Neonatal and Pediatric Parenteral Nutrition
advertisement

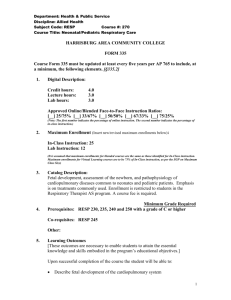
AACN Advanced Critical Care Volume 23, Number 4, pp.451-464 © 2012, AACN Neonatal and Pediatric Parenteral Nutrition Anne Gargasz, PharmD, BCPS ABSTRACT Parenteral nutrition is one of the most important therapeutic modalities invented in the last several decades. Since its introduction in the 1960s, this modality has saved thousands of lives by providing nutrients parenterally to sustain growth in premature neonates with severe intestinal immaturity and other pediatric patients with intestinal failure, such as a gastrointestinal fistula or short bowel syndrome. Although P arenteral nutrition (PN) is one of the most important therapeutic modalities invented in the last several decades. Parenteral nutrition, also known as hyperalimentation, was first introduced in the 1960s and used in beagle puppies and then later in a neonate with resection of 95% of her small bowel, with good nutritional outcomes.1 Since then, thousands of lives have been saved by the process of providing nutrients parenterally. It has helped sustain growth in premature neonates with severe intestinal immaturity and pediatric patients with intestinal failure as a result of gastrointestinal fistula or short bowel syndrome. In 2009, the National Center for Health Statistics reported that patients received PN in almost 360 000 hospital stays; 33% of the patients who received PN were children.2 Parenteral nutrition solutions are made either in a 2-in-1 (amino acids, carbohydrates, and electrolytes) solution with intravenous (IV) fat emulsion provided separately through a Y connector or in a 3-in-1 solution containing everything in a 2-in-1 formula plus lipids. This review discusses the nutritional requirements, common complications, medication additives, parenteral nutrition can be a lifesaving treatment, it is not benign. Many complications can result from either short- or longterm usage. This review discusses the nutritional requirements, common complications, medication additives, and special considerations for pediatric patients requiring parenteral nutrition. Keywords: neonatal, nutrition, parenteral nutrition, pediatric. and special considerations for neonatal and pediatric patients requiring PN. Goal of PN Goals for nutrition support in the pediatric population include obtaining body composition similar to age-matched children and maximizing long-term growth and neurodevelopment. In preterm neonates, the goal is to match the in utero human fetal growth rate of approximately 15 g/kg per day.3 The use of growth curves such as the one shown in Figure 1 for preterm infants is the standard rule of measure for determining appropriate height and weight gain in children.4 The Centers for Disease Control and Prevention (CDC) recommends the use of the World Health Organization growth standards to monitor growth for infants and children 0 to 2 years of age and the use of the Anne Gargasz is Pediatric Clinical Pharmacist, Tampa General Hospital, 1 Tampa General Circle, Tampa, FL 33606 (annegargasz @tgh.org). The author declares no conflicts of interest. DOI: 10.1097/NCI.0b013e31826e8f8b 451 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 451 15/10/12 3:24 PM G A R GAS Z A ACN Figure 1: Fenton growth chart for preterm infants. Reprinted with permission from Fenton TR. A new growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr. 2003;3:13–22. http://www.biomedcentral.com/1471-2431/3/13. Copyright 2003 Fenton; licensee BioMed Central Ltd. CDC growth charts for children 2 years of age and older (http://www.cdc.gov/growthcharts). Initial Considerations When writing or reviewing PN orders, clinicians should consider 3 things: the specific indication for PN for the patient, the patient’s current IV fluids, and whether the patient is at risk for refeeding syndrome (defined later). The specific indication for PN for a patient will determine his or her need for more or less fluid, macronutri- ents, or micronutrients. For example, if the patient has small bowel syndrome, has increased ostomy output, and is lagging behind on the growth chart, the clinician should provide more volume, protein, and calories. Next, the patient’s current IV fluids can be a helpful starting point in writing the PN formula. For example, if a 5-year-old patient weighing 23 kg has been receiving 5% dextrose in water and 0.45% sodium chloride with 20 mEq/L potassium chloride at 65 mL/h for the past 24 hours and 452 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 452 15/10/12 3:24 PM VOL UME 2 3 • N U MBER 4 • OCTOBER–DECEM BER 2012 NE ONATA L A ND P E D IAT RIC PA RE NT E RA L NUT RIT ION his laboratory values were within normal limits, PN can be started with 10% dextrose, 5 mEq/kg per day sodium chloride, and 1.3 mEq/kg per day potassium chloride at 65 mL/h. Finally, if this patient was at risk for refeeding syndrome, the clinician should use a lower caloric starting point, increase calories toward the goal more slowly, and consider adding more potassium, magnesium, and phosphorus than for a patient not at risk. Before starting PN, clinicians should obtain laboratory levels including a complete metabolic panel, magnesium, phosphorus, triglycerides, and prealbumin. Then a daily basic metabolic panel with magnesium and phosphorus should be ordered until laboratory values are within normal limits; once this goal has been achieved, weekly basic metabolic panel, magnesium, phosphorus, prealbumin, and triglyceride levels should be monitored. Although obtaining these laboratory values as specified is helpful, it may not always be practical in neonatal patients for whom the volume of blood required for these laboratory tests is large in comparison with their total blood volume. The need for laboratory tests must be weighed against the risk of making the patient anemic from blood draws. Indications for PN Although PN can be a lifesaving treatment, it is not benign. Many complications can result from either short- or long-term PN; therefore, one must carefully consider the initiation of PN for a patient. Outcomes consistently favor the use of enteral feeding over PN; therefore, enteral feeding is preferred whenever possible. Common indications for pediatric PN include pancreatitis, small bowel syndrome, severe malnutrition/failure to thrive, and an inability to tolerate oral or nasogastric feeds as well as other clinical scenarios in which the pediatric patient is expected to take nothing by mouth for more than 5 to 7 days. In the neonatal population, PN is