Corbis Bisoprolol
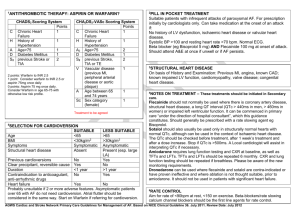
advertisement

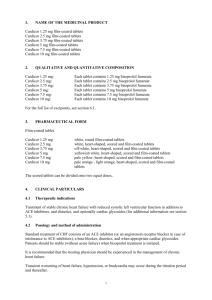
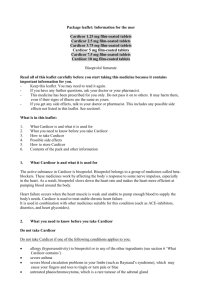
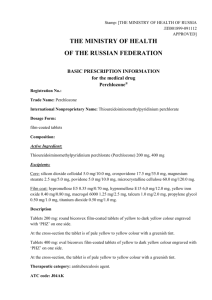
Corbis Bisoprolol Oral use Film-coated tablets Formulae Corbis 2.5 Film-coated tablets: Each film-coated tablet contains Bisoprolol fumarate 2.5 mg. Excipients: Pregelatinized corn starch; Crospovidone; Colloidal silicon dioxide; Microcr ystalline cellulose; Magnesium stearate; Hydroxypropyl methylcellulose; Titanium dioxide; Triacetin. Corbis 5 Film-coated tablets: Each film-coated tablet contains Bisoprolol fumarate 5 mg. Excipients: Pregelatinized corn starch; Crospovidone; Colloidal silicon dioxide; Microcr ystalline cellulose; Magnesium stearate; Hydroxypropyl methylcellulose; Titanium dioxide; Triacetin; Red ferric oxide; Yellow ferric oxide. Corbis 10 Film-coated tablets: Each film-coated tablet contains Bisoprolol fumarate 10 mg. Excipients: Pregelatinized corn starch; Crospovidone; Colloidal silicon dioxide; Microcr ystalline cellulose; Magnesium stearate; Hydroxypropyl methylcellulose; Titanium dioxide; Triacetin. Therapeutic Action ß 1-selective adrenergic blocking agent. Ing.10410 Indications Treatment of hypertension. Prevention of angina pectoris. Treatment of moderate to severe stable congestive heart failure associated to decrease in ventricular systolic function, in combination with angiotensin-conver ting enzyme (ACE) inhibitors, diuretics and in some cases cardiac glycosides. Pharmacological Action Bisoprolol is a potent and highly ß 1 -selective adrenergic blocking agent. It does not exhibit intrinsic sympathomimetic nor relevant membrane-stabilizing activity. Due to its poor affinity for ß 2 -adrenergic receptors of bronchial and vascular smooth muscle and for those involved in metabolic regulation Bisoprolol should not affect airways resistance nor metabolic effects mediated by these receptors. Like for other betablockers, the mechanism of action of Bisoprolol in hypertension was not completely established, although it is known that it reduces cardiac output, plasma renin activity and tonic sympathetic outflow from the vasomotor centers in the brain. In patients suffering from angina pectoris, the ß1-adrenergic receptor blocking effect leads to a decrease in cardiac demand of oxygen due to a decrease in cardiac activity. In patients with stable congestive heart failure under treatment with diuretics and ACE-inhibitors treatment with Bisoprolol was shown to improve left ventricular function, reducing hospitalizations due to decompensation, to improve the NYHA functional class and to decrease the incidence of sudden death increasing sur vival rate. Pharmacokinetics: Bisoprolol is absorbed almost completely in the gastrointestinal tract. Its first pass metabolism is ver y low, thus showing a bioavailability of nearly 90%. Its protein binding is of about 30%. The plasma elimination half-life ranges from 10 to 12 hours, which accounts for a 24-hours activity with a once daily dosing. Nearly 95% of the dose administered is eliminated in the urine, with about 50% of this amount appearing as unchanged Bisoprolol. No pharmacologically active metabolites were found in humans. Dose adjustment is generally not necessar y in patients with renal or hepatic failure. In patients suffering from chronic stable heart failure (NYHA class III) higher plasma levels and an extension in plasma elimination half-life (17 ± 5 hours) were obser ved. Dosage and Administration Adults: Hypertension and angina pectoris: Usual dose is 10 mg once daily. In some patients a 2.5 mg or 5 mg dose once daily may be sufficient. Maximum recommended daily dosage is 20 mg. Heart failure: Its use is recommended for patients suffering from chronic stable heart failure who did not show acute decompensation in the course of the last six weeks and did not require changes in their basic treatment during the last two weeks. These patients should be under treatment with optimal doses of ACE-inhibitors (or other vasodilators in case of intolerance to ACE-inhibitors), diuretics and eventually cardiac glycosides. Treatment with Corbis should be initiated at minimum doses, tapering it gradually according to following scheme: • 1.25 mg once daily during 1 week; in case of good tolerability increase to • 2.5 mg once daily during another week; in case of good tolerability