDEPENDENCE/BALANCE EVAL ASSIST SCORE ASSISTIVE DEVICES/COMMENTS TASKS Roll/Turn Sit/Supine Scoot/Bridge Sit/Stand Elbow Bed/Wheelchair Forearm Toilet Wrist Floor Fingers Auto Hip Static Sitting Dynamic Sitting Static Standing Knee Dynamic Standing Ankle Propulsion Foot Pressure Reliefs AREA Foot Rests ROM Locks MANUAL MUSCLE TEST (MMT) MUSCLE STRENGTH FUNCTIONAL INDEPENDENCE SCALE (bed mobility, transfers, balance, W/C Skills) GRADE DESCRIPTION DESCRIPTION GRADE 5 Normal functional strength - against gravity - full resistance Independent - physically able and independent 6 Supervision and/or verbal cues - 100% patient effort 5 Good strength - against gravity with some resistance 4 4 Contact guard - 100% patient effort Fair strength - against gravity - no resistance - safety compromise 3 3 Minimum assist (Min A) - 75% patient/client effort Poor strength - unable to move against gravity 2 2 Moderate assist (Mod A) - 50% patient effort Trace strength - slight muscle contraction - no motion 1 Maximum assist (Max A) - 25%-50% patient/client effort 1 Zero - no active muscle contraction Totally dependent - total care/support 0 0 SAFETY ISSUES FUNCTIONAL RANGE OF MOTION (ROM) SCALE GRADE Obstructive pathways Equipment in poor condition DESCRIPTION GRADE DESCRIPTION Home environment Bathroom 5 100% active functional motion 2 25% active function motion Stairs Impaired judgement/safety 75% active functional motion 4 Less than 25% 1 Unsteady gait Other (specify) 50% active functional motion 3 Verbal cues required GAIT Left Right Left SURFACES: TRANSFERS BALANCE W/C SKILLS .p n SA sy M ste PL m E .co Independent Level SBA Uneven WEIGHT BEARING STATUS: ASSISTIVE DEVICE(S): Contact guard Minimum assist Moderate assist FWB WBAT PWB Cane Quad Cane Other (specify): TTWB Crutches Maximum assist Unable DISTANCE/TIME: Stairs (number/condition) w ASSISTANCE: w w SPINE LOWER EXTREM. Flex/Extend Abd/Add. Int. Rot./Ext. Rot. Flex/Extend Sup./Pron. Flex/Extend Flex/Extend Flex/Extend Abd./Add. Int. Rot./Ext. Rot. Flex/Extend Plant./Dors. Inver./Ever. ACTION STRENGTH m Shoulder Right NWB Hemi Walker Walker Wheeled Walker QUALITY/DEVIATIONS/POSTURES: SUMMARY INSTRUCTION PROVIDED: Safety Exercise Other (describe) Equipment needed (describe) DISCHARGE DISCUSSED WITH: Patient/Family Care Manager Physician APPROXIMATE NEXT VISIT DATE: Other (specify) CARE COORDINATION: MSW PTA / / PLAN FOR NEXT VISIT COTA None Aide Physician SN PT OT ST Case Manager Other (specify) x Therapist Printed Name and Title x Therapist (signature) / Date / PHYSICAL THERAPY CARE PLAN SOC DATE Diagnosis: FREQUENCY AND DURATION: Patient/Caregiver aware and agreeable to POC and Frequency Duration: Yes / / No (explain) INTERVENTIONS Evaluation Establish rehab. program Establish home exercise program Copy given to patient Copy attached to chart Patient/Client/Family education Therapeutic/Isometric/Isotonic Exercises Muscle Strengthening Passive/Active/Resistive exercises Stretching exercises Transfer Training Pain Management CPM (Specify) Functionality Mobility Training Teach safe/effective use of adaptive/ assist device (specify) Teach safe stair climbing skills Teach Bed mobility skills Teach hip safety precautions Falls Prevention Body Mechanics/Posture Training Pulse Ox Gait training Home exercise program upgrade Pulmonary Physical Therapy Disease Process and Management