indicated in premature patients and those with either very low birth weight (VLBW) (⬍ 1500 g) or extremely low birth weight (⬍ 1000 g). Full enteral feeds are not expected to be tolerated for some time in these populations as a result of gut immaturity, and withholding nutrition for even 1 day may lead to poor outcomes. Refeeding Syndrome Refeeding syndrome refers to the metabolic and clinical changes that occur as a result of providing aggressive nutritional support to a malnourished patient. Malnourished patients can have depleted intracellular phosphate stores. Refeeding causes a shift from fat and protein metabolism to carbohydrate metabolism. Hypophosphatemia, hypokalemia, and hypomagnesemia result from insulin secretion in response to a carbohydrate load, which shifts these electrolytes intracellularly. Medical complications that occur as a result of these fluid and electrolyte shifts can include tremors, seizures, cardiopulmonary abnormalities, and coma. At-risk patients generally include those who have been underfed for at least 10 to 14 days or who have had an acute weight loss of greater than 10% in the past 1 to 2 months. The greatest risk may occur during the first 2 to 3 weeks of aggressive nutritional augmentation to the patient; therefore, daily laboratory tests are recommended for the first 1 to 2 weeks and then twice weekly. These patients require a lower caloric starting point, calories are increased toward the goal more slowly, and more potassium, magnesium, and phosphorus may be required in their PN. Calculating Maintenance IV Fluid Volume and Other Fluid Considerations Total body water decreases dramatically from intrauterine life to adulthood: water constitutes 90% of body weight in the preterm infant, 71% to 83% of body weight in fullterm infants, and 50% to 60% of body weight in adults.5 The maintenance IV fluid (MIVF) volume for a pediatric patient may be determined by using either the HollidaySegar Method 100-50-20 rule (calculating the total daily volume) or the 4-2-1 rule (calculating an hourly rate) (Table 1).6 Patients with the following conditions may have increased fluid requirements: fever, burn, diabetes insipidus, diarrhea, ileostomy or biliary drainage, and hyperbilirubinemia. Patients with hypothermia, syndrome of inappropriate antidiuretic hormone, oliguric renal failure, or patent ductus arteriosus may have decreased volume requirements. Once the patient’s daily fluid requirement has been determined, the following equation can be used to calculate the actual volume that may be allotted to PN: PN volume ⫽ MIVF ⫺ lipid volume ⫺ drip/IV medication volumes ⫺ oral/nasogastric feeds. 453 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 453 15/10/12 3:24 PM G A R GAS Z A ACN Table 1: Calculations for Maintenance Fluid Requirements in Pediatric Patientsa Weight, kg Total Maintenance Fluids (mL/kg per day) Holliday-Segar Method “100-50-20 Rule” Fluid Rate (mL/kg per hour) Holliday-Segar Estimate “4-2-1 Rule” 100 mL/kg per day 4 mL/kg per hour 0-10 10-20 1000 mL ⫹ 50 mL/kg for every kg ⬎10 40 ⫹ 2⫻ every kg ⬎10 ⬎20 1500 mL ⫹ 20 mL/kg for every kg ⬎20 60 ⫹ 1⫻ every kg ⬎20 a Data from Holliday and Segar.6 Calculating Daily Energy Needs and Caloric Requirements The nutritional needs of pediatric patients are determined by their basal metabolic rate, physical activity, growth, and preexisting malnutrition. Caloric supply should aim at covering these needs. The preferred method to assess caloric needs in children is to measure total energy expenditure or resting energy expenditure.7 Equations for calculating specific basal metabolic rate or resting energy expenditure are shown in Table 2. In lieu of these equations, total parenteral energy needs may be roughly estimated using the ranges in Table 3.8 Patient conditions that require increased caloric needs may include fever, sepsis, burn, cardiac or pulmonary disease, major complicated surgery, and patients requiring “catch up” growth. Patients requiring fewer calories are those who are sedated, in a pentobarbital coma, being treated with mechanical ventilation, or paralyzed. Macronutrients Caloric needs are met by a proper balance of carbohydrates, proteins, and fats, which are supplied as follows: dextrose, amino acids, and lipids in the PN. Generally 40% to 60% of a patient’s caloric needs are derived from dextrose, 10% to 15% from amino acids, and 20% to 40% from intralipids. Dextrose Dextrose is the main source of calories in PN and usually comprises most of the osmolality of the solution. Each gram of dextrose provides 3.4 kcal. Normally when initiating PN in a pediatric patient, one would begin with either a 5% or 10% dextrose concentration and, based on the patient’s serum glucose levels, titrate the dose daily toward the patient’s goal dextrose in increments of 2.5% to 5%. For neonates, carbohydrate delivery should begin between 4 and 8 mg/kg per minute (4-6 mg/kg per minute for those weighing ⬍ 500 g and limited to 5 mg/kg per minute in critically ill children) of dextrose Table 2: Equations Recommended by the European Society for Clinical Nutrition and Metabolism for Calculating Basal Metabolic Rate or Resting Energy Expenditure in Childrena Age, y 0-3 Source WHO Schofield (WH) 3-10 WHO Schofield (WH) 10-18 Harris-Benedict Gender Equation Male REE ⫽ (60.9 ⫻ Wt) ⫺ 54 Female REE ⫽ (61 ⫻ Wt) ⫺ 51 Male BMR ⫽ (0.167 ⫻ Wt) ⫹ (1517.4 ⫻ Ht) ⫺ 617.6 Female BMR ⫽ (16.25 ⫻ Wt) ⫹ (1023.2 ⫻ Ht) ⫺ 423.5 Male REE ⫽ (22.7 ⫻ Wt) ⫹ 495 Female REE ⫽ (22.4 ⫻ Wt) ⫹ 499 Male BMR ⫽ (19.6 ⫻ Wt) ⫹ (130.3 ⫻ Ht) ⫹ 414.9 Female BMR ⫽ (16.97 ⫻ Wt) ⫹ (161.8 ⫻ Ht) ⫹ 371.2 Male REE ⫽ 66.47 ⫹ (13.75 ⫻ Wt) ⫹ (5 ⫻ Ht) ⫺ (6.76 ⫻ age) Female REE ⫽ 655.1 ⫹ (9.56 ⫻ Wt) ⫹ (1.85 ⫻ Ht) ⫺ (4.68 ⫻ age) Abbreviations: BMR, basic metabolic rate; Ht, length in meters (Schofield (WH) equations); Ht, length in cm (Harris-Benedict equation); REE, resting energy expenditure; WHO, World Health Organization; Wt, body weight in kilograms. a Data from Koletzko et al.7 454 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 454 15/10/12 3:24 PM VOL UME 2 3 • N U MBER 4 • OCTOBER–DECEM BER 2012 NE ONATA L A ND P E D IAT RIC PA RE NT E RA L NUT RIT ION Table 3: Estimation of Parenteral Nutrition Caloric Needsa Age Table 4: Estimates of Protein Requirements for Healthy Pediatric Patientsa Caloric Needs, kcal/kg per day Age Protein Requirements, g/kg per day Preterm neonate 90-120 ⬍6 mo Low birth weight/ preterm neonate 3-4 85-105 6-12 mo 80-100 Infant (1-12 mo) 2-3 1-7 y 75-90 Children (⬎10 kg or 1-10 y) 1-2 7-12 y 50-75 ⬎12-18 y 30-50 a Adolescents (11-17 y) a 