Opportunistic Infections
advertisement

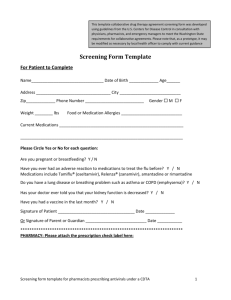
Opportunistic Infections Objectives: After reviewing this material and attending lecture, the student should be able to 1) Define an opportunistic infection (OI). 2) Recommend an appropriate treatment for the following OIs, given diagnosis and relevant patient information a. PCP b. Toxoplasmosis c. MAC disease d. Cryptococcal Meningitis e. Histoplasmosis f. Cryptosporidiosis g. Microsporidiosis h. Coccidioidomycosis 3) Recommend appropriate primary or secondary prophylaxis, if given relevant information for a patient. 4) Identify monitoring parameters to evaluate the patient’s treatment for a given OI. 1) Definition a) Opportunistic infection (OI) = “infection that occurs in persons with weak immune systems” b) Examples of persons at risk for OIs • HIV/AIDS • Cancer • Immunosuppressive drugs ◊ Long-term, high-dose corticosteroids ◊ Chemotherapy ◊ Immunosuppressive drugs used for stem cell and organ transplants c) Examples of OIs • Bacterial pneumonias • Pneumocystis jiroveci pneumonia • Histoplasmosis • Tuberculosis • Syphilis • Mucocutaneous candidiasis • Aspergillosis • Cryptosporidiosis • Mycobacterium avium complex disease • Cryptococcus • Cytomegalovirus (CMV) disease • Hepatitis B and C 2) Treatment versus prophylaxis a) Prophylaxis = trying to prevent disease for which the patient is at risk • Primary prophylaxis ◊ Patient has never had the disease before • Secondary prophylaxis ◊ Patient has had disease before but wish to prevent recurrence of disease b) Treatment = eradicate/control organism causing infection and eliminating signs and symptoms of disease 3) Pneumocystis jiroveci pneumonia (PCP) a) Cause • Pneumocystis jiroveci (fungal organism) • Previously called P. carinii b) Transmission • Usually occurs due to a latent infection that is reactivated • Airborne transmission (?) c) Signs/symptoms • 90% of cases in those with CD4< 200 cells/µL or CD4< 15% • Progressive over days to weeks ◊ Exertional dyspnea ◊ Fever ◊ Nonproductive cough • Labs ◊ PaO2 at room air ♦ PaO2 > 70 mm/Hg: mild-to-moderate PCP ♦ PaO2 < 70 mm/Hg: severe PCP ◊ LDH > 500 mg/dL ◊ Chest X-ray ♦ Early on, X-ray will appear normal ♦ Later in disease, will see diffuse, bilateral infiltrates; no cavitation or pleural effusion ◊ CT scan ♦ Ground-glass attenuation ♦ Usually will show abnormalities that are not seen on X-ray with mild to moderate cases d) Diagnosis • Culture of organisms ◊ Bronchoalveolar lavage fluid (BALF) ◊ Induced sputum • Sensitivity of culture depends on method used and technique ◊ Induced sputum: < 50% - >90% ◊ Bronchoscopy with BALF: 90 – 99% ◊ Transbronchial biopsy: 95 – 100% ◊ Open lung biopsy: 95 – 100% e) Treatment • Length of therapy (LOT): 21 days, regardless of antibiotic regimen chosen First-Line Therapies Alternative Therapies Trimethoprim-sulfamethoxazole (TMP-SMX) Pentamidine (severe cases) Dosing is based on trimethoprim component 4 mg/kg IV qday 15 – 20 mg/kg/day IV or PO ÷ 3- 4 doses (q6h – q8h dosing) PO dose usually works out to be TMP/SMX DS 2 tabs TID Corticosteroids Primaquine and clindamycin (mild to moderate cases) Indicated only for severe cases of PCP P 15 – 30 mg base PO qday + C 300 – 450 mg PO qday ÷ 3 – 4 doses Prednisone 40 mg BID x 5 days (If consider IV clindamycin, dose is 600 – 900 mg/day ÷ 3 – 4 doses) Prednisone 40 mg qday x 5 days Prednisone 20 mg qday x 11 days (IV methylprednisolone = 75% of PO prednisone dose) Dapsone and trimethoprim (mild to moderate cases) D 100 mg PO qday + T 15 mg/kg/day ÷ 3 doses (PO) Trimetrexate and leucovorin (mild to moderate cases) T 1.2 mg/kg (45 mg/m2) IV qday + L 0.5 mg/kg (20 mg/m2) IV or PO qday Leucovorin should be continued for 3 days after end of trimetrexate treatment Atovaquone (mild cases) 750 mg PO BID with food f) Prophylaxis First-Line Therapies Trimethoprim-sulfamethoxazole (TMP-SMX) TMP-SMX DS 1 tab qday Trimethoprim-sulfamethoxazole (TMP-SMX) TMP-SMX SS 1 tab qday Alternative Therapies Dapsone 50 mg PO BID or 100 mg PO qday Atovaquone 1500 mg PO qday Trimethoprim-sulfamethoxazole (TMP-SMX) TMP-SMX DS 3x/ week Dapsone and Pyrimethamine and Leucovorin D 50 mg PO qday + P 50 mg PO qweek + L 25 mg PO qweek OR D 200 mg PO + P 75 mg PO + L 25 mg PO, all qweek (Consider if intolerant of TMP-SMX and want to cover toxoplasmosis as well) Pentamidine, aerosolized 300 mg q month (nebulized with