Example - UNC School of Medicine
advertisement
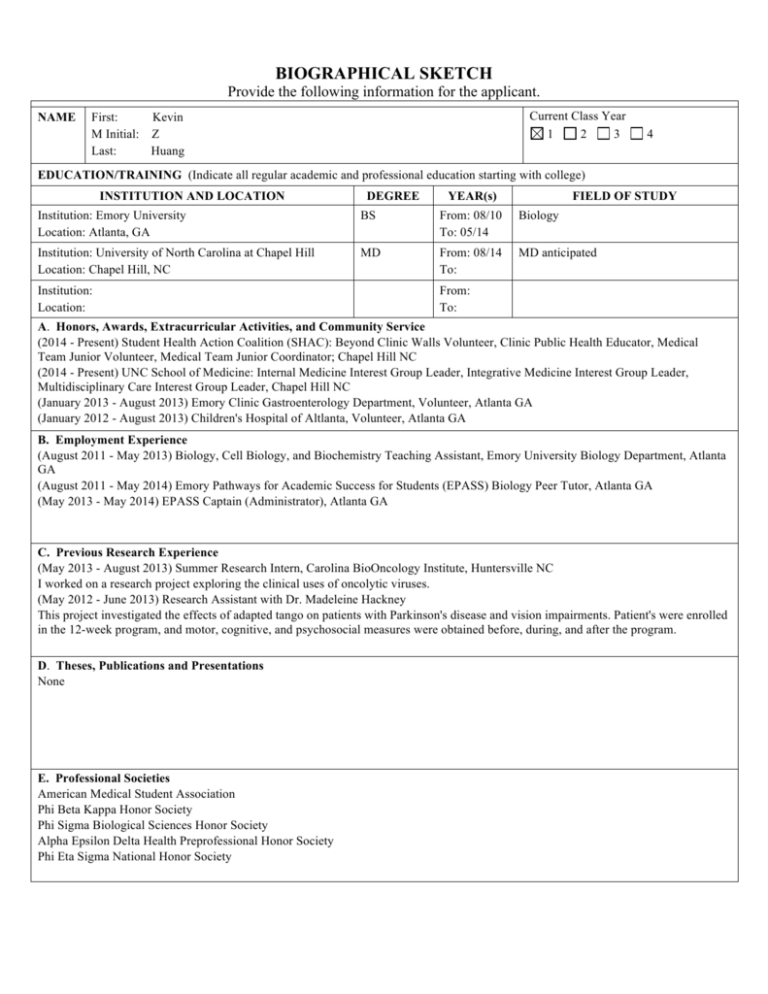
BIOGRAPHICAL SKETCH Provide the following information for the applicant. NAME Current Class Year 1 2 3 First: Kevin M Initial: Z Last: Huang 4 EDUCATION/TRAINING (Indicate all regular academic and professional education starting with college) INSTITUTION AND LOCATION DEGREE YEAR(s) FIELD OF STUDY Institution: Emory University Location: Atlanta, GA BS From: 08/10 To: 05/14 Biology Institution: University of North Carolina at Chapel Hill Location: Chapel Hill, NC MD From: 08/14 To: MD anticipated Institution: Location: From: To: A. Honors, Awards, Extracurricular Activities, and Community Service (2014 - Present) Student Health Action Coalition (SHAC): Beyond Clinic Walls Volunteer, Clinic Public Health Educator, Medical Team Junior Volunteer, Medical Team Junior Coordinator; Chapel Hill NC (2014 - Present) UNC School of Medicine: Internal Medicine Interest Group Leader, Integrative Medicine Interest Group Leader, Multidisciplinary Care Interest Group Leader, Chapel Hill NC (January 2013 - August 2013) Emory Clinic Gastroenterology Department, Volunteer, Atlanta GA (January 2012 - August 2013) Children's Hospital of Altlanta, Volunteer, Atlanta GA B. Employment Experience (August 2011 - May 2013) Biology, Cell Biology, and Biochemistry Teaching Assistant, Emory University Biology Department, Atlanta GA (August 2011 - May 2014) Emory Pathways for Academic Success for Students (EPASS) Biology Peer Tutor, Atlanta GA (May 2013 - May 2014) EPASS Captain (Administrator), Atlanta GA C. Previous Research Experience (May 2013 - August 2013) Summer Research Intern, Carolina BioOncology Institute, Huntersville NC I worked on a research project exploring the clinical uses of oncolytic viruses. (May 2012 - June 2013) Research Assistant with Dr. Madeleine Hackney This project investigated the effects of adapted tango on patients with Parkinson's disease and vision impairments. Patient's were enrolled in the 12-week program, and motor, cognitive, and psychosocial measures were obtained before, during, and after the program. D. Theses, Publications and Presentations None E. Professional Societies American Medical Student Association Phi Beta Kappa Honor Society Phi Sigma Biological Sciences Honor Society Alpha Epsilon Delta Health Preprofessional Honor Society Phi Eta Sigma National Honor Society THE UNIVERSITY of NORTH CAROLINA at CHAPEL HILL EVAN S. DELLON, MD, MPH Associate Professor of Medicine Division of Gastroenterology and Hepatology T 919.966.9757 F 919.843.2508 edellon@med.unc.edu 4140 BIOINFORMATICS BUILDING CAMPUS BOX 7080 CHAPEL HILL, NC 27599-7080 To: Office of Medical Student Research UNC School of Medicine Re: Summer medical student research application for Kevin Huang January 26, 2015 Dear colleagues, It is my pleasure to write this letter supporting Kevin Huang’s application for the Carolina Medical Student Research Program. I have met with him on multiple occasions, have helped him develop his application, and I feel that he is an excellent candidate for this program. Kevin was first introduced to biomedical research during his college years, and has had experiences both in the lab (with oncolytic viruses) and in a clinical setting (evaluating and rehabilitating patients with Parkinson’s). He also excelled academically, being elected to national honors societies in both the humanities and sciences. These early research experiences, now coupled with his first year medical school curriculum, have strongly interested him in exploring clinical and epidemiologic research. For the CMSRP, we have designed a focused research project on eosinophilic esophagitis (EoE) that will give him this introduction to clinical and epidemiologic research. EoE is a newly recognized disease about which much is yet unknown, including the growth outcomes in children treated with different modalities. Specifically, this project aims to determine whether treatment type (topical steroids, dietary