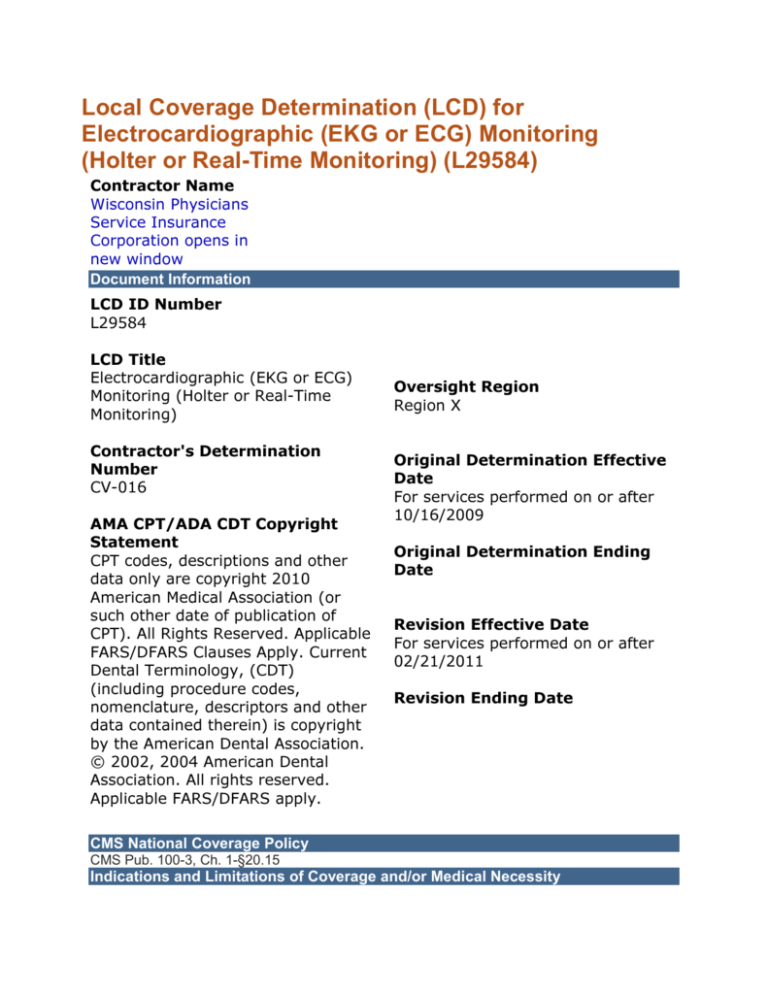
Local Coverage Determination (LCD) for
Electrocardiographic (EKG or ECG) Monitoring
(Holter or Real-Time Monitoring) (L29584)
Contractor Name
Wisconsin Physicians
Service Insurance
Corporation opens in
new window
Document Information
LCD ID Number
L29584
LCD Title
Electrocardiographic (EKG or ECG)
Monitoring (Holter or Real-Time
Monitoring)
Contractor's Determination
Number
CV-016
AMA CPT/ADA CDT Copyright
Statement
CPT codes, descriptions and other
data only are copyright 2010
American Medical Association (or
such other date of publication of
CPT). All Rights Reserved. Applicable
FARS/DFARS Clauses Apply. Current
Dental Terminology, (CDT)
(including procedure codes,
nomenclature, descriptors and other
data contained therein) is copyright
by the American Dental Association.
© 2002, 2004 American Dental
Association. All rights reserved.
Applicable FARS/DFARS apply.
Oversight Region
Region X
Original Determination Effective
Date
For services performed on or after
10/16/2009
Original Determination Ending
Date
Revision Effective Date
For services performed on or after
02/21/2011
Revision Ending Date
CMS National Coverage Policy
CMS Pub. 100-3, Ch. 1-§20.15
Indications and Limitations of Coverage and/or Medical Necessity
Long-Term ECG Monitoring is defined as a diagnostic procedure, which can provide continuous
recording capabilities of ECG activities of the patient's heart while the patient is engaged in daily
activities. These can include continuous, patient-demand or *auto-detection devices. The
purpose of these tests is to provide information about rhythm disturbances and waveform
abnormalities and to note the frequency of their occurrence.
Definitions:
Cardiac Event Detection (CED) is a 30-day service for the purpose of documentation and
diagnosis of paroxysmal or suspected arrhythmias.
Holter Monitoring (24-hour ECG monitoring) is a study used to evaluate the patient's ambient
heart rhythm during a full day's (24 Hours) cycle. It is a wearable EKG monitor that records the
overall rhythm and significant arrhythmias.
A. Medical Necessity:
The medical necessity indications listed in this policy must be present in order for these tests to
be covered.
B. Indications for external 48-hour ECG recording (CPT/HCPCS codes 93224-93227) include
one or more of the following
1. Symptoms:
a. Arrhythmias (ICD-9 codes 426.0-426.9, 427.0-427.42, 427.60-427.9)
b. Chest pain (ICD-9 codes 411.1, 786.50, 786.51, 786.59)
c. Syncope (lightheadedness) or near syncope (ICD-9 code 780.2)
d. Vertigo (dizziness) (ICD-9 code 780.4)
e. Palpitations (ICD-9 code 785.1)
f. Transient ischemic episodes (ICD-9 codes 780.02, 781.0, 781.4)
g. Dyspnea (shortness of breath) (ICD-9 codes 786.00-786.09)
2. Evaluation of the response to antiarrhythmic drug therapy (ICD-9 codes V58.69).
3. Evaluation of myocardial infarction (MI) survivors with an ejection fraction of 40% or less.
(ICD-9 codes 410.00-410.92, 411.0, and 412).
4. Assessment of patients with coronary artery disease with active symptoms, to correlate chest
pain with ST-segment changes (ICD-9 codes 413.0-413.9).
5. Other acute and subacute forms of ischemic heart disease. (411.0-411.89).
6. To detect arrhythmias post ablation procedures.
C. Long term 30-day monitoring; Telephonic Transmission of ECG (CPT codes 93228, 93229,
and 93268-93272) involve 24 hour attended monitoring per 30 day period of time; no other EKG
monitoring codes can be billed simultaneously with these codes.
Indications for performing a Telephonic Transmission:
a. Arrhythmias (ICD-9 codes 426.0-426.9, 427.0-427.42, 427.60-427.9);
b. Chest pain (ICD-9 codes 411.1, 786.50, 786.51, 786.59);
c. Syncope (lightheadedness) or near syncope (ICD-9 code 780.2);
d. Vertigo (dizziness) (ICD-9 code 780.4);
e. Palpitations (ICD-9 code 785.1);
f. Transient ischemic episodes (ICD-9 codes 780.02, 781.0, 781.4);
g. Dyspnea (shortness of breath) (ICD-9 codes 786.00-786.09).
h. To initiate, revise or discontinue arrhythmia drug therapy. (V58.69)
i. Evaluation of myocardial infarction (MI) survivors. (ICD-9 codes 410.00-410.92, 411.0, and
412).
j. Evaluation of acute and subacute forms of ischemic heart disease. (411.0-411.89).
k. Assessment of patients with coronary artery disease with active symptoms, to correlate chest
pain with ST-segment changes (ICD-9 codes 413.0-413.9).
Bill Type Codes:
Contractors may specify Bill Types to help providers identify those Bill Types typically used to
report this service. Absence of a Bill Type does not guarantee that the policy does not apply to
that Bill Type. Complete absence of all Bill Types indicates that coverage is not influenced by
Bill Type and the policy should be assumed to apply equally to all claims.
