Nausea and vomiting Chemotherapy
advertisement

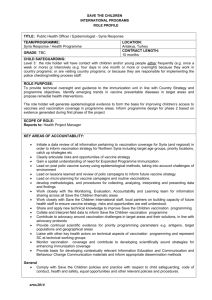
Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Nurse Practitioner Clinical Protocol Amendment For Haematology Prepared by Christina Crosbie RN, BSc, MN (NP) August 2014 Sir Charles Gairdner Hospital North Metropolitan Health Service Author: Christina Crosbie Version 1.2 Effective: August 2014 – Review: 2017 Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Contents Clinical Protocol Amendment Panel....................................................................................... 3 1. Introduction ...................................................................................................................... 4 2. Patient Group – No change. ............................................................................................. 4 3. Provision of Care – No Change ........................................................................................ 4 4. Diagnostic Tests and Investigations – No Change ............................................................ 4 5. Medications ...................................................................................................................... 4 6. Collaboration and Referral – No change. .......................................................................... 4 7. Accountability and Professionalism – No change. ............................................................ 4 8. Clinical Protocol................................................................................................................ 4 9. Medication Formulary ....................................................................................................... 7 Formulary Monograph ....................................................................................................... 8 Appendix 1 ...........................................................................................................................31 Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Clinical Protocol Amendment Panel Name: Position Professional Qualifications: Organisation: Signature: Name: Position Professional Qualifications: Organisation: Signature: Name: Position Professional Qualifications: Organisation: Signature: Name: Position Professional Qualifications: Organisation: Signature: Name: Position Professional Qualifications: Organisation: Signature: Name: Position Professional Qualifications: Organisation: Signature: Author: Christina Crosbie V1.2 Date: Date: Date: Date: Date: Date: Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment 1. Introduction The previous versions of this Clinical Protocol (V1 and V1.1) continue to be current and relevant. This amendment includes additions to the scope of practice and care provided to patients within haematology at Sir Charles Gairdner Hospital. 2. Patient Group – No change. 3. Provision of Care – No Change 4. Diagnostic Tests and Investigations – No Change 5. Medications Addition to Clinical Protocol Introduction of Vaccination program for stem cell transplant patients. Studies have shown that the levels of antibodies to diseases that can be prevented by vaccination decrease during the first few years after a stem cell or bone marrow transplant. The immunities acquired by the patient prior to the transplant are generally lost. This can occur after both allogeneic and autologous stem cell transplantation. Transplant patients are at a higher risk of infection until their immune systems become stronger. Vaccination can protect the post-transplant patient from infections such as childhood diseases, influenza and pneumococcal pneumonia. A copy of the newly introduced post transplant vaccination protocol is included in Appendix 1. The prescribing and administration of vaccines will be carried out by the Nurse Practitioner in Haematology and all vaccines are listed within the formulary. Other additions (listed in Formulary Section 9) Tranexamic Acid Norethisterone Voriconazole Posaconazole Within the formulary section will be a description for use in practice. 6. Collaboration and Referral – No change. 7. Accountability and Professionalism – No change. 8. Clinical Protocol Additions to the clinical protocol are detailed within this section. Addition Decision making for insertion/removal of Vascular Access Devices The addition to the scope of practice within the NP role is to make the independent and/or collaborative decision to insert and/or remove central venous access devices. Central venous access devices (CVAD’s) include Central Venous Catheters (CVC), Peripherally Inserted Central Catheters (PICC), VASCATH’s. These devices are inserted to assist with the administration of chemotherapy, emergency venous access after treatment, stem cell Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment collection procedure, administration of blood products and administration of intravenous antibiotics etc. The insertion and removal of an access device is decided upon on an individual patient basis, this decision can also be in collaboration with the patients treating consultant if any doubt arises. Vascular Access Device Central Venous Catheter Decision Insertion Prior to chemotherapy treatment Prior to Stem Cell Transplant As directed by any haematology consultant or registrar Peripherally Inserted Central Catheter Non-tunnelled large bore, central venous catheters (VASCATH) Prior to chemotherapy treatment Removal • Chemotherapy treatment completion and platelet count of approximately ≥30x10*9/L • Thrombosis and in consultation with the patients treating haematology consultant • Transplant recovery and platelet count of approximately ≥30x10*9/L • Thrombosis and in consultation with the patients treating haematology consultant • As