0.8-1.5 Reprinted with permission from Mirtallo et al.8 Reprinted with permission from Mirtallo et al.8 to maintain adequate glucose levels and then advance to a goal of 10 to 13 mg/kg per minute as tolerated.3,7 Because of osmolarity reasons, most institutions have a peripheral IV catheter maximum limit of 10% to 12.5% dextrose (~900 mOsm/L) and a central venous catheter limit of 25% to 30% dextrose. Potential complications occurring from the IV administration of dextrose include hyperglycemia or hypoglycemia, glycosuria and potential osmotic diuresis, cholestasis, and hepatic steatosis (usually from long-term high-concentration infusion). Often difficulty may arise with patients who become hyperglycemic as a result of abnormal glucose tolerance yet have not reached their dextrose or nutritional goals. For these patients, especially those in the intensive care unit setting, adult studies have shown that the use of insulin to maintain a blood glucose level between 80 and 110 mg/dL can reduce overall mortality rate and blood-stream infections.7 Amino Acids Amino acids are crucial to making the structural components of all cells in the body and are essential for tissue turnover and repair. Each gram of amino acid is equal to 4 kcal. The protein requirements of neonates and children depend on age and weight (Table 4). The protein needs of pediatric patients are higher than those of the adult population when compared by body weight. Neonates also have higher demands as they are not able to fully synthesize all amino acids, making certain amino acids conditionally essential. To maintain growth rates similar to those in utero, low-birth-weight neonates need 2 to 4 g/kg per day of protein.9 Other populations requiring an increased amount of amino acids include patients with short bowel syndrome, stress, surgery, and wound healing. Potential complications and risks of providing IV amino acids include acidosis, elevated blood urea nitrogen, hyperammonemia, and cholestasis with prolonged administration. Inadequate supplementation of energy from carbohydrates and lipids results in protein breakdown for energy instead of growth. Generally, amino acids are started at 1 to 1.5 g/kg per day and advanced or weaned, depending on the serum blood urea nitrogen level and protein goals. Lipids Fats are provided in PN in the form of long-chain fatty acid emulsions. Several concentrations of lipid emulsion are available commercially; however, to conserve volume in the pediatric population and improve tolerance, clinicians use a 20% concentration. Twenty percent lipids are calorically dense, with each gram providing 10 kcal, and have a low osmolarity. In addition, they provide essential fatty acids, help decrease carbon dioxide production (compared to carbohydrates), and help maintain a net-nitrogen balance.7 The lipid requirements of neonates and children depend on age and weight (Table 5). Lipid needs are increased in the first 2 years of life, and enteral fat intake should be unrestricted in the infant diet. After the second year, many organizations recommend a slow transition from unrestricted dietary fat to a goal of less than 30% total fat and less than 10% saturated fat. Generally, lipids are initiated in PN at 1 g/kg per day and titrated toward the goal as tolerated by serum triglyceride levels. In the critical care patient, concomitant medications containing lipids must be considered in calculating caloric intake. For example, propofol provides 1.1 kcal/ mL from fat, and patients receiving propofol infusions should have that fat intake calculated into total fat intake. 455 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 455 15/10/12 3:24 PM G A R GAS Z A ACN Table 5: Estimates of Lipid Requirements for Healthy Pediatric Patientsa Age Lipid Requirements, g/kg per day Neonates and infants 3-4 Children aged ⬎1 y 2-3 a Data from Koletzko et al.7 A lipid intake of 0.1 to 0.25 g/kg per day is required to prevent essential fatty acid deficiency.7 However, complications can result from IV administration of lipids, such as hyperlipidemia, cholestasis, lipid overload syndrome with coagulopathy and liver failure, and potentially kernicterus in premature infants. Triglyceride levels (drawn via venipuncture, at the end of a lipid infusion after flushing the catheter, or from a separate central catheter) must be tested at least weekly to prevent or provide early identification of these complications. When triglyceride levels become elevated (⬎ 200 mg/dL), consider decreasing the daily dose and, if severely elevated (⬎ 300 mg/dL), omit lipids until levels return to normal. Micronutrients: Electrolytes, Vitamins, and Minerals In considering electrolytes provided in PN, a review of how the body uses them and what affects their serum values is warranted. Table 6 shows common starting ranges for varying age groups when initiating or reviewing electrolytes in PN. Electrolytes Sodium is pivotal to fluid and electrolyte balance and homeostasis of all systems in the body. It constitutes 90% to 95% of all solutes in extracellular fluid. Potassium is the main intracellular cation. It is required for neuromuscular function, metabolic activity, protein synthesis, and resting membrane potential. Acidosis shifts potassium out of the cell, and alkalosis will shift potassium into the cell. Calcium is important for normal blood clotting, cell membrane permeability, secretory behavior, and neuromuscular excitability. Calcium is bound to albumin. In patients with low album levels, either a corrected calcium value should be calculated ([4 ⫺ plasma albumin in g/dL] ⫻ 0.8 ⫹ serum calcium) or an ionized calcium level should be obtained. When converting a patient’s home PN to an inpatient order, occasionally a conversion from mEq to mg is required (1 mEq elemental calcium ⫽ 20 mg elemental calcium). Another important consideration with calcium in regard to PN is its precipitation with phosphate. Most hospitals use PN computer systems that will calculate the calcium and phosphorus curve or product to ensure that precipitation does not occur. The equation for determining calcium phosphorus ratio manually is as follows: calcium (mEq/L) ⫻ phosphorus (mmol/L) ⱕ 300. In the neonatal period, the optimal ratio of calcium to phosphorus in a range of 1.3 to 1.7 (mol/mol) should be provided to achieve adequate bone mineralization.7 Half of the body’s magnesium is in the skeleton, with the other half being intracellular in the heart, liver, and skeletal muscle. Magnesium activates coenzymes needed for carbohydrate and protein metabolism. In addition, normal magnesium levels are required to achieve calcium and potassium homeostasis. Phosphate is the major intracellular anion and is required for cell function and integrity. Normal values are age related as a result of Table 6: Daily Electrolyte and Mineral Requirements for Pediatric Patientsa,b Preterm Neonates Infants/Children Adolescents and Children, ⬎50 kg Sodium 2-5 mEq/kg 2-5 mEq/kg 1-2 mEq/kg Potassium 2-4 mEq/kg 2-4 mEq/kg 1-2 mEq/kg Electrolyte Calcium 2-4 mEq/kg 0.5-4 mEq/kg 10-20 mEq Phosphorus 1-2 mmol/kg 0.5-2 mmol/kg 10-40 mmol Magnesium 0.3-0.5 mEq/kg 0.3-0.5 mEq/kg 10-30 mEq Acetate and chloride a As needed to maintain acid-base balance Reprinted with permission from Mirtallo et al.8 b Assumes normal age-related organ function and normal losses. 