013x Hospital Outpatient
085x Critical Access Hospital
Revenue Codes:
Contractors may specify Revenue Codes to help providers identify those Revenue Codes
typically used to report this service. In most instances Revenue Codes are purely advisory;
unless specified in the policy services reported under other Revenue Codes are equally subject
to this coverage determination. Complete absence of all Revenue Codes indicates that
coverage is not influenced by Revenue Code and the policy should be assumed to apply equally
to all Revenue Codes.
Revenue codes only apply to providers who bill these services to the fiscal intermediary or Part
A MAC. Revenue codes do not apply to physicians, other professionals and suppliers who bill
these services to the carrier or Part B MAC.
Please note that not all revenue codes apply to every type of bill code. Providers are
encouraged to refer to the FISS revenue code file for allowable bill types. Similarly, not all
revenue codes apply to each CPT/HCPCS code. Providers are encouraged to refer to the FISS
HCPCS file for allowable revenue codes.
0489
073X
Cardiology - Other Cardiology
EKG/ECG (Electrocardiogram) - General Classification
CPT/HCPCS Codes
Memory Loop Recordings
93268
93270
EXTERNAL PATIENT AND, WHEN PERFORMED, AUTO
ACTIVATED ELECTROCARDIOGRAPHIC RHYTHM DERIVED
EVENT RECORDING WITH SYMPTOM-RELATED MEMORY
LOOP WITH REMOTE DOWNLOAD CAPABILITY UP TO 30
DAYS, 24-HOUR ATTENDED MONITORING; INCLUDES
TRANSMISSION, PHYSICIAN REVIEW AND INTERPRETATION
EXTERNAL PATIENT AND, WHEN PERFORMED, AUTO
ACTIVATED ELECTROCARDIOGRAPHIC RHYTHM DERIVED
EVENT RECORDING WITH SYMPTOM-RELATED MEMORY
LOOP WITH REMOTE DOWNLOAD CAPABILITY UP TO 30
DAYS, 24-HOUR ATTENDED MONITORING; RECORDING
93271
93272
(INCLUDES CONNECTION, RECORDING, AND
DISCONNECTION)
EXTERNAL PATIENT AND, WHEN PERFORMED, AUTO
ACTIVATED ELECTROCARDIOGRAPHIC RHYTHM DERIVED
EVENT RECORDING WITH SYMPTOM-RELATED MEMORY
LOOP WITH REMOTE DOWNLOAD CAPABILITY UP TO 30
DAYS, 24-HOUR ATTENDED MONITORING; TRANSMISSION
DOWNLOAD AND ANALYSIS
EXTERNAL PATIENT AND, WHEN PERFORMED, AUTO
ACTIVATED ELECTROCARDIOGRAPHIC RHYTHM DERIVED
EVENT RECORDING WITH SYMPTOM-RELATED MEMORY
LOOP WITH REMOTE DOWNLOAD CAPABILITY UP TO 30
DAYS, 24-HOUR ATTENDED MONITORING; PHYSICIAN
REVIEW AND INTERPRETATION
Other up to 48-Hour Recordings
93224
93225
93226
93227
93228
93229
EXTERNAL ELECTROCARDIOGRAPHIC RECORDING UP TO 48
HOURS BY CONTINUOUS RHYTHM RECORDING AND
STORAGE; INCLUDES RECORDING, SCANNING ANALYSIS
WITH REPORT, PHYSICIAN REVIEW AND INTERPRETATION
EXTERNAL ELECTROCARDIOGRAPHIC RECORDING UP TO 48
HOURS BY CONTINUOUS RHYTHM RECORDING AND
STORAGE; RECORDING (INCLUDES CONNECTION,
RECORDING, AND DISCONNECTION)
EXTERNAL ELECTROCARDIOGRAPHIC RECORDING UP TO 48
HOURS BY CONTINUOUS RHYTHM RECORDING AND
STORAGE; SCANNING ANALYSIS WITH REPORT
EXTERNAL ELECTROCARDIOGRAPHIC RECORDING UP TO 48
HOURS BY CONTINUOUS RHYTHM RECORDING AND
STORAGE; PHYSICIAN REVIEW AND INTERPRETATION
EXTERNAL MOBILE CARDIOVASCULAR TELEMETRY WITH
ELECTROCARDIOGRAPHIC RECORDING, CONCURRENT
COMPUTERIZED REAL TIME DATA ANALYSIS AND GREATER
THAN 24 HOURS OF ACCESSIBLE ECG DATA STORAGE
(RETRIEVABLE WITH QUERY) WITH ECG TRIGGERED AND
PATIENT SELECTED EVENTS TRANSMITTED TO A REMOTE
ATTENDED SURVEILLANCE CENTER FOR UP TO 30 DAYS;
PHYSICIAN REVIEW AND INTERPRETATION WITH REPORT
EXTERNAL MOBILE CARDIOVASCULAR TELEMETRY WITH
ELECTROCARDIOGRAPHIC RECORDING, CONCURRENT
COMPUTERIZED REAL TIME DATA ANALYSIS AND GREATER
THAN 24 HOURS OF ACCESSIBLE ECG DATA STORAGE
(RETRIEVABLE WITH QUERY) WITH ECG TRIGGERED AND
PATIENT SELECTED EVENTS TRANSMITTED TO A REMOTE
ATTENDED SURVEILLANCE CENTER FOR UP TO 30 DAYS;
TECHNICAL SUPPORT FOR CONNECTION AND PATIENT
INSTRUCTIONS FOR USE, ATTENDED SURVEILLANCE,
ANALYSIS AND PHYSICIAN PRESCRIBED TRANSMISSION OF
DAILY AND EMERGENT DATA REPORTS
ICD-9 Codes that Support Medical Necessity
Note: ICD-9 codes must be coded to the highest level of specificity.
ACUTE MYOCARDIAL INFARCTION OF ANTEROLATERAL WALL
410.00 - EPISODE OF CARE UNSPECIFIED - ACUTE MYOCARDIAL
410.92 INFARCTION OF UNSPECIFIED SITE SUBSEQUENT EPISODE OF
CARE
411.0 - POSTMYOCARDIAL INFARCTION SYNDROME - OTHER ACUTE AND
411.89 SUBACUTE FORMS OF ISCHEMIC HEART DISEASE OTHER
412
OLD MYOCARDIAL INFARCTION
413.0 - ANGINA DECUBITUS - OTHER AND UNSPECIFIED ANGINA
413.9
PECTORIS
426.0 - ATRIOVENTRICULAR BLOCK COMPLETE - CONDUCTION DISORDER
426.9
UNSPECIFIED
427.0 - PAROXYSMAL SUPRAVENTRICULAR TACHYCARDIA - VENTRICULAR
427.42 FLUTTER
427.60 - PREMATURE BEATS UNSPECIFIED - CARDIAC DYSRHYTHMIA
427.9
UNSPECIFIED
780.02 TRANSIENT ALTERATION OF AWARENESS
780.2
SYNCOPE AND COLLAPSE
780.4
DIZZINESS AND GIDDINESS
781.0
ABNORMAL INVOLUNTARY MOVEMENTS
781.4
TRANSIENT PARALYSIS OF LIMB
785.1
PALPITATIONS
786.00 - RESPIRATORY ABNORMALITY UNSPECIFIED - RESPIRATORY
786.09 ABNORMALITY OTHER
786.50 UNSPECIFIED CHEST PAIN
786.51 PRECORDIAL PAIN
786.59 OTHER CHEST PAIN
V58.69 LONG-TERM (CURRENT) USE OF OTHER MEDICATIONS
Diagnoses that Support Medical Necessity
Diagnoses listed above
ICD-9 Codes that DO NOT Support Medical Necessity
ICD-9 Codes that DO NOT Support Medical Necessity Asterisk Explanation
Diagnoses that DO NOT Support Medical Necessity
Diagnoses not listed above
Documentations Requirements
Medicare Part B monitors for medical necessity, which can include frequency.
