Adrenergic Blocker
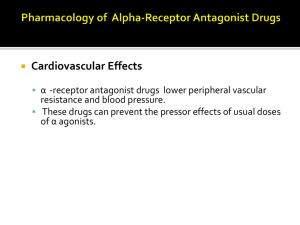
advertisement

ADRENERGIC ANTAGONISTS The adrenergic antagonists, also called blockers. The adrenergic antagonists are classified according to their relative affinity for α or β receptors in the peripheral nervous system. Classification of Adrenergic Blockersα-blockers or antagonists Selective α1-blockers Prazosin Doxazosin Alfuzosin Terazosin Tamsulosin Indoramin Selective α2-blockers Yohimbine Non – selective α-blockers Phenoxybenzamine Phentolamine; Tolazoline β-blockers or antagonists Selective β1-blockers Atenolol Acebutolol Metoprolol Bisoprolol Esmolol Betaxolol Selective β2-Blocker Butoxamine Non-selective β-blockers Propranolol Pindolol Timolol Nadolol Penbutolol Sotalol Mixed antagonists Both α & β- blockers Labetalol Carvedilol α1-adrenergic blockers Pharmacological EffectsA. Cardiovascular effects1. Prazosin, Terazosin, Doxazosin block α1-receptors on peripheral vascular smooth muscles, cause vasodolation, decrease peripheral vascular resistance, decrease blood pressure. 2.Postural hypotension 3.Reflex tachycardia B.Other effects1.Miosis 2.Nasal stuffiness 3.Decreased resistance to the flow of urine 4.Decrease adrenergic sweating Therapeutic uses1.Primary systemic hypertension 2.Congestive Cardiac Failure (CCF) 3.Benign prostatic hyperplasia 4.In Raynaud’s disease Adverse Effects-First dose phenomenon -Postural hypotension -Reflex tachycardia -Headache -Nasal congestion Prazosin was the first α1-selective antagonist. It is a short acting. Doxazosin & Terazosin have longer half-lives with once - daily dosing. They are highly selective & cause vasodilatation & fall in arterial pressure, but less tachycardia than occurs with nonselective α-adrenoceptor antagonists. Some postural hypotension may occur. PhenoxybenzaminePhenoxybenzamine block α-receptors irreversibly, so its duration of action is prolong (14-48 hours). Phenoxybenzamine blocks catecholamine-induced vasoconstriction, decrease peripheral vascular resistance, decrease blood pressure. • Uses1.In the treatment of Pheochromocytoma 2.In Raynaud’s disease • Adverse Effects-Postural hypotension - Fatigue -Tachycardia -Sedation -Nasal stuffiness -Nausea -Inhibition of ejaculation Phentolamine Phentolamine produces a competitive block of α1 and α2 receptors. Phentolamine causes a reduction in peripheral vascular resistance through blockade of α1 receptors and possibly α2 receptors on vascular smooth muscle. • Uses• In the treatment and diagnosis of pheochromocytoma. • Adverse Effects• • • • • Severe tachycardia Arrhythmia Myocardial ischemia Diarrhoea Increase gastric acid production • Clinical uses of α-receptor blocking drugs1. Pheochromocytoma (Phenoxybenzamine, Phentolamine) 2. Hypertensive emergencies (due to pheochromocytoma, overdosage of sympathethomimetic drugs or clonidine withdrawl - Phentolamine) 3. Chr. Hypertension (Prazosin, Terazosin, Doxazosin, Indoramin) 4. Benign prostatic hyperplasia. (Prazosin, Terazosin, Doxazosin, Tamsulosin) 5. Peripheral vascular disease eg.Raynaud’s disease (Phentolamine, Prazosin, Phenoxybenzamine) 6. Local vasoconstrictor excess (Phentolamine) 7. Urinary obstruction eg.Benign prostatic hyperplasia (Prazosin, Terazosin, Doxazosin, Tamsulosin) Β-Adrenoceptor Blockers • • • • • • Selective β1-blockers-Atenolol -Acebutolol -Metoprolol -Esmolol -Betaxolol -Bisoprolol Non-selective β-blockers• • • • • • -Propranolol -Penbutolol -Pindolol -Nadolol -Carteolol -Timolol • PropranololIt is very useful for lowering blood pressure in mild to moderate hypertension. In severe hypertension, propranolol is especially useful in preventing the reflex tachycardia that often results from treatment with direct vasodilators. It is also used in angina and arrhythmia. • M/A• As Antihypertensive – Propranolol blocks the β1 receptors in the heart and causes myocardial depression, decrease heart rate, decrease force of contraction, decrease cardiac output, decrease blood pressure. Propranolol by blocking β1-receptors in the kidney suppress renin-angiotensin mechanism and decrease blood pressure. By central anxiolytic activity, it decreases peripheral sympathetic effect and decrease vascular resistance and decrease blood pressure. As AntianginalPropranolol blocks the β1-receptor in the heart, decrease force of contraction, decrease heart rate & thus decrease myocardial work load. As a result myocardial oxygen requirement is decreased & relief angina. • PharmacokineticsA. AbsorptionPropranolol is well absorbed after oral administration. Peak concentration occur 1-3 hours after ingestion. B.BioavailabilityPropranolol undergoes extensive hepatic metabolism, its bioavailability is relatively low(20%). C.Distribution and clearenceThe β-antagonists are rapidly distributed and have large volume of distribution. Propranolol and penbutolol are quite lipophilic and readily cross blood brain barrier. Most β-antagonists have half-lives in the range of 3-10 hrs. Esmolol is rapidly hydrolyzed and has a half-life of 10 min. Propranolol and metoprolol are extensively metabolized in the liver. Atenolol and pindolol are less completely metabolized. Nadolol is excreted unchanged in the urine. Pharmacological effects of β-blockers1. Effects on the Cardiovascular System-Decrease force of contraction of heart -Decrease heart rate -Decrease cardiac output -Decrease Blood Pressure 2. Effects on the Respiratory TractBy blocking β2 receptors in the bronchial smooth muscle, increase airway resistance particularly in patients with Br. asthma. 