Biology 2402 Notes - Cardiovascular System : Blood Ch 12
advertisement
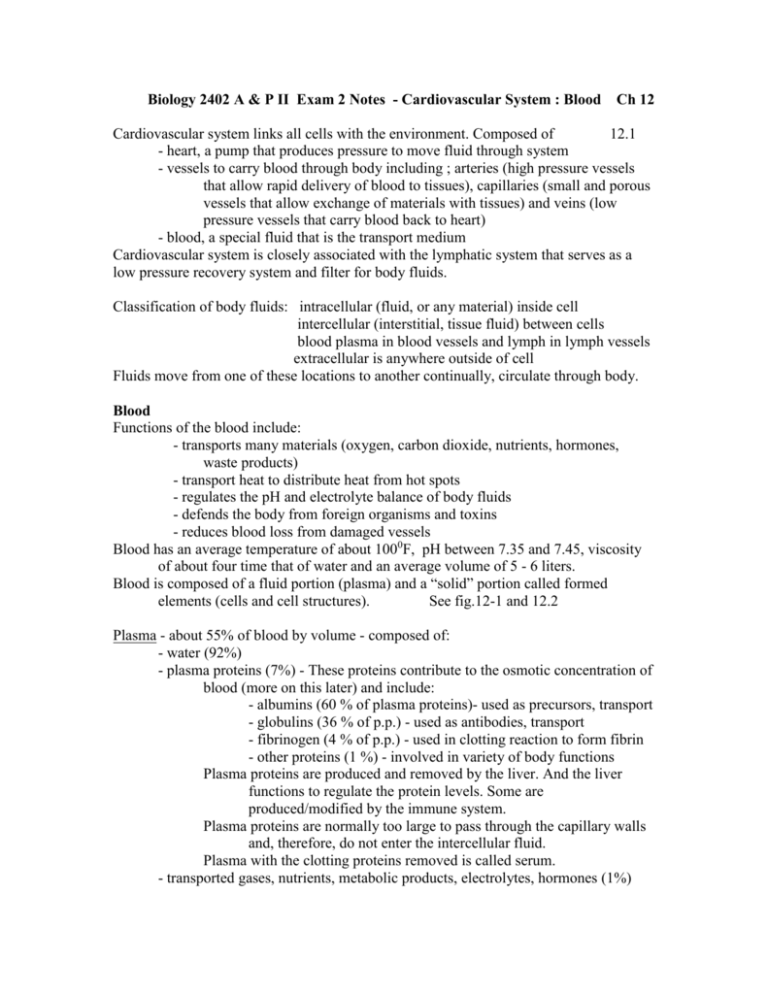
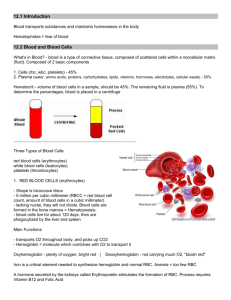
Biology 2402 A & P II Exam 2 Notes - Cardiovascular System : Blood Ch 12 Cardiovascular system links all cells with the environment. Composed of 12.1 - heart, a pump that produces pressure to move fluid through system - vessels to carry blood through body including ; arteries (high pressure vessels that allow rapid delivery of blood to tissues), capillaries (small and porous vessels that allow exchange of materials with tissues) and veins (low pressure vessels that carry blood back to heart) - blood, a special fluid that is the transport medium Cardiovascular system is closely associated with the lymphatic system that serves as a low pressure recovery system and filter for body fluids. Classification of body fluids: intracellular (fluid, or any material) inside cell intercellular (interstitial, tissue fluid) between cells blood plasma in blood vessels and lymph in lymph vessels extracellular is anywhere outside of cell Fluids move from one of these locations to another continually, circulate through body. Blood Functions of the blood include: - transports many materials (oxygen, carbon dioxide, nutrients, hormones, waste products) - transport heat to distribute heat from hot spots - regulates the pH and electrolyte balance of body fluids - defends the body from foreign organisms and toxins - reduces blood loss from damaged vessels Blood has an average temperature of about 1000F, pH between 7.35 and 7.45, viscosity of about four time that of water and an average volume of 5 - 6 liters. Blood is composed of a fluid portion (plasma) and a “solid” portion called formed elements (cells and cell structures). See fig.12-1 and 12.2 Plasma - about 55% of blood by volume - composed of: - water (92%) - plasma proteins (7%) - These proteins contribute to the osmotic concentration of blood (more on this later) and include: - albumins (60 % of plasma proteins)- used as precursors, transport - globulins (36 % of p.p.) - used as antibodies, transport - fibrinogen (4 % of p.p.) - used in clotting reaction to form fibrin - other proteins (1 %) - involved in variety of body functions Plasma proteins are produced and removed by the liver. And the liver functions to regulate the protein levels. Some are produced/modified by the immune system. Plasma proteins are normally too large to pass through the capillary walls and, therefore, do not enter the intercellular fluid. Plasma with the clotting proteins removed is called serum. - transported gases, nutrients, metabolic products, electrolytes, hormones (1%) Formed elements - about 45% of blood by volume - composed of cells or cell parts: - Hematocrit is a measure of blood that is composed of cells (rbc). Slightly higher in males (average 46%) and lower in females (average 42%). - erythrocytes (red blood cells), leukocytes (white blood cells) and platelets. - Process of forming blood cells is called hemopoiesis or hematopoiesis. - All of the blood cells come from stem cells called hematopoietic stem cells. - In adults the site of hemopoiesis is the red bone marrow, but in the fetus hemopoiesis occurs in many locations (liver, spleen, thymus, bone marrow). Inactive red marrow is replaced by fat, called yellow marrow. - Blood cell producing tissues, like red marrow, are also called myeloid tissues. 1. Erythrocytes (red blood cells) Red blood cells are the most numerous blood cells (99.9 %) of all blood cells; 5.4 million per mm3 in males, 4.8 million per mm3 in females. (The space inside this “o” is close to 1 mm3 ) The function of red blood cells is to transport oxygen from the lungs to all body cells and to transport carbon dioxide from body cells to the lungs. Oxygen is used in the break down of glucose in cellular respiration to produce ATP energy. Carbon dioxide is the metabolic waste product from this process. The structure of red blood cells is that of a biconcave disc (flat and caved in on both sides so that they are thinner in the