elimination, or elemental formula) is associated improved growth outcomes, both in patients being treated the first time and in treatment-refractory patients. This project is circumscribed and feasible in the limited time frame, as data collection and analysis will utilize an existing and previously identified patient population. Specifically, it will use the Carolinas EoE Collaborative (CEoEC), a multicenter network of EoE providers (gastroenterologists, allergist, and dieticians). I am a co-founder of the CEoEC, and a close collaborator with the other co-founders at the non-UNC sites (Asthma and Allergy Specialists in Charlotte, NC; and Pediatric GI in the Greenville, SC, Health System). I will be mentoring Kevin closely on this project. We will meet at minimum on a weekly basis and I expect he will learn not only a substantial amount of background information about EoE, but also key tenants of epidemiologic study design and statistical analysis. I will provide appropriate education about these topics, as well as the financial resources to conduct the data collection and analysis. Kevin is a primary author of, and has been actively involved in, the research design process. My expectation is that with my assistance he will draft and submit the IRB application, identify patients from the three sites and extract data using standard case report forms, create and manage a database, participate in data analysis, interpret the data, present the findings, and draft a manuscript. In short, he will have ownership of this project. I am excited to participate as a mentor in this project and to work with Kevin. I think his selfmotivation, organization, and inquisitiveness that I have already observed, as well as a keen interest in obtaining more exposure to clinical research, makes me confident that he will successfully complete this project. Moreover, I should also note that of his own volition, this past winter he has started to assist me on a separate research project related to EoE, and he will be a co-author on that paper as well in the coming months. In addition, I have worked with a number of medical students at UNC, including those who have participated in the CMSRP, and have successfully mentored them on projects that have been published. Kevin is a great fit for the CMSRP, and he has my strongest recommendation for being accepted. Please do not hesitate to contact me with any questions. Sincerely, Evan S. Dellon, MD MPH Associate Professor of Medicine Division of Gastroenterology and Hepatology University of North Carolina School of Medicine BIOGRAPHICAL SKETCH Provide the following information for the Senior/key personnel and other significant contributors. Follow this format for each person. DO NOT EXCEED FOUR PAGES. NAME POSITION TITLE Dellon, Evan Samuel Associate Professor of Medicine Adjunct Associate Professor of Epidemiology eRA COMMONS USER NAME (credential, e.g., agency login) edellon EDUCATION/TRAINING (Begin with baccalaureate or other initial professional education, such as nursing, and include postdoctoral training and residency training if applicable.) DEGREE INSTITUTION AND LOCATION MM/YY FIELD OF STUDY (if applicable) Brown University, Providence RI Johns Hopkins School of Medicine, Baltimore, MD Massachusetts General Hospital (MGH), Boston, MA – Intern and resident University of North Carolina (UNC) School of Medicine, Department of Medicine, Chapel Hill, NC – Clinical fellow UNC School of Medicine, Department of Medicine, Chapel Hill, NC – Research fellow UNC School of Public Health, Chapel Hill, NC AB 5/95 Health & Society; Music MD 5/99 Medicine -- 1999-2002 Internal Medicine -- 2004-2006 Gastroenterology -- 2006-2008 Gastroenterology MPH 12/07 Epidemiology A. Personal Statement I am an academic gastroenterologist with formal research training in epidemiology, clinical research, and clinical trial design. My goal as a physician-scientist is to lead and collaborate with a multidisciplinary research team in the area of