Documentation would include a history and physical exam. The record should document the
evaluation, which focuses on the cause(s) of the presenting symptoms and/or the need for
this testing. Some examples are:
1. The patient record has an evaluation and management service that documents the
symptoms experienced by the patient.
2. The patient has had a full workup in the past month with initial tests performed, and
presents with continuing symptoms that indicate the need for long-term monitoring;
3. The patient requires a change in antiarrhythmic medication. In this case, an assessment
of the patient's complaints, the name of the medication stopped and the name of the new
medication should be indicated.
4. In the case of referred tests, documentation of medical necessity may be requested from
the referring physician. These are considered purchased diagnostic tests.
5. Independent diagnostic testing facilities (IDTF) and suppliers must retain records that
include:
a. The referring physician's written orders; and
b. The identity of the employee setting up the tracing.
Documentation should be submitted as indicated when requested or when unusual
circumstances are present. The EMC narrative may be used.
Appendices
Utilization Guidelines
N/A
Sources of Information and Basis for Decision
Pub 100-3, Ch 1- §20.15
Final Rule, Federal Register, Dec. 31, 2002
Other Medical Carriers
Advisory Committee Meeting Notes
This LCD consolidates and replaces all previous policies and publications on this subject by
the carrier and fiscal intermediary predecessors of Wisconsin Physicians Service. This
coverage determination also applies within states outside the primary geographic
jurisdiction that have nominated Wisconsin Physicians Service to process their claims.
Meeting Date
Wisconsin 01/16/2009
Illinois 01/28/2009
Michigan 01/07/2009
Minnesota 01/22/2009
Iowa, Kansas, Missouri, Nebraska 02/12/2009
Any Carrier Advisory Committee (CAC) related information, including Start date and End
Date of Comment Period, reflects the last time this LCD passed through the Comment and
Notice process.
Start Date of Comment Period
02/12/2009
End Date of Comment Period
03/30/2009
Start Date of Notice Period
09/01/2009
Revision History Number
X
Revision History Explanation
09/02/2009 No change to coverage.
06/30/2009 The contractor number 05392 will no longer be valid as of 8/1/2009 as it will be
joining with the W MO number.
Revision to draft 6/30/2009
04/19/2010—In accordance with Section 911 of the Medicare Modernization Act of 2003,
the states of American Somoa, California, Guam, Hawaii, Nevada and Northern Mariana
Islands were removed from this LCD because claims processing for those states are
transitioning from FI Contractor Wisconsin Physician Services (WPS - 52280) to MAC Part A
Contractor Palmetto.
8/1/2010 - The description for Bill Type Code 13 was changed
8/1/2010 - The description for Bill Type Code 85 was changed
8/1/2010
8/1/2010
8/1/2010
8/1/2010
8/1/2010
-
The
The
The
The
The
description
description
description
description
description
for
for
for
for
for
Revenue
Revenue
Revenue
Revenue
Revenue
code
code
code
code
code
0489
0730
0731
0732
0739
was
was
was
was
was
changed
changed
changed
changed
changed
10/18/2010 - In accordance with Section 911 of the Medicare Modernization Act of 2003,
the states of Colorado, New Mexico, Oklahoma and Texas were removed from this LCD
because claims processing for those states are transitioning from FI Wisconsin Physicians
Service (52280) to MAC Part A Trailblazer (04901).
11/21/2010 - For the following CPT/HCPCS codes either the short description and/or the
long description was changed. Depending on which description is used in this LCD, there
may not be any change in how the code displays in the document:
93268 descriptor was changed in Group 2
93270 descriptor was changed in Group 2
93271 descriptor was changed in Group 2
93272 descriptor was changed in Group 2
93224 descriptor was changed in Group 3
93225 descriptor was changed in Group 3
93226 descriptor was changed in Group 3
93227 descriptor was changed in Group 3
93228 descriptor was changed in Group 3
93229 descriptor was changed in Group 3
11/21/2010 - The following CPT/HCPCS codes were deleted:
93012 was deleted from Group 1
93014 was deleted from Group 1
93230 was deleted from Group 3
93231 was deleted from Group 3
93232 was deleted from Group 3
93233 was deleted from Group 3
93235 was deleted from Group 3
93236 was deleted from Group 3
93237 was deleted from Group 3
*01/01/2011, CPT 2011 revisions; Discontinued CPT codes 93012, 93014, 93230, 93231,
93232, 93233, 93235, 93236, and 93237. CPT long description changes CPT codes 93224,
93225, 93226, 93227, 93228, 93229, 93268, 93270, 93271, and 93272. Deleted under
Indications and Limitations paragraph C. Effective 01/01/2011 (one).
02/21/2011 — In accordance with Section 911 of the Medicare Modernization Act of 2003,
the states of Delaware, District of Columbia, Maryland, New Jersey and Pennsylvania were
removed from this LCD because claims processing for these states are transitioning from FI
Wisconsin Physician Service (WPS 52280) to MAC Part A contractor Highmark (12901).
04/01/2011: Annual review. Reformatted. No coverage changes (two).
Reason for Change
Last Reviewed On Date
04/01/2011
Related Documents
This LCD has no Related Documents.
LCD Attachments
Coding and Billing Guidelines opens in new window (PDF - 44 KB )
Final Comments and Response opens in new window (a comment and response document)
(PDF - 49 KB )
Billing and Coding Guidelines 01/01/2011 opens in new window (PDF - 24 KB )
Billing and Coding Guidelines 04/01/2011 opens in new window (PDF - 26 KB )
Updated on 03/24/2011 with effective dates 02/21/2011 - N/A
Updated on 02/10/2011 with effective dates 02/21/2011 - N/A
Updated on 12/16/2010 with effective dates 01/01/2011 - 02/20/2011
Updated on 10/06/2010 with effective dates 10/18/2010 - 12/31/2010
Updated on 10/04/2010 with effective dates 04/19/2010 - 10/17/2010
Updated on 08/01/2010 with effective dates 04/19/2010 - N/A
Updated on 08/01/2010 with effective dates 04/19/2010 - N/A
Updated on 04/14/2010 with effective dates 04/19/2010 - N/A
Updated on 09/02/2009 with effective dates 10/16/2009 - 04/18/2010
Updated on 08/13/2009 with effective dates 10/16/2009 - N/A
Coding and Billing Article
Article Type
Coding and Billing Guidelines
Article Title
Coding and Billing Guidelines for CV-016; Electrocardiographic (EKG or ECG) Monitoring (Holter or
Real-Time Monitoring)
Document Effective Date
10/16/2009
Revision Effective Date:
NA
Article Text:
This article contains the coding and billing guidelines and reasons for denial for LCD CV-016. This
article is intended for use with LCD Electrocardiographic (EKG or ECG) Monitoring (Holter or RealTime Monitoring).