Energy Conservation Techniques Prosthetic Training Preprosthetic Training Management and Evaluation of Care Plan Other: Muscle/Neuro Re-Education Breathing/CP Conditioning Exercises Balance training/activities m Monitor Vital Signs: PROVIDE: U.S. to _______________________________________________ at _______________ warts/cm2 x ___________ minutes. Pulse EMS to _____________________________________________________________ x ______________ minutes. Respirations .p n SA sy M ste PL m E .co Heat/Cold to _____________________________________________________________ x _______________ minutes. Therapeutic massage to ___________________________________________________ x ________________ minutes. Blood Pressure Joint Mobilization __________________________________________________________________________________ SHORT TERM GOALS Demonstrate effective pain management within Improve bed mobility to weeks assist within weeks Improve transfers to assist using within weeks Decrease pain level to within weeks Patient to be independent with safety issues in weeks Improve wheelchair use to within Patient will ambulate with weeks w feet R L UE to /5 in weeks Increase strength of R L LE to /5 in weeks Improve strength of to Increase ROM of degree extension in Increase ROM of Of /5 within joint to in weeks weeks weeks Ambulation endurance will be within weeks weeks Fair R L UE to /5 in weeks Increase strength of R L LE to /5 in weeks to /5 within joint to weeks weeks degree flexion joint to degree Increase ROM of of in weeks Demonstrate ROM to WNL within weeks in Good ADDITIONAL INFORMATION: PTA is following the case Plan developed by (Name/Signature/Title) PATIENT NAME - Last, First, Middle Initial feet Increase strength of GOALS: PHYSICAL THERAPY Other Patient will be discharged to care of self/caregiver with self/caregiver arranged healthcare Other Poor weeks minutes or Improve balance to Other REHAB POTENTIAL: DISCHARGE PLAN: weeks weeks device with assist Patient will ambulate with within weeks Increase ROM of degree extension in and weeks in assist using Improve strength of degree weeks Demonstrate ROM to WNL within Improve balance to Other weeks assist within Patient will be able to climb stairs/uneven surfaces device with with assist within degree flexion joint to weeks within Improve transfers to weeks minutes or weeks Patient to be independent with safety issues in Improve wheelchair use to within Increase strength of and Decrease pain level to within w Ambulation distance will be within weeks weeks weeks Improve bed mobility to weeks Patient will be able to climb stairs/uneven surfaces with device with assist within Return to pre-injury/illness level of function within Patient will meet maximum rehab potential within Return to optimal and safe functionality within device with assist w within LONG TERM GOALS Date ID# weeks THERAPY DISCHARGE SUMMARY PATIENT LAST NAME FIRST NAME PATIENT # PARTIAL - STILL RECEIVING SERVICES OF: COMPLETE DISCH DATE DR TYPE OF DISCHARGE: ADM DATE PT OT ST HHA SN ADDRESS DIAGNOSIS (PRIMARY) CITY, ST VISITS RENDERED BY: RN HHA PT OT GOALS MET HOSPITALIZATION SKILLED NURSING FACILITY TRANSFER TO ANOTHER AGENCY REASON FOR DISCHARGE: ZIP ST MSW MOVED OUT OF AREA PATIENT EXPIRED CARE REFUSED SKILLED CARE NO LONGER NEEDED OTHER NH ACLF FAMILY CARE OTHER IMPROVED STABLE UNSTABLE DECEASED REGRESSED DEPENDENT