esophageal diseases, and eosinophilic esophagitis (EoE) in particular. My current research focuses on optimizing the diagnosis, characterizing the epidemiology, studying the pathogenesis, and refining the treatment and management of EoE, with the overall goal of improving patient care and outcomes in EoE. I have published over 50 manuscripts and 65 abstracts specifically related to EoE. I am also actively involved in mentoring and advising medical students (including those in the CMSPR program), residents, and postdoctoral fellows in research projects, and this work has also yielded multiple publications. Through my NIHsupported research (KL2, K23, R01), I have established a number of patient cohorts, including the UNC EoE Clinicopathologic Database and the UNC EoE Patient Registry and Specimen Biobank, as well as co-founded the Carolinas EoE Collaborative (CEoEC). This latter resource, a pre-existing multi-site network with existing patient registries, will be utilized for the proposed project. Given my research experience in EoE, my background in clinical, epidemiologic, and translational research techniques, and my ongoing role in mentoring, I am well-suited to be the mentor for this summer research project (please see my letter for full details). B. Positions and Honors Positions and Employment 2002-2004 Hospitalist, Medical Access Unit, Department of Medicine, MGH, Boston, MA 2002-2004 Assistant in Medicine, Department of Medicine, MGH, Boston, MA 2002-2004 Instructor, Harvard Medical School, Boston, MA 2002-2004 In-house physician, Emerson Hospital, Concord, MA 2004 Assistant Director, Medical Access Unit, Department of Medicine, MGHl, Boston, MA 2007-2008 Clinical Instructor, Department of Medicine, UNC, Chapel Hill, NC 2008-2013 Assistant Professor of Medicine, Division of Gastroenterology, UNC, Chapel Hill, NC 2009-2013 Adjunct Asst. Prof. of Epidemiology, UNC School of Public Health, Chapel Hill, NC 2013-present Associate Professor of Medicine, Division of Gastroenterology, UNC, Chapel Hill, NC 2013-present Adjunct Assoc. Prof. of Epidemiology, UNC School of Public Health, Chapel Hill, NC Board Certifications, Professional Memberships, and Other Experience 1997-2000 1999-2004 2002-present 2004-present 2004-present 2004-present 2005-present 2007-present 2007-present 2009-present United States Medical Licensing Exam, completed steps 1-3 Massachusetts Board of Registration in Medicine, licensee American Board of Internal Medicine, Diplomate in Internal Medicine, 2002 North Carolina Medical Board, licensee Member, American Gastroenterological Association Member, American Society for Gastrointestinal Endoscopy Member, American College of Gastroenterology Member, North Carolina Society of Gastroenterology American Board of Internal Medicine, Diplomate in Gastroenterology, 2007 Associate Editor, Digital Atlas of Video Education (http://daveproject.org) Selected Honors 1990 Cricklair Award for best non-M.D. presentation at the Plastic Surgery Research Council meeting 1994 Phi Beta Kappa 1999 Alpha Omega Alpha 1999 Warfield T. Longcope Prize for excellence by a medical student entering the field of Internal Medicine 2005 ACG Travel Award for a top presentation at the 2005 ACG National Fellow’s Forum in Boston 2006 UNC-Wessex Exchange, selected to participate in a GI-fellow exchange to Wessex, England 2008 NC Society of Gastroenterology Clinical Vignette Award 2008 AstraZeneca Emerging Leaders, selected to participate in international program 2008 America College of Gastroenterology (ACG), Junior Faculty Development Award 2008 UNC Clinical Translation Science Award / KL2 Scholars Program participant 2008 ACG/AstraZeneca Senior Fellow Award for a top abstract submitted to the 2008 ACG meeting 2009 UNC Teaching Scholar, selected to participate in this year-long program 2010 UNC GI Fellows Award for Excellence in Mentoring 2010 Best Doctors in America, elected by peers, 2011-2014. 