456 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 456 15/10/12 3:24 PM VOL UME 2 3 • N U MBER 4 • OCTOBER–DECEM BER 2012 NE ONATA L A ND P E D IAT RIC PA RE NT E RA L NUT RIT ION Table 7: Phosphate Normal Ranges by Agea Age Normal Values, mg/dL Newborns 4.2-9 6 wk to 19 mo 3.8-6.7 19 mo to 3 y 2.9-5.9 3-15 y 3.6-5.6 ⬎15 y a 2.5-5 Data from Taketomo et al. 10 differences in the maturation of the renal system and the rate of bone growth and turnover (Table 7).10 Often laboratory test results report only the normal range for adults; therefore, pediatric normal ranges should be referenced, as normal ranges change with age. Trace Elements Trace elements are often included in standard PN formulas unless otherwise written to be omitted. Although the American Society for Parenteral and Enteral Nutrition (ASPEN) guidelines state that the recommended intakes of trace elements can be achieved only through the use of individualized trace element products, most institutions use commercially available combination products.8 The recommended daily intake of trace elements for pediatric patients (Table 8) can generally be obtained by providing the following amounts of the neonatal or pediatric parenteral trace element products: 0.25 mL/kg (neonatal product) for neonates weighing less than 1.5 kg, 0.2 mL/kg (neonatal product) for neonates weighing 1.5 kg to 10 kg, 2 mL (pediatric product) for pediatric patients weighing 10 kg to 20 kg, and 4 mL (pediatric product) for patients weighing more than 20 kg (Table 9).3 Trace elements commonly provided in PN include chromium, copper, manganese, and zinc. Selenium is not provided in most commercially available neonatal or pediatric trace element products and therefore must be provided either separately or by diluting the adult product. Current practice standards are to supplement 1 to 3 mcg/kg per day in infants and children who are exclusively being fed via PN for greater than 4 weeks or lowbirth-weight infants.7,8,13 Chromium mediates insulin reactions and is important for peripheral nerve function. Copper is important for transferrin and leukocyte production, as well as bone formation. Manganese is a cofactor in the production of many enzymes. As both copper and manganese are eliminated hepatically, serum levels should be obtained in patients with liver dysfunction, as these trace elements can accumulate and become toxic. Selenium helps prevent oxidative tissue damage and is important in thyroid metabolism. Finally, zinc is a cofactor in many enzymes, is critical for normal growth and immune functions, and maintains the integrity of skin and gastrointestinal tract mucosa. Premature and term infants often require extra supplementation of zinc in addition to what is provided via commercial trace element preparations (450500 mcg/kg per day for premature infants, 250 mcg/kg per day for infants younger than 3 months, 100 mcg/kg per day for infants 3 months and older) because of their rapid growth.7 In addition, zinc may need to be added for those patients with zinc losses from diarrhea or increased ostomy output. Vitamins Similar to trace elements, multivitamins are often standard in PN unless requested otherwise. The recommended daily intake of vitamins can Table 8: Trace Element Daily Requirements for Pediatricsa Preterm Neonates ⬍3 kg (mcg/kg per day) Term Neonates 3-10 kg (mcg/kg per day) Infants/Children 10-40 kg (mcg/kg per day) Zinc 400 50-250 50-125 2-5 mg Copper 20 20 5-20 200-500 mcg Trace Element Adolescents ⬎40 kg (per day) Manganese 1 1 1 40-100 mcg Chromium 0.05-0.2 0.2 0.14-0.2 5-15 mcg Selenium 1.5-2 2 1-2 40-60 mcg a Reprinted with permission from Mirtallo et al.8 457 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 457 15/10/12 3:24 PM G A R GAS Z A ACN intramuscularly 3 times weekly for 4 weeks in addition to what is provided in the PN solution for the VLBW infant. Table 9: Content of Neonatal/Pediatric Parenteral Trace Element Productsa Content per 1 mL (mcg) Trace Element Neonatal Trace Pediatric Trace Chromium 0.85 1 Copper 100 100 Manganese Zinc a 25 30 1500 500 Additional Additives A limited number of medications may be added directly to the PN formulation based on the needs of patients as well as stability and compatibility information in the PN solution. The medications most commonly added to 2-in-1 PN solutions are iron dextran, H2 antagonists, insulin, cysteine, carnitine, and heparin. Data from Multitrace-4 Neonatal11 and Trace elements injection 4.12 generally be obtained by providing the following amounts of the pediatric parenteral multivitamin product: 1.5 mL for patients weighing less than 1 kg, 3 mL for those weighing 1 kg to less than 3 kg, and 5 mL for those weighing 3 kg or more (Table 10).14 Vitamins included in PN include both fat-soluble vitamins (A, D, E, K) and water-soluble vitamins (C, B1,2,3,6,7,9,12). Some adult multivitamin products (generally used in patients older than 11 years) do not contain vitamin K, and therefore it must be added separately. Also, studies have shown a reduction in death and oxygen requirement in VLBW infants when additional vitamin A is supplemented (the number needed to treat to benefit is 13-20).15 On the basis of these studies, some centers provide 5000 U of vitamin A Iron Dextran Iron is not a current component of trace elements and is not routinely added to PN formulations.7–9 However, patients receiving long-term PN who are unable to tolerate or unable to absorb oral formulations (eg, short bowel syndrome) often require IV supplementation for iron-deficiency anemia. Intravenous iron in the form of iron dextran is the most common form used in PN because of its compatibility information, although literature is increasing about iron sucrose compatibility at certain concentrations in PN formulations. Iron dextran