INDEPENDENT REQUIRES SUPERVISION/ASSIST GAIT TRAINING: N.W.B. R.U.E. ACTIVE R.L.E. HOYER LIFT EVEN SURFACES ASSISTANCE REQUIRED: MAXIMUM DISTANCE AMBULATED: 20 ft. INSTRUCTED ON HOME PROGRAM: PATIENT L.U.E. L.L.E. RESISTIVE TRUNK NECK CRUTCHES WALKER CANE QUAD CANE P.W.B. F.W.B. STAIRS UNEVEN SURFACES MINIMUM MODERATE GUARDING OTHER 40 ft. 60 ft. 80 ft. 100 ft. SIGNIFICANT OTHER FAMILY OTHER 120 ft. Physical Therapy w w NARRATIVE: ACTIVE ASSISTIVE .p n SA sy M ste PL m E .co W/C PASSIVE m SELF CARE DISPOSITION CONDITION DEPENDENCY EXERCISES PERFORMED WITH: TRANSFER ACTIVITIES: SUMMATION OF SERVICES RENDERED AND GOALS ACHIEVED PATIENT HAS ACHIEVED ANTICIPATED GOALS w DEMONSTRATES TRANSFER TECHNIQUE AND USE OF SPECIAL DEVICES PATIENT IS SAFELY INDEPENDENT WITHIN DISEASE LIMITATIONS ABSENCE OF PAIN DEMONSTRATES ABILITY TO DO SPECIAL TREATMENTS HEALED INCISION FREE OF CONTRACTURES DEMONSTRATES STUMP WRAPPING AND HYGIENE RANGE OF MOTION OF ALL JOINTS IS WITHIN NORMAL RANGE DEMONSTRATES TECHNIQUE TO CARE FOR AND PROTECT FUNCTIONING EXTREMITY DEMONSTRATES RANGE OF MOTION EXERCISES DEMONSTRATES MUSCLE STRENGTHENING EXERCISES DESCRIBES PHANTOM LIMB SENSATION DEMONSTRATES TURNING AND POSITIONING SCHEDULE PATIENT DEMONSTRATES STABILIZATION OF AMBULATION AMBULATES SAFELY WITH ASSISTIVE DEVICE AMBULATES SAFELY WITHOUT ASSISTIVE DEVICE Occupational Therapy PATIENT HAS REACHED ALL REALISTIC ACHIEVABLE GOALS Speech Therapy DEMONSTRATES KNOWLEDGE OF OPERATION & CARE OF ADAPTIVE EQUIPMENT PATIENT HAS REACHED ALL REALISTIC ACHIEVABLE GOALS PATIENT HAS ATTAINED MAXIMUM BENEFIT FROM THERAPEUTIC PROGRAM DEMONSTRATES ENERGY CONSERVATION/WORK SIMPLIFICATION TECHNIQUES VERBAL AND SENTENCE FORMULATION AND COMPREHENSION IMPROVED TO MAXIMUM ATTAINMENT WITHIN DISEASE LIMITATIONS PATIENT/S.O. RESPONSE AND ADHERENCE TO TEACHING: DEMONSTRATIONS COMPENSATORY & SAFETY TECHNIQUES FAIR GOOD THERAPY GOALS MET: YES NO IF NO, EXPLAIN PATIENT/S.O.GOALS MET: YES NO IF NO, EXPLAIN POOR COMMENTS: PATIENTS/So. INSTRUCTED ON IMPORTANCE OF ADHERENCE OF EXERCISE PROGRAM, M.D. FOLLOW-UP AND NOTIFY M.D. IF COMPLICATIONS OCCUR. DATE THERAPIST SIGNATURE White: Medical Records Yellow: Physician M.D. NOTIFIED OF DISCHARGE Visit made No visit PHYSICAL THERAPY DISCHARGE SUMMARY PATIENT CR# TO: DR. ADDRESS CITY PARTIAL - continued services HIC# 1st VISIT SOC COMPLETE or D/C DATE REASON FOR DISCHARGE: NUMBER OF VISITS: PT OT DIAGNOSES: SLP MSS ADMISSION STATUS AIDE DISCHARGE STATUS Pain due to ROM Str/End Balance Coordination Bed Mobility Transfers Ambulation Fine Motor Coord S/P Awareness S/P Coord Receptive Com Expressive Com Swallowing Knowledge level of Disease Process HEP Treatments Care Management Safety Other Other , level .p n SA sy M ste PL m E .co m , level w w w Pain due to ROM Strength and Endurance Balance Coordination Bed Mobility Transfers Ambulation Fine Motor Coordination Sensory/ Perceptual Awareness Sensory/Perceptual Coordination Receptive Communication Expressive Communication Swallowing Knowledge level of Disease Process HEP Treatments Care Management Safety Other Other ZIP PROBLEMS IDENTIFIED AFTER START OF CARE: SELF CARE ACTIVITY ON ADMISSION: Self Care resumed; or Assist to be provided by At d/c: Transferred to or Instruction, Observation/Evaluation, Personal care as ordered, CARE PROVIDED: Treatments as ordered, Other I UNMET NEEDS: INSTRUCTIONS