2011 ACG Governors Award for Excellence in Clinical Research at the 2011 ACG meeting 2012 AGA-June and Donald O. Castell Esophageal Clinical Research Award 2012 Gastroenterology Research Group-AGA Young Investigator Clinical Science Award 2012 Ruth and Phillip Hettleman Prize for Artistic and Scholarly Achievement at UNC C. Selected Peer-reviewed Publications (Selected from 109 peer-reviewed publications) Most relevant to the current application 1. Dellon ES, Aderoju A, Woosley J, Sandler RS, Shaheen NJ. Variability in diagnostic criteria for eosinophilic esophagitis: A systematic review. Am J Gastroenterol 2007; 102:2300-2313. [PMID 17617209] 2. Dellon ES, Gibbs WB, Fritchie KJ, Rubinas TC, Wilson LA, Woosley JT, Shaheen NJ. Clinical, endoscopic, and histologic findings distinguish eosinophilic esophagitis from gastroesophageal reflux disease. Clin Gastroenterol Hepatol 2009; 7:2695-2703. [PMID 19733260; PMC2789852] 3. Dellon ES, Gibbs WB, Rubinas TC, Fritchie KJ, Madanick RD, Woosley JT, Shaheen NJ. Esophageal dilation in eosinophilic esophagitis: Safety and predictors of clinical response and complications. Gastroinest Endosc 2010; 71: 706-12. [PMID 20170913; PMC Journal – In Process] 4. Dellon ES, Chen X, Miller CR, Fritchie KF, Rubinas TC, Woosley JT, Shaheen NJ. Tryptase staining of mast cells may differentiate eosinophilic esophagitis from gastroesophageal reflux disease. Am J Gastroenterol 2011; 106: 264-71. [PMID 20978486; PMC Journal – In Process] 5. Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood S, Bonis PA, Burks W, Chehade M, Collins MH, Dellon ES, Dohil R, Falk GW, Gonsalves N, Gupta SK, Katzka D, Lucendo AJ, Markowitz J, Noel RJ, Odze RD, Putnam PE, Richter JE, Romero Y, Ruchelli E, Sampson HA, Schoepfer A, Shaheen NJ, Sicherer SH, Spechler S, Spergel JM, Straumann A, Wershil BK, Rothenberg ME, Aceves S. Eosinophilic Esophagitis: Updated Consensus Recommendations for Children and Adults. J Allergy Clin Immunol, 2011; 128: 3-20. [PMID 21477849; PMC Journal – In Progress] 6. Dellon ES, Peery AP, Shaheen NJ, Morgan DM, Hurrell JM, Lash RH, Genta RM. Inverse association of esophageal eosinophilia with Helicobacter pylori infection based on analysis of a US pathology database. Gastroenterology. 2011; 141: 1586-1592 [PMID 21762663; PMC Journal – In Process] 7. Dellon ES, Sheikh A, Speck O, Woodward K, Whitlow AB, Hores J, Ivanovic M, Chau A, Woosley JT, Madanick RD, Orlando RC, Shaheen NJ. Viscous topical is more effective than nebulized steroid therapy for patients with eosinophilic esophagitis. Gastroenterology. 2012; 143: 321-324.e1. [PMID 22561055; PMC Journal – In Process] 8. Kim HP, Vance RB, Shaheen NJ, Dellon ES. The prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis: A meta-analysis. Clin Gastroenterol Hepatol. 2012; 10: 988-996.e5. [PMID 22610003; PMC Journal – In Process] 9. Dellon ES, Chen X, Miller CR, Woosley JT, Shaheen NJ. Diagnostic utility of major basic protein, eotaxin3, and leukotriene enzyme staining in eosinophilic esophagitis. Am J Gastroenterol. In press, 2012. Epub July 10, 2012. [PMID 22777338; PMC Journal – In Process] 10. Dellon ES,* Gonsalves N,* Hirano I,* Furuta GT, Liacouras CA, Katzka DA. Evidence based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am J Gastroenterol. 2103; 108: 679-92. [PMID 23567357; PMC Journal – In Process] (*Co-first authors) 11. Jensen ET, Kappelman MD, Kim HP, Ringel-Kukla T, Dellon ES. Early life exposures as risk factors for pediatric eosinophilic esophagitis: A pilot and feasibility study. J Pediatr Gastroenterol Nutr. 2013; 57: 6771. 12. Dellon ES, Jensen EC, Martin CF, Shaheen NJ, Kappelman MD. The prevalence of eosinophilic esophagitis in the United States. Clin Gastro Hepatol. 2014; 12: 589-596.e1. 13. Wolf WA, Jerath MR, Sperry SLW, Shaheen NJ, Dellon ES. Dietary elimination therapy is an effective option for adults with eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2014; 12: 1272-9. 