directed by any haematology consultant or registrar • Thrombosis and in consultation with the patients treating haematology consultant • Chemotherapy treatment completion • Thrombosis and in consultation with the patients treating haematology consultant Prior to Stem Cell Transplant • • Transplant recovery Thrombosis and in consultation with the patients treating haematology consultant As directed by any haematology consultant or registrar • Prior to Stem Cell Collection (If patient has poor venous access for procedure) • • As directed by any haematology consultant or registrar Thrombosis and in consultation with the patients treating haematology consultant After Stem Cell Collection As directed by the haematology medical team Platelet count of approximately ≥30x10*9/L Author: Christina Crosbie V1.2 • • Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Hydration for Haematology Patients Dehydration is a common side effect after chemotherapy/stem cell transplant and Intravenous Hydration (IVH) can be required at this time. Dehydration can be due to a number of factors. These factors can include reduced fluid intake, vomiting, diarrhoea and use of antihypertensive medication. This can result in patients experiencing varying symptoms and include hypotension, postural hypotension, increased nausea and altered renal function. Each patient will be assessed for IVH on presentation of a documented hypotension and/or symptoms of dehydration. Decision on volume and rate is decided upon on an individual patient basis and in collaboration with medical staff where required. Initial hydration solution will be Normal Saline 0.9% and further hydration will be decided after collaboration with the medical team. Intravenous Hydration (IVH) Decrease in oral fluid intake after Reason for chemotherapy and/or stem cell commencing IV transplant hydration Decrease in renal function Hypotension due to vomiting and/or diarrhoea post chemotherapy/stem cell transplant. Hypotension after chemotherapy and/or stem cell transplant while taking antihypertensive medication As directed by any haematology consultant or registrar Post lumbar Puncture (LP) headache Author: Christina Crosbie V1.2 Effective: Documented hypotension and/or symptoms Intake less than 1 litre in 24 hrs Slow IVH IVH administered after consultation with haematology consultant or registrar Hypotension recorded and/or vomiting and diarrhoea. IVH given alongside anti-emetics Documented hypotension and/or symptoms IVH to restore blood pressure and withhold anti-hypertensive medication if required As discussed and documented IVH alongside regular analgesia medication intervention and admission for post LP headache Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment 9. Medication Formulary Additions – Additional vaccinations and mediations added to the existing formulary. The following Medications are additions to V1 and V1.1. The following list contains details of the additions of medications and is endorsed by the Oncology Pharmacist within the Medical Specialties Division (previously Cancer Division) of Sir Charles Gairdner Hospital. Drug Vaccinations Prevenar 13 (13vPCV) Pneumovax (23vPPV) Route Intramuscular Subcutaneous Intramuscular Hiberix (Hib) Intramuscular Ipol (IPV) Subcutaneous Boostrix (dTpa) Intramuscular ADT (dT) Intramuscular H-B-Vax II 40 mcg - (dialysis formulation) Fluvax (Inactivated) Priorix (MMR) Live vaccine Varivax (Varicella) Intramuscular Menactra (Meningococcal) Gardasil (HPV Intramuscular Intramuscular Subcutaneous Intramuscular Subcutaneous Intramuscular Other Medications Tranexamic Acid Oral Norethisterone Oral Voriconazole Posaconazole Oral Oral Author: Christina Crosbie V1.2 Section Dose Range Poisons Schedule 0.5 mL prefilled syringe 0.5 mL prefilled syringe S4 VaccinesImmunology VaccinesImmunology VaccinesImmunology VaccinesImmunology VaccinesImmunology 0.5 mL S4 0.5 mL S4 0.5 mL S4 0.5 mL S4 40 mcg/1mL S4 VaccinesImmunology or VaccinesImmunology VaccinesImmunology VaccinesImmunology VaccinesImmunology 0.5mL S4 0.5 mL S4 0.5 mL S4 0.5 mL S4 0.5 mL S4 500-1000mg one - three times daily S3 (36 tabs) S4 (all others S4 VaccinesImmunology or VaccinesImmunology Haemostatic agents Cardiovascular System Contraceptive Agents Antifungal agent Antifungal agent Effective: 5-10mg one three times daily 50-200mg 200-400mg S4 S4 S4 Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccination – Streptococcus pneumoniae Drug generic name: 13vPCV (Prevenar 13) Poisons schedule: S4 Dosage range: 0.5ml prefilled syringe Route: Intra-muscular – as per manufacturer recommendation on administration Frequency of administration: As per vaccination protocol (Appendix 1) Duration of order: Once Actions: The protection afforded by Prevenar 13 vaccination is mediated by the induction of antibodies against the pneumococcal capsular serotypes in the vaccine. B-cells produce antibodies in response to antigenic stimulation via T-dependent and Tindependent mechanisms. The immune response to most antigens is T-dependent and involves the collaboration of CD4+ T-cells and B-cells, recognizing the antigen in a linked fashion. CD4+ T-cells (T-helper cells) provide signals to B-cells directly through cell surface protein interactions, and indirectly through the release of cytokines. These signals result in proliferation and differentiation of the B-cells, and production of high affinity antibodies. CD4+ T-cell signaling is a requisite for the generation of long lived B-cells called plasma cells, which continuously produce antibodies of several isotypes (with an IgG component) and memory B-cells that rapidly mobilize and secrete antibodies upon re-exposure to the same antigen. Bacterial capsular polysaccharides (PSs), while varied in chemical structure, share