CMS National Coverage Policy
Title XVIII of the Social Security Act section 1862 (a) (1) (A). This section allows coverage and
payment of those services that are considered to be medically reasonable and necessary.
Title XVIII of the Social Security Act section 1862 (a) (7). This section excludes routine physical
examinations and services
Title XVIII of the Social Security Act section 1833 (e). This section prohibits Medicare payment for any
claim which lacks the necessary information to process the claim.
*An asterisk indicates a revision to that section of the companion document
*Italicized font - represents CMS national policy language/wording copied directly from CMS Manuals
or CMS transmittals.
AMA CPT/ ADA CDT Copyright Statement
CPT codes, descriptions and other data only are copyright 2009 American Medical Association (or such
other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS Clauses Apply. Current
Dental Terminology, (CDT) (including procedure codes, nomenclature, descriptors and other data
contained therein) is copyright by the American Dental Association. © 2002, 2004 American Dental
Association. All rights reserved. Applicable FARS/DFARS apply
A. Coding Guidelines
The HCPCS/CPT code(s) may be subject to Correct Coding Initiative (CCI) edits. This information does
not take precedence over CCI edits. Please refer to CCI for correct coding guidelines and specific
applicable code combinations prior to billing Medicare
1. List the appropriate procedure code.
a. If billing for 48 hours for codes 93224-93227 and 93230-93237, indicate this by placing
each date of service on a separate line with a 1 in the unit's box (e.g., 010).
b. The documentation in the progress notes must reflect medical necessity for the service.
2. List the ICD-9 code(s) indicating the reason for the test.
3. The name and NPI number of the referring/ordering physician or qualified non-physician
practitioner must be reported in boxes 17 and 17a of CMS-1500 form or in the EAO record fields
20.0 (for NPI number) and 22.0 (name) when submitting electronically.
4. The physician interpreting the test must be identified on the claim form with his/her sequence
number in Box 24K. For EMC, use NSF format field FA0 - 23, or ANSI - 837 or NM1 - 09 (loop
2310).
5. The codes describing technical work may be billed by an independent diagnostic testing facility
(IDTF) if they meet all requirements listed in the code descriptions and coverage requirements.
They may bill the total component only if the physician interpreting the test is employed or
contracted by the laboratory and is not billing for the interpretation separately. The physician's
name and address must be on record with our WPS Provider Enrollment Department. A letter
should be sent by the physician assigning all monies collected by the laboratory for the
professional codes to the billing laboratory. If a letter is not on file, professional services billed by
the IDTF laboratories will be denied.
6. Do not use the "TC" or "26" modifier with the codes 93012-93237, 93268, 93270, 93271, or
93272, listed in the CPT/HCPCS section of the LCD.
7. For the same dates of service, either the wearable patient monitor or the 24-hour monitor will be
covered (not both).
8. Wearable Mobile Cardiovascular Telemetry
As of 01/01/2009, CPT codes 93228 and 93229 describe wearable mobile cardiovascular
telemetry services. Because of this, wearable mobile cardiovascular telemetry services should no
longer be reported using 93799 Providers are instructed to bill one (1) unit of procedure code
93228 and/or 93229 per a course of treatment that includes up to 30 consecutive days of cardiac
monitoring.
For dates of service prior to 01/01/2009, claims for outpatient mobile cardiovascular telemetry
should be submitted using CPT code 93799 (unlisted cardiovascular service procedure).
CPT code 93229 is the technical component of this service and includes all of the following
within a course of treatment that includes up to 30 consecutive days of cardiac monitoring:
a. Patient hook-up and patient-specific instruction and education
b. Transmission and receipt of ECG
c. Analysis of ECG by nonphysician personnel
d. Medical chart documentation including daily report, patient and/or physician
interaction and response, and summary report at the end of the monitoring
episode
e. Equipment maintenance.
f. All supplies necessary for completion of the monitoring
CPT code 93228 is the professional component of this service and includes review and
interpretation of each 24-hour cardiac surveillance as well as 24-hour availability and response to
monitoring events within a course of treatment that includes up to 30 consecutive days of cardiac
monitoring.
The following documentation requirements apply to all claims reporting CPT code 93228 and/or
93229:
a. The date of service must be reported as the date the patient was initially placed
on the monitor.
b. A monitoring episode (one to 30 consecutive days) is reported as a unit of one.
c. Any additional claims reporting procedure code 93228 or 93229 for ECG
arrhythmia detection and alarm system within an episode of care (one to 30 days
after an initial service) will be denied.
GY and GZ Modifiers
When billing for services, requested by the beneficiary for denial, that are statutorily excluded by
Medicare (i.e. screening), report a screening ICD-9 code and the GY modifier (items or services
statutorily excluded or does not meet the definition of any Medicare benefit)
When billing for services, requested by the beneficiary for denial, that would be considered not
reasonable and necessary, report an ICD-9 code that best describes the patients condition and the GA
modifier if an ABN signed by the beneficiary is on file or the GZ modifier (items or services expected to
be denied as not reasonable) when there is no ABN for the service on file.
B. Types of monitoring and coverage:
1. Continuous 24-hour Monitoring (CPT codes 93224-93227, 93230-93233 and 9323593237) includes a coverage period of 24 hours for one unit of service. No other EKG
monitoring codes can be billed simultaneously with these codes.
2. Patient-Activated 24-Hour Monitoring (CPT codes 93235-93237) includes a coverage
period of 24 hours per unit of service (these codes may be used for up to 48 hours of
continuous or activated monitoring in certain cases).
3. CPT codes 93012-93014 and 93268-93272)
Cardiac event monitor technology varies among different devices. For patient-activated
event monitors, the patient initiates recording when symptoms appear or when instructed
to do so by a physician (e.g., following exercise). For self-sensing automatically
triggered monitors, an EKG is automatically recorded when the device detects an
arrhythmia, without patient intervention. Some devices permit a patient to transmit EKG
data trans-telephonically (i.e., via telephone) to a receiving center where the data is
reviewed. A technician may be available at these centers to review transmitted data 24hours per day. In some instances, when the EKG is determined to be outside certain preset
criteria by a technician or other non-physician, a physician is available 24 hours per
day to review the transmitted data and make clinical decisions regarding the patient.
These services are known as 24 hour "attended monitoring". In other instances,
transmitted EKG data is reviewed at a later time and are, therefore, considered "nonattended."
.
a. The person receiving the transmission must be a technician, nurse, or a
physician trained in interpreting ECG's and abnormal rhythms.
b. A physician must be available 24 hours a day for immediate consultation
to review the transmission in case of significant symptoms or ECG
abnormalities
4. Additionally, the transmitting devices must meet at least the following criteria;
a. They must be capable transmitting EKG Leads I, II or III; and
b. The tracing must be sufficiently comparable to a conventional EKG.
24-hour attended coverage used as early post-hospital monitoring of patients discharged
after MI is only covered if provision is made for such 24-hour attended coverage in the
manner described below.
5. 24-hour attended coverage means there must be, at a monitoring site or central data center, an
EKG technician or other non-physician, receiving calls and/or EKG data. Tape recording
devices do not meet this requirement. Further, such technicians should have immediate 24-hour
access to a physician to review transmitted data and make clinical decisions regarding the
patient. The technician should also be instructed as to when how to contact available facilities to
assist the patient in case of emergencies.