Respirgard nebulizer) When to start? ◊ Primary prophylaxis ♦ CD4< 200 cells/µL ♦ CD4% < 14% ♦ Diagnosis of oropharyngeal candidiasis ♦ History of AIDS-defining illness ◊ Secondary prophylaxis ♦ After completion of treatment therapy for PCP • When to stop? ◊ Primary prophylaxis ♦ CD4 > 200 cells/µL for > 3 months ◊ Secondary prophylaxis ♦ CD4 increase from < 200 cells/µL to > 200 cells/µL for > 3 months due to HAART ♦ Consider for life if PCP episode at CD4 > 200 cells/µL Monitoring • Disease ◊ Should see improvement in 4 – 8 days in ABGs, pulmonary function ♦ If lack of improvement, consider adding to a regimen or switching regimen ♦ If patient is not on corticosteroids, patient may worsen initially in 3 – 5 days due to inflammatory response (i) Should still wait up to 8 days to monitor progress ♦ If fail TMP-SMX for moderate-to-severe cases, consider using (i) Pentamidine (ii) Primaquine + clindamycin (iii) Trimetrexate + leucovorin + dapsone (iv) No data has evaluated which one of these options is the best to switch to after TMP-SMX failure ♦ If fail TMP-SMX for mild cases, consider using (i) Atovaquone • Drugs: See Table 1 at end of notes • g) 4) Toxoplasmosis a) Cause • Toxoplasma gondii b) Transmission • Primary infection ◊ eating undercooked meat with tissue cysts ◊ exposure from cat feces • Disease usually result of reactivation of latent tissue cysts c) Signs/symptoms • Usually seen in patients with CD4 < 100, with greatest risk at CD4 < 50 • Primary infection may either be acute cerebral disease (encephalitis) or disseminated disease • Encephalitis (most common presentation) ◊ Headache ◊ Confusion ◊ Motor weakness ◊ Fever ◊ Without treatment, disease will progress to seizures, stupor, and coma ◊ Physical exam/ laboratory findings ♦ Focal neurological abnormalities ♦ CT scan/ MRI (i) Multiple contrast-enhancing lesions, often with edema • Disseminated disease ◊ Retinochoroiditis ◊ Pneumonia ◊ Multifocal organ system failure d) Diagnosis • Immunological studies ◊ Anti-toxoplasma IgG antibody positive ◊ Lack IgM antibodies • Definitive diagnosis ◊ Immunological studies AND ◊ Compatible clinical syndromes AND ◊ Identification of one or more mass lesions on CT, MRI OR ◊ Detection of organism in clinical sample ♦ Requires brain biopsy ◊ Some may choose to use first three criteria after eliminating all other causes in the differential diagnosis, only choosing to do brain biopsy with failure to respond to therapy • PCR of CSF ◊ High specificity, low sensitivity ◊ Once therapy started, will have negative results e) Treatment • LOT > 6 weeks First-Line Therapies Alternative Therapies Pyrimethamine and sulfadiazine and leucovorin Pyrimethamine and leucovorin and clindamycin P 200 mg PO x 1, then P 200 mg PO x 1, then If weight < 60 kg: If weight < 60 kg: P 50 mg PO qday + S 1,000 mg q6h + L 10 -20 mg P 50 mg PO qday + L 10 -20 mg qday + C 600 mg IV or PO q6h qday If weight > 60 kg: If weight > 60 kg: P 75 mg PO qday + L 10 -20 mg qday + C 600 mg IV or PO q6h P 75 mg PO qday + S 1,500 mg q6h + L 10 -20 mg (leucovorin may be increased up to > 50 mg) qday (leucovorin may be increased up to > 50 mg) Trimethoprim-sulfamethoxazole 5 mg/kg TMP IV or PO BID Atovaquone and pyrimethamine and leucovorin P 200 mg PO x 1, then If weight < 60 kg: A 1500 mg PO BID + P 50 mg PO qday + L 10 -20 mg qday If weight > 60 kg: A 1500 mg PO BID + P 75 mg PO qday + L 10 -20 mg qday (leucovorin may be increased up to > 50 mg) First-Line Therapies, continued Alternative Therapies, continued Atovaquone and sulfadiazine A 1500 mg PO BID and S 1,000 – 1,500 mg PO q6h Atovaquone 1500 mg BID with meals Pyrimethamine and leucovorin and azithromycin P 200 mg PO x 1, then If weight < 60 kg: P 50 mg PO qday + L 10 -20 mg qday + A 900 – 1200 mg PO qday If weight > 60 kg: P 75 mg PO qday + L 10 -20 mg qday + A 900 – 1200 mg PO qday (leucovorin may be increased up to > 50 mg) ◊ In addition to above therapies, may consider use of dexamethasone to avoid brain damage due to edema ♦ Must consider effect of edema vs. effect of immunosuppression due to corticosteroids ♦ D/C as soon as possible ◊ Antiseizure medications should be used in those patients with a history of seizures f) Prophylaxis • Primary prophylaxis ◊ What to start? First-Line Therapies Alternative Therapies Trimethoprim-sulfamethoxazole (TMP-SMX) Trimethoprim-sulfamethoxazole (TMP-SMX) TMP-SMX DS 1 tab qday TMP-SMX SS 1 tab