cannot be added to lipid emulsions or all-in-one mixtures because it destabilizes the emulsion. Dosing can be estimated on the Table 10: Content of Pediatric Parenteral Multivitamin Productsa Vitamin Content per 5 mL A 2300 IU D 400 IU E 7 IU K Importance/Function Immune function, respiratory benefits Maintains calcium and phosphorus homeostasis Antioxidant 200 mcg Regulates coagulation factors (VII, IX, X, II) B1 (thiamine) 1.2 mg Lipid synthesis, carbohydrate metabolism B2 (riboflavin) 1.4 mg Assists in energy metabolism B3 (niacin) 17 mg Involved with electron transport and metabolism B5 (pantothenic acid) 5 mg Precursor to coenzyme A, energy metabolism B6 (pyridoxine) 1 mg Metabolism of carbohydrates and amino acids, immune and neurological function B7 (biotin) 20 mg Cell growth, fatty acids, metabolism of lipids and amino acids 140 mcg Amino acid metabolism, synthesis of purines and pyrimidines, catabolism of histidine B9 (folic acid) B12 (cyanocobalamin) 1 mcg Synthesis of DNA nucleotides C (ascorbic acid) 80 mg Cofactor and antioxidant Abbreviation: IU, international unit. a Data from Infuvite Pediatric.14 458 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 458 15/10/12 3:24 PM VOL UME 2 3 • N U MBER 4 • OCTOBER–DECEM BER 2012 NE ONATA L A ND P E D IAT RIC PA RE NT E RA L NUT RIT ION basis of either weight and hemoglobin concentration or age and weight.10 A test dose must be given prior to the infusion to evaluate susceptibility to potential anaphylactic and other adverse reactions. Serum ferritin levels should be obtained every 1 to 3 months when providing ongoing IV supplementation to minimize the risk of iron overload. A theoretical concern with IV iron administration is that it may stimulate bacterial growth and impair immune function, thereby increasing the risk of infection by iron-requiring pathogens (Klebsiella, Pseudomonas, Salmonella, Yersinia, Listeria, Haemophilus influenzae, and Staphylococcus species).7,14 Iron facilitates viral replication and reverses the bactericidal effect of lactoferrin and lysozyme. However, certain aspects of the immune response, such as the generation of oxidative burst, are suppressed in iron deficiency, and numerous clinical studies have found no correlation between iron therapy and risk of death or infection.7,16 Heparin Catheter occlusion, dislodgement, and thrombosis are common complications associated with central venous catheters in the pediatric population, and these risks are even greater in neonates.7,17 Risk factors for these complications include younger age, wrist and scalp IV insertions, small-gauge catheters, low flow rates, turbulent flow, blood stasis, blood hyperviscosity, hypercoagulability, and the composition of the catheter.7,18 Heparin has been used prophylactically at a dose of 0.25 to 1 U/mL of PN solution by some centers to prolong the duration of catheter patency and prevent the incidence of catheter-related venous thrombosis in neonates with umbilical and central venous catheters.9,19,20 Several Cochrane Database reviews have investigated the use of continuous heparin infusion to prevent catheter occlusion and thrombosis. One review examined 3 randomized trials including 267 neonates with central venous catheters and found a reduced risk of catheter occlusion but no statistically significant decrease in thrombosis or catheter-related sepsis with a heparin dose of 0.5 U/kg per hour.17 Another review focusing on 10 studies involving peripheral IV catheter use in neonates found varying effects on catheter patency and therefore found no basis to recommend heparin usage for peripheral catheters.21 The European Society for Parenteral and Enteral Nutrition guidelines specifically recommend against heparin use in peripheral catheters.7 Heparin is also recommended at a dose of 1 U/mL of PN solution in the neonatal population to enhance the clearance of lipid emulsions. Heparin has been shown to increase lipoprotein lipase levels and lipolytic activity, thereby stabilizing triglyceride levels.9 Cysteine As recommended by manufacturers of neonatal and infant amino acid formulations, the current practice is to add cysteine (40 mg/g of amino acids) to 2-in-1 PN solutions just prior to administration for the first year of life because of immaturity of the synthesis pathway in this age group. The addition of cysteine decreases the pH, therefore improving the solubility of calcium and phosphorus.8 The European Society for Parenteral and Enteral Nutrition guidelines recommend a minimum intake of 30 to 55 mg/kg per day in infants and young children to maintain redox potential and calcium homeostasis.7 Carnitine Carnitine plays a role in the transport of longchain fatty acids to mitochondria for oxidation, thereby aiding fat metabolism.13 Primary carnitine deficiency has been associated with cholestasis and steatosis. Carnitine may be conditionally essential in neonates on longterm PN because of their low plasma and tissue concentrations at birth, immature conservation mechanisms, and biosynthetic capabilities.9,22 Carnitine also has been shown to increase lipid clearance and prevent hypertriglyceridemia in the neonatal population.9 Supplementing carnitine in the PN solution of patients receiving long-term PN can help mobilize hepatic fat stores and prevent steatosis and cholestasis.22 Typical dosing is either a bolus of 50 mg/kg per day for 3 days given when measured levels are low or prophylactically at a dose of 10 to 30 mg/kg per day.9,13,23 Insulin and H2 Antagonists Patients not at their goal dextrose caloric intake because of hyperglycemia may require the addition of insulin to their PN treatment regimen to continue to provide appropriate nutrition as well as avoid the complications associated with elevated glucose levels in patients with cardiac and infectious diseases. Caution is advised when determining the 459 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 459 15/10/12 3:24 PM G A R GAS Z A ACN amount of insulin to be added; Marcoud et al24 report that a higher percentage of insulin added to PN solution reaches the patient than previously published. Subcutaneous sliding scale insulin supplementation or a separate insulin infusion is always an option. For patients requiring stress ulcer prophylaxis or gastroesophageal reflux treatment with an H2 antagonist such as famotidine or ranitidine, clinicians may choose to discontinue the separate IV injection and instead add it to the PN solution to save nursing administration time. The benefits of these agents as well as proton pump inhibitors must be weighed against the