3. Effects on EyeSeveral β-blockers (Timolol, Betaxolol) reduce intraocular pressure, specially in glaucomatous eyes by decreasing aqueous humor production. 4. Metabolic and Endocrine effects-Inhibit glycogenolysis in the liver. -Increase plasma concentration of VLDL and decrease concentration of HDL. 5.On KidneyBy blocking β1-receptors in the juxtraglomerulas apparatus, decrease renin secretion, decrease renin angiotensin mechanism and decrease blood pressure. 6.Local anaesthetic effectLocal anaesthetic effect or membrane stabilizing effect is due to blockade of sodium channel. Pharmacological Actions1.Antihypertensive Effect 2.Antianginal Effect 3.Antiarrhythmic Effect Clinical uses of β- blockers1. Hypertension. 2. Ischaemic Heart Disease. 3.Cardiac Arrhythmia 4.Glaucoma 5.Hyperthyroidism (Decrease peripheral conversion of thyroxine to tri-iodothyronine) 6.Migrain headache 7. Certain tremors. 8.Treating alcohol withdrawal 9.Decrease portal vein pressure in patient with cirrhosis • Toxicity/ Adverse Effects1. Drug allergy-eg. Rash, Fever- Rare. 2. Withdrawal symptomsEg.-Nervousness -Tachycardia -Increased intensity of angina -MI may occur. 3. Bronchoconstriction 4. Disturbances of Metabolism - Decrease glycogenolysis -Decrease Glucagon secretion -Fasting hypoglycemia may occur. -Increase Triglycerides -Increase VLDL, decrease HDL 5. CNS EffectsNight mares, lassitude, mental depression, insomnia. 6. Peripheral vascular disease or vasospastic disorders. 7. Drug interactionCimetidine, Frusemide, Chlorpromazine potentiate antihypertensive effects of propranolol by decreasing its metabolism. Conversely, Barbiturate, Phenytoin and Rifampicin decrease its antihypertensive effects by stimulating its metabolism. • Contraindications• • • • • 1.Br. Asthma 2.Diabetes Mellitus 3.Hypotension 4.Bradycardia 5.Congestive Cardiac Failure • Atenolol, MetoprololThey are selective β1 –blockers. These agents may be safer in patients who experience bronchoconstriction responses to propranolol. Β1-selective antagonists may be preferable in patients with diabetes or peripheral vascular disease. They are not appreciably metabolized and are excreted in the urine. Atenolol produce fewer CNS related effects than other β1-blockers. Atenolol is used for Angina Pectoris and Hypertension. • Dose25mg-100mg orally once a day. • Betaxolol and BisoprololThey are β1- selective blockers that are primarily metabolized in the liver but have long half-lives. These drugs can be administered once daily. • Esmolol• Esmolol is an ultrashort acting β1-selective adrenoceptor antagonist. Esmolol has a short half-life (about 10 min).Therefore, during continuous infusion of esmolol, steady state concentrations are achieved quickly and the therapeutic actions of the drug are terminated rapidly when its infusion • is discontinued. Esmolol is potentially much safer to use than long-acting antagonists in critically ill patients who require a β-adrenoceptor antagonist. Esmolol may be useful in controlling supraventricular arrhythmias, peri-operative hypertension and myocardial ischaemia in acutely ill patients. • Timolol• Timolol is a non-selective agent with no local anaesthetic activity. It has excellent ocular hypotensive effects when administered topically in the eye. • Labetalol and CarvedilolLabetalol and Carvedilol block both α and β receptors. Blood pressure is lowered by reduction of systemic vascular resistance without significant alteration in heart rate or cardiac output. Because of its combined α and β-blocking activity, labetalol is useful in treating hypertension of pheochromocytoma and hypertensive emergencies. Carvedilol antagonizes the actions of catecholamines more potentially at βreceptors than at α-receptors. The drug has a half-life of about 6-8 hours. The usual starting dosage of carvedilol for ordinary hypertension is 6.25mg twice daily. It is extensively metabolized in the liver. Because of its vasodilator and antioxidant properties, carvedilol may be used following myocardial infarction to protect against dysrhythmias and repeated infarction.These effects may contribute to the clinical benefits of the drug in congestive heart- failure.