increase to • 3.75 mg once daily during another week; in case of good tolerability increase to • 5 mg once daily during 4 weeks; in case of good tolerability increase to • 7.5 mg once daily during 4 weeks; in case of good tolerability increase to • 10 mg once daily for maintenance treatment. Maximum recommended dose is of 10 mg once daily and it should be achieved in not less than 12 weeks. After administration of the first 1.25 mg dose, the patient should be observed during about 4 hours, specially monitoring blood pressure, hear t rate and eventual signs of impairment of congestive heart failure or conduction disorders. At the first signs of adverse events (symptomatic bradycardia, hypotension, impairment of congestive hear t failure) the administration of the maximum recommended dosage may not be achieved. If necessary, the maximum dose achieved should be reduced gradually. If necessar y, treatment may be discontinued and reinitiated when considered appropriate. In case of impairment of congestive heart failure, it is recommended to adjust the doses of the basic treatment (ACE-inhibitors, diuretics). It is recommended not to discontinue treatment with Bisoprolol in an abrupt manner as a transient impairment in congestive heart failure may occur. In case discontinuation of Bisoprolol treatment turns necessar y, it is recommended to taper therapy by halves at weekly inter vals. Treatment of chronic stable heart failure with Bisoprolol usually is of long-term duration. Patients with renal or hepatic impairment: In patients with severe renal failure (creatinine clearance < 20 ml/minute) or severe hepatic failure, maximum daily dose should not exceed 10 mg. There are no evidences suggesting that dosage should be altered in patients undergoing hemodialysis. Treatment of congestive heart failure in patients with renal or hepatic failure, requires a cautious dose-adjustment. Geriatric patients: Usually no dose-adjustment is required, but in some patients 5 mg once a day may be sufficient. Contraindications Known hypersensitivity to Bisoprolol or to any components of the product. A s w i t h o t h e r ß 1- a d r e n e r g i c b l o c k i n g a g e n t s , B i s o p r o l o l s h o u l d n o t b e administered to patients with untreated congestive hear t failure, cardiogenic s h o c k , s in u s b lo c k , s in u s n o d e d is e a s e , s e c o n d o r t h ir d d e gr e e AV b lo c k (without pacemaker), bradycardia with a hear t rate of <60 beats/minute prior to treatment, hypotension (systolic blood pressure <100 mm/Hg), advanced peripheral ar terial occlusive disease, Raynaud’s syndrome, severe asthma or severe obstructive airways disease, untreated pheochromocytoma and metabolic acidosis. Warnings Although Bisoprolol is a highly ß 1-selective adrenergic blocking agent it should be administered with caution to patients with chronic obstructive air ways disease or familiar histor y of bronchial asthma. In some patients suffering f r o m a s t h m a o c c a s i o n a l l y a n i n c r e a s e i n a i r w a y s r e s i s t a n c e m a y o c c u r. Usually this type of bronchospasm shows a good response to bronchodilators w i t h ß 2- a d r e n e r g i c r e c e p t o r a g o n i s t e f f e c t l i k e s a l b u t a m o l . L i k e o t h e r betablocking agents, Bisoprolol may increase allergen sensitivity and severity of allergic reactions and may modif y results of adrenaline treatment. Bisoprolol may mask clinical signs of hyperthyroidism (thyrotoxicosis). There is no clinical experience in the treatment of congestive hear t failure in patients with diabetes mellitus type I (insulin-dependent patients), renal failure (serum creatinine ≥ 3.4 mg/dl) or hepatic failure. Precautions Use with caution in patients with first degree AV block or extended PR inter val, Prinzmetal’s angina, bronchospasms (bronchial asthma or obstructive air ways disease), diabetes mellitus with impor tant fluctuations in glycemia (clinical signs of hypoglycemia may be masked), metabolic acidosis, prolonged fasting, ongoing desensitization treatment and peripheral circulator y disorders like occlusive ar terial disease or Raynaud’s syndrome. In patients with ischemic hear t disease treatment should not be discontinued abruptly. Corbis should be administered with caution in diabetic patients as hypoglycemia symptoms (specially tachycardia) may be masked. In patients