14. Dellon ES, Rusin S, Gebhart JH, Covey S, Higgins LL, Beitia R, Speck O, Woodward K, Woosley JT, Shaheen NJ. Utility of a non-invasive serum biomarker panel for diagnosis and monitoring of EoE: A prospective study. Am J Gastroenterol. In press, 2015 15. Burk CM,* Beitia R, Lund PK, Dellon ES. High rate of galactose-alpha-1,3-galactose sensitization in both eosinophilic esophagitis and patients undergoing upper endoscopy. Dis Esoph. In press, 2015. (*2014 CMSRP summer student) D. Research Support Ongoing Research Support NIH K23 DK090073 Dellon (PI) 9/15/2011-7/31/2015 Risk factors and biomarkers for diagnosis and treatment of eosinophilic esophagitis The goals of this proposal are to validate our previously developed model of risk factors for diagnosis of EoE, to assess the utility of serum levels of eotaxin-3 and IL-13 as non-invasive biomarkers in diagnosis and monitoring of treatment of EoE (but there is not an aim to predict treatment response using baseline values), and to develop the PI’s career via a comprehensive training plan designed to increase his knowledge of translational research techniques. ACG Clinic Research Award Dellon (PI) 7/1/2013-6/30/2015 Gene-environment interactions in the development of eosinophilic esophagitis The goal of the proposed study is to assess whether there is interaction between the eotaxin-3 SNP and selected early life exposures that increase odds of developing EoE in children, specifically antibiotic use in infancy and Cesarean delivery. CURED Foundation Dellon (PI) 7/1/2014-6/30/2015 Diagnosis and monitoring of eosinophilic esophagitis using the Cytosponge The goal of this project is to assess the safety, acceptability, and accuracy of Cytosponge for diagnosis and monitoring of EoE in comparison to endoscopy and biopsy as the gold standard NIH R01 CA168959 Mehrotra, PI 8/1/2013-4/30/2017 Measuring and improving colonoscopy quality using natural language processing Evaluation of Growth Outcomes in Children with Eosinophilic Esophagitis Introduction Eosinophilic esophagitis (EoE) is a chronic inflammatory disease characterized by eosinophilic infiltration of esophageal epithelium. Adult patients typically present with food impaction and dysphagia, whereas children present with vomiting, feeding dysfunction, and failure to thrive.1 EoE is thought to be an allergic disease with the underlying pathogenesis related to exposure to food allergens.2 Accordingly, dietary elimination is an effective initial therapy for EoE. Strategies for dietary treatment include selective elimination diets, in which potential food allergens are removed from the diet, and elemental formulas, in which hypoallergenic liquid formulations are administered as the sole source of nutrition. Growth and development is a major concern for pediatric EoE patients, as feeding dysfunction and restrictive diets can prevent patients with EoE from receiving sufficient nutrient intake. Moreover, elimination diets can lead to poor growth and development if nutritional replacements for the eliminated food are not provided.3 Milk and wheat, the two most common allergic triggers of EoE,1 are highly important parts of a child’s diet, and replacement sources are necessary to ensure normal growth and development.3 Use of elemental formulas can circumvent these disadvantages because they provide a complete source of nutrients. Thus, elemental formulas may help children with EoE achieve normal growth by providing a more complete source of nutrients compared to restrictive diets. However, despite the importance of nutrition and growth in children with EoE, outcomes related to growth and EoE-specific treatments have never been examined, and this is a major gap in knowledge. The proposed study seeks to investigate the growth rates for pediatric EoE patients using elemental formulas as compared to elimination diets and pharmacological therapies. We will analyze patient data from the Carolinas EoE Collaborative (CEoEC), a multi-center network that includes UNC (Chapel Hill, NC), Asthma and Allergy Specialists Clinic (Charlotte, NC), and Greenville Health System Children’s Hospital Pediatric