qday (Will provide coverage for both toxoplasmosis and PCP) Dapsone and Pyrimethamine and Leucovorin D 50 mg PO qday + P 50 mg PO qweek + L 25 mg PO qweek OR D 200 mg PO + P 75 mg PO + L 25 mg PO, all qweek (Consider if intolerant of TMP-SMX and want to cover PCP as well) Atovaquone 750 mg PO q6-12h + (pyrimethamine 25 mg PO qday and leucovorin 10 mg PO qday) (Reserve as last line therapy; use only if other options are not feasible) ◊ When to start? ♦ Must be IgG Ab+ to T. gondii ♦ CD4 < 100 cells/µL ♦ If restarting, consider at CD4 < 100 – 200 cells/µL ◊ When to stop? ♦ CD4 > 200 cells/µL increase for > 3 months due to HAART ◊ Other considerations ♦ For those patients who are IgG negative, counsel on avoiding environmental exposure (i) No raw/undercooked meats (ii) Hand washing after meat preparation and gardening (iii) Avoid changing cat litter • Secondary prophylaxis ◊ What to start? First-Line Therapies Alternative Therapies Sulfadiazine and Pyrimethamine and Leucovorin Clindamycin and Pyrimethamine and Leucovorin S 500 – 1,000 mg PO 4x/day + P 25 – 50 mg PO qday + C 300 – 450 mg PO q6-8h + P 25 – 50 mg PO qday + L 10 – 25 mg PO L 10 – 25 mg PO qday qday Atovaquone 750 mg PO q6-12h + (pyrimethamine 25 mg PO qday and leucovorin 10 mg PO qday) (Reserve as last line therapy; use only if other options are not feasible) When to start? ♦ After completion of initial treatment ♦ If stopped, restart if CD4 < 200 cells/µL ◊ When to stop? ♦ May consider after (i) Successful completion of initial therapy (ii) Asymptomatic (iii) Sustained increase of CD4 > 200 cells/µL after HAART for > 6 months Monitoring • Disease ◊ Clinical and radiological improvement ◊ Antibody titer changes are not helpful in monitoring therapy ◊ Failure ♦ Clinical, radiological deterioration within first week with adequate therapy ♦ No clinical improvement seen within 2 weeks (i) If not done previously, consider brain biopsy: if histopathologically confirmed, switch to alternative regimen ◊ Recurrence is unusual as long as patient is compliant with therapy • Drugs: See Table 1 at end of notes ◊ g) 5) Mycobacterium avium complex (MAC) disease a) Cause • Mycobacterium avium b) Transmission • Present in the environment, with prevalence varying in geographic region • Infection due to inhalation, ingestion, or inoculation through respiratory or GI tract • Unlikely transmission is person-to-person c) Signs/ symptoms • Persons with CD4 < 50 cells/µL most at risk • May manifest in several different ways ◊ Disseminated multiorgan infection ◊ Immune reconstitution inflammatory syndrome (IRIS) ◊ Localized syndromes ♦ Cervical or mesenteric lymphadenitis ♦ Pneumonitis ♦ Pericarditis ♦ Osteomyelitis ♦ SSTI with abscesses ♦ Genital ulcers ♦ CNS infection • Immune reconstitution inflammatory syndrome ◊ Focal lymphadenitis ◊ Fever ◊ No bacteremia ◊ Inflammatory response that is indistinguishable from active disease ◊ Usually seen in those with subclinical or established MAC disease along with advanced immunosuppression and are started on HAART with rapid increased in CD4 ♦ May be benign, self-limiting OR may be severe and require systemic anti-inflammatory therapy (i) NSAID or systemic corticosteroid therapy x 4 – 8 weeks • Disseminated multiorgan infections ◊ Early symptoms may be minimal, present before disease is actually detectable ♦ Fever ♦ Night sweats ♦ Weight loss d) e) f) ♦ Fatigue ♦ Diarrhea ♦ Abdominal pain ◊ Laboratory findings ♦ Anemia ♦ Elevated alkaline phosphatase ◊ Physical exam ♦ Hepatomegaly ♦ Splenomegaly ♦ Lymphadenopathy Diagnosis • Confirmed diagnosis ◊ Compatible clinical signs and ◊ Isolate of MAC from cultures of blood, bone marrow, other sterile tissues or body fluids • Other helpful tests ◊ AFB smear ◊ Culture of stool or biopsy of material from tissue or organ ◊ Radiographic imaging of abdomen or mediastinum for detection of lymphadenopathy Treatment • LOT: Lifelong therapy unless patient with sustained immune recovery on HAART • All initial therapies for treatment must include at least TWO drugs from different classes ♦ Consider increasing number of drugs to three or four for patients with advanced immune suppression (CD4 < 50 cells/µL), high mycobacterial loads (> 102 cfu/ mL of blood), or absence of effective HAART First-Line Therapies Alternative Therapies Additional Drugs to Consider Adding Clarithromycin Azithromycin Rifabutin 500 mg PO BID 500 – 600 mg PO