with histor y of psoriasis, administration of betablocking agents should be cautiously evaluated based upon risk/benefit ratio. Based upon individual differences in the response to Bisoprolol, it should be administered with caution in patients operating automobiles and hazardous machiner y or engaging in other tasks requiring aler tness, especially when initiating treatment, when switching to other doses and in patients drinking alcoholic beverages. Pregnancy: Betablocking agents may develop certain pharmacological effects affecting gestation and the fetus. Administration of betablocking agents during the last stage of pregnancy may produce bradycardia or hypotension in the fetus or the newborn. As with other betablocking agents, Corbis should only be administered during pregnancy if strictly necessar y and if the potential benefit for the mother justifies the potential risk to the mother and the fetus. In case of administration, fetal growth and uteroplacental blood flow should be closely monitored. The newborn must also be closely monitored, as bradycardia or hypoglycemia may appear in the course of the first 3 days of life. Nursing: There are no adequate and well-controlled studies regarding excretion of Bisoprolol in human milk. Af ter evaluating the risk/benefit ratio of the administration of Corbis to nursing mothers and if the potential benefit justifies its use, discontinuation of nursing should be considered. Pediatric use: Since safety and effectiveness of Bisoprolol in pediatric patients have not been established, its administration is not recommended. Use in the elderly: There are no adequate and well-controlled studies in the treatment of congestive hear t failure in patients over 80 years. Overdosage The most common signs expected with overdosage of a betablocking agent are: Bradycardia, hypotension, congestive heart failure, bronchospasm and hypoglycemia. The few cases of overdosage (up to 2000 mg) with Bisoprolol reported were characterized by bradycardia and hypotension. Limited data suggest that Bisoprolol is not dialyzable. In case of overdosage cessation of treatment is recommended, providing symptomatic and supportive treatment. Bradycardia: Administer intravenous atropine. If the response is inadequate, isoproterenol or another agent with positive chronotropic properties may be given cautiously. Under some circumstances, transvenous pacemaker insertion may be necessary. Hypotension: Intravenous fluids or vasopressors should be administered. Intravenous glucagon may be useful. Second or third degree atrioventricular block: Patients should be carefully monitored and treated with isoproterenol infusion or transvenous cardiac pacemaker insertion, as appropriate. Congestive heart failure: Initiate conventional therapy (digitalis glycosides, diuretics, inotropic agents, vasodilators). Bronchospasm: Administer bronchodilator therapy (isoproterenol, ß 2 -adrenergic agonists and / or aminophylline). Hypoglycemia: Administer intravenous glucose. In the event of overdosage attend the nearest hospital or contact the Toxicology Centers: Children’s Hospital Ricardo Gutiérrez: (011) 4962-6666 / 2247, Hospital A. Posadas: (011) 4654-6648 / 4658-7777. Sold under prescription Made in Argentina Product authorized by the Ministry of Health Certificate Nº 48,411 Technical Director: Mirta Beatriz Fariña, Pharmacist Manufactured at José E. Rodó 6424, C1440AKJ Autonomous City of Buenos Aires Last revised: September 2001 Medicinal product Keep out of the reach of children Keep in a dry place at temperature below 30°C Information to Health Care Professionals and Patients: Roemmers S.A.I.C.F. Fray Justo Sarmiento 2350, B1636AKJ Olivos, Pcia. de Buenos Aires www.roemmers.com.ar How Supplied Corbis 2,5 Film-coated tablets: Packages containing 30 film-coated tablets. White, round film-coated tablets, scored and coded BP 2.5 on one side of the tablet, and marked with Roemmers’ identification isologue on the other side. Corbis 5 Film-coated tablets: Packages containing 30 film-coated tablets. Salmon colored, round film-coated tablets, scored and coded BP 5 on one side of the tablet, and marked with Roemmers’ identification isologue on the other side. Corbis 10 Film-coated tablets: Packages containing 30 film-coated tablets. White, round film-coated tablets, scored and coded BP 10 on one side of the tablet, and marked with Roemmers’ identification isologue on the other side. Instructions for breaking scored tablets: I f du e t o m e dic al r e c o mm e n datio n, t able t br e ak ing is n e c e s s ar y, p r o c e e d a s f o llow s: Place the tablet on an even and rigid sur face. Press with the tip of the fingers of both hands, simultaneously, on both sides of the score until breaking the film- coated tablet. 