6. Nationally Non-covered Indications
The following indications are non-covered nationally unless otherwise specified below:
a. The time-sampling mode of operation of ambulatory EKG cardiac event
monitoring recording.
b. Separate physician services other than those rendered by an IDTF unless
rendered by the patient's attending or consulting physician.
c. Home EKG services without documentation of medical necessity.
d. Emergency EKG services by a portable x-ray supplier without a physician in
attendance at the time of the service or immediately thereafter.
e. 24-hour attended coverage used as early post-hospital monitoring of patients
discharged after MI unless provision is made for such 24-hour attended coverage
in the manner described in section 4 above.
Published: *09/01/2009
Revision History, Number/Explanation
Final Comments CV-016 Version 2
Bonnie and Dr. Bussan
Final Comments for Electrocardiographic (EKG or ECG) Monitoring (Holter or Real-Time
Monitoring (CV-016)
Comment
A request to add the following comments in the Indications and Limitations of Coverage
and/or Medical Necessity was received and evaluated:
B Indications for 24-hour ECG monitoring include (for CPT/HCPCS codes 9322493237, 93268-93272). Add an indication to state “To detect arrhythmias post
ablation.’
C Extension of 24-hour monitoring codes (93224-93237) to 48 hours will be
allowed under the following conditions only. Add an indication to state “To better
identify arrhythmias in high risk patients.”
Response
The above two statements have been included. The policy now states;
B Indications 24-hour ECG monitoring (CPT/HCPCS codes 93224-93227, 9323093233, and 93235-93237) include one or more of the following
6. To detect arrhythmias post ablation procedures
C Extension of 24-hour monitoring CPT codes (93224-93237) to 48 hours will be
allowed under the following conditions only
4. To better identify arrhythmias in high risk patients. (For ICD-9 codes see
section B above, sentence 1. a).
Comment
For CPT code 93229 please clarify “physician prescribed”, and what supporting
documentation is required.
Response
CPT code 93229 must be physician ordered.
The following documentation applies to all claims reporting CPT code 93228 and/or
93229:
a. The date of service must be reported as the date the patient was
initially placed on the monitor.
b. A monitoring episode (one to 30 consecutive days) is reported as a
unit of one.
c. The total number days the patient was monitored must be reported
in the claim narrative. (E.g. ECG arrhythmia detection and alarm
system 10 days).
d. Any additional claims reporting procedure code 93228 or 93229
for ECG arrhythmia detection and alarm system within an episode
of care (one to 30 days after an initial service) will be denied.
Comment:
In the Cardiac Event Monitor scenario, 30 days of service, is the physician required to
review reports everyday?
Responses
No daily report is required.
Final Comments CV-016 Version 2
Bonnie and Dr. Bussan
Comment:
The title of the LCD could be revised to make it clear that it includes all types of longterm
ECG monitoring – not only holter and “real-time” monitoring.
Response
The title is Electrocardiographic (EKG or ECG) Monitoring. The subtitle is (Holter or Real-Time
Monitoring) and is not meant to be all-inclusive. WPS is confident that this title and subtitle
accurately describe the policy.
Comment:
Some of the terminology is confusing. It would be helpful if you included definitions.
Response
The following definitions have been added under section Indications and Limitations of
Coverage and/or Medical Necessity:
Definitions:
Cardiac Event Detection (CED) is a 30-day service for the purpose of
documentation and diagnosis of paroxysmal or suspected arrhythmias.
Holter Monitoring (24-hour ECG monitoring) is a study used to evaluate the
patient’s ambient heart rhythm during a full day’s (24 Hours) cycle. It is a
wearable EKG monitor that records the overall rhythm and significant
arrhythmias.
Comment
Paragraph B should only include the 24 hour monitoring codes. The list in paragraph B
should be 93224-93227, 93230-93233 and 93235-93237.
Response
Paragraph B has been revised to only include CPT codes 93224-93227, 93230-93233 and
93235-93237.
Comment
CPT Codes 93268-93272 referenced in paragraph B are 30-day codes and thus should be in
paragraph D with the other 30-day codes
Response
Paragraph B has been revised to only include CPT codes 93224-93227, 93230-93233 and
93235-93237. CPT codes 93268-93272 have been moved to paragraph D.
Comment
CPT codes 93224-93237 referenced in paragraph B would incorrectly include new CPT codes
93228 and 93229 which describe 30-day cardiac telemetry.
Response
Paragraph B has been revised to only include CPT codes 93224-93227, 93230-93233 and
93235-93237, specific for 24 hour monitoring.
Comment
Final Comments CV-016 Version 2
Bonnie and Dr. Bussan
Paragraph C erroneously includes the new CPT codes 93228 and 93229 for 30 day
telemetry services. CPT codes 93228 and 93229 belong in Paragraph D.
Response
CPT codes 93228 and 93229 have been moved to paragraph D.
Comment
The statement in the coding guidelines, section B, paragraph 1, referring to continuous 24-hour
monitoring as including CPT codes 93224-93237 is incorrect since that range of codes also
includes the new 30-day telemetry codes. This should be revised to refer to CPT Codes 9322493227, 93230-93233 and 93235-93237.
Response
The statement in the coding guidelines referenced above has been revised to state the following;
Continuous 24-hour Monitoring (CPT codes 93224-93227, 93230-93233 and
93235-93237) includes a coverage period of 24 hours for one unit of service. No
other EKG monitoring codes can be billed simultaneously with these codes.
Comment
The statement in the coding guidelines found in Section B; paragraph 2 seems to allow for
multiple continuous days of billing. However, CPT codes (93232-93237) are defined as codes for
24 hours. Allowing these codes to be used on a daily basis for continuous monitoring for
more than 24 hours undermines CPT and Medicare coding and reimbursement principles
which require that multiple days of monitoring, beyond 24 or, in certain cases, 48 hours
should be coded using the 30-day codes.
Response.
The statement in the coding guidelines, section B, paragraph 2 has been revised to state the
following;
Patient-Activated 24-Hour Monitoring (CPT codes 93235-93237) includes a
coverage period of 24 hours per unit of service (these codes may be used for up to
48 hours of continuous or activated monitoring in certain cases
Comment
The statement found in the coding guidelines, section B, paragraph three should be
clarified by adding the specific CPT codes that apply which are 93012-93014 and 9326893272.
3. Cardiac event monitor technology varies among different devices. For
patient-activated event monitors, the patient initiates recording when
symptoms appear or when instructed to do so by a physician (e.g.,
following exercise). For self-sensing automatically triggered monitors, an
EKG is automatically recorded when the device detects an arrhythmia,
without patient intervention. Some devices permit a patient to transmit
EKG data trans-telephonically (i.e., via telephone) to a receiving center
where the data is reviewed. A technician may be available at these
centers to review transmitted data 24- hours per day. In some instances,
when the EKG is determined to be outside certain pre-set criteria by a
technician or other non-physician, a physician is available 24 hours per
day to review the transmitted data and make clinical decisions regarding
the patient. These services are known as 24 hour "attended monitoring".
Final Comments CV-016 Version 2
Bonnie and Dr. Bussan
In other instances, transmitted EKG data is reviewed at a later time and
are, therefore, considered "non-attended."
Response
To clearly identify the codes this section pertain to, CPT Codes 93012-93014 and 9326893272 now precedes the statement from CMS found in section B, paragraph three.