the common immunological property of being largely T-independent antigens. In the absence of T-cell help, PS stimulated B-cells predominantly produce IgM antibodies; there is generally no affinity maturation of the antibodies, and no memory B-cells are generated. As vaccines, PSs are associated with poor or absent immunogenicity in infants less than 24 months of age and failure to induce immunological memory at any age. Conjugation of PSs to a protein carrier overcomes the T-cell independent nature of PS antigens. Protein carrier specific Tcells provide the signals needed for maturation of the B-cell response and generation of Bcell memory. Conversion of Streptococcus pneumoniae PSs to a T-cell dependent antigen by covalent coupling to the immunogenic protein carrier CRM197 enhances the antibody response and induces immune memory. This has been demonstrated to elicit booster responses on re-exposure in infants and young children to pneumococcal polysaccharides. Indications for use: Active immunisation for the prevention of disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F (including invasive disease, pneumonia and acute otitis media) in infants and children from 6 weeks up to 17 years of age. Active immunisation for the prevention of pneumococcal disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F in adults aged 50 years and older. Contraindications for use: Hypersensitivity to the active substances or to any of the excipients, or to diphtheria toxoid. Allergic reaction or anaphylactic reaction following prior administration of Prevenar. Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Adverse effects Very common: fever, any injection site erythema, induration/swelling or pain/tenderness; injection site erythema or induration/swelling 2.5-7.0 cm (after toddler dose and in older children [age 2 to 5 years]). Common: fever greater than 39deg. C, injection site erythema or induration/swelling 2.5-7.0 cm (after infant series); injection site pain/tenderness interfering with movement. Uncommon: injection site induration/swelling or erythema greater than 7.0 cm. Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccination - Pneumococcal Drug generic name: 23vPPV (Pneumovax 23) Poisons schedule: S4 Dosage range: single dose of Pneumovax 23 0.5 mL Route: Subcutaneous or intramuscular as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Indications for use: Pneumovax is indicated for immunisation of individuals in the following situations. • All individuals over the age of 65 years. • Individuals with asplenia, either functional or anatomical, including sickle cell disease, in persons more than 2 years of age; where possible the vaccine should be given at least 14 days before splenectomy. • Immunocompromised patients at increased risk of pneumococcal disease (e.g. patients with HIV infection before the development of AIDS, nephrotic syndrome, multiple myeloma, lymphoma, Hodgkin's disease and organ transplantation). • Aboriginal and Torres Strait Islander people over 50 years of age. Immunocompetent persons at increased risk of complications from pneumococcal disease because of chronic illness (e.g. chronic cardiac, renal or pulmonary disease, diabetes mellitus, alcoholism and cirrhosis). • Patients with cerebrospinal fluid leaks. Contraindications for use: Hypersensitivity to any component of the vaccine. Adverse effects - Intradermal administration may cause severe local reactions Common – fever (less than or equal to 38.8deg. C), injection site reactions including soreness, erythema, warmth, swelling and local induration. Rare – Cellulitis like reaction at injection site. Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccination - Haemophilus influenzae type b capsular polysaccharide. Drug generic name: Hib (Hiberix) Poisons schedule: S4 Dosage range: single dose of 0.5 mL Route: Intramuscular - as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Induce anti-PRP antibodies above the level known to be protective against invasive disease due to Haemophilus influenzae type b. An anti-PRP antibody titre greater than or equal to 0.15 microgram/mL correlates with immediate protection against Hib infection and greater than or equal to 1.0 microgram/mL correlates with long-term protection. Indications for use: Active immunisation against Haemophilus influenzae type b infection in children aged from two months to five years. Contraindications for use: Known hypersensitivity to any component of the vaccine, or subjects having shown signs of hypersensitivity after previous administration of Hib vaccines. As for any vaccine, Hiberix should not be administered to subjects suffering from acute severe febrile illness. However, the presence of minor infection does not contraindicate vaccination. Adverse effects Very Common – Fever, erythematous rash, injection site reaction, redness, pain and swelling at injection site. Common – Loss of appetite, vomiting, diarrhoea, conjunctivitis, otitis media, rhinitis, coughing, respiratory disorder, upper respiratory tract infection and bronchitis, Uncommon - Sweating increased, purpura and abdominal pain. Rare – Loss of appetite, vomiting, diarrhoea. Uncommon: spastic paralysis, insomnia, emotional lability, restlessness and unusual crying Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccination - Poliomyelitis Drug generic name: IPV (Ipol) Poisons schedule: S4 Dosage range: Single Dose 0.5 m/L Route: Subcutaneous - as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Indications for use: Ipol is indicated for active immunisation of infants, children and adults for the prevention of poliomyelitis. Recommendations for the use of live and inactivated poliovirus vaccines are described in the national immunisation guidelines. 