growing literature for increased risk of pneumonia, necrotizing enterocolitis, and other infections associated with their use. Complications Hypertriglyceridemia and Essential Fatty Acid Deficiency Essential fatty acid deficiency, which causes platelet dysfunction, hair loss, poor wound healing, and dry scaly skin, can occur 2 to 4 weeks after the administration of a fat-free PN solution. It results from a failure to provide at least 2% to 4% of the total caloric intake as linoleic acid and 0.25% to 0.5% as ␣-linoleic acids.8 The European Society for Parenteral and Enteral Nutrition recommendations are to provide a minimum of 0.25 kg/kg per day of lipids to preterm infants and 0.1 g/kg per day to term infants and older children.7 Conversely, excessive or too rapid lipid intake can result in lipid overload syndrome. This syndrome is characterized by coagulopathies, elevated liver enzymes, hyperbilirubinemia, hepatomegaly, thrombocytopenia, and respiratory distress. In preterm neonates, tolerance of lipid emulsions is improved by infusing them over a 24-hour period. Parenteral nutrition– associated hypertriglyceridemia can also occur in pediatric patients with low birth weight and sepsis, which is usually due to excessive administration of lipids or uncontrolled hyperglycemia.9 As mentioned previously, the addition of heparin and carnitine to the PN solution can facilitate the clearance of lipids, therefore stabilizing serum triglyceride levels. Hyperglycemia in Neonates Hyperglycemia (plasma glucose ⬎ 150 mg/dL) occurs frequently in VLBW and premature neonates, especially during the first days of life.25 Physiological factors such as immaturity of the liver and pancreas, as well as saturation of insulin receptors, predispose the premature neonate to hyperglycemia. Other contributing factors, such as surgery, respiratory distress, and sepsis, can worsen hyperglycemia.9 Complications associated with hyperglycemia include retinopathy of prematurity, bronchopulmonary dysplasia (BPD), necrotizing enterocolitis, bacterial and fungal infections, intraventricular hemorrhage, longer hospital stays, and death.25 Treatment of hyperglycemia during PN use is targeted toward avoiding excess dextrose and providing IV fat emulsion, as insufficient evidence exists to show a higher versus lower glucose infusion rate has an impact.25,26 A recent Cochrane Database review evaluated 2 trials comparing insulin infusion with standard care and determined that the evidence did not support the routine use of insulin infusions to prevent hyperglycemia.25 The ASPEN guidelines also recommend against insulin use to prevent hyperglycemia; however, these guidelines state that insulin may be indicated for treatment of persistent hyperglycemia due to sepsis and medications.26 Metabolic Bone Disease Although more data exist in adults, metabolic bone disease has been reported in premature neonates and infants receiving long-term PN. This disorder is thought to be due to a combination of phosphorus, calcium, and vitamin D deficiencies, as well as aluminum accumulation. Patients with malabsorptive disorders, as well as those taking glucocorticoids and antineoplastic medications, may be at increased risk for metabolic bone disease. Although no specific treatment is available for this disorder, ASPEN guidelines suggest providing adequate amounts of calcium and phosphate in a ratio of 1:2 and measuring serum aluminum concentrations whenever unexplained metabolic bone disease is present.9 PN-Associated Cholestasis With a prevalence of 30% to 70% in infants, PN-associated cholestasis is diagnosed by a progressive rise in alkaline phosphatase and/or conjugated bilirubin (direct bili ⬎ 2 mg/dL).22 The exact cause is unknown, although several theories have been proposed, including a continuous PN maintaining a high insulin level and promoting a fatty liver, lipid intake greater than 1 g/kg per day, excessive or an imbalance of amino acids, and excess carbohydrates that 460 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 460 15/10/12 3:24 PM VOL UME 2 3 • N U MBER 4 • OCTOBER–DECEM BER 2012 NE ONATA L A ND P E D IAT RIC PA RE NT E RA L NUT RIT ION stimulate insulin. Insulin then stimulates enzymes involved in fatty acid synthesis. Cholestasis may progress to cirrhosis and liver failure if left untreated. Treatment of PN-associated liver disease or cholestasis includes cycling the PN over 12 to 20 hours, adding carnitine to the PN solution, initiating oral ursodiol, and providing as much enteral nutrition as tolerated. Cycling the PN by alternating periods of fasting and feeding allows for mobilization of fat during periods of fasting.23 Carnitine at a dose of 10 to 30 mg/kg per day, as discussed previously, can theoretically help mobilize fat stores. Ursodiol at a dose of 30 mg/kg per day works by reducing the secretion of cholesterol from the liver, reducing the cholesterol content of bile. It then becomes the predominant biliary acid, thus displacing potentially hepatotoxic bile salts. Catheter-Related Blood Stream Infections Because of the osmolarity of PN solutions, a central venous catheter is often required. Unfortunately, having a long-term central venous catheter predisposes patients to infection, especially those with short bowel syndrome and neonates with a birth weight of less than 1000 g.3 Emphasis should be placed on prevention of catheter-related infections by using aseptic technique, changing the infusion sets for amino acid and glucose infusions at least every 72 hours, and having a hang time of no more than 12 hours for IV fat emulsion.3,7 For patients on long-term cycled PN, ethanol locks may be more effective than heparin locks in preventing catheterrelated blood stream infections (CRBSIs) and possibly decrease the need for catheter replacement as well. A meta-analysis of ethanol locks for the prevention of CRBSIs including 53 patients aged 4 months to 21 years found that, compared with heparin locks, ethanol locks reduced the CRBSI rate by 81% and catheter replacements by 72%. The CDC recommends the use of ethanol locks in patients with longterm catheters who have a history of multiple CRBSIs despite aseptic technique.27 Further Considerations and Concerns Extracorporeal Membrane Oxygenation Extracorporeal membrane oxygenation (ECMO) is a treatment using an extracorporeal heart-lung machine with a membrane oxygenator provid- ing both cardiac and respiratory support. Indications for ECMO use in pediatric patients include congenital heart disease, persistent pulmonary hypertension, meconium aspiration, and congenital