middle). See Fig. 12.3 This shape produces a large surface-area-to-volume ratio (Why is this important?) and is a shape that flexes easily to prevent “jamming” in small vessels. During development of red blood cells most of the cell organelles are removed (nucleus, ribosome, mitochondria) and the mature cells are filled mostly with hemoglobin (about 35% volume) , a protein that binds to and carries oxygen and carbon dioxide. *Describe the structure of red blood cells - list three features that allow these cells to perform their function. *Why is it important that the mitochondria are removed? * What are two important advantages of the biconcave shape of rbc? *What is the function of hemoglobin? The average life span is about 120 days - red blood cells have no way to repair themselves. They are removed in the liver, spleen and bone marrow by phagocytes. About 1% (200 -300 trillion per day) are removed and replaced per day! Protein (amino acid) and Fe++ reused to make hemoglobin, heme excreted by liver as bile. *What is anemia? Describe at least one cause of anemia. *Why is it important that worn red blood cells are recognized and destroyed. Production of red blood cells (a process called erythropoiesis): see Fig. 12.4 hematopoietic stem cells - that can produce any blood cell proerythroblast - cells committed to become red blood cells, divide rapidly erythroblast - produce large quantity of hemoglobin reticulocytes - nucleus, mitochondria, ribosomes removed; cytoskeleton pulls cell into biconcave disc - cells enter circulation mature red blood cells *List four things that occur in the process of a hematopoietic stem cell becoming a mature rbc. Negative feedback regulation of erythropoiesis (Why is this important?): see Fig. 12.5 - particular cells in the kidney are sensitive to hypoxia (low oxygen) - these cells release the hormone erythropoietin, which circulates to bone marrow - erythropoietin stimulates more rapid division of stem cells and production of hemoglobin in erythroblast - more rbc are produced, which increase oxygen transported in blood *What does the hormone erythropoietin do to maintain homeostasis? Where is it produced and what triggers its production? *Why do we call this method of controlling rbc production a "negative feedback"? Blood groups and transfusion reactions: Red blood cells (and most other cells) have genetically determined molecules in their cell membranes that identify them as “self” and their location in the body. The presence of markers determines blood type. One gene, with several variations, determines the ABO blood type. Individuals produce antibodies against “non-self” shortly after birth without exposure. Describe the possible blood types of humans and the molecules markers (antigens) and antibodies present in each blood type. See Fig. 12.17 - 12.18 Describe the events that occur in a cross-reaction. An antibody will attach to its antigen and cause clumping (agglutination). Fig. 12.18 Genes Antigens Blood Type Antibodies (agglutinogen) (agglutinin) A A A I I or I i A only A anti-B IBIB or IBi B only B anti-A IAIB A and B AB none ii none O anti-A and anti-B *What antibodies would a person with blood type A have? Type AB? Type O? Another gene with two variations determines another marker, the Rh factor. DD or Dd Rh Rh+ none -dd none Rh anti-Rh after exposure Many other markers are known but have minor effects on blood compatibility. 2. Leukocytes (white blood cells) - are much less numerous than erythrocytes (4,000 - 11,000/mm3). - defend the body from foreign microbes and toxins, remove foreign material and waste, and destroy abnormal cells and cell debris. - circulate in the blood but also move from the blood into the tissues - the number in the blood is only a small part of the total number. White blood cells have some distinctive properties and abilities: - have a nucleus and other cell organelles - can move on their own by amoeboid movement - can move through very small openings (like in the pores of capillaries) by a process called diapedesis Fig. 12.12 - can move toward an area of