Gastroenterology Clinic (Greenville, SC). Specific Aims and Hypotheses Aim 1: To determine the growth rates of children with EoE who were treated initially with elemental formula therapy as compared to those who were initially administered topical steroids and dietary elimination therapies. Hypothesis for Aim 1: Growth rates will be higher in pediatric EoE patients on an elemental formula therapy than those not on an elemental formula therapy. Aim 2: Evaluate the growth of children with refractory EoE (no response to pharmacological or diet elimination therapies) who were placed on elemental formula as compared with the growth of children with refractory EoE who were placed on other second-line treatments. Hypothesis for Aim 2: Children with refractory EoE will have an improved growth rate after starting an elemental formula diet. Background Eosinophilic Esophagitis: Symptoms and Diagnosis Eosinophilic esophagitis (EoE) is a chronic inflammatory disease that is characterized by eosinophilic infiltration of esophageal epithelium. Adult patients typically present with food impaction and dysphagia, whereas children typically present with vomiting, abdominal pain, feeding dysfunction, and failure to thrive.1 Diagnosis of EoE is based on these clinical symptoms and histological evidence of eosinophilic infiltration of the esophageal epithelium.1 Treatments for EoE currently include topical steroids (fluticasone, budesonide), dietary therapies, and endoscopic dilation.1 EoE is linked to food allergies EoE is currently thought to be an allergic disease based on epidemiological data, pathophysiological evidence, and clinical response to trigger food elimination. Like other atopic conditions such as asthma and allergic rhinitis, incidence and prevalence of EoE has grown markedly in the past two decades.4-8 Cohort studies have shown that the majority of EoE patients have concomitant asthma, allergic rhinitis, or atopic dermatitis.7 At the cellular level, EoE is largely a TH2 mediated response, with IL-5 and IL-13 cytokines being critically involved in EoE pathogenesis.7,9-11 Histological remission and symptom improvement in EoE patients undergoing elimination diets provides clinical evidence supporting the link between EoE and food allergies.2 Dietary therapies are effective as treatment of EoE patients Both elemental diets and elimination diets are effective in managing EoE in children.3 Elemental diets involve replacing all intact protein in the diet with a liquid formulation of amino acids.16 Elemental diets have been shown to be more effective at inducing remission than any other therapy including topical steroids,16 and are much more likely to achieve mucosal healing and result in lower residual eosinophil counts.3 However, the high cost of elemental formulas, poor oral tolerability, and need for a feeding tube for certain patients are disadvantages of this approach.1 Because of this, elimination diets based on either allergy test results (“targeted elimination diets”) or with the six most common allergens eliminated (“six-food elimination diets”; SFED) have been developed. Response rates for these approaches range from 60-75%, a level that is comparable to pharmacologic therapy.17 Growth is an important but poorly described consideration in pediatric EoE patients Children with EoE who present with feeding dysfunction can develop maladaptive feeding behaviors.13 Moreover, dietary therapies used to address such symptoms can often lead to impairments in nutritional intake, which can affect growth.3 When compared to healthy controls and expected values based on age, children with food allergies in general, and allergy to cow’s milk in particular, show decreased growth.14,15 While monitoring nutritional intake is important when children are placed on long-term elimination diets,2 outcomes related to this for EoE are poorly described in the current literature. In particular, there is a surprising and unacceptable lack of data concerning growth outcomes based on