diaphragmatic hernia failing conventional ventilatory support. The patient being treated with ECMO typically receives fluid volume from multiple IV medications and infusions and may also require fluid restriction because of underlying pathophysiology, thereby leaving minimal volume available to provide the PN solution. Calcium supplementation may need to be reduced by half because of an alteration in calcium and vitamin D regulation in those receiving ECMO.3 In addition, ASPEN guidelines recommend that nutrition support be initiated expeditiously in ECMO patients, providing up to 3 g/kg per day protein and allowing the same caloric requirements as recommended for healthy neonates. Enteral feedings should be initiated when the patient is clinically stable. Care must be taken for the provision up to 3 g/kg per day protein for up to 3 weeks after a patient has been successfully weaned from ECMO as a result of a persistent catabolic state.3,28 Compatibility Patients receiving PN are frequently unable to tolerate oral feeds and oral medications, necessitating IV administration of medications. For patients with multiple-lumen catheters, this limitation is not a problem; however, for those patients with only 1 lumen, clinicians must consider the compatibility of the medication running via Y site into the same catheter as the PN solution. Table 11 lists compatibility information for many common medications coinfused via the Y site for both 2-in-1 and 3-in-1 PN solutions.29 Photoprotective Covering for Neonatal PN Exposure of PN solutions to light generates peroxides, which can cause oxidative stress in neonates, potentially leading to lung remodeling and an increased incidence of BPD. Shielding the PN solution from light may help decrease levels of peroxides and thus decrease the incidence of premature neonate complications such as BPD. One post hoc analysis, including 77 patients randomized to either light-protected or light-exposed PN, found a 30% reduction in BPD in those receiving light-protected PN, although results were not 461 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 461 15/10/12 3:24 PM G A R GAS Z A ACN Table 11: Y-Site Medication Compatibility With 2-in-1 and 3-in-1 PN Solutionsa (Continued) Table 11: Y-Site Medication Compatibility With 2-in-1 and 3-in-1 PN Solutionsa PN Solution Medication Acyclovir Amphotericin B Ampicillin Bumetanide PN Solution 2-in-1 3-in-1 I I Medication I I Mannitol C/I C Meperidine HCL C Meropenem C 2-in-1 3-in-1 C C C C NA C C C Calcium gluconate C C Mesna Cefazolin C/I C Methotrexate I C Methylprednisolone sodium succinate C C Metoclopramide I/C C Metronidazole C C Micafungin sodium C NA Midazolam I/C I Milrinone C NA Cefepime C NA Cefotaxime C C Ceftazidime C C Ceftriaxone C C Cefuroxime C C Ciprofloxacin I C Cisplatin I C Clindamycin C C Morphine sulfate (concentration 1 mg/mL) C C Cyclophosphamide C C Norepinephrine bitartrate C C Dexamethasone sodium phosphate C C Octreotide acetate C C Digoxin C C Ondansetron HCl C I Diphenhydramine C C Pentobarbital sodium C I Dobutamine C C Phenobarbital sodium C I Dopamine C C/I Phenytoin sodium I NA Epinephrine C NA Piperacillin sodium– tazobactam sodium C C Epoetin alfa C NA Potassium chloride C C Famotidine C C Potassium phosphate I I Fentanyl citrate C C Propofol C NA Fluconazole C C Ranitidine C C 5-Fluorouracil C/I C/I Sodium bicarbonate I/C C Furosemide C/I C Sodium nitroprusside C C Gentamicin sulfate C C Sodium phosphate I I Heparin sodium C I Tacrolimus C C Hydrocortisone sodium phosphate C C Tobramycin sulfate C C Hydromorphone C I/C Trimethoprimsulfamethoxazole C C Ifosfamide C C Vancomycin C C Imipenem-cilastatin C C Vecuronium bromide C NA Indomethacin I NA Zidovudine C C Insulin regular C C Leucovorin calcium C C Linezolid C NA Lorazepam C Magnesium sulfate C I C (continues) Abbreviations: C, compatible; C/I, conflicting compatibility, but strength of evidence supports compatibility; I, incompatible; I/C, conflicting compatibility and strength of evidence supports compatibility; IU, international units; NA, compatibility data not available; PN, parenteral nutrition, Y-site injection; drug administration via piggyback, IV push, or other IV methods at the Y-site injection port or other access port (ie, stopcock) between the PN solution and the central venous catheter. a Modified with permission from Mirtallo.29 462 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 462 15/10/12 3:24 PM VOL UME 2 3 • N U MBER 4 • OCTOBER–DECEM BER 2012 NE ONATA L A ND P E D IAT RIC PA RE NT E RA L NUT RIT ION statistically significant.30 Another study (retrospective analysis) reviewed the charts of 866 infants from 26 neonatal intensive care units comparing those receiving light-exposed PN and partial light-protected PN (bag covered, but tubing exposed). The incidence of BPD or death was 66% with the partial light-protected group versus 59% with the light-exposed group, revealing no association between lightprotected PN solution and BPD.31 Further studies are needed to adequately assess whether the cost associated with this practice is justified by the possible benefits. Aluminum Content Despite the Food and Drug Administration’s restriction of aluminum contamination of large-volume commercially available parenterals to less than 25 mcg/L, aluminum is found in small amounts in several components of the PN solution: amino acids, lipids, calcium, phosphate, heparin, vitamins, and trace elements. In addition, compounding bags and administration sets can contribute another 40% to these commercial products as a result of leaching.32 Accumulation from these sources can occur in the neonatal population as a result of impaired kidney function causing metabolic bone disease as well as central nervous system toxicity. Studies have shown that neonates receiving more than 5 mcg/kg per day of parenteral aluminum can have accumulations of toxic levels, leading to these complications. Although avoiding the administration of greater than 5 mcg/kg per day aluminum to neonates may be impossible, caution must be taken to minimize the amounts contained in the PN solution as much as possible. Suggested strategies include purchasing products with the lowest aluminum content (ie, calcium acetate instead of calcium gluconate) and washing out or flushing bags, burettes, and catheters with a few milliliters of sterile water before compounding.9,32,33 has published standards of practice for nutrition-support nurses that have the potential to be applied to critical care nursing as well.35 Some of these standards include participating in nutrition screening, assessment, management, and/or placement of appropriate enteral or vascular access devices; participating in the development of the patient’s individualized nutrition care plan; evaluating the patient’s nutritional goals and possible complications of care, and integrating research findings into practice.35 REFERENCES Conclusions Advanced registered nurse practitioners have played a major role in identifying, writing, and monitoring PN for critically ill neonatal and pediatric patients in many institutions. The role of clinical nurse specialists and other critical care nurses, however, is not well delineated in relation to optimizing nutrition, even though these nurses are well-positioned among the interdisciplinary critical care team.34 ASPEN 1. Dudrick SJ. History of parenteral nutrition. J Am Coll Nutr. 2009;28(3):225–243. 