qday 300 mg PO qday Ethambutol Ciprofloxacin 15 mg/kg PO qday 500 -750 mg PO qday Levofloxacin 500 mg PO qday Amikacin 10 – 15 mg/kg IV qday Prophylaxis • Primary prophylaxis ◊ What to start? First-Line Therapies Alternative Therapies Azithromycin Rifabutin 1200 mg PO qweek 300 mg PO qday Clarithromycin Azithromycin and rifabutin 500 mg PO BID A 1200 mg PO qday + R 300 mg PO qday ◊ When to start? ♦ CD4 < 50 cells/µL ♦ If restarting, consider with CD4 < 50 -100 cells/µL ◊ When to stop? ♦ CD4 increase to > 100 cells/µL for > 3 months due to HAART • Secondary prophylaxis ◊ What to start? First-Line Therapies Alternative Therapies Clarithromycin and ethambutol (and rifabutin) Azithromycin and ethambutol (and rifabutin) C 500 mg PO BID + E 15 mg/kg PO qday + R 300 mg PO A 500 mg PO qday + E 15 mg/kg PO qday + R 300 mg PO qday qday When to start? ♦ Continuation of initial therapy ♦ Restart when CD4 < 100 cells/µL ◊ When to stop? ♦ May be at low risk for MAC if (i) Completed treatment course of > 12 months (ii) Asymptomatic (iii) CD4 > 100 cells/µL for > 6 months due to HAART Monitoring • Disease ◊ Improvement of fever, mycobacterial load in blood or tissue seen within 2 – 4 weeks ♦ May be delayed with more extensive disease or advanced immunosuppression ◊ Blood cultures should be taken at 4 – 8 weeks if fail to have clinical response to appropriate therapy ♦ Isolates from cultures should be tested for susceptibility to clarithromycin and azithromycin, as well as ethambutol, rifabutin, ciprofloxacin, levofloxacin, amikacin ◊ Treatment failure ♦ Construct new multidrug regimen of at least two susceptible drugs (i) Do not use clofazimine, even if susceptible (increased risk of death) ♦ Optimized HAART ♦ Not enough data to support the use of immunomodulators for adjunctive treatment, but may be considered after failing all other antimycobacterial treatments • Drugs: See Table 1 at end of notes ◊ g) 6) Cryptococcal meningitis a) Cause • Cryptococcus neoformans var neoformans • Cryptococcus neoformans var. gattii • Cryptococcus neoformans var. grubii b) Transmission • Ordinarily found in soil • Inhalation of fungus c) Signs/ symptoms • Those most at risk have CD4 < 50 cells/µL • Most cases present as meningitis, but up to ½ have disseminated disease with pulmonary involvement, presenting with cough, dyspnea, abnormal chest X-ray • Meningitis presentation ◊ Fever ◊ Malaise ◊ Headache ◊ Neck stiffness (one-fourth to one-third of cases) ◊ Photophobia ◊ Lethargy ◊ Altered mentation ◊ Personality changes ◊ Memory loss • Laboratory and Physical Examination ◊ CSF ♦ Mildly elevated serum protein ♦ Normal or slightly low glucose ♦ Few lymphocytes ♦ Elevated opening pressure (>200 mm of water) ◊ Blood culture – up to 75% positive in meningitis d) Diagnosis • Cryptococcal antigen in CSF positive • Serum cryptococcal antigen also usually positive e) Treatment • Persons most at risk have CD4 < 50 cells/uL • If left untreated, outcome is fatal • First-line therapy for meningitis First-Line Therapies INDUCTION THERAPY x 2 weeks Amphotericin B deoxycholate + flucytosine A 0.7 mg/kg/day IV q24h + F 25 mg/kg PO 4x/day Liposomal amphotericin B + flucytosine LA 4 mg/kg/day IV q24h + F 25 mg/kg PO 4x/day f) Alternative Therapies (for mild to moderate disease) INDUCTION THERAPY x 2 weeks Amphotericin B 0.7 mg/kg/day IV Fluconazole + flucytosine Flucon 400 – 800 mg/day (PO or IV) + Flucyto 25 mg PO 4x/day (This regimen should be used for 4 – 6 weeks) CONSOLIDATION THERAPY x at least 8 weeks Fluconazole 400 mg PO qday CONSOLIDATION THERAPY x at least 8 weeks Itraconazole 200 mg PO BID CHRONIC MAINTENANCE THERAPY Fluconazole 200 mg PO qday CHRONIC MAINTENANCE THERAPY Itraconazole 200 mg PO qday Prophylaxis • Primary prophylaxis ◊ Not recommended ◊ If used, may consider using fluconazole 100 -200 mg qday for patients with CD4 < 50 cells/µL • Secondary prophylaxis ◊ What to start? First-Line Therapies Alternative Therapies Fluconazole Amphotericin B 200 mg PO qday 0.6 – 1.0 mg/kg IV weekly – three times/week Itraconazole 200 mg qday ◊ When to start? ♦ After completion of initial therapy ♦ Restart if CD4 < 100 – 200 cells/µL ◊ When to stop? ♦ May be at low risk for cryptococcal meningitis if (i) Successfully completed a course of initial therapy (ii) Remain asymptomatic (iii) > 6 month increase in CD4 > 100 – 200 cells/µL ♦ Some HIV specialists would prefer an LP with culture-negative