treatment type. Further research is needed to better understand how dietary management of EoE in children impacts growth rates. Present Study To date, elemental diets, elimination diets, and other EoE treatments have only been compared for their effectiveness in producing clinical and histological remissions. Growth, which is especially important in children with EoE, has not been extensively assessed as a specific outcome, and the various treatment modalities have not been compared with respect to growth outcomes. Analyzing these differences could help pediatric gastroenterologists and nutritionists guide the treatment of pediatric EoE patients and select optimal treatment and nutritional approaches. Therefore, the overall goal of this study is to assess growth outcomes by treatment types in children with EoE, and the central hypothesis is that those who take elemental formula will have better growth outcomes. To do this, we will analyze data from children with EoE from three centers in the Carolinas EoE Collaborative (CEoEC), a consortium of EoE centers in North and South Carolina cofounded and co-directed by the faculty advisor on this project. Research Design and Methods Study Population Our study population will include all children (<18) diagnosed with EoE at University of North Carolina Hospitals (Chapel Hill, NC), Asthma and Allergy Specialists Clinic (Charlotte, NC), and Greenville Health System Children’s Hospital Pediatric Gastroenterology Clinic (Greenville, SC), three of the centers in the CEoEC. We will review records from 2005 - 2014. To assess growth, we will include patients who have at least 3 visits. Study Design and Data This will be a retrospective cohort study. Data on age, demographic, clinical symptoms, endoscopic features, histological findings, anthropometric measures (height, weight, growth velocity), treatment approaches and adherence, and frequency of encounters with the physician and nutritionist will be extracted using a standardized case report form. The same form will be utilized at all sites. Student’s Role The student’s role in this study will be to assist in the study’s design, medical record data abstraction, data analysis, and write up of the results of the study for presentation and publication. Data Analysis Statistical analysis Demographic, clinical, endoscopic, histologic, and treatment-related data for the study population will be summarized using descriptive statistics. Baseline characteristics of EoE patients will be compared by treatment type (steroids vs dietary elimination vs elemental formula) and by the presence or absence of elemental formula supplementation. The primary outcome of interest will be growth. We will use metrics standardized to a normative population, and will specifically calculate both the change in the BMI Z-score and the change in height Z-score pre- and post-therapy. To test the hypotheses stated above, these changes will be compared between initial treatment types (Aim 1) and for refractory treatment types (Aim 2). A longitudinal modeling approach will accommodate adjustment for potential confounders (ie presence of other atopic conditions, EoE disease duration, age, gender, etc), use of multiple data points over time, with variable numbers of data points per subject. We will explore whether a linear mixed effects model may be appropriate to assess change over time, introducing a random effect for intercept (baseline BMI Z-score). Sample Size We have already established that, between 2005 and 2014, approximately 700 pediatric patients have been treated for EoE at the above three centers in the CEoEC. Aim 1: Assuming 80% of patients have a minimum of 3 visits on record, we anticipate a study sample of 560 patients. Aim 2: Of these 560 patients, assuming 40% are refractory to first line elimination diet or pharmacological treatments, we anticipate a study sample of 224 patients. Expected Outcome / Alternative Approaches We predict that EoE patients receiving elemental formulas