Comment From:
There is a concern that physicians may not be able to use or bill for an extended holter
test if the existing holter codes cannot be used to bill for more than a 24 or 48 hour holter
test. Physicians have indicated that for some patients, traditional holters, CEMs, or even
the new MCT devices, may not be as efficient and effective as an extended holter for
assessing AF Burden (the extended holter eliminates the noise of patient activated and
auto-trigger events during the extended study period). In addition, the extended holter
devices may also be more effective in monitoring how different drug regimens affect
atrial fibrillation or PVC suppression.
Response
Holter monitoring is only allowed up to 48 hours. If you have literature supporting the
use of holter monitoring for longer than 48 hours WPS Medicare will be happy to review
the literature.
Comment
A request was made asking that the LCD clearly identify the types of ECG monitoring
services that are covered. The draft LCD uses the terms holter monitoring, real-time
monitoring, long-term ECG monitoring, continuous 24 hour monitoring, patient
activiaterd 24 hour monitoring, and telephonic transmission of ECG without definition,
which will cause confusion if implemented. It is not clear whether these are overlapping
terms or whether they each refer to a different type of service. It would be helpful if the
terminology was defined and consistent. and if the
Response
WPS has added definitions and has changed patient activated to wearable where applicable.
Comment
Please clarify section A; Paragraph 7 found in the coding and billing guidelines. Statement that
either the patient-activated or the 24-hour monitor will be covered but not both needs
clarification. Does this refer to two services furnished on the same day, or simply at anytime for
the same beneficiary? It is very common for a patient to require a 30-day event monitor
following a 24-hour holter monitor if the 24-hour monitor has failed to detect the patient’s
arrhythmia.
Response
Section A, paragraph seven now states; “For the same dates of service, either the wearable
patient monitor or the 24-hour monitor will be covered (not both)”.
Comment
Section A; Paragraph seven: Request clarification of what is meant by the “patient-activated
monitor.” CPT codes 93268-93272, which are 30-day event monitoring codes are “patientactivated”
and 93225-93227, which are 24-hour codes, are also possibly “patient-activated.”
Response.
Final Comments CV-016 Version 2
Bonnie and Dr. Bussan
Where applicable, patient activated has been revised to say wearable.
Comment
In the coding and billing article, section A; paragraph eight, the reference to “Automatic Sensing
Device Detected Arrhythmia Monitoring” is not correct terminology for CPT Codes 93228 and
93229. We ask that the terminology be changed to “wearable mobile cardiovascular telemetry,”
so as to be consistent with CPT.
Response
All references to Automatic Sensing Device Detected Arrhythmia Monitoring have been
changed to Wearable Mobile Cardiovascular Telemetry.
Comment
In the coding and billing article, section A; paragraph eight, we do not see any reason to
require the provider include in the narrative the total number of days the patient was
monitored. This is not required with respect to any of the other 30-day cardiac
monitoring codes and would not have implications for payment since the payment is for
30 days regardless of the number of days monitored.
Response
The statement “The total number days the patient was monitored must be reported in the
claim narrative. (E.g. ECG arrhythmia detection and alarm system 10 days)” has been
deleted.
Comment
In the coding and billing guidelines, section A; paragraph eight request that WPS clarify that CPT
codes 93228 and 93229 do not “replace CPT code 93799, but rather state “ wearable mobile
cardiovascular telemetry should no longer be reported using 93799.
Response
The coding and billing guideline section referenced above has been revised and now says:
As of 01/01/2009, CPT codes 93228 and 93229 describe wearable mobile
cardiovascular telemetry services. Because of this, wearable mobile
cardiovascular telemetry services should no longer be reported using 93799
Providers are instructed to bill one (1) unit of procedure code 93228 and/or 93229
per a course of treatment that includes up to 30 consecutive days of cardiac
monitoring.
For dates of service prior to 01/01/2009, claims for outpatient mobile
cardiovascular telemetry should be submitted using CPT code 93799 (unlisted
cardiovascular service procedure
Billing and Coding Guidelines
Title
Billing and Coding Guidelines for CV-016; Electrocardiographic (EKG or ECG) Monitoring (Holter or
Real-Time Monitoring)
Document Effective Date
10/16/2009
Revision Effective Date:
*01/01/2011
Text:
This document contains the coding and billing guidelines and reasons for denial for LCD CV-016. This
article is intended for use with LCD Electrocardiographic (EKG or ECG) Monitoring (Holter or RealTime Monitoring).
CMS National Coverage Policy
Title XVIII of the Social Security Act section 1862 (a) (1) (A). This section allows coverage and payment
of those services that are considered to be medically reasonable and necessary.
Title XVIII of the Social Security Act section 1862 (a) (7). This section excludes routine physical
examinations and services
Title XVIII of the Social Security Act section 1833 (e). This section prohibits Medicare payment for any
claim which lacks the necessary information to process the claim.
*An asterisk indicates a revision to that section of the companion document
*Italicized font - represents CMS national policy language/wording copied directly from CMS Manuals
or CMS transmittals.
AMA CPT/ ADA CDT Copyright Statement
CPT codes, descriptions and other data only are copyright 2009 American Medical Association (or such
other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS Clauses Apply. Current
Dental Terminology, (CDT) (including procedure codes, nomenclature, descriptors and other data
contained therein) is copyright by the American Dental Association. © 2002, 2004 American Dental
Association. All rights reserved. Applicable FARS/DFARS apply
A. Coding Guidelines
The HCPCS/CPT code(s) may be subject to Correct Coding Initiative (CCI) edits. This information does
not take precedence over CCI edits. Please refer to CCI for correct coding guidelines and specific
applicable code combinations prior to billing Medicare
1. List the appropriate procedure code.
a. If billing for 48 hours for codes 93224-93227, indicate this by placing each date of service on a
separate line with a 1 in the unit's box (e.g., 010).
b.
The documentation in the progress notes must reflect medical necessity for the service.
2. List the ICD-9 code(s) indicating the reason for the test.
3. The name and NPI number of the referring/ordering physician or qualified non-physician practitioner
must be reported in boxes 17 and 17a of CMS-1500 form or in the EAO record fields 20.0 (for
NPI number) and 22.0 (name) when submitting electronically.
1.
The physician interpreting the test must be identified on the claim form with his/her sequence number in
Box 24K. For EMC, use NSF format field FA0 - 23, or ANSI - 837 or NM1 - 09 (loop 2310).
5. The codes describing technical work may be billed by an independent diagnostic testing facility (IDTF)
if they meet all requirements listed in the code descriptions and coverage requirements. They may
bill the total component only if the physician interpreting the test is employed or contracted by
the laboratory and is not billing for the interpretation separately. The physician's name and
address must be on record with our WPS Provider Enrollment Department. A letter should be sent
by the physician assigning all monies collected by the laboratory for the professional codes to the
billing laboratory. If a letter is not on file, professional services billed by the IDTF laboratories
will be denied.
6. Do not use the "TC" or "26" modifier with the codes 93224-93229, 93268, 93270, 93271, or 93272,
listed in the CPT/HCPCS section of the LCD.
1.
For the same dates of service, either the wearable patient monitor or the up to 48-hour monitor will be
covered (not both).
8. Wearable Mobile Cardiovascular
As of 01/01/2009, CPT codes 93228 and 93229 describe wearable mobile cardiovascular
telemetry services. Because of this, wearable mobile cardiovascular telemetry services should no
longer be reported using 93799 Providers are instructed to bill one (1) unit of procedure code
93228 and/or 93229 per a course of treatment that includes up to 30 consecutive days of cardiac
monitoring
For dates of service prior to 01/01/2009, claims for outpatient mobile cardiovascular telemetry
should be submitted using CPT code 93799 (unlisted cardiovascular service procedure).