results for CSF g) Monitoring • Disease ◊ New symptoms, clinical findings after 2 weeks of treatment ♦ Consider repeat LP (i) Measure opening pressure ◊ Failure with fluconazole due to resistance rare ♦ Check that fluconazole dosing is appropriate and consider increasing and/or adding flucytosine ♦ Consider switching to amphotericin B + flucytosine ♦ Voriconazole may be an alternative For those patients that have relapse ♦ Must perform fungal culture (i) Serum CrAg not reliable to indicate if disease or not in those that have been previously diagnosed (ii) Consider relapse if increase in titer of 2 dilutions in comparison to convalescence CSF CrAg ♦ Evaluate for relapse vs. IRIS, especially if HAART started recently (usually within past 6 weeks but up to several months) ◊ Consider resistance testing in patients with multiple recurrences in patients with adherence to therapy Drugs: See Table 1 at end of notes ◊ • 7) Histoplasmosis a) Cause • Histoplasma capsulatum b) Transmission • Inhalation of organisms • May be reactivation of latent infection in some patients • Endemic in Ohio and Mississippi River valleys, mostly central and southeastern states; Puerto Rico ◊ Exposure to soil c) Signs/ Symptoms • Those most at risk for disseminated disease for CD4 < 150 cells/µL • Localized pulmonary infections tend to occur in immunocompetent patients (CD4 > 300 cells/µL) • Disseminated disease presentation ◊ Fever ◊ Fatigue ◊ Weight loss ◊ Up to 50% will have respiratory symptoms ♦ Cough ♦ Chest pain ♦ Dyspnea ◊ Less than 10% will present with septic shock, CNS, GI, or cutaneous manifestations • Severe disseminated cases (meet one or more selected criteria) ◊ Temperature 102ºF ◊ SBP < 90 mmHg ◊ pO2 < 70 torr ◊ Weight loss > 5% ◊ Karnofsky performance score < 70 ◊ Hemoglobin <10 g/dL ◊ Neutrophil count < 1000 cells/µL ◊ Platelet count < 100,000 cells/µL ◊ AST > 2.5 times normal ◊ Bilirubin > 2 times normal ◊ Creatinine > 2 times normal ◊ Albumin < 3.5 g/dl ◊ Coagulopathy ◊ Presence of other organ system dysfunction ◊ Confirmed meningitis d) Diagnosis • Histoplasma antigen in blood or urine ◊ 95% sensitive in urine, 85% sensitive in serum ◊ Sensitive for disseminated histoplasmosis ◊ Insensitive for pulmonary infection • May be isolated from blood, bone marrow, respiratory secretions, localized lesions ◊ Usually takes 2 – 4 weeks e) Treatment • Severe cases First-Line Therapies ACUTE PHASE (3 – 10 days or until clinically improved) Amphotericin B deoxycholate A 0.7 mg/kg/day IV q24h Liposomal amphotericin B LA 4 mg/kg/day IV q24h CONTINUATION PHASE (12 weeks) Itraconazole 200 mg PO BID Alternative Therapies ACUTE PHASE (3 – 10 days or until clinically improved) Itraconazole 400 mg IV qday CONTINUATION PHASE (12 weeks) Itraconazole oral solution 200 mg PO BID Fluconazole 800 mg PO qday Less severe cases First-Line Therapies Alternative Therapies Itraconazole Fluconazole 200 mg PO TID x 3 days, then 200 mg PO BID x 12 weeks 800 mg PO qday x 12 weeks • Meningitis ◊ Amphotericin B deoxycholate or liposomal for 12 – 16 weeks, then continue high dose fluconazole for at least 9 – 12 months • Disease in patients with CD4 > 500 cells/µL ◊ Consider treating as would be managed in an immunocompetent host f) Prophylaxis • Primary prophylaxis ◊ Not routinely recommended ◊ Should consider for patients that meet the following criteria ♦ CD4 < 100 cells/uL ♦ At high risk (i) Because of occupational exposure OR (ii) Live in community with hyperendemic rate of histoplasmosis (>10 cases/ 100 patient-years) ◊ Persons with CD4 < 200 cells/µL do not necessarily need to be prophylaxed but should consider avoiding activities with an increased risk ♦ Creating dust with working with surface soil ♦ Cleaning chicken coops heavily contaminated with droppings or disturbing soil beneath bird roosting sites ♦ Cleaning, remodeling, or demolishing old buildings ♦ Spelunking ◊ Therapies ♦ Itraconazole 200 mg PO qday • Secondary prophylaxis ◊ What to start? First-Line Therapies Alternative Therapies Itraconazole Amphotericin B 200 mg PO BID 50 mg IV 1-2x/week (~ 0.7 mg/kg/day) ◊ When to start? ♦ After completion of treatment phase ◊ When to stop? ♦ Not recommended at this time. g) Monitoring Parameters • Diseases ◊ Monitor Histoplasma Ag every 3 – 6 months during therapy for evidence of continuing suppression ♦ If on fluconazole, at least every 4 months, especially monitoring for possible