FOR CONTINUING CARE NEEDS: Other Home program, Equipment management, ADDITIONAL COMMENTS/ Referrals made: __ Physician contacted on Therapist Signature and discharge is approved. Date Physician follow-up, PHYSICAL THERAPY DISCHARGE SUMMARY ADDENDUM PHYSICAL THERAPY GOALS REACHED MAINTAIN/COMPLY WITH HOME SAFETY PROGRAM POC (485) GOALS REACHED: PATIENT DEMONSTRATED CORRECT BODY MECHANICS PATIENT AND/OR CG COMPREHEND AND DEMONSTRATED HOME EXERCISE PROGRAM ABLE TO COMPLY WITH EXERCISES: BOTH PASSIVE AND ACTIVE EXERCISE REGIMEN DEMONSTRATED EFFECTIVE FALL PREVENTION PROGRAM IMPROVED THE USE OF ASSISTIVE DEVICE: ________________ CARE PLAN SHORT/LONG TERM GOALS REACHED: PATIENT AMBULATED WITH __________________ (device) FOR _____________ FT WITH ________ ASSIST INCREASED STRENGTH OF RUE LUE RLE LLE TO ALLOW PATIENT TO PERFORM THE FOLLOWING ACTIVITIES: _______________________________________. INCREASED RANGE OF MOTION (ROM) OF __________________ JOINT TO ________ DEGREE FLEXION AND ______ DEGREE EXTENSION IN ____ WEEKS TO ALLOW PATIENT TO PERFORM THE FOLLOWING ACTIVITY: ____________________________. MUSCLE STRENGTH Pt. able to hold weigh _______ lb GENERAL Pt. able to oppose flexion or extension force over _____ Gait increased tinetti gait score to _____ / 12 Improved gait requiring ____ to _____ from _____ to ______ PAIN Pain decreased from _______/10 to ________ /10 Pt. able to turn side (facing up) to lateral (left/right) PATIENT EXPERIENCED A DECREASE IN PAIN .p n SA sy M ste PL m E .co Pt. able to lie back down DEMONSTRATED EFFECTIVE PAIN MANAGEMENT m BED MOBILITY ROM Pt. able to sit up independently _______ Pt. able to self reposition Pt. increased ROM of ________ by ______ degrees flexion/extension IMPROVED BED MOBILITY (INDEPENDENT) BALANCE SAFETY Pt. able to use ________________ independently to ________ feet Increased tinetti balance score to _____/16 Pt. able to reach steady static/dynamic sitting/standing balance with/without assistance Pt. able to self propel wheel chair _________ feet Pt able to finalize and demonstrated to follow up HEP. OTHER: TRANSFER Pt. able to transfer from _________ to _________ with/without assistance INDEPENDENT WITH TRANSFER SKILLS STAIR/UNEVEN SURFACE w w Pt. able to climb stair/uneven surface with/without assistance _____ steps # _______ w ADDITIONAL SPECIFIC THERAPY GOALS REACHED Patient Expectation DISCHARGE INSTRUCTIONS DISCUSSED WITH: Patient/Family Physician Other (specify) Care Manager CARE WAS COORDINATED: Physician MSW Aide PTA Other (specify) REHAB STATUS: Poor Fair OT SN ST Good Excellent ABLE TO UNDERSTAND MEDICATION REGIME AND CARE RELATED TO DISEASE PATIENT NAME - Last, First, Middle Initial DISCHARGED: PATIENT AND/OR CAREGIVER IS/ARE ABLE TO DEMONSTRATE KNOWLEDGE OF DISEASE MANAGEMENT, S/S COMPLICATIONS. PATIENT IS ABLE TO FUNCTION INDEPENDENTLY WITHIN HIS/HER CURRENT LIMITATION AT HOME. RETURNED TO INDEPENDENT LEVEL OF SELF CARE. ABLE TO REMAIN SAFELY IN RESIDENCE WITH ASSISTANT OF ________________________ DISCHARGED: MAXIMUM FUNCTIONAL POTENTIAL REACHED Goals documented by: LONG TERM SHORT TERM ABLE TO REMAIN IN HOME/RESIDENCE/ALF WITH ASSISTANCE OF PRIMARY CAEGIVER/SUPPORT AT HOME ABLE TO UNDERSTAND MEDICATION REGIMEN, AND CARE RELATED TO HIS/HER DISEASE. DISCHARGED: MAXIMUM FUNCTIONAL POTENTIAL REACHED. Date Therapist Name/Signature/title ID# www.pnsystem.com