CPT code 93229 is the technical component of this service and includes all of the following
within a course of treatment that includes up to 30 consecutive days of cardiac monitoring:
a. Patient hook-up and patient-specific instruction and education b. Transmission and
receipt of ECG
c. Analysis of ECG by nonphysician personnel
d. Medical chart documentation including daily report, patient and/or physician
interaction and response, and summary report at the end of the monitoring
episode
e. Equipment maintenance.
f. All supplies necessary for completion of the monitoring
CPT code 93228 is the professional component of this service and includes review and
interpretation of each 24-hour cardiac surveillance as well as 24-hour availability and response to
monitoring events within a course of treatment that includes up to 30 consecutive days of cardiac
monitoring.
The following documentation requirements apply to all claims reporting CPT code 93228 and/or
93229:
a. The date of service must be reported as the date the patient was initially placed on the
monitor.
b. A monitoring episode (one to 30 consecutive days) is reported as a unit of one.
c. Any additional claims reporting procedure code 93228 or 93229 for ECG arrhythmia
detection and alarm system within an episode of care (one to 30 days after an
initial service) will be denied.
GY and GZ Modifiers
When billing for services, requested by the beneficiary for denial, that are statutorily excluded by
Medicare (i.e. screening), report a screening ICD-9 code and the GY modifier (items or services
statutorily excluded or does not meet the definition of any Medicare benefit)
When billing for services, requested by the beneficiary for denial, that would be considered not
reasonable and necessary, report an ICD-9 code that best describes the patients condition and the GA
modifier if an ABN signed by the beneficiary is on file or the GZ modifier (items or services expected to
be denied as not reasonable) when there is no ABN for the service on file.
B. Types of monitoring and coverage:
1. Continuous up to 48-hour Monitoring (CPT codes 93224-93227), includes a coverage period of
up to 48-hours for one unit of service. No other EKG monitoring codes can be billed
simultaneously with these codes.
1.
CPT codes 93268-93272
Cardiac event monitor technology varies among different devices. For patient-activated
event monitors, the patient initiates recording when symptoms appear or when instructed
to do so by a physician (e.g., following exercise). For self-sensing automatically
triggered monitors, an EKG is automatically recorded when the device detects an
arrhythmia, without patient intervention. Some devices permit a patient to transmit EKG
data trans-telephonically (i.e., via telephone) to a receiving center where the data is
reviewed. A technician may be available at these centers to review transmitted data 24hours per day. In some instances, when the EKG is determined to be outside certain preset criteria by a technician or other non-physician, a physician is available 24 hours per
day to review the transmitted data and make clinical decisions regarding the patient.
These services are known as 24 hour "attended monitoring". In other instances,
transmitted EKG data is reviewed at a later time and are, therefore, considered "nonattended."
.
a.
The person receiving the transmission must be a technician, nurse, or a physician trained in interpreting
ECG's and abnormal rhythms.
b.
A physician must be available 24 hours a day for immediate consultation to review the transmission in
case of significant symptoms or ECG abnormalities
1.
Additionally, the transmitting devices must meet at least the following criteria;
a.
They must be capable transmitting EKG Leads I, II or III; and
b.
The tracing must be sufficiently comparable to a conventional EKG.
24-hour attended coverage used as early post-hospital monitoring of patients discharged
after MI is only covered if provision is made for such 24-hour attended coverage in the
manner described below.
1.
24-hour attended coverage means there must be, at a monitoring site or central data center, an EKG
technician or other non-physician, receiving calls and/or EKG data. Tape recording devices do not meet
this requirement. Further, such technicians should have immediate 24-hour access to a physician to
review transmitted data and make clinical decisions regarding the patient. The technician should also be
instructed as to when how to contact available facilities to assist the patient in case of emergencies.
6. Nationally Non-covered Indications
The following indications are non-covered nationally unless otherwise specified below:
a.
The time-sampling mode of operation of ambulatory EKG cardiac event monitoring recording.
b.
Separate physician services other than those rendered by an IDTF unless rendered by the patient's
attending or consulting physician.
c.
Home EKG services without documentation of medical necessity.
d.
Emergency EKG services by a portable x-ray supplier without a physician in attendance at the time of the
service or immediately thereafter.
e.
24-hour attended coverage used as early post-hospital monitoring of patients discharged after MI unless
provision is made for such 24-hour attended coverage in the manner described in section 4 above.
Published: 09/01/2009
Revision History, Number/Explanation
01/01/2011, Billing and Coding document revised to reflect the 2011 CPT Coding revisions. Revisions
include the following; Deleted under Coding Guidelines section, sentence six, CPT codes 93012 and
93014. Changed under Coding Guidelines section, sentence seven to state up to 48-hours. Revised under
section B;Types of monitoring and coverage sentence one to state up to 48-hours and deleted CPT codes
93230-93233 and 93235-93237. Deleted under section B;Types of monitoring and coverage, sentence
two. Under section B;Types changed sentence three to sentence two and deleted CPT codes 93012 and
93014 (one).
Billing and Coding Guidelines
Title
Billing and Coding Guidelines for CV-016; Electrocardiographic (EKG or ECG) Monitoring (Holter or
Real-Time Monitoring)
Document Effective Date
10/16/2009
Revision Effective Date:
*04/01/2011
Text:
This document contains the coding and billing guidelines and reasons for denial for LCD CV-016. This
article is intended for use with LCD Electrocardiographic (EKG or ECG) Monitoring (Holter or RealTime Monitoring).
CMS National Coverage Policy
Title XVIII of the Social Security Act section 1862 (a) (1) (A). This section allows coverage and payment
of those services that are considered to be medically reasonable and necessary.
Title XVIII of the Social Security Act section 1862 (a) (7). This section excludes routine physical
examinations and services
Title XVIII of the Social Security Act section 1833 (e). This section prohibits Medicare payment for any
claim which lacks the necessary information to process the claim.
*An asterisk indicates a revision to that section of the companion document
*Italicized font - represents CMS national policy language/wording copied directly from CMS Manuals
or CMS transmittals.
AMA CPT/ ADA CDT Copyright Statement
CPT codes, descriptions and other data only are copyright 2009 American Medical Association (or such
other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS Clauses Apply. Current
Dental Terminology, (CDT) (including procedure codes, nomenclature, descriptors and other data
contained therein) is copyright by the American Dental Association. © 2002, 2004 American Dental
Association. All rights reserved. Applicable FARS/DFARS apply
A. Coding Guidelines
The HCPCS/CPT code(s) may be subject to Correct Coding Initiative (CCI) edits. This information does
not take precedence over CCI edits. Please refer to CCI for correct coding guidelines and specific
applicable code combinations prior to billing Medicare
1.
*CPT codes for holter monitoring services (CPT codes 93224-93227) are intended for up to 48 hours of
continuous recording. For 48 hour monitoring codes (CPT 93224-93227):
a.
The documentation in the progress notes must reflect medical necessity for the service.
b. These services may be reported globally with CPT codes 93224. Use the date of physician review
as the date of service (DOS).
c. When submitting claims for the recording only (CPT code 93225) or for the analysis
with report only (CPT code 93226) use the date the service was performed as the
DOS.
d. When submitting claims for physician review and interpretation (CPT code 93227) use
the date the service was performed as the DOS.
e. For less than 12 hours continuous recording, modifier -52 (reduced services) should be
appended. (2011 Insider’s View p. 181)
2. List the ICD-9 code(s) indicating the reason for the test.
3. The name and NPI number of the referring/ordering physician or qualified non-physician practitioner
must be reported in boxes 17 and 17a of CMS-1500 form or in the EAO record fields 20.0 (for
NPI number) and 22.0 (name) when submitting electronically.