high concentration of some chemicals, chemotaxis - can crawl around an object and engulf it, phagocytosis. Membrane sacs of digestive enzymes called lysosomes in these cells allow the object to be digested. *How do white blood cells leave the blood vessels while the smaller red blood cells are normally not able to? *What is chemotaxis and why is it important to body defense? *Why are white blood cells not considered when the hematocrit is measured? White blood cells are classified by their staining characteristic (the particular stain that the cells accept). Granular and agranular leukocytes are distinguished by the presence of staining particle in the cytoplasm. See Fig. 12.7 - 12.11 Five different white blood cells circulate in the blood and each has it particular function: - neutrophils - 54-62% of wbc - phagocytosis of bacteria, arrive at infection site quickly - eosinophil - 1-3% of wbc - phagocytosis of antibody/antigen complex - allergic reactions and parasitic infections (antibody “tagged”) increase number - basophils - 1% of wbc - move to damaged tissues and release chemicals that enhance inflammation (heparin and histamines) and attract other wbc (chemotaxis) - monocytes - 3-9% - become macrophage in tissues, large cells that remove any foreign material by phagocytosis. Slower but more effective than smaller phagocytes. - lymphocytes - 25-33% of wbc - most are located in lymphatic tissues where they are involved in immunity (antibodies). (more on these cells later) A blood test called a differential wbc count compares the numbers of the different wbc and can be used to identify and distinguish infections. White blood cell production See Fig. 12.4 - from hematopoietic stem cells in bone marrow (lymphocyte may develop from stem cells that have located in lymphoid tissues) - regulation of white blood cell production is poorly understood, but involves several hormones called interleukins and colony-stimulating factors. These are chemicals released by damaged cells and white blood cells encountering foreign material (microbes, toxins, etc.). *List five types of leukocytes and tell what the main job of each one is? *What is the job of colony-stimulating factors - what do they do? *Describe three things that white blood cells can do that red blood cells cannot do. 3. Platelets (thrombocytes) - produced by large cells in the bone marrow called megakaryocytes. These cells develop from hematopoietic stem cells, like all other blood cells, under the influence of the hormone thrombopoietin . Fig. 12.4 - platelets are membrane sacs with cytoplasm and chemicals that are fragments of a megakaryocyte, several thousand per megakaryocyte. - blood contains 130,000 - 360,000 platelets per mm3 which have a relatively short life span of 10-12 days - platelets are involved in the blood clotting process to maintain hemostasis Hemostasis is a series of steps that prevent blood loss from damaged blood vessels: - vascular spasm, contraction of smooth muscle in vessel walls to restrict blood flow - first response - vascular phase - damaged cells of vessel attract and become sticky to platelets, which attract and stick to other platelets - form platelet plug - platelet phase Fig. 12.13 - clotting (coagulation) forms fibrin clot that seals and pulls together damaged vessel walls - coagulation phase Fig. 12.14 - 12.16 - caused by a chain reaction called a cascade - initiated by chemicals released by damaged cells - inactive plasma proteins are converted into soluble active proteins, which is the stimulus for the next reaction - tissue plasminogen activators (tpa) are proteins that are released by damaged cells and dissolve clot - are slower to start acting but later dissolve clot - thrombus is a clot in place, an embolus is a clot that breaks loose and flows with blood - can block small vessels *List the three stages of hemostasis from the quickest to the slowest. *List the reactions in the clot formation starting with the release of prothrombin activator from damaged cells. *What are tissue plasminogen activators and why are they important?