will have favorable growth rates than EoE patients not on elemental formulas. We also predict that EoE patients refractory to other treatments will regain or experience improved growth following the initiation of elemental diet therapy. It is possible that a number of subjects may have incomplete follow-up data. If that is the case, we will first then compare those with and without incomplete records or missing data to assess for systematic biases. If this does not resolve this issue, we can modify our IRB applications to contact the pediatricians of the patients with incomplete records to acquire the necessary growth data. Candidates Statement The CMSRP program was designed to provide students like me with a meaningful exposure to medical research. My undergraduate and medical studies have peaked my interest in research and the generation of new knowledge, and thus, I believe I would be a perfect fit for this program. This experience will not only be invaluable to my development as a physician-scientist, but will also help me explore the possibilities of pursuing an academic career in medical research in the future. During the course of this research study, I will gain experience working on all aspects of this project, including study design, data collection, analysis, and reporting of results. I am very much looking forward to the process of gaining these skills and working with Dr. Dellon on this project during the upcoming summer. Bibliography 1. Dellon ES, Gonsalves N, Hirano I, et al. ACG clinical guideline: Evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am J Gastroenterol. 2013;108(5):679-92. 2. Kagalwalla AF. Dietary treatment of eosinophilic esophagitis in children. Dig Dis. 2014;32(1-2):114-9. 3. Mehta H, Groetch M, Wang J. Growth and nutritional concerns in children with food allergy. Curr Opin Allergy Clin Immunol. 2013;13(3):275-9. 4. Dellon ES. Epidemiology of eosinophilic esophagitis. Gastroenterol Clin North Am. 2014;43(2):201-18. 5. Hruz P, Straumann A, Bussmann C, et al. Escalating incidence of eosinophilic esophagitis: a 20-year prospective, population-based study in Olten County, Switzerland. J Allergy Clin Immunol. 2011;128(6):1349-1350.e5. 6. Lin SK, Sabharwal G, Ghaffari G. A review of the evidence linking eosinophilic esophagitis and food allergy. Allergy Asthma Proc. 2015;36(1):26-33. 7. Brown-whitehorn TF, Spergel JM. The link between allergies and eosinophilic esophagitis: implications for management strategies. Expert Rev Clin Immunol. 2010;6(1):101-9. 8. Okada H, Kuhn C, Feillet H, Bach JF. The 'hygiene hypothesis' for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010;160(1):1-9. 9. Maggi E. The TH1/TH2 paradigm in allergy. Immunotechnology. 1998;3(4):233-44. 10. Bhardwaj N, Ghaffari G. Biomarkers for eosinophilic esophagitis: a review. Ann Allergy Asthma Immunol. 2012;109(3):155-9. 11. Blanchard C, Wang N, Stringer KF, et al. Eotaxin-3 and a uniquely conserved gene-expression profile in eosinophilic esophagitis. J Clin Invest. 2006;116(2):536-47. 12. Matsuura H, Ishiguro A, Abe H, et al. Elevation of plasma eotaxin levels in children with food allergy. Nihon Rinsho Meneki Gakkai Kaishi. 2009;32(3):180-5. 13. Menard-katcher C, Henry M, Furuta GT, Atkins D, Maune NC, Haas AM. Significance of feeding dysfunction in eosinophilic esophagitis. World J Gastroenterol. 2014;20(31):11019-22. 14. Isolauri E, Sütas Y, Salo MK, Isosomppi R, Kaila M. Elimination diet in cow's milk allergy: risk for impaired growth in young children. J Pediatr. 1998;132(6):1004-9. 15. Mehta H, Ramesh M, Feuille E, Groetch M, Wang J. Growth comparison in children with and without food allergies in 2 different demographic populations. J Pediatr. 2014;165(4):842-8. 16. Wechsler JB, Schwartz S, Amsden K, Kagalwalla AF. Elimination diets in the management of eosinophilic esophagitis. J Asthma Allergy. 2014;7:85-94. 17. Dellon ES, Liacouras CA. Advances in Clinical Management of Eosinophilic Esophagitis. Gastroenterology. 2014;147(6):1238-1254.