increase due to resistance • Drugs: See Table 1 at end of notes • 8) Cryptosporidiosis a) Cause • Cryptosporidium hominis • C. parvum • C. melagridis b) Transmission • Ingestion of Cryptosporidium oocysts ◊ Contaminated water supplies ◊ Oral-anal sex ◊ Child-to-adult through diapering c) Signs/ Symptoms • Persons with CD4< 100 cells/ µL at greatest risk • Acute or subacute onset of profuse, nonbloody watery diarrhea • N/V • Lower abdominal cramping • Fever • Prolonged disease can lead to cholangitis, pancreatitis d) Diagnosis • Microscopic ID of oocysts in stool or tissue e) Treatment • First-line therapy ◊ Immune restoration with HAART ◊ Supportive therapy for fluid losses through diarrhea ♦ Antimotility agents not consistently effective • Alternatives (Not routinely used or recommended) ◊ Nitazoxanide 500 mg PO BID ♦ Short-term study showed increased cure rates compared with controls in patients with CD4 > 50 cells/µL ♦ Package insert states “have not been shown to be superior to placebo for treatment of diarrhea caused by Cryptosporidium parvum in HIV-infected or immunodeficient patients.” ◊ Paromomycin 25 – 35 mg/kg PO ÷ 2 – 4 doses ♦ May have good initial response, but high rate of relapse ♦ Safe, but probably not effective f) Prevention • No drug regimen is effective in prevention • Best way is to avoid exposure ◊ Avoid contact with human and animal feces. ♦ Avoid sexual practices that might result in oral exposure to feces. ◊ Practice good hygiene during activities that may put one at risk. ♦ Wash hands after diaper changing, handling pets, and after gardening or other exposure to soil. ◊ Avoid drinking water directly from lakes or rivers. ◊ Avoid swimming in areas known to be contaminated and avoid swallowing water when swimming. ◊ Boil water in outbreaks before using or consider consuming other beverages during this time. ◊ Avoid food that may be contaminated. ♦ Raw oysters g) Monitoring • Disease ◊ Signs/ symptoms of volume depletion, electrolyte and weight loss, malnutrition ◊ Treatment failure ♦ Optimize HAART ♦ Continue supportive treatment • Drugs: See Table 1 at end of notes 9) Microsporidiosis a) b) c) d) e) f) Causes • Encephalitozoon spp. • Enterocytozoon spp. • Trachipleistophora spp. • Pleistophora spp • Microsporidium spp • Nosema spp. • Brachiola spp. Transmission • Ubiquitous in the environment • Zoonotic and/or waterborne origins • May be asymptomatic carriers Signs/symptoms • Persons most at risk are those with CD4 < 100 cells/µL • Diarrhea (most common symptom) • Others include (dependent on infecting organism) ◊ Encephalitis ◊ Ocular infection ◊ Sinusitis ◊ Myositis ◊ Disseminated infection Diagnosis • Demonstration of organisms by light or electron microscope examination of clinical specimens (including stood, duodenal aspirate, urine, sputum, nasal discharge, BALF, conjunctival discharge) • Urine cultures will isolate Trachipleistophora species • All may be cultured in vitro except E. bieneusi Treatment • First-line therapies ◊ Immune reconstitution with ART ◊ Supportive treatment for those with diarrhea and wasting ◊ For disseminated infections (not ocular), intestinal infections ♦ Albendazole 400 mg PO BID (i) May stop once CD4 > 100 - 200 cells/µL ◊ Ocular infection ♦ Fumidil®B 3 mg/mL in saline (final concentration = fumagillin 70 µg/mL) eye drops indefinitely (i) Fumidil® B powder must be obtained from Continent Agrimarketing and specially compounded ♦ Consider adding albendazole if also systemic infection ◊ Intestinal infections due to Enterocytozoon bienuesi ♦ Fumagillin 60 mg PO qday (i) Not available in the United states ♦ Albendazole may also be considered • Alternative therapies ◊ Itraconazole 400 mg PO qday with albendazole for disseminated disease due to Trachipleistophora or Brachiola spp. Prophylaxis • Primary prophylaxis ◊ Good hygiene • Secondary prophylaxis ◊ No recommendations than to continue chronic maintenance therapy ♦ Treatment for ocular infection should be continued indefinitely, but may consider D/Cing with appropriate immune reconstitution ♦ For those with disseminated disease, may consider D/Cing once CD4 > 100 – 200 cells/µL for at least 6 months g) Monitoring • Disease ◊ Signs/ symptoms of volume depletion, electrolyte and weight loss, malnutrition ◊ Treatment failure ♦ Optimize HAART ♦ Continue supportive treatment • Drugs: See Table 1 at end of notes 10) Coccidioidomycosis a) Cause • Coccidioides immitis b) Transmission • Reactivation of latent infection • Endemic in the SW US ◊ Soil exposure c) Signs/symptoms • Those with CD4 < 250 cells/µL are most at risk • Common clinical presentation ◊ Localized pneumonia ◊ Disseminated infection ♦ Generalized lymphadenopathy ♦ Skin nodules or ulcers ♦ Peritonitis ♦ Liver abnormalities ♦ Bone and joint involvement • May also present as meningitis with lethargy, fever, headache, N/V, confusion ◊ CSF ♦ Lymphocytic pleocytosis ♦ Glucose < 50 mg/mL ♦ Protein normal or mildly elevated d) Diagnosis • Culture of organism from clinical specimens • Demonstration of typical spherule on histopathological examination of involved tissue • Blood cultures may be positive, but this is in a minority of cases • CSF may be IgG+ e) Treatment • First-line therapies ◊ Diffuse pulmonary or disseminated disease ♦ Acute phase (i) Amphotericin B deoxycholate 0.5 – 1.0 mg/kg IV qday continued until clinical improvement 1. Usual dose = 500 – 1,000 mg total dose ♦ Chronic maintenance therapy (i) Fluconazole 400 mg PO qday (ii) Itraconazole 200 mg PO BID ◊ Milder disease ♦ Acute phase (i) Fluconazole 400 – 800 mg PO qday (ii) Itraconazole 200 mg PO BID ♦ Chronic maintenance therapy (i) Same as above ◊ Meningeal infections ♦ Fluconazole 400 – 800 mg IV or PO qday ♦ Should consider infectious disease consult • Alternative therapies Diffuse pulmonary or disseminated disease ♦ Acute phase (i) Addition of azole to amphotericin B therapy ♦ Chronic maintenance therapy (i) Ketoconazole 400 mg PO qday ◊ Milder disease ♦ Acute phase (i) Ketoconazole 400 mg PO qday Prophylaxis • Primary prophylaxis ◊ Avoid activities with increased risk ♦ Extensive exposure to disturbed native soil (i) Building excavations (ii) Dust storms • Secondary prophylaxis ◊ After completing acute phase of treatment, patients should remain indefinitely on chronic maintenance therapy Monitoring • Disease ◊ Pulmonary disease ♦ Monitor with serial physical exam, C-Xray or CT, serial fungal sputum culture, CF antibodies in serum ◊ Extrapulmonary disease ♦ Serial physical exam, imaging if appropriate, CF antibodies ◊ Meningeal disease ♦ Same as pulmonary disease, plus CSF CF antibodies ◊ Obtain CF Ab titers every 6 – 12 weeks to evaluate response ♦ Will see lag in first 1 – 2 months • Drugs: See Table 1 at end of notes ◊ f) g) Table 1. Notable Adverse Reaction and Monitoring Parameters for Drugs Commonly Used to Treat Opportunistic Infections in HIV/AIDS Drug Drugs for PCP Trimethoprim-Sulfamethoxazole (TMP-SMX) Pentamidine Clindamycin Dapsone Adverse Reactions Monitoring Parameters Comments Rashes, including Stevens-Johnson Syndrome (SJS) Bone marrow suppression CBC, inc. H/H and Plt May cause hemolytic anemia in G6PD deficiency Hepatotoxicity Renal dysfunction LFTs inc AST, ALT, Alk Phos SCr/BUN Dosage should be renally adjusted if renal dysfunction occurs N/V Nephrotoxicity SCr/BUN, K+ Reversible with discontinuation; avoid other nephrotoxins; ensure adequate hydration Hypoglycemia Hyperglycemia Glucose, s/sx of hypo – or hyperglycemia Pentamidine destroys β-cells of pancreas, first leading to increased release of insulin from dead cells, then lack of insulin due to lack of production Hypotension and arrhythmias Hepatitis Electrolyte abnormalities Diarrhea, including C. difficile diarrhea Pseudomembranous colitis Rash Hemolytic anemia Blood pressure LFTs Ca2+, Mg2+, K+ Frequency of stools Usually infusion-related Methemoglobinemia Other blood dyscrasias Rash Photosensitivity N/V/D Hepatitis Rashes tend to be more common persons with HIV CBC with diff Because of immunosuppression, may not see dramatic increase in WBC as seen with many cases of C. difficile Hemolytic anemia and methemoglobinemia due to G6PD deficiency; consider checking prior to therapy for those most at risk: black males, males from Mediterranean descent Usually treated with IV methylene blue 1-2 mg/kg over 10 – 15 minutes LFTs Primaquine Trimetrexate Atovaquone Pyrimethamine Drugs for Toxoplasmosis Pyrimethamine Sulfadiazine Clindamycin Azithromycin Atovaquone Dapsone Hemolytic anemia Methemoglobinemia N/V/D Bone marrow suppression Stomatitis Fever Rash Hepatitis N/V/D Rash Headache Pancytopenia N/V, abdominal pain Rash HA Dizziness Insomnia SEE ABOVE Rash, including SJS Bone marrow suppression N/V/D Crystalluria Renal dysfunction SEE ABOVE N/V/D Abdominal pain Skin rash Hepatotoxicity Ototoxicity SEE ABOVE SEE ABOVE CBC with diff Hemolytic anemia and methemoglobinemia due to G6PD deficiency; consider checking prior to therapy for those most at risk: black males, males from Mediterranean descent Usually treated with IV methylene blue CBC with diff Because trimetrexate affects folic acid synthesis, leucovorin must always be given. LFTs Available as liquid formulation for those that cannot swallow pills CBC with diff Because pyrimethamine affects folic acid synthesis, leucovorin must always be given. Rash tends to be more common persons with HIV, especially when given with sulfas. SEE ABOVE CBC with diff SEE ABOVE Avoid in sulfa allergies; Alternative – can desensitize patient to sulfas with available protocol. I+O SCr/BUN SEE ABOVE SEE ABOVE LFTs Hearing tests, with long-term azithromycin tx SEE ABOVE SEE ABOVE Hearing loss will resolve following discontinuation SEE ABOVE SEE ABOVE Drugs for MAC Clarithromycin Ethambutol Rifabutin Ciprofloxacin/ Levofloxacin Amikacin N/V/D Taste disturbance Abdominal cramps Skin rash, including SJS Urticaria Hepatotoxicity Ototoxicity (hearing loss, tinnitus) Optic neuritis Peripheral neuropathy N/V Headache Anorexia Hepatotoxicity Hyperuricemia Hepatotoxicity Uveitis Neutropenia Red-orange discoloration of body fluids Skin rash N/V/D Abdominal pain Headache Dizziness Sleep disturbances Renal impairment Photosensitivity Neurotoxicity Nephrotoxicity Ototoxicity (auditory and vestibular) LFTs Hearing tests Basic visual acuity and color discrimination test – monthly Reversible Often presents as inability to differentiate colors, like green and red LFTs Uric acid Regular eye exams CBC with diff Rifabutin is generally preferred over rifampin in HIV because drug interactions are less problematic than with rifampin. SCr/BUN Dosage should be renally adjusted if renal dysfunction occurs SCr/BUN; peak and trough concentrations Especially with high dose or in patients with renal dysfunction Dosage should be renally adjusted if renal dysfunction occurs Drugs for Cryptococcal Meningitis Amphotericin B deoxycholate (often just referred to as Amphotericin B) Nephrotoxicity Infusion-related reactions (inc. fever, chills, N/V, HA, thrombophlebitis, myalgias, arthralgias) SCr/BUN Dosage should be renally adjusted if renal dysfunction occurs Reactions may be avoided by premedicating with antiemetics, antiinflammatories, antipyretics; thrombophlebitis can be avoided by slowing infusion rate; Meperidine is preferred agent to treat amphotericin rigors associated with infusion. Electrolyte imbalances N/V K+, Ca2+, Mg2+, Associated with hyper- and hypokalemia, hypocalcemia, hypomagnesemia Anemia CBC with diff The lipid formulation of amphotericin B is generally used to lower the risk of nephrotoxicity and infusion-related reactions Flucytosine Fluconazole Itraconazole N/V/D Bone marrow suppression Hepatotoxicity Renal dysfunction N/V/D Headache Hepatotoxicity Rash N/V/D Rash, including SJS Hepatotoxicity Congestive heart failure Edema Hypokalemia Renal dysfunction CBC with diff LFTs SCr/BUN Dosage should be renally adjusted if renal dysfunction occurs Dosage should be renally adjusted if renal dysfunction is present LFTs LFTs I + Os K+ SCr/BUN Drugs for Histoplasmosis Amphotericin B Itraconazole SEE ABOVE SEE ABOVE SEE ABOVE SEE ABOVE Fluconazole SEE ABOVE SEE ABOVE Only associated with IV itraconazole Associated more with IV; if occurs, consider switching to PO; otherwise, does not need to be adjusted for renal dysfunction SEE ABOVE Some may consider monitoring drug concentrations: free drug > 1 mg/mL; free + hydroxylated metabolite > 2 µg/mL SEE ABOVE Drugs for Cryptosporidiosis Nitazoxanide Paromomycin Drugs for Microsporidiosis Albendazole Fumagillin (ocular therapy) Drugs for Coccidioidomycosis Amphotericin B Fluconazole Itraconazole Ketoconazole N/V/D Abdominal pain Headache N/V/D Abdominal pain N/V Abdominal pain Neutropenia Hepatotoxicity Dizziness Headache Minimal systemic or local effect SEE ABOVE SEE ABOVE SEE ABOVE Pruritis N/V, abdominal pain Decreased testosterone levels Hepatotoxicity Avoid use in patients with intestinal blockages CBC with diff LFTs SEE ABOVE SEE ABOVE SEE ABOVE SEE ABOVE SEE ABOVE SEE ABOVE **** It is important to check possible drug interactions of these drugs with antiretroviral therapy as well as other medications the patient may be taking and adjust therapy as necessary. ****