49 Adverse Reactions Corbis is usually well tolerated. Adverse events reported are normally attributed to its pharmacological action. They generally appear when starting treatment, are mild and resume within 1-2 weeks of treatment. C e n t r a l n e r v o u s s y s t e m : O c c a s io n a l l y, w h e n s t a r t i n g t r e a t m e n t, as t he n i a , fatigue, vertigo and mild headache. Ver y rarely: Sleep disturbances, depression. S p e c i a l s e n s e s : Ve r y r a r e l y: Re d u c e d l a c r i m a t i o n, h e a r i n g d i s t u r b a n c e s . C a r d i o v a s c u l a r : O c c a s i o n a l l y: Pa r e s t h e s i a a n d c o l d e x t r e m i t i e s . R a r e l y: Bradycardia, atrioventricular conduction disturbances, congestive heart failure impairment, abrupt fall in blood pressure, orthostatic hypotension. Respirator y: Rarely: Bronchospasm in patients with histor y of bronchial asthma or obstructive airways disease. Digestive: Occasionally: Nausea, vomiting, diarrhea and constipation. Musculoskeletal: Rarely: Muscle weakness, myalgia, muscle twitching. B 1109303872 Ing.10410 0411 Drug Interactions Bisoprolol may potentiate the effects of concomitantly administered antihypertensive agents. Concomitant administration of reserpine, guanethidine, alfa methyldopa and clonidine may produce excessive reduction of sympathetic activity and hear t rate. In patients receiving concurrent therapy with clonidine (not recommended combination) there is an increased risk of rebound hyper tension. If therapy with clonidine is to be discontinued, it is suggested that Corbis be discontinued for several days before the withdrawal of clonidine. Bisoprolol should be used with care when myocardial depressants or inhibitors of AV conduction, such as cer tain calcium antagonists (par ticularly of the phenylalkylamine [verapamil] and benzothiazepine [diltiazem] classes) (not recommended combination) or class I antiarrhythmic agents, such as disopyramide, or class III antiarrhythmic agents, such as amiodarone, are used concurrently. Concurrent administration with digitalis glycosides may decrease hear t rate and slow atrioventricular conduction. It is recommended not to administer intravenous calcium antagonists or antiarrhythmics during treatment with Bisoprolol. Concomitant administration of parasympathomimetics, even tacrine, may slow atrioventricular conduction. Ergotamine derivatives may exacerbate peripheral circulator y disorders. Prostaglandin synthesis inhibitors may decrease the hypotensive effect of Bisoprolol. Concurrent use of rifampicin may shor ten the plasma elimination half-life of Bisoprolol, however usually no dose adjustment is required. Phamacokinetic studies document no clinically relevant interactions with other agents given concomitantly, including thiazide diuretics, and cimetidine. There was no effect of Bisoprolol on prothrombin in patients on stable doses of war farin. Bisoprolol may potentiate the effects of insulin and oral hypoglycemic agents. In case anesthesia is needed, the anesthesiologist must be informed beforehand that the patient is treated with Bisoprolol. In patients with severe ischemic cardiopathy the convenience of continuing treatment with Bisoprolol should be evaluated. Caution should be exer ted when administering cyclopropane or trichloroethylene. Tr i c y c l i c a n t i d e p r e s s a n t s , b a r b i t u r a t e s , p h e n o t h i a z i n e s a n d o t h e r antihyper tensive agents may increase the hypotensive effect of Bisoprolol. Since monoamine A oxidase inhibitors may increase the hypotensive effect of betablocking agents as well as generate the risk of a hyper tensive crisis, their association with Bisoprolol is not recommended. Mefloquine may enhance the risk of bradycardia in patients under treatment with Bisoprolol. Concomitant use of Bisoprolol and sympathomimetic agents may reduce the effect of both medications. Higher doses of epinephrine might be required when treating allergic reactions. 0-800-333-5658