2. Parenteral Nutrition Fact Sheet ASPEN April 2012. http:// www.nutritioncare.org/About_ASPEN/What…/PN_Fact_ Sheet_April_2012. Accessed May 28, 2012. 3. Kamper C. Parenteral nutrition in the neonate. In: Richardson M, Chant C, Chessman KH, et al., eds. Pharmacotherapy Self-Assessment Program, Pediatrics. 7th ed. Lenexa, KS: American College of Clinical Pharmacy; 2010:127–142. 4. Fenton TR. A new growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr. 2003;3:13–22. 5. Massanari M, McLocklin A, Sayles R, Fariello A, Mueller Grinder D. Age-based competency assessment of pharmacists in pediatrics, part II: Application of developmental pharmacokinetics to pediatric pharmacy practice. J Pediatr Pharm Prac. 1997;2(3):139–157. 6. Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics. 1957;19:823–832. 7. Koletzko B, Agostoni C, Ball P, et al. ESPEN/ESPGHAN guidelines on paediatric parenteral nutrition. Clin Nutr. 2006;25:177–360. 8. Mirtallo J, Canada T, Johnson D, et al. Safe practices for parenteral nutrition. JPEN J Parenter Enteral Nutr. 2004; 28(6):S39–S70. 9. August D, Teitelbaum D, Albina J, et al. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr. 2002;26(1): S1–S137. 10. Taketomo CK, Hodding JH, Kraus DM. Pediatric Dosage Handbook. 18th ed. New York: Lexi Comp; 2011. 11. Multitrace-4 Neonatal [package insert]. Shirley, NY: American Regent; January 2009. 12. Trace elements injection 4, USP pediatric [package insert]. Shirley, NY: American Regent; January 2009. 13. Slicker J, Vermilyea S. Pediatric parenteral nutrition: putting the microscope on macronutrients and micronutrients. Nutr Clin Pract. 2009;24(4):481–486. 14. Infuvite Pediatric [package insert]. Boucherville, Quebec, Canada: Sandoz Canada Inc; September 2007. 15. Darlow BA, Graham BJ. Vitamin A supplementation to prevent mortality and short- and long-term morbidity in very low birthweight infants. [Review]. Update Cochrane Database Syst Rev. 2007;(4):CD000501; PMID:17943744. Cochrane Database Syst Rev. 2011;(10):CD000501. 16. Daquid E, Nakhla E, Sharma R. Is iron therapy for anemia harmful in the setting of infection? Cleve Clin J Med. 2011;78(3):168–170. 17. Shah PS, Shah VS. Continuous heparin infusion to prevent thrombosis and catheter occlusion in neonates with peripherally placed percutaneous central venous catheters (review). Cochrane Database Syst Rev. 2008;(2): CD002772. 463 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 463 15/10/12 3:24 PM G A R GAS Z A ACN 18. Tripathi S, Kaushik V, Singh V. Peripheral IVs: factors affecting complications and patency—a randomized controlled trial. J Infus Nurs. 2008;31(3):182–188. 19. Moreno Villares JM, Fernandez Shaw TC, Munoz Garcia MJ, Gomis Munoz P. Survey on parenteral nutrition preparation variability in pediatrics. Nutr Hosp. 2002;17(5): 251–255. 20. Ankola PA, Atakent YS. Effect of adding heparin in very low concentration to the infusate to prolong the patency of umbilical artery catheters. Am J Perinatol. 1993;10(3): 229–232. 21. Shah PS, Ng E, Sinha AK. Heparin for prolonging peripheral intravenous catheter use in neonates. Cochrane Database Syst Rev. 2005;(4):CD002774. 22. Kumpf V. Parenteral nutrition–associated liver disease in adult and pediatric patients. Nutr Clin Pract. 2006;21(3): 279–289. 23. Jeejeebhoy K. Management of PN-induced cholestasis. Pract Gastroenterol. 2005;24:62–68. 24. Marcoud SP, Dunham B, Hobbs A, Caro JF. Availability of insulin from total parenteral nutrition. JPEN J Parenter Enteral Nutr. 1990;14(3):262–264. 25. Sinclair JC, Bottino M, Cowett RM. Interventions for prevention of neonatal hyperglycemia in very low birth weight infants. Cochrane Database Syst Rev. 2011;(10):CD007615. 26. Arsenault D, Brenn M, Kim S, et al. ASPEN clinical guidelines: hyperglycemia and hypoglycemia in the neonate receiving parenteral nutrition. JPEN J Parenter Enteral Nutr. 2012;36(1):81–95. 27. Oliveira C, Nasr A, Brindle M, Wales PW. Ethanol locks to prevent catheter-related bloodstream infections in 28. 29. 30. 31. 32. 33. 34. 35. parenteral nutrition: a meta-analysis. Pediatrics. 2012; 129(2):319–329. Jaksic T, Hull M, Modi BP, et al. ASPEN clinical guidelines: nutrition support of neonates supported with extracorporeal membrane oxygenation. JPEN J Parenter Enteral Nutr. 2010;34(3):247–253. Mirtallo J. Assessment Tools and Guidelines: Parenteral Nutrition Therapy. Cleveland, OH: McMahon Publishing; 2008. Chessex P, Harrison A, Khashu M, Lavoie JC. In preterm neonates, is the risk of developing bronchopulmonary dysplasia influenced by the failure to protect total parenteral nutrition from exposure to ambient light? J Pediatr. 2007;151:213–214. Sherlock R, Chessex P. Shielding parenteral nutrition from light: does the available evidence support a randomized, controlled trial? Pediatrics. 2009;123(6): 1529–1532. de Oliveira SR, Bohrer D, Garcia SC, Cicero do Nascimento P, Noremberg S. Aluminum content in intravenous solutions for administration to neonates: role of product preparation and administration methods. JPEN J Parenter Enteral Nutr. 2010;34(3):322–328. Charney PJ. ASPEN statement on aluminum in parenteral nutrition solutions. Nutr Clin Pract. 2004;19:416–417. Marshall AP, Cahill NE, Gramlich L, MacDonald G, Alberda C, Heyland D. Optimizing nutrition in intensive care units: empowering critical care nurses to be effective agents of change. Am J Crit Care. 2012;21(3):186–194. DiMaria-Ghalili RA, Bankhead R, Fisher AA, Kovacevich D, Resler R, Guenter PA. Standards of practice for nutrition support nurses. Nutr Clin Pract. 2007;22:458–465. 464 Copyright © 2012 American Association of Critical-Care Nurses. Unauthorized reproduction of this article is prohibited. NCI200234.indd 464 15/10/12 3:24 PM