1.
The physician interpreting the test must be identified on the claim form with his/her sequence number in
Box 24K. For EMC, use NSF format field FA0 - 23, or ANSI - 837 or NM1 - 09 (loop 2310).
5. The codes describing technical work may be billed by an independent diagnostic testing facility (IDTF)
if they meet all requirements listed in the code descriptions and coverage requirements. They may
bill the total component only if the physician interpreting the test is employed or contracted by
the IDTF and is not billing for the interpretation separately. The physician's name and address
must be on record with our WPS Provider Enrollment Department. A letter should be sent by the
physician assigning all monies collected by the IDTF for the professional codes to the billing
IDTF. If a letter is not on file, professional services billed by the IDTF will be denied.
6. Do not use the "TC" or "26" modifier with the codes 93224-93229, 93268, 93270, 93271, or 93272,
listed in the CPT/HCPCS section of the LCD.
1.
For the same dates of service, either the wearable patient monitor or the up to 48-hour monitor will be
covered (not both).
8. External Mobile Cardiac Telemetry Monitors
As of 01/01/2009, CPT codes 93228 and 93229 describe wearable mobile cardiovascular
telemetry services. Because of this, wearable mobile cardiovascular telemetry services should no
longer be reported using 93799 Providers are instructed to bill one (1) unit of procedure code
93228 and/or 93229 per a course of treatment that includes up to 30 consecutive days of cardiac
monitoring
*As of 01/01/2011, the term wearable mobile cardiovascular telemetry services, is changed to
external mobile cardiovascular telemetry services.
*As of 01/01/2011, do not report CPT code 93228 with CPT codes 93224 and 93227.
*As of 01/01/2011, do not report CPT code 93229 with CPT codes 93224 and 93226.
For dates of service prior to 01/01/2009, claims for outpatient mobile cardiovascular telemetry
should be submitted using CPT code 93799 (unlisted cardiovascular service procedure).
CPT code 93229 is the technical component of this service and includes all of the following
within a course of treatment that includes up to 30 consecutive days of cardiac monitoring:
a. Patient hook-up and patient-specific instruction and education b. Transmission and
receipt of ECG
c. Analysis of ECG by nonphysician personnel
d. Medical chart documentation including daily report, patient and/or physician
interaction and response, and summary report at the end of the monitoring
episode
e. Equipment maintenance.
f. All supplies necessary for completion of the monitoring
CPT code 93228 is the professional component of this service and includes review and
interpretation of each 24-hour cardiac surveillance as well as 24-hour availability and response to
monitoring events within a course of treatment that includes up to 30 consecutive days of cardiac
monitoring.
The following documentation requirements apply to all claims reporting CPT code 93228 and/or
93229:
a. The date of service must be reported as the date the patient was initially placed on the
monitor.
b. A monitoring episode (one to 30 consecutive days) is reported as a unit of one.
c. Any additional claims reporting procedure code 93228 or 93229 for ECG arrhythmia
detection and alarm system within an episode of care (one to 30 days after an
initial service) will be denied.
GY and GZ Modifiers
When billing for services, requested by the beneficiary for denial, that are statutorily excluded by
Medicare (i.e. screening), report a screening ICD-9 code and the GY modifier (items or services
statutorily excluded or does not meet the definition of any Medicare benefit)
When billing for services, requested by the beneficiary for denial, that would be considered not
reasonable and necessary, report an ICD-9 code that best describes the patients condition and the GA
modifier if an ABN signed by the beneficiary is on file or the GZ modifier (items or services expected to
be denied as not reasonable) when there is no ABN for the service on file.
B. Types of monitoring and coverage:
1. Continuous up to 48-hour Monitoring (CPT codes 93224-93227), includes a coverage period of
up to 48-hours for one unit of service. No other EKG monitoring codes can be billed
simultaneously with these codes.
1.
CPT codes 93268-93272
Cardiac event monitor technology varies among different devices. For patient-activated
event monitors, the patient initiates recording when symptoms appear or when instructed
to do so by a physician (e.g., following exercise). For self-sensing automatically
triggered monitors, an EKG is automatically recorded when the device detects an
arrhythmia, without patient intervention. Some devices permit a patient to transmit EKG
data trans-telephonically (i.e., via telephone) to a receiving center where the data is
reviewed. A technician may be available at these centers to review transmitted data 24hours per day. In some instances, when the EKG is determined to be outside certain preset criteria by a technician or other non-physician, a physician is available 24 hours per
day to review the transmitted data and make clinical decisions regarding the patient.
These services are known as 24 hour "attended monitoring". In other instances,
transmitted EKG data is reviewed at a later time and are, therefore, considered "nonattended."
.
a.
The person receiving the transmission must be a technician, nurse, or a physician trained in interpreting
ECG's and abnormal rhythms.
b.
A physician must be available 24 hours a day for immediate consultation to review the transmission in
case of significant symptoms or ECG abnormalities
1.
Additionally, the transmitting devices must meet at least the following criteria;
a.
They must be capable transmitting EKG Leads I, II or III; and
b.
The tracing must be sufficiently comparable to a conventional EKG.
24-hour attended coverage used as early post-hospital monitoring of patients discharged
after MI is only covered if provision is made for such 24-hour attended coverage in the
manner described below.
1.
24-hour attended coverage means there must be, at a monitoring site or central data center, an EKG
technician or other non-physician, receiving calls and/or EKG data. Tape recording devices do not meet
this requirement. Further, such technicians should have immediate 24-hour access to a physician to
review transmitted data and make clinical decisions regarding the patient. The technician should also be
instructed as to when how to contact available facilities to assist the patient in case of emergencies.
6. Nationally Non-covered Indications
The following indications are non-covered nationally unless otherwise specified below:
a.
The time-sampling mode of operation of ambulatory EKG cardiac event monitoring recording.
b.
Separate physician services other than those rendered by an IDTF unless rendered by the patient's
attending or consulting physician.
c.
Home EKG services without documentation of medical necessity.
d.
Emergency EKG services by a portable x-ray supplier without a physician in attendance at the time of the
service or immediately thereafter.
e.
24-hour attended coverage used as early post-hospital monitoring of patients discharged after MI unless
provision is made for such 24-hour attended coverage in the manner described in section 4 above.
Published: 09/01/2009
Revision History, Number/Explanation
04/01/2011: Clarified instructions for CPT codes 93224-93227 found in Coding Guidelines Section,
paragraph one (1).Changed the term wearable mobile cardiovascular telemetry services, per the 2011 CPT
coding update, to external mobile cardiovascular telemetry services; (two).
01/01/2011, Billing and Coding document revised to reflect the 2011 CPT Coding revisions. Revisions
include the following; Deleted under Coding Guidelines section, sentence six, CPT codes 93012 and
93014. Changed under Coding Guidelines section, sentence seven to state up to 48-hours. Revised under
section B; Types of monitoring and coverage sentence one to state up to 48-hours and deleted CPT codes
93230-93233 and 93235-93237. Deleted under section B; Types of monitoring and coverage, sentence
two. Under section B;Types changed sentence three to sentence two and deleted CPT codes 93012 and
93014 (one).