1. General recommendations. It is recommended that all infants, unimmunised children and adolescents not previously immunised be vaccinated routinely against paralytic poliomyelitis. Ipol should be offered to patients who have refused OPV, or in whom OPV is contraindicated. 2. Ipol is also indicated for: the primary vaccination of immunocompromised individuals of all ages (see Precautions), and household contacts of such individuals (when vaccination is indicated); unvaccinated or inadequately vaccinated* adults, particularly if at increased risk of exposure to live poliovirus, including: travellers to areas or countries where poliomyelitis is epidemic or endemic; laboratory workers handling specimens which may contain polioviruses; healthcare workers in close contact with patients who may be excreting polioviruses. Contraindications for use: Known systemic hypersensitivity to any component of Ipol or serious reaction after previous administration of the vaccine or vaccine containing the same substances. Vaccination should be postponed in cases of febrile or acute disease. Adverse effects Common – local reactions at injection site and fever Very rare – lymphadenopathy, injection site oedema, injection site pain, injection site rash or injection site mass within 48 hours Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccinations – Diptheria, Tetanus, Pertussis Drug generic name: dTPA (boostrix) Poisons schedule: S4 Dosage range: 0.5 mL Route: Intramuscular - as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Boostrix (dTpa vaccine) induces antibodies against all vaccine components. Indications for use: Booster vaccination against diphtheria, tetanus and pertussis of individuals aged ten years and older. Contraindications for use: Boostrix should not be administered to subjects with known hypersensitivity to any component of the vaccine, or to subjects having shown signs of hypersensitivity after previous administration of diphtheria, tetanus or pertussis vaccines. As with other vaccines, the administration of Boostrix should be postponed in subjects suffering from acute severe febrile illness. The presence of a minor infection, however, is not a contraindication. Boostrix is contraindicated if the subject has experienced an encephalopathy of unknown aetiology, occurring within seven days following previous vaccination with pertussis containing vaccine. In these circumstances, pertussis vaccination should be discontinued and the vaccination course should be continued with diphtheria and tetanus vaccines. Boostrix should not be administered to subjects who have experienced transient thrombocytopenia or neurological complications following an earlier immunisation against diphtheria and/or tetanus. Adverse effects Common – crying, irritability, drowsiness, limb swelling in children, Vaccines containing polio antigen: vomiting, diarrhoea, loss of appetite Infrequent - lethargy, myalgia, malaise Rare – Urticaria, peripheral neuropathy, encephalopathy, seizure, limb swelling (adults), hypotonic-hyporesponsive episodes. Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccinations – Diptheria/Tetanus Drug generic name: dT (ADT) Poisons schedule: S4 Dosage range: 0.5 mL Route: Intramuscular - as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Following intramuscular injection, ADT Booster stimulates the immune system with the effect that antibodies are formed that protect against the diseases caused by exposure to Corynebacterium diphtheriae and Clostridium tetani. Protection against diphtheria and tetanus can be expected to last for up to ten years. Indications for use: Vaccination of children (greater than or equal to 5 years of age) and adults who have previously received at least three doses of a vaccine for primary immunisation against diphtheria and tetanus. ADT Booster is not intended for primary immunisation against diphtheria and tetanus. Contraindications for use: ADT Booster should not be administered to subjects who have previously experienced a serious reaction (e.g. anaphylaxis) to this vaccine or who are known to be hypersensitive to any of the vaccine components. Adverse effects: Common – Malaise, fever greater than or equal to 38deg. C, redness/ swelling at the injection site. Uncommon: redness/ swelling greater than or equal to 6 cm at the injection site. Rare: high fever > 40deg. C, granuloma or sterile abscess at the injection site. Infrequent – Eczema, dermatitis. Rare – Anaphylactic reactions, urticarial reactions. Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccinations – Hepatitis B Drug generic name: H-B-Vax II 40mcg – (Dialysis formulation) Poisons schedule: S4 Dosage range: 40mcg Route: Intramuscular - as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Clinical studies have established that H-B-Vax II, when injected into the deltoid muscle, induced protective levels of antibody (defined as greater than or equal to 10 mIU/mL anti-HBs) in 96% of 1,213 healthy adults who received the recommended three dose regimen. Indications for use: -B-Vax II is indicated for immunisation against infection caused by all known subtypes of hepatitis B virus. Adolescent vaccination is not necessary for children who have received a primary course of hepatitis B vaccine. Vaccination is recommended in adults who are at substantial risk of hepatitis B virus infection and have been demonstrated or judged to be susceptible. Vaccination of individuals who have antibodies against hepatitis B virus from a previous infection is not necessary. Contraindications for use: Hypersensitivity to any component of the vaccine. Hypersensitivity to yeast (Saccharomyces cerevisiae). Patients who develop symptoms suggestive of hypersensitivity after an injection should not receive further injections of H-BVax II. Adverse effects Common – transient injection site reactions (pain, redness, itching, swelling or burning, small hard lump that may persist for some weeks), transient fever, fainting (more common in adolescents). Rare – malaise, myalgia, arthralgia, lymphadenopathy, peripheral neuropathy, delayed hypersensitivity reactions. Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccinations - Influenza A&B Drug generic name: Fluvax Poisons schedule: S4 Dosage range: 0.5mL Route: Intramuscular - as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Induce antibodies to the viral surface glycoproteins, haemagglutinin and neuraminidase. These antibodies are important in the prevention of natural infection. Seroprotection is generally obtained within 2 to 3 weeks. The duration of post vaccination immunity to homologous strains or to strains closely related to the vaccine strains varies, but is usually 6 to 12 months. Indications for use: For the prevention of influenza caused by influenza virus types A and B. Contraindications for use: Fluvax vaccine must not be used in children under 5 years. Anaphylactic hypersensitivity to previous influenza vaccination or to eggs, neomycin, polymyxin B sulfate or any of the constituents or trace residues of this vaccine. Immunisation must be postponed in people who have febrile illness or acute infection. Adverse effects: Common – Fever, malaise, myalgia, headache (these reactions may last 1–2 days). Infrequent - Transient injection site reactions (pain, redness, itching, swelling or burning, small hard lump that may persist for some weeks), transient fever, fainting (more common in adolescents). Rare – Allergic reactions (hives, angioedema, asthma, anaphylaxis). Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccinations – Measles,Mumps and Rubella (MMR) Drug generic name: Priorix (Live Vaccine) Poisons schedule: S4 Dosage range: 0.5mL Route: Subcutaneous/intramuscular - as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Indications for use: Prevention of measles, mumps and rubella, Immunosuppression. Children with history of seizures—may require treatment to reduce fever 5–12 days after vaccination, see Paracetamol. Untreated TB—MMR vaccination may theoretically exacerbate the condition; vaccinate when TB is being treated. Treatment with immunoglobulins, other blood products (excluding washed red blood cells)— may interfere with the immune response; see the latest Australian Immunisation Handbook for the recommended interval before giving MMR vaccine (varies depending on blood product and its dosage; may be up to 11 months). If immunoglobulin or blood products are given within 3 weeks after an MMR vaccine, test for immunity after 6 months or revaccinate after recommended interval. Contraindications for use: History of anaphylaxis Treatment with immunoglobulins—may interfere with the immune response to some live virus vaccines; seek specialist advice. Adverse effects Common – Headache, fever (usually 5–12 days after vaccination, lasting 2–3 days); arthritis and arthralgia (in women), sore throat, lymphadenopathy and rash may occur 1–3 weeks after vaccination and are usually transient Infrequent - Febrile seizures, parotid swelling; arthritis and arthralgia (in children) may occur 1–3 weeks after vaccination and are usually transient. Rare – Allergic reactions including anaphylaxis Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccinations – Varicella Zoster Virus Drug generic name: Varivax Poisons schedule: S4 Dosage range: 0.5 mL Route: Subcutaneous - as per manufacturer recommendation on administration Frequency of administration: Once Duration of order: As per vaccination protocol (Appendix 1) Actions: Indications for use: Varicella vaccine: Prevention of varicella (chickenpox). Zoster vaccine: Prevention of herpes zoster (shingles) in people >50 years, and reduction of zoster-associated pain in people >60 years Contraindications for use: • • • • • • • • • • A history of hypersensitivity to any component of the vaccine, including gelatin. A history of anaphylactoid reaction to neomycin (each dose of reconstituted vaccine contains trace quantities of neomycin). Individuals with blood dyscrasias, leukaemia, lymphomas of any type, or other malignant neoplasms affecting the bone marrow or lymphatic systems. Individuals receiving immunosuppressive therapy. Individuals who are on immunosuppressant drugs are more susceptible to infections than healthy individuals. Vaccination with live attenuated varicella vaccine can result in a more extensive vaccine associated rash or disseminated disease in individuals on immunosuppressant doses of corticosteroids. Individuals with primary and acquired immunodeficiency states, including those who are immunosuppressed in association with AIDS or other clinical manifestations of infection with human immunodeficiency virus; cellular immune deficiencies; and hypogammaglobulinaemic and dysgammaglobulinaemic states. A family history of congenital or hereditary immunodeficiency, unless the immune competence of the potential vaccine recipient is demonstrated. Active untreated tuberculosis. Any febrile respiratory illness or other active febrile infection. Pregnancy; the possible effects of the vaccine on fetal development are unknown at this time. However, wild-type varicella is known to sometimes cause fetal harm. If vaccination of postpubertal females is undertaken, pregnancy should be avoided for three months following vaccination. Adverse effects: Common – Transient injection site reactions (pain, redness, itching, swelling or burning, small hard lump that may persist for some weeks), transient fever, fainting (more common in adolescents). Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Varicella vaccines: Mild papular-vesicular rash (usually within 5–26 days), Zoster vaccine: headache, haematoma. Rare – Allergic reactions including anaphylaxis. Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccinations – Meningococcal Drug generic name: Menactra (Meningococcal) Poisons schedule: S4 Dosage range: 0.5 mL Route: Intramuscular - as per manufacturer recommendation on administration Frequency of administration: once Duration of order: As per vaccination protocol (Appendix 1) Actions: The presence of bactericidal anticapsular meningococcal antibodies has been associated with protection from invasive meningococcal disease. Menactra vaccine induces the production of bactericidal antibodies specific to the capsular polysaccharides of serogroups A, C, Y and W-135. Indications for use: • Menactra vaccine is indicated for active immunisation of individuals 2 through 55 years of age for the prevention of invasive meningococcal disease caused by N. meningitidis serogroups A, C, Y and W-135. • Menactra vaccine is not indicated for the prevention of meningitis caused by other microorganisms or for the prevention of invasive meningococcal disease caused by N. meningitidis serogroup B. • Menactra vaccine is not indicated for treatment of meningococcal infections. • Menactra vaccine is not indicated for immunisation against diphtheria. Contraindications for use: • Known hypersensitivity to any component of Menactra vaccine including diphtheria toxoid, or a life threatening reaction after previous administration of a vaccine containing similar components, are contraindications to vaccine administration. • Known history of Guillain-Barre syndrome (see Precautions section) is a contraindication to vaccine administration. • Vaccination must be postponed in case of febrile or acute disease. However a minor febrile or nonfebrile illness, such as mild upper respiratory infection, is not usually a reason to postpone immunisation. Adverse effects Common - Headache, irritability, malaise, GI symptoms (eg nausea), loss of appetite, rash. Bexsero®: fever (70–80%), vomiting, diarrhoea (in infants); myalgia, arthralgia (in adolescents). infrequent - Transient injection site reactions (pain, redness, itching, swelling or burning, small hard lump that may persist for some weeks), transient fever, fainting (more common in adolescents). Rare - Allergic reactions including anaphylaxis. Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Vaccinations – Human Papillomavirus (HPV) Drug generic name: Human Papillomavirus Vaccination - Gardasil Poisons schedule: S4 Dosage range: 0.5 mL Route: Intramuscular - as per manufacturer recommendation on administration Frequency of administration: 3 doses – second dose two months after first dose, third dose six months after the first dose. Duration of order: As per vaccination protocol (Appendix 1) Actions: Gardasil contains HPV 6, 11, 16 and 18 L1 VLPs. Each VLP is composed of a unique recombinant L1 major capsid protein for the respective HPV type. Because the viruslike particles contain no viral DNA, they cannot infect cells or reproduce. Preclinical data suggest that the efficacy of L1 VLP vaccines is mediated by the development of humoral immune responses. Induction of antipapillomavirus antibodies with L1 VLP vaccines resulted in protection against infection. Administration of serum from vaccinated to unvaccinated animals resulted in the transfer of protection against HPV to the unvaccinated animals. The induction of a strong anamnestic (immune memory) response has been further demonstrated in clinical trials. Indications for use: Prevention of cervical, vulvar, vaginal, anal cancer, precancerous or dysplastic lesions, genital warts, infection caused by HPV types 6, 11, 16, 18 in females 945. Contraindications for use: Hypersensitivity to the active substances or to any of the excipients of the vaccine (see Excipients). Individuals who develop symptoms indicative of hypersensitivity after receiving a dose of Gardasil should not receive further doses of Gardasil. Practice Point - observe for 15 minutes post vaccination Adverse effects: Common - Transient injection site reactions (pain, redness, itching, swelling or burning, small hard lump that may persist for some weeks), transient fever, fainting (more common in adolescents). Rare - Allergic reactions including anaphylaxis. Indications for use in practice: Use in conjunction with the vaccinations protocol described in Appendix 1 Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Drug generic name: Tranexamic Acid Poisons schedule: S3 for 36 (blister pack) tablets/S4 for all other presentations Dosage range: 500-1000mg up to three times daily Route: Oral Frequency of administration: from 1-3 times daily Duration of order: 30 days Actions: Tranexamic acid is a competitive inhibitor of plasminogen activation and at much higher concentrations a non-competitive inhibitor of plasmin, thus implying that tranexamic acid interferes with the fibrinolytic process in the same way as aminocaproic acid. Indications for use: Short-term use in the treatment of hyphaemia and in patients with established coagulopathies who are undergoing minor surgery and menorrhagia. Contraindications for use: Patients with a history or risk of thrombosis should not be given tranexamic acid, unless at the same time it is possible to give treatment with anticoagulants. Active thromboembolic disease such as deep vein thrombosis (DVT), pulmonary embolism and cerebral thrombosis. The preparation should not be given to patients with acquired disturbances of colour vision. If disturbances of colour vision arise during the course of treatment, the administration of the preparation should be discontinued. Patients with subarachnoid haemorrhage should not be given tranexamic acid as anecdotal experience indicates that cerebral oedema and cerebral infarction may be caused in such cases. Hypersensitivity to tranexamic acid or any of its excipients. Adverse effects Common - Nausea, vomiting, diarrhoea. Rare - Thrombosis, visual disturbances including transient disturbance of colour vision. Allergic skin reactions. Indications for use in practice: Prescribed only after consultation with the patients treating consultant haematologist. Patients with end stage haematological malignancy experiencing bleeding with an acceptable platelet count of more than 10x10*9/L. Not for patients who have a clotting disorder or receiving anti-coagulation therapy unless directed by the patients treating haematologist. Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: _______________________ Formulary Monograph Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Drug generic name: Norethisterone Poisons schedule: S4 Dosage range: 5-10mg Route: Oral Frequency of administration: 1 or 2 tablets, 1-3 times daily Duration of order: 30 days Actions: Norethisterone is a progestogen with negligible androgenic effects. Complete transformation of the endometrium from a proliferative to a secretory state was achieved in oestrogen primed castrated or climacteric women who were administered oral doses of norethisterone 100-150 mg/cycle. The progestogenic effects of norethisterone on the endometrium is the basis of the treatment of dysfunctional bleeding, primary and secondary amenorrhoea and endometriosis with Primolut N.Gonadotropin secretion inhibition and anovulation can be achieved with a daily intake of norethisterone 0.5 mg. Positive effects of Primolut N on premenstrual symptoms can be traced back to suppression of ovarian function. Due to the stabilising effects of norethisterone on the endometrium, administration of Primolut N can be used to shift the timing of menstruation. Like progesterone, norethisterone is thermogenic and alters the basal body temperature. Indications for use: Dysfunctional bleeding; primary, sec amenorrhoea; premenstrual syndrome; delay menstruation; endometriosis; oestrogen replacement therapy (adjunct). Contraindications for use: Presence or history of thrombosis, thromboembolism (e.g. DVT, PE, MI), CVA; thrombosis prodromi (e.g. TIA, angina); history of migraine with focal neurological symptoms; severe hepatic dysfunction (or history) with abnormal Liver function tests; liver tumour (including history); diabetes with vascular involvement; known, suspected sex hormone dependent malignancy; Dubin-Johnson, Rotor syndrome; missed abortion; undiagnosed genitourinary bleeding, breast disease; pregnancy (including suspected), lactation. Adverse effects Caution in patients with a history of depression, diabetes, Fluid retention Contraception: reversible ovarian cysts. Common - menstrual irregularity, prolonged bleeding, spotting, amenorrhoea, breast tenderness, depression, acne. Infrequent – nausea, vomiting, headache, dizziness, lethargy. Rare - cholestatic jaundice, decreased libido, androgenic effects (hirsutism, greasy hair), anaphylactic reaction. Indications for use in practice: Prescribed only after consultation with the patients treating consultant haematologist. To delay menstruation during the course of chemotherapy treatment and/or stem cell transplantation until bone marrow recovery Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: Author: Christina Crosbie V1.2 Effective: ______________________ Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Drug generic name: Voriconazole Poisons schedule: S4 Dosage range: 50-200mg twice daily Route: Oral - Take either 1 hour before or 1 hour after food. Frequency of administration: As directed by the medical team Duration of order: As directed by the medical team Actions: Voriconazole is a triazole antifungal agent. Voriconazole's primary mode of action is the inhibition of fungal cytochrome P450 mediated 14 alpha-sterol demethylation, an essential step in ergosterol biosynthesis. Voriconazole is more selective than some other azole drugs for fungal as opposed to various mammalian cytochrome P450 enzyme systems. The subsequent loss of normal sterols correlates with the accumulation of 14 alpha-methyl sterols in fungi and may be responsible for its fungistatic/ fungicidal activity. Indications for use: For treatment of the following fungal infections. Invasive aspergillosis. Serious Candida infections (including Candida krusei), including oesophageal and systemic Candida infections (hepatosplenic candidiasis, disseminated candidiasis, candidaemia). Serious fungal infections caused by Scedosporium sp. and Fusarium sp. Other serious fungal infections, in patients intolerant of, or refractory to, other therapy. Prophylaxis in patients who are at high risk of developing invasive fungal infections. The indication is based on studies including patients undergoing haematopoietic stem cell transplantation. Contraindications for use: • Known hypersensitivity to voriconazole or to any of the excipients. Coadministration of the CYP3A4 substrates pimozide or quinidine with voriconazole is contraindicated since increased plasma concentrations of these medicinal products can lead to QTc prolongation and rare occurrences of torsades de pointes. • Coadministration of voriconazole with rifabutin, rifampicin, carbamazepine and long acting barbiturates (e.g. phenobarbitone) is contraindicated since these medicinal products are likely to decrease plasma voriconazole concentrations significantly. • Coadministration with efavirenz at a dose of 400 mg once daily or above is contraindicated because efavirenz significantly decreases plasma voriconazole concentrations in healthy subjects at this dose. • Coadministration of voriconazole with high dose ritonavir (400 mg and above twice daily) is contraindicated because ritonavir significantly decreased plasma voriconazole concentrations in healthy subjects at this dose. • Coadministration of ergot alkaloids (ergotamine, dihydroergotamine), which are CYP3A4 substrates, is contraindicated since increased plasma concentrations of these medicinal products can lead to ergotism. • Coadministration of voriconazole and sirolimus is contraindicated, since voriconazole is likely to increase plasma concentrations of sirolimus. • Coadministration of voriconazole with St John's Wort is contraindicated. Adverse effects: Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Common – Sinusitis, thrombocytopenia, anaemia, leukopenia, pancytopenia, hypokalaemia, hypoglycaemia, hallucinations, confusion, depression, anxiety, agitation, headache, dizzyness, tremor, paraesthesia, rash, face oedema, maculopapular rash, back pain, elevated liver function, increased creatinine, acute kidney failure, fever. Infrequent – Lymphadenopathy, agranulocytosis, eosinophilia, disseminated intravascular coagulation, marrow depression, allergic reaction, anaphylactiod reaction, adrenal cortex insufficiency, hypercholesterolaemia, chills. Rare – Hyperthyroidism, hypothyroidism, Guillain-Barre syndrome, insomnia, angioedema. Indications for use in practice: Initial prescription will be at the instruction of the patients treating consultant and Infectious Diseases (ID). Subsequent prescriptions will be for repeat prescriptions only and only after discussion with the patients treating consultant haematologist and or ID. Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: Author: Christina Crosbie V1.2 Effective: ______________________ Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Formulary Monograph Drug generic name: Posaconazole Poisons schedule: S4 Dosage range: 200-400mg: as directed by the medical team Route: Oral Frequency of administration: As directed by the medical team Duration of order: As directed by the medical team Actions: Posaconazole is a triazole antifungal agent. It is an inhibitor of the enzyme lanosterol 14alpha-demethylase, which catalyses an essential step in ergosterol biosynthesis. Ergosterol depletion, coupled with the accumulation of methylated sterol precursors, is thought to impair membrane integrity and the function of some membrane associated proteins. This results in the inhibition of cell growth and/or cell death. Indications for use: • For use in the treatment of the following invasive fungal infections in patients 13 years of age or older. • Invasive aspergillosis in patients intolerant of, or with disease that is refractory to, alternative therapy. • Fusariosis, zygomycosis, coccidioidomycosis, chromoblastomycosis and mycetoma in patients intolerant of, or with disease that is refractory to, alternative therapy. Noxafil is also indicated for the following: • • Treatment of oropharyngeal candidiasis in immunocompromised adults, including patients with disease that is refractory to itraconazole and fluconazole. Prophylaxis of invasive fungal infections among patients 13 years of age and older, who are at high risk of developing these infections, such as patients with prolonged neutropenia or haemopoietic stem cell transplant (HSCT) recipients. Contraindications for use: • Noxafil is contraindicated in patients with known hypersensitivity to posaconazole or to any of the excipients. • Coadministration of posaconazole and ergot alkaloids (ergotamine, dihydroergotamine) is contraindicated as posaconazole may increase the plasma concentration of ergot alkaloids, which may lead to ergotism (see Interactions with Other Medicines). • Coadministration with the HMG-CoA reductase inhibitors that are primarily metabolised through CYP3A4 is contraindicated since increased plasma concentration of these drugs can lead to rhabdomyolysis. • Although not studied in vitro or in vivo, coadministration of posaconazole and certain drugs metabolised through the CYP3A4 system (terfenadine, astemizole, cisapride, pimozide and quinidine) may result in increased plasma concentrations of those drugs, leading to potentially serious and/or life threatening adverse events, such as QT prolongation and rare occurrences of torsades de pointes (see Interactions with Other Medicines). Author: Christina Crosbie V1.2 Effective: Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Adverse effects: Common – Neutropenia, fever, rash, headache, dizziness nausea, vomiting, abdominal pain, diarrhoea, elevated liver enzymes. Infrequent – Hypokalaemia, respiratory insufficiency, oedema constipation. Rare – adrenal insufficiency, tongue or facial oedema, thrombocytopenia, other blood dyscrasias, serious hepatotoxicity including hepatic failure, anaphylactic/anaphylactoid reactions, alopecia (especially with prolonged courses), peripheral neuropathy (more common with long-term use). Indications for use in practice: Initial prescription will be at the instruction of the patients treating consultant and Infectious Diseases (ID). Subsequent prescriptions will be for repeat prescriptions only and only after discussion with the patients treating consultant haematologist and/or ID.. Endorsed By: ____________________________________________________ Date: ________________________ Effective Date: _______________________ Review Date: Author: Christina Crosbie V1.2 Effective: ______________________ Christina Crosbie – Sir Charles Gairdner Hospital – Nurse Practitioner Haematology Clinical Protocol Amendment Appendix 1 Author: Christina Crosbie V1.2 Effective: Author: Christina Crosbie Version 1.2 Effective: August 2014 – Review: 2017 Author: Christina Crosbie V1.2 Effective: Author: Christina Crosbie V1.2 Effective: Author: Christina Crosbie V1.2 Effective: