Clinical Research Program 2014 Progress Report
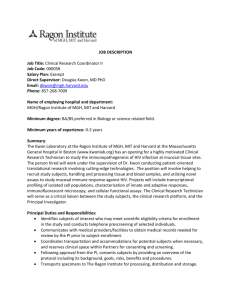
advertisement

Clinical Research Program Program Review 2014 Clinical Research @ MGH: CRP Program Review 2014 Table of Contents Executive Summary 1 Clinical Research Support Office (CRSO) 4 1. CRSO: PIs served per Year, 1997-2014 4 2. CRSO: PIs served by Faculty Rank 5 3. CRSO: Served by Department 5 4. Study Coordinators: Projects by Dept. & PIs per Yr., 2007-2014 6 5. CRSO: Consulting Hours by Service Type 7 6. RSVP for Health: Registrants’ Demographics 10 Clinical Research Education Unit (CREU) 1. Attendance, Web Views and Lectures, 2010-2014 2. Distribution of PI attendance per course category 3. Distribution of Study Staff attendance per course category 4. Clinical Research Education Unit Courses & Participation 12 12 13 14 17 Clinical Effectiveness Research and Survey Unit (CERSU) 1. Numbers of CRP CERSU Consults 2. Distribution of CRP CERSU Consults by Department 3. Distribution of CRP CERSU Consults by Academic Rank 4. Update on Clinical Innovation Awards (CIA) 19 20 20 21 21 Omics Unit 1. 2. 3. 25 27 28 29 Grand Rounds Omics Courses Course Attendee’s Research Role Information Technology Unit (ITU) 1. Activity on clinicaltrials.partners.org and crnet.mgh.harvard.edu, 1998-2014 2. Patient Recruitment Tool Metrics 32 34 35 Translational Research Center (TRC) 37 Electronic Health Records (EHR) Research Unit 40 Patient Centered Outcomes Research (PCOR) Unit 42 Biostatistics Unit 1. Percent of Projects by Faculty Ranks, Department, and Types 2. Percent of Submitted NIH Grants by PI Department 44 45 46 Appendix: CRP Website and Evaluation Tools 49 2014 Clinical Research Program (CRP) Executive Summary Maurizio Fava, M.D., Director of Clinical Research, MGH th Founded in 1996, the CRP is now entering its 19 year. The past year marked a leadership change in the CRP. Dr. William F. Crowley, Jr., who led the CRP since its inception stepped down and, after an extensive search with many highly qualified and talented candidates, Dr. Maurizio Fava was appointed to lead the CRP effective April 1, 2014. Over the past two decades, the CRP has become fundamental to leading MGH in thinking about not only clinical research and where we are heading, but also creating a robust infrastructure and extensive training to support and prepare our clinical research community for where we need to be in the future. Additionally, in the past year, three major initiatives came out of the MGH Strategic Plan and CRP is involved in all of them: 1. MGH Research Institute which seeks to promote, support, and guide the diverse MGH research enterprise by: • increasing its visibility • managing and growing its assets (people, funding, space, infrastructure) • preserving its leadership in innovation • fully integrating it with the clinical mission to better the human condition. 2. Translational Research Center (TRC which will close the research / clinical gap by establishing a specialized center focused on first-in-human studies 3. Biobank which will engage patients as partners in research and obtaining samples for research purposes Since its inception, the CRP has had a simple and constant Mission: to increase the quality, quantity, and efficiency of translating basic science advances into improved care for our patients. Following CRP’s Mission as well as MGH Strategic Plan recommendations, the following progress has been made since April 2014: Key Changes • • • • • • • • CRP is now the Division of Clinical Research of the MGH Research Institute Clinical Research Council expanded (held monthly and open to all) A new Committee on Clinical Research has been created, with representation from all departments, major divisions, and thematic centers A close partnership with Harvard Catalyst and MGH CRC has been established The new Translational Research Center (TRC): 18-bed unit on White 12 co-located with CRC - is being established CROI continues to be a key vehicle for community feedback Several thematic “Think Tanks” have been initiated (via meetings with representatives from Pfizer, Merck to discuss programmatic collaboration) EPIC for Research (revenue cycle) rollout at MGH has been facilitated CRP Program Review Executive Summary 1 • New CRP Units since April 1, 2014: Patient-Centered Outcomes Research (PCOR) Rationale: PCORI grant applications are rising at MGH, yet many PIs do not know how to design/implement PCOR studies. Services: consultation on study design, identification and incorporation of PROMs into clinical research setting and linkage with other clinical datasets, as well as stakeholder engagement. Faculty: Dr. Joshua Metlay Electronic Health Records (EHR) Research Rationale: Access to large population through EHR allows for critical investigations using Research Patient Data Registry (RPDR) and Informatics for Integrating Biology & the Bedside (i2b2); few investigators take advantage of such resource. Services: consultation on study design, generation of preliminary data, linkage with other clinical datasets and identification of potential collaborators. Faculty: Drs. Roy Perlis & Shawn Murphy (advisor) Imaging Biomarkers Rationale: Many investigators at MGH underutilize imaging resources and may not even be familiar with state-of-the-art technologies. Services: consultation on study design and imaging methodologies, feedback on draft research proposals, and identification of potential collaborators. Faculty: Drs. Brad Dickerson & Scott Gazelle Qualitative Research (coming in January 2015) Rationale: Grant mechanisms, such as PCORI and many NIH funding programs (K and R awards, CTSAs) increasingly require qualitative research components. Services: consultations and training Faculty: Dr. Elyse Park • Modified CRP Units: Education and IT Units are expanded to serve the MGH Research Institute Dr. Andrew Nierenberg is the Chair of the Education and Training Committee Dr. Henry Chueh is the co-Chair of the IT Committee OMICS Rationale: New technologies such as proteomics, metabolomics and transcriptomics are often underutilized at MGH Services: consulation on omics and genetic methodologies and study designs, human subject protection, and identification of particular resources. Faculty: Drs. Jordan Smoller & Rob Gerszten Biostatistics K-Awardees Rationale: K-award budgets do not provide for statistical support, though it’s critical for successful project execution. Services: ongoing grant/research paper preparation support and guidance throughout the duration of K-awards. Results Reporting to www.clinicaltrials.gov Rationale: In response to requests for support in submitting trial results to www.clinicaltrials.gov the Biostatistics Unit has developed a statistical computing support to allow investigators to retrieve the summary measures required by the website. Faculty: Drs. Dianne Finkelstein & Hang Lee CRP Program Review Executive Summary 2 New CRP Structure • • • Ten Units • Education • Biostatistics • IT • Comparative Effectiveness and Survey Research • OMICS • Clinical Research Support • PCOR • EHR • Imaging Biomarkers • Qualitative Research TRC CRC CRP Priorities for the Future • • • • • • • • • • • Create new Philanthropy Unit • Many PIs do not how to reach out to potential prospects Transform Simches 2 into a “hub for clinical research” • Create a CRC satellite • Move/consolidate bioinformatics • Establish IRB and Innovation office hours • Conduct a survey on the MGH PIs biostatistical needs Continue to expand CRP by working closely with leaders from key departments/centers as well as TRC, Catalyst/CRC, Biobank etc. Continue to transform expanded CRP into the Division of Clinical Research, once MGH Research Institute is fully established Continue to create new services for MGH clinical research community by working closely with internal and external partners Facilitate subject recruitment, capitalizing on eCARE Improve access to CTMS Enhance efficiency of central administration of clinical research Continue to improve interface with the central (Partners) clinical research administration Improve our image with industry and our overall “user friendliness” Create new Think Tanks CRP Program Review Executive Summary 3 Clinical Research Support Office (CRSO) Andrew A. Nierenberg, M.D., Director GOALS The role of the MGH Clinical Research Support Office (CRSO) is to provide infrastructure and logistical support for clinical research faculty, particularly for early career investigators seeking training and transitional support as well as for established investigators. Our goals are to: • • • Build the pipeline of early career physician-scientists; Support clinical research infrastructures; and Facilitate subject recruitment. ACCOMPLISHMENTS A. Utilization of CSRO Services A total of 135 investigators used services provided by the CRSO. Forty-seven (47) of these investigators utilized more than one CRSO service during 2014. These services included consulting with faculty on study implementation issues, accessing study coordinator support, utilizing project manager (PM) support to identify potential funding opportunities and assistance with assembling the administrative sections of grant applications, developing study budgets and training new staff to use the Budget Builder tool. PMs participate in the CRP’s Study Coordinator Orientation Program for MGH’s newly hired study staff; offer guidance and training on IRB submissions; and assist departments in training newly hired staff in tracking achievement of study milestones, invoicing sponsors and tracking payments, correcting errant patient care charges, and other practical interfaces with the Research Management and Financial Departments. Figure 1a: CRSO: PIs Served per Year, 1997-2014 174 163 153 145 136 146 135 121 121 118 99 91 70 68 27 10 12 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 Of the 135 investigators assisted by CRSO faculty, PMs and coordinators, 46.6% were junior faculty members (instructors and assistant professors), 28.2% were senior faculty (associate professors and professors), 7.3% were residents and fellows, and 17.8 were other non-faculty professional staff such as doctorally prepared nurses, and department administrators (Fig. 1b). CRP Program Review Clinical Research Support Office (CRSO) 4 Figure 1b: CRSO: PIs Served by Faculty Rank in 2014 Resident 0.7% Lecturor 0.7% Fellow 5.9% Professor 12.6% Associate… 15.6% Other 17.8% Instructor 20.7% Assistant… 25.9% N = 135 PIs The 135 investigators come from academic departments throughout the hospital and administrative areas. Collectively Medicine, Surgery, Pediatrics, and Psychiatry accounted for over 60% of all investigators served (Fig. 1c). Figure 1c: CRSO: PIs Served by Dept., 2014 Physical Med &… 1.5% Nursing 1.5% Dermatology 1.5% Urology 2.2% Neurosurgery 2.2% Orthopaedics 2.2% Otolaryngology 2.2% Anesthesia 2.2% Pathology Radiology 3.0% 3.7% Dept. < 1% 4.4% Neurology 4.4% Other Psychiatry Pediatrics < 1% = Administration, Ob/Gyn, Oral Surgery, Radiation Oncology, Stem Cell & Regenerative; & Hair Follicles & Systems Biology Departments 5.2% 8.1% 8.9% Surgery 16.3% Medicine 30.4% N = 135 PIs A1. Study Coordinator Pool Many clinical research investigators need staff to manage the day-to-day operations of conducting clinical research. The CRSO fills this gap by providing temporary, as-needed, trained study coordinators. In 2014, six fully funded CRP study coordinators supported a wide variety of clinical research projects directed by MGH clinical investigators. The CRSO study coordinator pool assists with all aspects of a clinical study for a flat hourly rate of $45 and represents the only charged service of the CRP. Study coordinators manage study start up (IRB submissions) day-to-day clinical study coordination including data collection and entry and study close out. In addition, study coordinators provide investigators and study staff with free advice and consultations on IRB submissions and reporting requirements. CRP study coordinators supported 59 individual clinical investigators from 18 departments on 94 individual studies (Fig. 2a & 2b). It is not unusual for clinical investigators to contract with the CRP for experienced CRP Program Review Clinical Research Support Office (CRSO) 5 study coordinators on multiple studies. In addition, a growing number of investigators and study staff seeking advice and consultations on IRB submissions, either prior to their submission to the IRB or in drafting responses to the IRB’s questions. Figure 2a: Study Coordinator Pool: Projects by Dept., 2014 Radiation Oncology 1.1% Other 1.1% Urology 1.1% Orthopaedics 1.1% OB/Gyn 1.1% Dermatology 1.1% Systems Biology 2.1% Stem Cell & Regenerative Biology; & Hair Follicles 2.1% Psychiatry 2.1% Physical Med & Rehabilitation 2.1% Neurosurgery 2.1% Radiology 3.2% Anesthesia 3.2% Pathology 4.3% Otolaryngology 5.3% Neurology 7.4% Surgery 7.4% Pediatrics 9.6% Medicine 42.6% N = 94 Figure 2b: Study Coordinators: Projects & PIs per Year, 2008 - 2014 Projects 130 124 PIs 99 93 92 86 92 94 90 72 72 59 57 49 45 07 08 09 10 46 11 12 13 14 CRSO study coordinators play an important role in training other study staff throughout the MGH. These experienced study coordinators have been accredited by the Norman Knight Nursing Center for Clinical and Professional Development to train MGH non-nurse study coordinators in basic phlebotomy, measuring vital signs, and performing ECGs thus leveraging the CRP’s programs into the clinical operations. One hundred forty-four (144) MGH study staff participated in these training programs in 2014. Since 2010, the CRSO, in collaboration with the CRP’s Education Unit, has trained approximately 1,200 research coordinators at MGH. This service fills a critical training need for our clinical research community. CRP Program Review Clinical Research Support Office (CRSO) 6 A2. Project Management (PM) Support To support the largely unmet needs of MGH clinical investigators for assistance in project and financial management, the CRSO developed a project manager (PM) service to address these issues. For investigators who contract with the CRP for study coordinator support, these PMs supported 59 MGH investigators conducting a total of 94 protocols with monthly reports detailing the precise status of their project’s subject recruitment and their fund balances. For investigators who are supported by the CRP’s study coordinator, the service is provided free of charge. In their work with investigators, PMs verified fund expenditures, identified and removed errant grant charges, provided a realistic assessment of projected fund balances, and reviewed sponsor amendments which may affect study budgets. The PMs invoiced sponsors based on achievement of study milestones, and managed final fund reconciliation allowing PIs to close study funds quickly and avoid deficits caused by untimely accounting practices. Perhaps more importantly, CRP PMs reduced the broader institutional problem of fund deficits resulting from poor tracking of crucial clinical research financial details. In addition to fund reconciliation, PMs also assist PIs by researching funding opportunities, budgeting clinical studies, participating in the CRP’s Educational Unit programs, and advising on study implementation. (Fig. 2c Project Management consulting support in 2014). Figure 2c: CRSO: Consulting Hours by Service Type in 2014 Identifying funding sources 1.2% Working with eCare / Epic team / Ed Unit 2.3% RedCap Survey building & management 2.3% Epic Super User support CRP QI/QA & SOP Development 3.8% 5.3% Budgeting clinical studies Project Management for specific Pis 6.8% 10.7% Study implementation & consults 17.1% Fund Management, Reconciliation &… 18.3% Responding to queries from staff & public 32.2% N = 8189 hrs A3. Expanded Project Management Support Support of Epic (Revenue Cycle) launch at MGH: In 2014, the CRP’s project managers worked closely with the Partners eCare (PeC) team to support the Epic Revenue Cycle launch in several important areas: • The PMs identified experienced research nurses and study staff to advise the PeC team on the clinical research work flow so that the Epic system process mapped accurately on the clinical research process of identifying research subjects, scheduling research visits and reviewing and allocating patient care charges to research funds or patient insurance; • Over 600 study staff were identified and enrolled in Epic’s research coordinator 100 training programs prior to the Epic launch in mid July; • The CRP worked with departments with a significant number of active clinical research studies to identify and train experienced study staff as Epic “Super Users”, and trained its project managers as Super Users who acted as a resource to study staff in departments throughout MGH before and after the Epic launch in mid July. CRP Project Managers worked with the PeC team to identify erroneous requisitions provided additional at-the-elbow personal training to study staff, tracked the types of errors made in the first three months of the Epic launch and reported findings to the PeC team and to MGH operations staff. Given the number of new study staff hires in 2014 and 2015’s projected number of new hired, the CRP anticipates providing continued project manager/Super User support to the MGH clinical research community. Support of Research Programs and Departmental initiatives: In 2014, the CRP’s PMs initiated support for principal investigators which were requested by their department’s research leadership. A CRP PMs managed study coordinator staffing and subject recruitment for a large PI-initiated cardiac study, which CRP Program Review Clinical Research Support Office (CRSO) 7 successfully recruited and completed data collection on 600+ subjects over 6 months. In addition, in response to a request from the Department of Surgery, a PM was assigned to act as a one-on-one faculty “navigator” for surgical faculty seeking funding opportunities and assisted with starting up new clinical studies, which includes IRB submission, subject recruitment, data collection and analysis. The goal of this effort is to track the time and effort associated with supporting surgery clinical investigators, so that the department can recruit permanent staff at the appropriate level of effort. The Department of Psychiatry has requested support to assist junior study staffs who are initiating protocols. This support consists of one-on-one education and guidance for study staff in study start up and subject recruitment, training staff in the use of Epic system billing review, and providing quality assurance for study data collection and entry. B. Clinical Research Faculty Mentoring with an Emphasis on NIH K Awards and the Patient Centered Outcomes Research Institute CRSO and CRP faculty members mentor clinical researchers at MGH, with a focus on early and midcareer development. CRSO mentors augment departmental mentors to provide additional perspectives and a broader overview of clinical research career development. The goal is to help junior and mid-rank faculty advance their careers and their clinical research. More than 135 faculty and research fellows reached out to the CRSO in 2014 (Fig. 1a). Dr. Nierenberg has staffed consultations ranging from junior faculty preparing new Career Development (K) grant applications to working with current K award recipients in applying for independent funding to consulting on resubmissions of federal grants and assisting with study design issues for new clinical studies and research networks. In collaboration with the CRP Education Unit, we designed and implemented “Conquering the K”, an interactive workshop designed to help junior faculty apply for K-awards. The workshop faculty included CRP faculty and senior K24 awardees. The full range of faculty provided a broad multifaceted overview from multiple clinical research areas. With the workshop, we expanded our services to 27 junior faculty and fellows and provided the K24 awardees with the opportunity to expand their mentoring portfolios. The seven session workshop included a mix of small group lectures and peer review of specific aims along with a mentor. Of note, the K workshop was part of the philosophy of the CRSO and Education Unit to shift from passive to active learning based on principles of adult learning. C. CRSO Career Development Tool Kit Over the past 15 years, the CRSO has developed a wide range of support services to meet clinical investigator needs for consultation on career development, as well as guidance on all phases of study implementation. We have also developed actively curated email lists of MGH junior clinical research faculty, applicants and recipients of K awards, research fellows, and graduates of the Harvard School of Public Health’s Clinical Effectiveness course. These lists allow us to keep investigators up-to-date about CRP education, funding opportunities, and educational programs of particular interest to junior investigators. The CRSO and the CRP Education Unit also developed a new educational series specific for MGH junior faculty focusing on NIH Career Development Award applications (K08 and K23 awards) and mid level faculty interested in K24 opportunities. D. CRP Online Service Support In 2009 and 2010, the CRP designed and launched an interactive intranet web resource (HUB) that allows MGH clinical investigators and their support staff to share their questions and study implementation problems with the wider clinical research community. HUB contains recordings and PowerPoint handouts of courses and training programs offered by the CRP’s Education Unit which allows faculty to re-review material at time most convenient to them and on an as needed basis. Through the HUB, investigators and staff can also access Key Clinical Research Resources provided by MGH, Harvard Medical School’s Catalyst, and Partners for inclusion in their grant application’s Resources and Environment sections. CRP Program Review Clinical Research Support Office (CRSO) 8 As mentioned in section A, the CRSO also offers interactive workshops specifically for Clinical Investigators applying for an NIH K Awards. These workshops focus on practical approaches including timelines and grant structure, with an emphasis on the unique requirements of these grants. We offered the K workshops in March 2014, with 27 junior faculty and fellow attendees. The workshops also give senior investigators who already have a K24 an opportunity to mentor the larger MGH community beyond their departments. The attendee evaluations for both reported uniform Excellent and Good ratings on the content of the material provided. To further assist faculty applying for these K awards, the CRSO is continuing to assemble a library of K08 and K23 applications recently awarded to MGH junior faculty which will be made available to new applicants. E. RSVP for Health Database to Facilitate Subject Recruitment The Research Study Volunteer Program (RSVP for Health) is a CRP-initiated study volunteer registry where pre-registered individuals receive information about clinical research studies that are active at the MGH. These include patients, families of patients, and normal volunteers. This program has been so successful over the years, that now both MGH and BWH research staff use this program as a resource to recruit study subjects. RSVP for Health saw its first full year of operation in 2005 and has had another year of steady growth in the number of registrants and in the number of MGH and BWH users. By the end of 2014, RSVP for Health contained over 24,400 registrants, up from 23,000 registered in 2013 (Fig. 3). Of the current 24,481 registrants we have accumulated in RSVP, 15,773 (64.4%) are women. Of the 24,481 total registrants 18,313 (74.8%) have indicated an interest in participating in studies as healthy volunteers or controls in addition to participating in therapeutic studies. RSVP serves as a critical resource for translational and physiologic studies. The registrants’ therapeutic interests reflect common disorders such as diabetes, obesity, mental health, cardiovascular disease, etc. In 2014, MGH investigators used the RSVP database to recruit subjects for over 60 individual MGH protocols. The heaviest users are investigators in the departments of Medicine, Psychiatry, and Radiology. CRP Program Review Clinical Research Support Office (CRSO) 9 Figure 3: RSVP for Health: Registrants' Demographics Category Registrants Count % Gender Female Male Not Recorded Total 15,773 7,604 1,104 24,481 64% 31% 5% 100% Race American Indian/Alaskan Native Asian Black or African American Native Hawaiian/Pacific Islander White Other Not Recorded Total Ethnicity Hispanic or Latino Not Hispanic or Latino Not Recorded Total 95 1,229 2,972 81 16,249 1,077 2,778 24,481 1,651 16,246 6,584 24,481 0.4% 5.0% 12.1% 0.3% 66.4% 4.4% 11.3% 100.0% 6.7% 66.4% 26.9% 100.0% Age <35 36-45 46-65 66+ Not recorded Total Contact Method Email Post Total: 11,156 3,742 6,772 2,457 354 24,481 19,887 4,594 24,481 45.6% 15.3% 27.7% 10.0% 1.4% 100.0% 81.2% 18.8% 100.0% LESSONS LEARNED The CRSO served a total of 135 individual investigators in 2014. During the year, we established several new services and also expanded our existing services. This support was distributed among different departments. Increasingly, we have focused CRP services on junior faculty in recognition of their importance in the clinical research “pipeline”. The creation of a Clinical Research “Help Desk” makes the process of referral to CRP, PHS and Catalyst resources straightforward, and use of this resource has grown considerably. The hands-on K award workshops continue to be popular. We had to limit registration because the intensive interactive format required small groups. While these workshops focused on the specific aims for the K awards and CRP Program Review Clinical Research Support Office (CRSO) 10 provided the participants to critique other’s materials, it has become clear that many want to have instruction and guidance beyond the specific aims to successfully submit a K award. Finally, it has become apparent that several departments have challenges with the IRB or with managing finances of clinical research. We need to identify these challenges earlier and explore preventative measures in coordination with MGH Research Management. ADAPTATIONS PLANNED 1. Expand specific email notices of CRSO services targeted to clinical researchers. Such ‘push technology’ should enhance serving the individual and varied needs of the MGH clinical research community. 2. Integrate CRSO assistance with departmental mentorship. 3. Communicate directly with mentors and department chiefs about how CRSO services can benefit their department. 4. Encourage Department Chiefs to consider having Associate Professors in their departments apply for K24 awards. 5. Expand the K Award workshop to include all aspects of grant submissions. To this end, we are piloting an expansive “Conquering the K” seminar in 2013. 6. Facilitate early career faculty to submit their first RO1. 7. Create a dashboard to obtain feedback from mentees and follow up on K award applications. Build a database of successful K awards to be used as models for applicants. Build the database of critiques to discover patterns of frequent errors. Analyze the efficacy of the program by obtaining data about the success rates of participants vs. non-participants as well as finding out the return on investment. CRP Program Review Clinical Research Support Office (CRSO) 11 Clinical Research Education Unit (CREU) Andrew A. Nierenberg, M.D., Director GOAL The goal of the Clinical Research Education Unit (CREU) is to improve the quality and quantity of clinical research within the MGH by providing educational opportunities for clinical investigators and study staff. The CREU strives to fulfill the diverse and dynamic educational requirements of clinical investigators locally through development of innovative course content. In addition, the CREU provides educational programs for research nurses, project managers, coordinators and assistants, which are foundational and responsive to the ever-changing clinical research landscape. Well-trained, educated study staff is essential for the success of a clinical investigator. ACCOMPLISHMENTS The CREU offered 252 lectures in 2014 (fig. 1) This number reflects both an increase in online training modules and a new focus on workshop- type courses that have fewer participants but allow for more interactive instruction. Figure 1: Lectures 252 244 238 222 211 2010 2011 2012 2013 2014 *number of lectures includes online training modules CREU courses were well attended in 2014 (5,201 attendees) (fig. 2). This is a testament to the ongoing need for local educational programs for MGH clinical investigators and study staff. It is also indicative of the CREU’s ability to adapt to changing needs, recruit appropriately talented course faculty, and identify current topics to be covered in course content. Figure 2: Attendance 6044 5762 5229 5201 5064 2010 2011 2012 2013 2014 Course attendance remained steady in 2014. The CREU offered fewer IRB and QI related courses in 2014, which are generally well attended. Due to high demand, the CREU focused more on courses CRP Program Review Clinical Research Education Unit (CREU) 12 related to study management than regulatory compliance. The number of views for online courses also remained steady in 2014 (fig. 3). Figure 3: Views of Online Trainings 28 60 2010 2011 663 644 643 2012 2013 2014 Investigator Program The investigator track continues to be extremely popular with 2,533 attendees in 2014. Figure 4 illustrates investigator attendance for specific categories of courses. Figure 4: Investigator Courses 2014: Attendance per course category Human Subject Protections Grand Rounds Genetics/Genomics Professional Development Study Design and Analysis 140 275 397 454 474 Clinical Research Day 793 The CREU continues to offer a core curriculum to support junior investigators in their research careers that consists of the following four courses: 1. 2. 3. 4. “Fellows Orientation Part I and Part II” “The Design and Conduct of Clinical Trials” “Basic Biostatistics for Clinical Research” “Good Clinical Practice in Academic Research Institution In addition to this core curriculum, the CREU offers more advanced courses to support clinical investigators in Genetics and Genomics (Genetic Code, Genetic Literacy, Responsible Conduct of ‘Omics” Research, Biobanking), Professional Development (Conquering the K: Applying for an NIH Career Development Award) and Biostatistics (Applied and Problem-Based Biostatistics). For the first time in 2014, the CREU offered an introductory series on developing a grant proposal for submission to the Patient-Centered Outcomes Research Institute (PCORI). This series consisted of three sessions: “Introduction to PCORI, Considering PCORI Funding? What do you need to know before applying and PCORI Panel Discussion?” Based on interest from participants, the CREU is developing a more specific program that focuses on writing and submitting proposals. The goals of this course are to educate investigators on this new funding mechanism and provide feedback on proposals by experienced faculty. CRP Program Review Clinical Research Education Unit (CREU) 13 In order to assess the needs of junior investigators and allocate resources appropriately the CREU developed a survey to distribute to fellows at MGH. The goal of the survey is to identify topics that are important to the community and determine which courses should be developed in a live or online format. Study Staff Program The study staff curriculum supports MGH clinical investigators by providing educational resources and training for study staff. This track is a widely used resource with 2,650 attendees in 2014. These educational and community-building opportunities provide study staff with updates on clinical research regulations and operations, all of which are critical for their role in supporting MGH clinical investigators. Figure 5 illustrates the distribution of study staff attendance for each of the course categories. Figure 5:Study Staff Courses 2014: Attendance per course category IRB and QI Education 297 Clinical Skills Training 304 Orientation Program 567 1422 Continuing Education The CREU continues to offer a core curriculum for study staff which consists of the following courses: 1. 2. 3. 4. 5. “Study Staff Basic Skills Program” (online) “Introduction to Good Clinical Practice and Study Management Basics” (online) “Orientation Program: Clinical Research Resources at MGH” “IRB/QI Roundtables” “Good Clinical Practice in Academic Research Institution” A major initiative in 2014 was continuing with the Clinical Research Spotlight Series and IRB Hot Topics Series in collaboration with the PHRC. IRB Hot Topics for 2014 included: “IRB Issues in Survey Research, Reporting of Research Results, Ethics in Clinical Research Protocols, Exemptions and Minimal Risk Determinations.” The Spotlight Series, which is held monthly, focuses on study management issues. Topics for 2014 included: 1. 2. 3. 4. 5. 6. 7. 8. 9. Unanticipated Problems Bio-specimen Processing Basics Training a New Clinical Research Coordinator Benefits of Professional Certification Consenting Research subjects in Acutely Ill Subject Populations Subject Remuneration and E-Check Maintaining Subject Privacy and Confidentiality Epic Discussion Group Delegation of Responsibilities in Clinical Research In 2014, the CREU collaborated with MGH Research Compliance to launch a new mandatory training program for newly hired clinical research coordinators. The CREU was responsible for developing the content of two of the required online trainings: CRP Program Review Clinical Research Education Unit (CREU) 14 1. “Study Staff Basic Skills Program.” This is a 20-module online training for newly hired study staff. The purpose of this online training is to provide new study staff with a solid foundation in clinical research as well as the same skill set when beginning their research career at MGH. 2. “Introduction to Good Clinical Practice and Study Management Basics.” This is a four module course that highlights the importance of adhering to GCP during the conduct of a study. It also outlines the responsibilities of each member of the study team. This past year, the CREU played a key role in educating study staff on Epic and how this new system would impact daily workflow. The CREU hosted several sessions with Partners eCare to prepare for the launch. In addition, the CREU offered multiple workshops to provided individualized training. Due to high demand, the CREU and CRSO began offering a quarterly Clinical Research Coordinator Discussion Group in 2014. These discussion groups allow peer-to-peer interaction and discussion. Participants are able to state questions and receive input from study staff throughout the hospital with various levels of experience. In 2014, the CREU worked with the CRP IT Unit to launch the Clinical Research Forum. The Clinical Research Forum is an online community dedicated to supporting study staff at MGH. Study staff can post questions or suggestions about the conduct of clinical research at MGH and obtain valuable feedback from colleagues and/or insight from various research-related departments at MGH. The Forum will be monitored by the CREU to ensure that all questions are answered in a timely manner and in compliance with hospital policies and research regulations. Three hundred and four (304) participants took advantage of the CREU’s Clinical Skills Trainings (phlebotomy, ECG and vital signs) in 2014. After reviewing course evaluations, the phlebotomy course was revised. The practical portion of the course is now hosted in a phlebotomy lab to allow for a real-life experience. The didactic portion of the course was revised to include new hospital polices on phlebotomy as well as a step-by-step guide to preparing for a blood draw. Online Course Development and Course Recordings In 2014, the CREU developed two online courses. Investing time and effort in online education allowed for continued, innovated course development. It also supports clinical investigators and study staff by making courses readily accessible. New online courses developed in 2014 include: 1. Reading a Clinical Research Protocol (to be added to the mandatory training program in 2015) 2. Writing a Clinical Research Protocol The CREU continues to record and post courses on our website while tracking access. The CREU now has an extensive archive of past programs and a growing catalogue of recorded courses. ADDITIONAL EFFORTS The Clinical Research Council is a meeting hosted monthly to discuss clinical-research topics with the research community. In 2014, the CREU assumed responsibility for administration of the meeting. During this period attendance has increased considerably and participants include both investigator and study staff allowing for discussion that impacts the research community as whole. One of the major initiatives for the CREU in 2014 was organizing the Research Education Committee. This Committee will advise the newly formed Research Institute on educational offerings throughout MGH. Dr. Nierenberg will chair the committee in an effort to consolidate resources, advertise all hospital educational offerings and identify areas where training is needed or needs to be improved. As part of this initiative the CREU will work with the CRP IT Unit to create a course compendium to catalogue courses and online trainings relevant to the research community. CRP Program Review Clinical Research Education Unit (CREU) 15 Clinical Research Day Clinical Research Day continues as an important venue to celebrate clinical research. Clinical Research Day showcases the CRP’s efforts to build and support a viable community of clinical investigators and study staff across the institution. It is recognized as a platform for clinical investigators to present and receive attention and reward from the institution’s leadership for their work, as well as a venue for interactions and collaborations amongst investigators. Participation in the 2014 Clinical Research Day remained high, with an unprecedented 386 abstracts submitted, 65 team nominations and a vibrant and well-attended poster presentation session. The tradition of Clinical Research Day is to highlight issues at the forefront of clinical research at the national level and to discuss these in terms of the MGH clinical research community. The 2014 theme was integrating patient-centered research and patient care. Katrina Armstrong, MD, MSCE, Physician-inChief, MGH, Jackson Professor of Clinical Medicine, HMS served as the keynote speaker. Following Dr. Armstrong’s keynote address, a panel discussion, moderated by Maurizio Fava, MD, focused on bridging the clinical research gap through patient engagement and translational initiatives. Leaders in patientcentered research provided their insight and suggestions on this topic to a diverse audience of clinical investigators. LESSONS LEARNED 1. Interest. Interest in CREU educational programming at the local level remains high. There is a continuing demand for basic level courses as well as more advanced content for clinical investigators and study staff. (See Appendix A for full 2014 course listing). 2. Curriculum. In 2014, the CREU performed a systematic evaluation of the current curriculum and identified important gaps. 3. Online Education. Online education is a highly valuable resource to the MGH clinical research community. By making courses accessible at all times, the CREU is able to increase its impact and provide even better services and resources to the clinical research community. Placing more foundational and unchanging courses online will allow the CREU to better utilize the highly valuable time of its course faculty, focus its live courses on more current topic areas, and provide more interactive and in-depth in-person education. ADAPTATIONS PLANNED 1. The CREU will continue to invest in online education by enhancing and promoting its online education resources and creating additional online educational opportunities. 2. The CREU is transitioning to a more interactive-type series design. For 2015, the CREU is developing two new series: a. “Patient-Centered Outcomes Research”. This is a multi-session course designed to help investigators submit for an award from the Patient Centered Research Institute (PCORI). b. In the past the CREU and CEU have offered a basic survey design course for investigators and study staff. Due to high demand, the CREU and CEU are developing a more intense, multi-session course focusing not only on instrument design, but also on conducting survey research. 3. The CREU is working with several departments at MGH and Partners to develop a standardized training manual for newly hired clinical research coordinators. The goal of this project is to CRP Program Review Clinical Research Education Unit (CREU) 16 provide and document training for all clinical research coordinators at MGH. The manual will be made available to the research community through the CRP website. The CREU will be responsible for maintaining the information in the manual. 4. The CREU will work with the newly formed Qualitative Research Unit to develop a course on qualitative research. To date, education and training on designing and analyzing qualitative studies at MGH is nonexistent. 5. The CREU will adapt to ongoing changes in the research environment by continuing to develop, innovate, and create dynamic learning opportunities for study staff. Figure 5: CRP Education Unit - Courses and Participation 2014 Investigator Program Attended* Study Design and Analysis Introduction to Survey Research & Design 55 Basic Biostatistics for Clinical Research 180 Applied Biostatistics for Clinical Trials 90 Problem-Based Biostatistics 117 Design & Conduct of Clinical Trials 32 Genetics/Genomics Genetic Code 82 Genetic Literacy 87 Epigenetics 77 Biobank 70 Sequencing 81 Faculty Lectures Hours Views** 4 1 1 1 18 4 5 4 4 15 6 7.5 6 6 22.5 92 344 117 120 87 2 3 3 4 3 1 1 1 1 1 4 4 4 4 4 57 33 353 61 43 3 1 1 38 38 21 1 1 1 1 1 1 1 1.5 1.5 1 1 65 30 24 7 14 169 45 14 1 4 69 116 90 50 23 31 1 25 1 1 1 6 2 4 1 1 1 1 2 16 1 2 2 1.5 Issues in the Protection of Human Subjects Maintaining Research Subject Privacy and Information Security: What Clinical Researchers Must Know Ethics of Clinical Research Protocols Reporting of Results What Consitutes a Minimal Risk Study? Town Meeting for Relying on Commercial IRB Professional Development Conquering the K Clinical Research Fellows Orientation Part II: Starting Your Clinical Research Career at MGH How to Make a Poster Good Clinical Practice How to Give a Presentation What is PCORI? Considering PCORI Funding? PCORI Panel Grand Rounds Neurology: Toward Novel Therapeutics for Neuropsychiatry: Targeting Neuroplasticity Medicine: Atrial Fibrillation: Can Genetics Inform Patient Care? Medicine: Human genetics, type 2 diabetes and target validation for drug discovery Clinical Research Day Keynote Address Panel Discussion Abstract Submission Total, Investigator Program CRP Program Review 9 154 23 20 65 1 1 1 120 1 1 1 90 1 1 1 250 180 363 2 7 1 1 1 1 13 5 2,533 131 65 121.5 1,722 Clinical Research Education Unit (CREU) 17 Figure 5: CRP Education Unit - Courses and Participation 2014, cont. Study Staff Program Orientation Orientation Program: Clinical Research Resources at MGH Research Nurse Offerings RN Roundtable IRB/QI Roundtables Session I: Part I: IRB: New Submissions Initial Full Board Review Session I: Part II: QI: Study Start-Up Session II: Part I: IRB: Continuing Review & Amendments Session II: Part II: QI: Source Documentation Session III: Part I: IRB: Amendments & Reporting to the IRB Session III: Part II: QI: Protocol Adherence & Reporting Requirements Session IV: Part I: IRB: Consent Form Writing Session IV: Part II: QI: Informed Consent Process Clinical Skills Trainings ECG Training Phlebotomy Vital Signs Training Continuing Education ACRP The Next Step in your Clinical Research Career Auditing Bio-Specimen Processing Basics Budgeting for Industry Sponsored Clinical Trials CRC Discussion Group CRC Discussion Group on Epic Clinical Trials.gov Delegation of Responsibilities in a Clinical Research Study eIRB Training: Hands-on Introduction to eIRB Epic Research Functionality Overview Epic Lunch and Learn Epic Workshops: Registering Research Patients Hands-On MORA Training: Managing Monitor Online Record Access Managing and Reporting Unanticipated Problems Meet the Protocol Administrators and Managers of the Partners Human Research Office Pitching and Consenting Research Opportunities in Acutely Ill Subject Populations RedCap: Getting Started RedCap: Data Entry and Survey Admin RedCap: Making Changes to Projects Research Subject Advocacy Materials and Recourses for Research Nurses and Research Coordinators Research Subject Remuneration and Reimbursement: Policy Review and Navigating the Process SoCRA: The Benefits of Joining a Professional Clinical Research Org. Subject Recruitment and Retention Series Study Electronic Data Capture: StudyTRAX & REDCap Training a New CRC Online Trainings Research Patient Data Registry (RPDR) Good Clinical Practice and Study Management Basics Submitting your Medical Record/Health Info. Research Protocol to the IRB IATA Shipping Training for Transportation of Biological Materials and Dry Ice Infection Control Principles and Practice in Clinical Research Introduction to Clinical Research at MGH (online) Basics of Manuscript Writing for Clinical Researchers Subject Recruitment & Retention What Makes a Good Article? How to Review Scientific Literature to Guide Your Research Total, Study Staff Program Grand Total CRP Program Review Attended* Faculty Lectures Hours Views 140 10 4 5 72 14 1 3 3 8 31 29 21 22 22 34 27 37 1 1 2 1 2 1 2 1 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 64 144 96 2 3 1 10 20 15 20 40 30 20 41 30 27 32 29 180 30 3 1 1 3 5 2 1 1 1 1 1 1 2 1 2 1 1.5 1.5 1 1.5 2 1.5 4 1 51 240 42 66 11 47 1 2 1 1 1 2 8 2 3 20 3 1 16 1.5 1 33 18 1 1 2 30 56 38 29 1 1 1 1 1 1 1 1 1 1 1 1 8 4 3 2 20 4 1 1.5 67 2 1 1 17 11 58 86 65 1 5 2 3 1 3 3 1 1 4.5 3 1 49 26 71 170.5 292 519 2,241 10 63 11 346 53 74 35 16 22 2650 5,183 14 8 11 18 17 5 32 13 123 16 6 1 9 4 5 5 4 10 4 8 88 219 9 187 252 Clinical Research Education Unit (CREU) 18 Clinical Effectiveness Research and Survey Unit (CERSU) James B. Meigs M.D., M.P.H. and Eric G. Campbell Ph.D, Co-Directors GOALS The Clinical Research Program’s Clinical Effectiveness Research and Survey Unit (CERSU) has three main objectives: • Support clinical research aimed to improve the clinical practice of medicine and population health, • Provide mentorship and advice at MGH for academic research careers in clinical epidemiology and effectiveness, • Help investigators to design/conduct research survey. The CERSU focuses specifically on the “Second Translational Block” that exists between clinical trial and other research results and the implementation of their advances to improve clinical practice and public health. The principal activity of the CERSU has been research mentoring for MGH trainees and faculty at all levels. Most mentoring is for MGH’s junior faculty investigators. We provide advice and support for research that addresses a spectrum of approaches and topics from disease pathogenesis to the effectiveness, efficiency, and equity of health care delivery and delivery systems. Careers in this area are fundable and can lead to stable research and administrative careers, especially in the era of the Affordable Care Act and its Patient Centered Research arm, PCORI. We aim to support and attract the best and brightest MGH clinical investigators into these fields, as well as to help with their career development and retention. In response to increasing health care costs, the need for payment reform, and the continuing gap between evidence and practice, the Federal Government has substantially increased available funding to support comparative effectiveness research (CER). Defined as the conduct of research comparing the benefits and harms of different health care interventions and strategies, CER seeks to assess a wide range of health outcomes for diverse patients, patient populations and patient subgroups. This research requires the development, expansion, and use of data sources and methods to determine comparative effectiveness and disseminate the results. ACCOMPLISHMENTS Support for Clinical Effectiveness Research and Surveys The CERSU provides MGH’s clinical investigative community with the only MGH program for individual mentorship in the domains of epidemiology, study design, questionnaire and survey methods, and use of large clinical databases. The CERSU also provides data management and analytic support for investigators, operational planning for the use of clinical care data for clinical research, assistance with grant and Internal Review Board (IRB) preparation, and as a resource for locating potential funding. Mentorship and Consultation The research that the CERSU supports seeks to increase translation of evidence from clinical studies into clinical practice at the patient, provider and system levels. During 2013-2014, the CERSU provided mentoring services, consultation on career mentoring, hypothesis generation, study design and survey development, and data analysis/data management to the MGH community. The CERSU provided 44 consultations in 2014and the wide breadth of additional CERSU administrative services, available hospital-wide, included advice on IRB submissions, data assembly and management, IT implementation and application, data acquisition and analysis methods, are shown below. In 2013-2014, the CERSU CRP Program Review Clinical Effectiveness Research and Survey Unit (CERSU) 19 served 14 Departments and 5 Academic Ranks as shown in the Figures below. Of the 44 consultations, 82% were to early career investigators. Database Consulting and RPDR support Wei He, M.P.H. and Sue Regan, Ph.D. provide database consulting and RPDR support services, including: obtaining and providing cleaned RPDR, TSI, IDX and other electronic data searches in Access file format, review of protocol and data collection forms and review of existing or planned data entry systems. In addition, the service offers training in skills for day-to-day management of ongoing projects in Access databases such as report and query design, integrating external sources of data (e.g. from laboratories, other sites), and data export for analysis. Survey Consultation Service Eric Campbell, Ph.D., Professor of Medicine and member of MGH’s Institute for Health Policy and HMS, provides survey consultations and advice for all aspects of study design, execution and interpretation of survey data. During 2013-2014 survey consult topics ranged from surveys about local quality improvement and patient quality of life to national information and attitude gathering surveys to health professionals. Numbers of CRP CERSU Consults, 2014 5 Database Query & Manage 19 Mentor and Design 20 Survey Design N =,44 Clinical Effectivness and Survey (CERSU): Consultations by Dept. 2014 Urology 2.3% Physical Med. & Rehab. 2.3% Oral Surgery 2.3% Nursing 2.3% Dermatology 2.3% Surgery 4.5% Other 4.5% Orthopaedics 4.5% Psychiatry 6.8% Emergency 6.8% Anesthesia 6.8% Pediatrics Radiology Medicine CRP Program Review 9.1% 15.9% 29.5% Clinical Effectiveness Research and Survey Unit (CERSU) 20 Clinical Effectivness Research and Survey Unit (CERSU): Consults by Rank 2014 Other 9.1% Associate Professor 9.1% 18.2% Assistant Professor Instructor 27.3% Fellow 36.4% Clinical Innovation Awards (CIA): Translating Clinical Insights into Improved Care The Clinical Innovation Award (CIA) program was initiated in 2005 in collaboration with the CEO, Peter Slavin, M.D. Solicitation and evaluation of research proposals to integrate clinical insights into improved patient care were conducted using and NIH type review and award model. In 2011, CIA operations were transferred to MGH’s Department of Quality and Safety. MGH physicians, nurses, and allied health professionals participating in Care Redesign or Patient Affordability were eligible to apply for these awards. The award supports a portion of the PI’s salary to allow protected time to devote to the project (up to 20%); research infrastructure support necessary to carry out the project (e.g. biostatistics, project management, informatics development, study coordinators for data collection, and research assistant/study coordinator support); and faculty co-mentorship (with the Quality and Safety Office) from the MGH Clinical Research Program to help execute the projects. The four awards made in the 2012-2013 cycle are shown below. 2013 CLINICAL INNOVATION AWARD RECIPIENTS PROJECT LEADERS IMPACT (Improving Care After Chemotherapy): Through the project, advanced care nurses will call patients with nonsmall lung cancer or colorectal cancer who are receiving chemotherapy to discuss side effects and how to manage their symptoms. The goal of IMPACT is to improve patient outcomes and reduce utilization, which will improve the quality of care provided and reduce costs. Theresa McDonnell, ACNP and Jennifer Temel, MD Enhancing Shared Decision Making for Patients with Acute Low Back Pain: The project will test whether or not using a patient education tool and clinical decision support at the time of diagnosis for acute low back pain improves patients’ experience, outcomes, and efficiency. Remote Glucose Monitoring for More Efficient Insulin Titration in the Patient Centered Medical Home (PCMH): This project will assess the benefits of integrating remote glucose monitoring, through the Diabetes Connect platform, into the MGH Diabetes Care Redesign insulin initiation/titration process. The goal is to increase the volume of patient encounters with the Diabetes Champion without increasing the overall time spent on insulin management. CRP Program Review ALIGNMENT Lung and Colon Cancer Care Redesign Teams Leigh Simmons, MD and Karen Sepucha, Ph.D. Back Pain Care Redesign Team Nancy Wei, MD Diabetes Care Redesign Team Clinical Effectiveness Research and Survey Unit (CERSU) 21 PROJECT LEADERS Improving the Health of Patients with COPD in the integrated Care Management Program (iCMP): This project will focus interventions on COPD patients in the Integrated Care Management Program (iCMP), including patient education, care plans, and exercise through a remote tablet monitoring system. COPD Care Redesign Team: Paul Currier, MD; Fiona Gibbons, MD; Michael Sullivan, DPT; Christine Kaliris; Joan Strauss; Sanjay Chaudhary; Ryan Thompson, MD; Joanne Kaufman; Mary Neagle Applying Systems Engineering and Improvement Science to the MGH Emergency Department (ED): This project will use current systems engineering science to improve frequently utilized processes to reduce ED length of stay and patient care cost, and thus improve the value of care provided, focusing on the processes for urinalysis and plain film radiography. Benjamin White, MD ALIGNMENT COPD Care Redesign Team Patient Affordability The status of 5 awards is as follows: Title: Enhanced shared decision making for patients with acute low back pain PIs: Leigh Simmons, M.D. and Karen Sepucha, Ph.D. Project aims: improve patient’s decision making and confidence in their ability to self-mange their back pain; reduce inappropriate imaging studies and specialty referrals without negatively impacting on health outcomes. Progress to date: A core study team was identified to implement the study in the Medical Walk-In Unit and in Internal Medicine Associated Urgent Care clinic. Patients previously seen for back pain in the clinics were identified and several have completed a telephone needs assessment which allowed the study team to finalize the survey instruments. Progress Report: the intervention period provided standard care to subjects with a decision aid and worksheet. The results of the data analysis to date show that most patients wanted reassurance and diagnosis; about 20% expected a referral and imaging; there were some gaps in knowledge and self efficacy, and the point of care intervention has been well received by the subjects. Title: Applying systems engineering and improvement science in the MGH Emergency Department PI: Benjamin White, M.D. Project aims: to use current systems engineering science to improve frequently utilized processes in order to reduce ED LOS and patient care costs; improve the value of care provided. Progress to date: Over the 1 year of funding, the Principal Investigator carried out a number of interventions, and realized sustainable improvements in process flow metrics. Specifically, the PI piloted interventions, including a more rapid laboratory urinalysis collection and analysis process, and a technologist-based radiology transport pilot process. In a continuation of the pilot studies, and as a result of further rapid-cycle change regarding the laboratory urinalysis process, the study team implemented a new process intervention that minimized waste even further. Through rapid cycle studies, we developed a second intervention which informed much larger process mapping and systems improvement related to ED structural change planned and the IT (EDIS) updates. In Q3, the study team continued the interventions, and began the data analysis regarding its measurement, and potential further areas of improvement. Preliminary results showed, with a decrease in urine collection time for some patients, overall decrease in urinalysis cycle times, and laboratory cycle times for other laboratory testing as well. In Q4, the PI determined that both interventions would move from “pilot” phase to permanent process changes, and began generating manuscripts and presentations based on data and experience, and related grant applications. CRP Program Review Clinical Effectiveness Research and Survey Unit (CERSU) 22 Title: IMPACT: Improving Care after Chemotherapy PI: Theresa McDonnell, RN, NP and Jennifer Temel, M.D. Project Aims: to examine changes in patient-reported symptoms during the first two cycles of neoadjuvant or adjuvant chemotherapy for NSCLC and CRC among patients who receive standard care plus a practice nursing intervention relative to patients who receive standard care alone. Progress to date: The PIs held two focus groups with the MGH Cancer Center NP staff to obtain their perceptions of our current model of post-chemotherapy care and the proposed intervention. The feedback from the focus groups has been analyzed and incorporated into the project intervention design. Subjects were recruited in accordance with the protocol plan and data collected and analyzed. Research results were presented in October 2014: McCarty, C, Traeger, L, Temel, J, Greer, J, McDonnell, T. (2014, October). Prevalence and correlates of patient symptom burden at the initiation of chemotherapy. Poster presented at the inaugural Palliative Care in Oncology Symposium, Boston, MA. Title: Randomized Controlled Trial of a Multifaceted Tablet Based Intervention for Preventing Readmissions for Patients with COPD PI: Paul Currier, M.D., Fiona Gibbons, M.D., Michael Sullivan, PHS Information Systems Project Aims: reduce COPD related readmissions in the iCMP cohort compared to a control group at 90 days; improve level of activity in the group receiving intensive physical therapy as measured on the 6 minute walk test at 90 days. Progress to date: the research project consists of a RCT of the MGH integrated Care Management Program (iCMP) management of COPD patients admitted to hospital. Groups randomized to intervention would receive the tablet; the control group will receive an evaluation of their physical capacity at the beginning and end of the study. The Tablet will facilitate tracking patient metrics such as symptoms, oximetry, medicine compliance, and physical activity. The study team has defined the details of the study process flow for obtaining informed consent; evaluating educational triggers to be loaded onto the tablet; electronic alerts to the study coordinator when a patient in the iCMP/COPD cohort utilizes the ED and/or is admitted to the hospital; defining the home-based exercise program, and Identifying post study survey tools. The IT component and equipment for collecting data was finalized in fall 2014. The project will be implemented in 2015. Title: Remote glucose monitoring to improve insulin titration in the patient-centered medical home PI: Nancy Wei, M.D. Project Aims: Assess the benefit of integrating remote glucose monitoring into the Diabetes Care Redesign insulin initiation/titration process on improving clinical efficiency (frequency and quality of diabetes-related encounters), provider and patient satisfaction, and glycemic control (HbA1c change). Progress to date: PI established four participating practices (Beacon Hill Primary Care, MGH Back Bay, Bulfinch Medical Group and Mass General Medical Group).In collaboration with the Center for Connected Health, the PI has determined the appropriate remote monitoring tools. Diabetes Champions within these practices identified eligible patients via TopCare 2.0. The challenges to this study are continuous updates to the Technology; the diabetes teams within the practices experience turnover, and incomplete documentation of encounters by diabetes providers. The next steps in completing this project include the Center for Connected Health working on integrating a newer and less expensive device, and assistance of the Clinical Research program’s study coordinators in administering the baseline survey by phone to participants. LESSONS LEARNED The CERSU is a successful and well-established part of the MGH research and operations mission. Every year the CERSU is struck by a continuing demand for advice and mentorship form the MGH clinical research community. We provide on average one consult per week year-around. However in the 20132014 period CERSU consult numbers have fallen a few short of the count in 2012-2013. Also, we often hear from potential investigators that they have been unaware of the CRP’s diverse offerings. This says to us that we need to keep working on maintaining and increasing our visibility and exposure to make sure that we are reaching potential investigators who might benefit from our advice. There appears to be CRP Program Review Clinical Effectiveness Research and Survey Unit (CERSU) 23 a strong, rising interest in comparative effectiveness, clinical outcomes, clinical epidemiology, care redesign, patient affordability and accelerating improvements in efficiency research. We have shown repeatedly over the years that we can help young clinicians make careers in these areas. Also, with the CERSU, the MGH CRP remains visionary in clinical research support, as nothing comparable is available elsewhere in Partners or the Harvard Catalyst systems. ADAPTATIONS PLANNED CERSU adaptations to its support services considered for 2014-2015 will focus on increasing our exposure to the MGH community in an attempt to reach the broadest possible constituency. CER Consults: The CERSU is always seeking to find new ways to identify talented future MGH research faculty by increasing interactions with trainees (residents and fellows) through consulting with faculty in positions to mentor these individuals. To this end we will present the CERSU to all new, incoming Fellows in July, participate in MGH house staff research activities, present the CERSU intermittently at the monthly Clinical Research Council meeting, among other opportunities for public exposure. We remain available year around to provide consultation advice, and can usually meet with new consults within a week of the initial request. We will continue to offer one-on-one consultation and mentoring, for both simple advice as well as long-term support for a specific project or paper. We will continue to provide RPDR search and data management support services for those projects that need these services. CERSU Clinical Effectiveness Research Course: Workshop on Study Design: Using MGH Clinical Care Data for Clinical Effectiveness Research Since 2010, the CERSU has offered a Clinical Effectiveness Research course in collaboration with the CRP Education Unit. The course was not held in 2013-2014, but we will offer a redesigned curriculum in 2014-2015. This 5-session workshop will takes about 20 investigators step-by-step through the process of defining a CER hypothesis, obtaining expedited IRB approval for a data query, and designing and executing an RPDR data query. Additional didactic sessions will provide real-world examples from past and ongoing investigators who have successfully used the RPDR and other electronic data systems to address clinical epidemiology and effectiveness hypotheses. CRP Program Review Clinical Effectiveness Research and Survey Unit (CERSU) 24 Omics Unit (formerly Genetics and Genomics Unit (GGU)) Jordan Smoller, M.D., Sc.D. and Robert Gerszten, M.D., Co-Directors GOALS The missions of the Clinical Research Program’s Omics Unit are threefold: • Provide consultative support to clinical investigators initiating or planning genetic and genomic studies at Massachusetts General Hospital (MGH); • Educate and support clinical investigators already performing such studies through educational programs and process improvements; and • Serve as a link between the MGH clinical research community and the educational and technological platforms in Omics research of the Partners HealthCare System and the greater Harvard Medical community. As genomic medicine becomes a reality, the Omics Unit continues to make significant progress in arming MGH clinical research teams with the knowledge and tools needed to incorporate or expand genomic and other omics in their clinical research studies. The Omics Unit is well positioned to help MGH investigators capitalize on the Partners Biobank opportunities. TRANSITIONS With the growth of genomics, transcriptomics, proteomics and metabolomics, the Genetics and Genomics Unit has expanded and been renamed to encompass all fields of Omics research. In the past year, our unit has undergone a number of transitions. Dr. Susan Slaugenhaupt, Co-Director of the Unit, was appointed as the first Scientific Director of the MGH Research Institute. Due to her new responsibilities, Dr. Slaugenhaupt has left the Unit and we were delighted to have Dr. Gerszten join as Co-Director with Dr. Smoller. Dr. Gerszten’s research efforts focus on the intersection of cardiac and metabolic diseases. His laboratory has incorporated emerging proteomics and metabolomics technologies to help identify novel disease biomarkers and pathways. He is the Director of Clinical and Translational Research, Institute for Heart, Vascular and Stroke Care at MGH. ACCOMPLISHMENTS Omics research has arrived at a singular moment in which the technology, expertise, and resources for transformative discovery and clinical translation are now feasible. The Omics Unit is fortunate to be situated within a network of world-class scientific and medical research communities that are driving innovation and translational investigation. To enhance the scientific opportunities and resources available to MGH investigators, the Omics Unit has developed collaborative relationships with other key genetics and genomics centers and investigators. Through this network, the Omics Unit has been able to connect MGH investigators with core facilities, and provide consultation and educational opportunities across the larger Partners, Harvard, and MIT communities. Partners HealthCare Biobank. The Partners Biobank is a large-scale research project designed to facilitate medical discovery and improvements in clinical care by creating a repository of biological samples linked to electronic health records and other health information. More than 20,000 patients have enrolled thus far, and the Biobank is a key component of the MGH Strategic Plan. Dr. Smoller is coDirector of the Biobank at MGH and the Omics Unit is working with the MGH clinical research community CRP Program Review Omics Unit 25 to leverage this unique resource. In 2014, we launched a new educational course, in collaboration with the Harvard Catalyst, titled A Practical Guide to Biobanking for Biomarker and Personalized Medicine Research. The course provided an introduction to the use of biorepositories for clinical research, a practical guide to banking and the resources of the Partners Biobank, accessing, and using samples and phenotypic data, and an overview of relevant human subjects issues. Through our alliance with the Partners Biobank, we hope to continue the expansion of the phenotypic and biological sample resource and increase investigator participation at MGH. The MGH Center for Human Genetic Research (CHGR) is a trans-disciplinary research center devoted to human genetics and encompassing scientists and laboratories from numerous departments at MGH (including neurology, psychiatry, medicine, surgery, and pediatrics). As senior faculty members at CHGR, Dr. Smoller (Director of CHGR’s Psychiatric and Neurodevelopmental Genetics Unit) has been able to enlist other CHGR faculty to participate in the Omics Unit’s research consultation and educational programs. The core facilities of CHGR are also available to MGH investigators seeking genotyping and other services. CHGR’s clinical and phenotyping research space on Simches 2 provides clinical resources (exam rooms, interview/observation rooms, phlebotomy stations, and a specimen preparation laboratory) for phenotypic characterization of research participants. The Analytic and Translational Genetics Unit (ATGU) is an investigative group within the Department of Medicine. Its overall mission is to focus on the interpretation of individual genome sequence data for both the discovery of the genetic underpinnings of human disease and for the development of paradigms by which individuals’ genome sequence can be effectively integrated into clinical decision making. Drs. Benjamin Neale and Daniel MacArthur have presented at courses offered by the Omics Unit. The Partners HealthCare Personalized Medicine (PHPM) is devoted to promoting genetics and genomics in research and clinical medicine and to realizing the promise of personalized medicine by accelerating the integration of genetic knowledge into clinical care. PHPM offers CLIA-certified genetic testing for a variety of medical applications, core facilities for genotyping, sequencing and gene expression analysis, and IT solutions for the integration of genetics and clinical care. The Partners Biobank is also housed within the PHPM, and Dr. Smoller regularly attends the PHPM management meetings and plays a critical role in linking MGH to this resource. The Broad Institute of MIT and Harvard is a leading research institute in the areas of genomics, molecular medicine, and the development of novel therapeutic approaches. As Associate Members of the Broad, Drs. Smoller and Gerszten are able to facilitate access to Broad resources and core facilities for MGH researchers involved in omics research. Dr. Gerszten serves on the steering committee for the Proteomic and Metabolomic Platforms. Members of the Broad community have also played an active role in the educational offerings of the Omics Unit. For example, Senior Associate members Joel Hirschhorn and Bradley Bernstein have lectured in Genetic Literacy and Introduction to Epigenetics, respectively. The Harvard Catalyst is a pan-Harvard enterprise devoted to facilitating clinical and translational research. Dr. Smoller is leading the Genetics and Bioinformatics education program, with the goal of expanding the genetics curriculum and the associated faculty involved in peer teaching efforts. As more investigators are incorporating genetics and genomics into their research, there has been a greater need for statistical genetics services at MGH that are not the domain of traditional biostatisticians. After a needs assessment, the Omics Unit has addressed this demand by forging close links to the biostatistical and bioinformatics communities at MGH and other Harvard institutions. As a result, consultations in these areas are now available free of charge to all MGH clinical investigators. The Omics Unit has thus effectively bridged the gap between these Harvard-wide resources and has significantly enhanced the interactions and research programs of MGH investigators. The Omics Unit has grown in scope and expertise while broadening the level of service provided to MGH and it plays a critical role in forging cross-disciplinary and cross-institutional connections while maintaining a focus on MGH. CRP Program Review Omics Unit 26 Departmental Grand Rounds Program in Genetics and Genomics The highly successful MGH Seminars in Genetics and Genomics Clinical Grand Rounds Program is developed annually in collaboration with the CRP’s Education Unit. The goal of these seminars is to make maximal utilization of the individual clinical departmental Grand Rounds program settings to highlight opportunities and advances in genetic research to the clinical community. In this way, both clinicians and clinical investigators can hear of the opportunities made available to them by the latest genetic advances in the context of the individual clinical care issues of their specialty. Such ‘context setting’ in clinical arenas will ultimately be crucial to the broader adaption of genetics to personalize medicine in several specialties. Each lecture is thus dedicated to a Genetics & Genomics topic based in clinical medicine and centered on a disease state and clinical case presentation. Through this series, genetic education is embedded within each department and reaches a unique population of clinicians and clinical investigators. The 2014 Omics Unit Grand Rounds Series is illustrated in Fig. 1. Figure 1: 2014 Grand Rounds Medical Grand Rounds March 20 “Atrial Fibrillation: Can Genetics Inform Patient Care” Patrick Thomas Ellinor, MD, PhD April 24 “Human Genetics, Type 2 Diabetes and Target Validation for Drug Discovery” David Altshuler, MD, PhD October 9 (Clinical Research Day) “Integrating Patient-Centered Research and Patient Care” Katrina Armstrong, M.D., MSCE, Physician-in-Chief, Jackson Professor of Clinical Medicine, MGH Neurology Grand Rounds March 13 “Toward Novel Therapeutics for Neuropsychiatry: Targeting Neuroplasticity” Stephen J. Haggarty, PhD, Associate Professor of Neurology, Harvard Medical School Educational Curriculum In collaboration with the CRP’s Education Unit, the Omics Unit updated its 2014 curriculum primarily in response to feedback from past course participants. This curriculum is primarily aimed at clinical investigators with some specific courses for clinical research coordinators, nurses, and study staff. Course evaluations were extremely positive for each course, rating consistently “very good” to “excellent”. In 2014, the Omics Unit developed a core genetics curriculum to meet the needs of a variety of learning levels in which the Omics Unit draws heavily on faculty in the MGH Center for Human Genetic Research and the Analytic and Translational Genetics Unit as instructors. This core curriculum is the cornerstone of our program and was taught in 2014 by recurring courses such as Genetic Code, Genetic Literacy and Sequencing. In 2014, we launched a new course, titled Introduction to Proteomics and Metabolomics, directed by Dr. Gerszten. We will continue to focus on the needs of MGH clinical investigators as we create the 2015 curriculum in conjunction with the Harvard Catalyst education group, led by Dr. Smoller to expand the MGH’s broad educational courses in genetics and genomics. CRP Program Review Omics Unit 27 Fig. 2 lists the 2014 Omics Unit courses and faculty. Figure 2: 2014 Omics Unit Courses • “Welcome to the Genetic Code: An Overview of Basic Genetics” This introductory course reviewed fundamental language and concepts including DNA anatomy and genome organization; genotype-phenotype correlations; basic population genetics; and genotyping. Attendees – 85 Faculty included: Susan Slaugenhaupt, Ph.D., Jordan Smoller, M.D., Sc.D. • “Genetic Literacy: An Guide to Understanding the Language and Concepts of Modern Genetic Research” This course was designed to briefly describe the terminology, technologies, and methodologies of modern genetics. Intended for clinicians, investigators, nurses and other clinical research staff with an interest in genetics and genomics. Attendees – 87 Faculty included: Joel Hirschhorn, M.D., Ph.D., Joshua Levin, Ph.D., Michael Talkowski, Ph.D. • “Epigenetics: An Introduction and Applications” This course provided attendees with introductory lectures defining epigenetics and its effect on gene regulation and inherited disease. Attendees – 77 Faculty included: Robert Kingston, Ph.D., Johnathan Whetstine, Ph.D., Bradley Bernstein, M.D., Ph.D. • “Next Gen Sequencing: An Introduction and Clinical Applications” The course included an introductory lecture on next-generation sequencing technology and sample preparation, lectures on how to interpret the data and how the analysis is applied in Genomics. The goal was to provide attendees with fundamental knowledge of sequencing methodologies and how to apply them in studying genetic variation and human diseases. Attendees – 81 Faculty included: Niall Lennon, Ph.D., Benjamin Neale, Ph.D., Daniel MacArthur, Ph.D. • “A Practical Guide to Biobanking for Biomarker and Personalized Medicine Research” This course provided an introduction to the use of biorepositories for clinical research, a practical guide to banking, accessing, and using samples and phenotypic data, and had an overview of relevant human subjects issues. The course was geared towards investigators and staff at all levels interested in the utility of biorepositories for their research. Attendees- 70 Faculty included: Jordan Smoller, M.D., Sc.D., Scott T. Weiss, M.D., M.S., Elizabeth Karlson, M.D., P. Pearl O’Rourke, M.D., Lynn Bry, M.D., Ph.D. • “Introduction to Proteomics and Metabolomics” This introductory course is intended for clinicians, investigators, graduate and medical students, and clinical research staff with an interest in functional genomics and precision medicine. It will introduce fundamental language and concepts including basic concepts behind analytical tools, sample preparation, quantitative considerations, protein-protein interaction networks, post-translational modifications, data analysis, biomarker discovery and validation, translational introduction of diagnostic and prognostic biomarkers into the clinic, approaches to understand basic disease mechanisms and to identify potential novel drug targets, as well as applications for personalized medicine. Attendees – As of this report there are 160 registered participants. Faculty includes: Robert Gerszten, M.D., Steve Carr, Ph.D., Namrata Udeshi, Ph.D., Matthew Vander Heiden, M.D., Ph.D. CRP Program Review Omics Unit 28 As shown in Figures 3, the Omics Unit educational curriculum served a broad range of junior and senior faculty as well as trainees. Figure 3: Course Attendee's Research Role Study Staff 41% Investigators 59% n = 350 Investigators (Professor, Assistant Professor, Associate Professor, Instructor, Clinical /Research Fellow, Resident) and Study Staff (Research staff, Student) Consultations to Investigators One of the Omics Unit’s goals is to provide consultation and triage for the MGH clinical research community. A consult request is completed online by individual investigators at all academic levels requesting help in genetic study design and execution, human subject protection, career advice, and/or identification of particular resources. Requests are triaged by the Omics Unit and assigned to specific consultants depending on expertise and availability. In 2014, MGH investigators from numerous departments (including Cardiology, Psychiatry, Neuroendocrinology, Neurology, and Radiology) received consultations through the Unit. Access to the Omics Unit Resources The Omics Unit webpage within the CRP website has been updated with available resources. The website offers the research community a wealth of educational information and links to resources both within the MGH and beyond. LESSONS LEARNED 1. Need for expansion of services to cover the broad range of omics research. Our Unit was established at a time when genetic and genomic research was emerging frontier for clinical research. The focus was on expanding the involvement and knowledge base of clinical investigators in these areas, which were underutilized. Over the past several years, genomics has become a widely adopted component of clinical and translational investigation at MGH (in part, we believe, through the services and educational offerings of the Omics Unit). At the same time, advances in functional genomic and related components of systems biology have created new opportunities for translational investigation using transcriptomics, proteomics, metabolomics, metagenomics, and metatranscriptomics. To better serve the clinical/translational community, we have expanded our Unit to encompass the full range of Omics research. 2. Need for expanded availability of services for bioinformatics, computational biology, and statistical genetics. As a growing number of investigators engage in clinical research involving Omics, there is an increasing need for sophisticated bioinformatics and computational support. Although the MGH community includes leading experts in these areas, their ability to collaborate and consult is, of course, not infinite. Many clinical and translational investigators are accumulating datasets that may harbor discoveries, and there is a risk that computational and bioinformatics resources will become a rate-limiting step in mining these data and may slow progress in translational research. Expansion of resources in this area (including bioinformatics or analytics core services) may be needed to address these needs. CRP Program Review Omics Unit 29 3. Need for basic genetics education and expansion of online resources. Every year our introductory course offerings, Genetic Code and Genetic Literacy, draw large crowds and the course evaluations highly praise the basic level of the material taught. It has become increasingly clear that the MGH’s need for basic genetics instruction is growing as research in all disciplines is increasingly incorporating genomics. We also provide the opportunity for students enrolled in Genetic Code to pre-submit specific questions that they would like answered. In 2014, we had over 150 questions, and we tried to touch on most of the topics during our lectures and/or during the question and answer period. This service has proved extremely popular as it provides an accessible and widely used forum for individuals to ask any question in an ‘anonymous’ fashion which is important since many clinical investigators are often not sufficiently confident to ask questions related to these new technologies. Lastly, we recognize the increasing need for additional online courses and resources. In 2014, our course A Practical Guide to Biobanking was recorded and will be made available to our online audience and the Partners Biobank. 4. Need for diverse and specialized course offerings in the expanding domain of omics research. The field of omics research is evolving rapidly, and every year brings new technology and innovations that soon become essential components of clinical research in this area. Thus, we note the continued need for the development of new courses and resource fairs focusing on the latest technology. For example, courses such as A Practical Guide to Biobanking and Introduction to Proteomics and Metabolomics have been added to keep investigators abreast of the latest tools and techniques of the field. ADAPTATION PLANNED 1. With the addition of Dr. Gerszten, we will expand our Unit to provide a broad range of Omics related research to include biomarkers, metabolites, and more. 2. The Omics Unit will continue to work closely with its network of collaborating investigators and centers (CHGR, PHPM, Broad Institute, ATGU, and the Harvard Catalyst) to address the evergrowing needs of the clinical research community at MGH and beyond. These collaborations have led to increased access to resources for MGH investigators, an increased pool of expertise, and expanded opportunities for collaborations. We will continue to serve all academic levels, from clinical fellows to senior investigators, and focus on making connections that will benefit MGH scientists. 3. We will continue to expand our curriculum in collaboration with the Harvard Catalyst to meet the demand for specialized courses. Upcoming offerings include: • Nanocourses. We will continue to offer half-day nanocourses that provide more advanced education on special topics in the genomics field (including proteomics, pharmacogenomics, use of bioinformatics tools, sequencing, and epigenetics). Topics for these courses are solicited from the community and are often based on evaluations from the core modules. The nanocourse curriculum is updated annually to incorporate emerging methods, tools and technologies. Sample courses include: “Epigenetics”, “Pharmacogenetics”, “Proteomics”, “Metabolomics”, “RNA-Seq”, and “Next-Generation Sequencing”. • Introduction to “Omics” Research (in development). This 5-day course will draw on expert faculty across the disciplines relevant to omics research and will provide an intensive introduction to the methods, tools, and technologies. Each day will comprise a morning session of lectures followed by an afternoon session of hands-on training in the use of analytic/bioinformatics methods and tools covered during the morning session. • “Bedside to Bench to Bedside” (in development) This new course, offered annually, will target clinicians and clinical investigators who seek to expand their involvement in research by identifying opportunities for translating clinical observations to scientific discovery. Topics covered will include: identifying clinical opportunities for discovery (e.g. unusual patients/pedigrees) ; CRP Program Review Omics Unit 30 accessing cores, tools, and technologies for data analysis, clinical interpretation of DNA sequence data; design of biomarkers and novel therapeutics. 4. The Omics Unit will continue to work with the Partners Biobank to fully integrate the operations of the biobanking efforts into the clinical mission at MGH in 2015. Further, discussions are already ongoing to perform pilot metabolite and proteomic profiling studies to validate whether the archived samples will be useful for biomarker studies to complement genetic analyses. All protocols and data would be provided to the broader scientific community as a resource for grant applications. 5. In 2015, we will continue to make all course materials available online to increase availability and access to the MGH clinical research community. 6. Educational opportunities will be expanded in 2015 in an effort to keep pace with the rapidly evolving technologies in this area. We are already planning a new flagship course, Introduction to Omics Research. This annual 5- day course will provide an intensive introduction to the landscape of methods, tools, and technologies involved in omics and systems biology research. 7. Responsible Conduct of Omics Research which will provide a practical introduction to human subjects issues in genetic research and biobanking, data sharing and data use agreements, conflict of interest, and other issues relevant to omics research. CRP Program Review Omics Unit 31 Information Technology Unit (ITU) Henry C. Chueh, M.D., M.S., Director GOALS The broad goal of the Clinical Research Program’s Information Technology Unit (ITU) has been to support the increasing information technology needs of the MGH’s clinical investigative community. Its specific approaches to meeting this goal have been: • Improving existing information management resources while creating a broad, new information management infrastructure to support the work of the clinical research community at MGH and PHS; • Providing IT management support for MGH clinical investigators, including assisting in the recruitment of study subjects and supporting the Clinical Research Program’s educational initiatives; • Establishing ongoing partnerships with clinical researchers to pilot applications and studies with new clinical informatics-based interventions that will create reusable technology platforms; • Envisioning and creating transformative informatics and IT solutions for the clinical research community and beyond; and Going forward these goals remain important, but will be addressed in a more generalized manner given the overall needs of the MGH Research Institute. ACCOMPLISHMENTS During the life of the program to date, the Information Technology Unit has added institutional value by supporting clinical investigators with a variety of informatics and IT solutions, both within the CRP, across MGH, and beyond. In addition, the CRP ITU has been responsible for some major innovations including the Partners RPDR and the informatics design of the i2b2 program, among others. Listed briefly below are some highlights: • Research Patient Data Registry (RPDR) – The CRP ITU envisioned and designed the initial version of the RPDR, a terabytes-scale clinical research database that has become a major research IT platform at Partners that has supported upwards of $100 Million dollars of grant funding. • i2b2 – As an extension of CRP ITU activities in clinical research data modeling, Dr. Henry Chueh was the Principal Investigator, architect, and author of the informatics core of the original i2b2 grant. Under the strong direction of Dr. Shawn Murphy and others, i2b2 has grown to be a national model for clinical research data management and analysis. • Data for Quality (D4Q) – The CRP ITU, in collaboration with the CERSU, envisioned models for data management that would support effective outcomes research analysis. Implemented and managed by the Center for Quality and Safety, the D4Q effort represents the integrative approach supported early on by the CRP. The D4Q data warehouse is used across MGH for clinical outcomes research and operations improvement. • Clinical trials visibility – Before clinicaltrials.gov, the CRP ITU established a clinical trials listing website used across the MGH and BWH, providing visibility for study recruitment. • Monitor Online Record Access (MORA) – MORA fills a clinical research community need to allow monitors to effectively audit clinical records for research purposes. The CRP ITU put MORA into CRP Program Review Information Technology Unit (ITU) 32 production in 2012 and it has already saved an enormous amount of study staff time that is better utilized in direct research activities. • Population Registries – The CRP ITU established and supported activities (in collaboration with general medicine, primary care, rheumatology, infectious disease and others) that have led to population registries for clinical care that also serve as platforms to test clinical interventions. The Partners Population Health Management program currently relies on the TopCare IT platform that is derived from this groundbreaking CRP activity. • RSVP for Health (RSVP) – Envisioned as a way to engage patients more directly in clinical research, RSVP was one of the first websites in the nation to allow patients to subscribe to clinical research areas of interest, and to also allow clinical investigators to connect to those patients anonymously for outreach. • Clinical Research Hub – As an evolution of the CRP ITU’s intramural support of the CRP Education Unit, the Hub is a knowledge management and learning platform that is designed for the future. When merged with investigator profiles, it can provide tracking, recommendation, and discovery of clinical research education. More recently, our work in 2014 has focused on platform development and adaptation to enable meeting investigator needs in the changing information systems environment, while continuing to meet service needs of investigators. Platform development has focused on these areas: • eCare Engagement Problem: During and after the transition to Epic-based systems clinical investigator access to clinical data must be insured Solution: During the past year, ITU staff participated in the Epic Revenue Cycle implementation at MGH. In this process, staff obtained invaluable experience in establishing HL-7 interfaces from Epic, as well as useful experience with eCare business processes and administrative structure. In addition, staff has begun to make use of the EDW, an essential resource that will become increasingly valuable as the Epic clinical implementations begin in 2015. • Scalable knowledge and learning management tools for research Problem: the growing breadth and depth of course offerings in the Clinical Research Program Education Unit and the ongoing institutional changes related to the formation of the MGH Research Institute make expansion of the scope of the educational system put into place for the Clinical Research Program necessary to meet more general MGH research needs. Solution: Making the Clinical Research Hub more accessible to the broader research community by implementing technical interfaces to other systems and reorganizing both resources and infrastructure in 2015 to meet the broader charge. • Centralized Researcher profiles Problem: Our support of an educational and knowledge management platform has revealed both the value of having meaningful, up-to-date data profile that pulls from diverse sources, and the difficulty of capturing detailed profile information and keeping it up-to-date across sources. Solution: We continued to work on leveraging and building on research profiles software we are adapting from our partners at the UCLA Computing Technologies Research Lab and promoting a pathway through Partners. We have involved key stakeholders to identify a comprehensive sources for MGH research community members’ profiles. This initiative serves two important institutional purposes: information security auditing and coordination of user identities for systems that depend on them (e.g. various research applications the research enterprise builds going forward). CRP Program Review Information Technology Unit (ITU) 33 • Establish a research registries service Problem: To design and implement a research registry service to support the needs of mid-level research programs that need greater flexibility and integration than can be supported by a free product like REDCap Solution: We have created a health EDC that makes collected data actionable triggering any number of potential actions. In the Sprout model, the data collection serves to knit together the patient’s personal, clinical and research experiences. The application is currently used by the MGH Lurie Center for Autism and the MGH Down Syndrome Program to support the electronic collection of patient-reported measures with a customized clinician narrative output. In addition, the Department of Urology will be using the application to support data capture for their Renal Cell Carcinoma registry by January 2015. MORA – Monitor Online Record Access MORA, the Monitor Online Record Access tool, is a tool for efficiently providing controlled, limited electronic access to clinical records for clinical study/trial monitors and auditors, replacing the typical manual and inefficient paper-based process. Since being released in 2012, MORA has been used at MGH on 217 protocols in more than 16,000 sessions (Figure 2), with an 85% increase in 2014. At MGH and Partners in general the preponderance of this activity has been for cancer trials: across Partners 89% of the protocols and 96% of the monitor sessions. Research Patient Data Registry (RPDR) The RPDR project, an innovation that was imagined and developed by the CRP’s IT unit, is a successful and widely accessible research database that was expanded through a collaboration between the CRP, Laboratory of Computer Science (LCS), and Partners’ Research Computing Group. The RPDR has ~4,500 users throughout the Partners Healthcare System. It holds data on over 7 million patients and 2.1 billion coded records from patient encounters, labs and results, and other medical care. The registry now contains patient demographic data, diagnoses and procedure data, pharmacy data, inpatient and outpatient encounter information, provider information, and laboratory data. Data from electronic health records, LMR and OnCall, are also included. Clinical Trials Recruitment Sites We have supported clinical trial listing sites for MGH and Partners since 1998 and the RSVP for Health research volunteer registry since 2003. The clinical trial listing site clinicaltrials.partners.org continues to get strong usage as indicated in Fig. 1. We believe automated clinical trials outreach we implemented using social media (Twitter feed @phstrials) has contributed to the 2014 increases outlined in Fig. 1 and 2. Figure 1: Activity (adjusted) on CRP website clinicaltrials.partners.org & crnet.mgh.harvard.edu 5,770 Public Adjusted 4,331 Inside PHS 3,557 average # of users per month* 2,972 2,084 291 98 1,171 690 71 231 00 1,616 1,504 238 02 244 04 163 06 2,023 2,286 407 08 10 12 14 * During 1999-2012 four different technologies for measuring user activity have been used. Figures have been adjusted to current equivalents using scale factors derived during periods when the methods of measurement overlapped. CRP Program Review Information Technology Unit (ITU) 34 Growth of the RSVP for Health research volunteer registry has persisted at approximately the level of the last several years, while usage has leveled off (Figure 2). Figure 2: CRP Information Technology Unit – Metrics • Clinical trials at Partners site sessions/month Sessions/month (16% increase from 2013 total) 8,056 • RSVP for Health New registrations in 2014 (2% decrease from 2013) 2,053 Cumulative registrants (4% increase from 2013) 24,470 Registrants sent one or more mailings (19% increase from 2013) 23,285 • MORA Cumulative MGH protocols with at least one monitor session with MORA (85% increase from 2013) Cumulative number of times monitors reviewed MGH patient records for MGH protocols (up 323% from 2013) 217 16,474 LESSONS LEARNED AND ADAPTATIONS PLANNED During this time of significant organizational transformation we continue to look for ways to support and interface at an enterprise level from an organizational and technological perspective. Based on previous major transitions we realize the importance of focusing on new opportunities that present themselves during this large-scale transformation of the institutional infrastructure and will be taking advantage of our experience as we to meet the needs of the greater research community that will come with the formation of the MGH Research Institute. EPIC/eCare – Continuing to acquire eCaredata interface expertise through supporting of transition to eCare of Population Health and Clinical Systems. As the clinical data infrastructure for the institution moves to Epic, ITU staff are learning the Epic data service calls needed to migrate existing systems. This will enable ITU staff to maintain their core expertise at accessing clinical and administrative data in all available modes. LCS work during the transition will guarantee that ITU staff will be able to make clinical data from eCare available to researchers in any form in which they may want to put it to use. Research Training and Compliance Tracking/Reporting Positive changes in the E-Learning technical landscape and our experience supporting the diverse clinical research training offerings of the Clinical Research Program’s Education Unit over the years have made it clear that a shift in focus is needed. We need to develop a more unified and flexible compliance tracking and reporting mechanism that can both support improvements in course content generation tools, pull from diverse educational systems/sources and meet the broader research education needs in the context of the MGH Research Institute. We want to support learning across websites, apps, in-person events, etc. and make them interoperable on a data level keeping each other up-to-date in a learning eco-system that goes beyond individual systems. We also plan to better support research compliance specific tracking and reporting that can be used by different groups (both administrative and technical) to track and report on required training, certification and re-certification. Shared Informatics Platform Currently, different informatics groups, labs and individual researchers run their own infrastructure and write their own software, which often results in duplication of effort and wasted resources across the research enterprise. Our goal is to create a shared computing platform that allows easy sharing of both applications across systems and machines and full research computing environments used to run analyses improving the ability to reproduce research results. Specifically, we are looking at rolling out standardized “computing containers”, which are doing to the computing world what standardized shipping CRP Program Review Information Technology Unit (ITU) 35 containers did to the logistics and transportation world. In summary we want to create an open and shared informatics platform for quickly building, sharing, and running research applications with all the necessary dependencies. MGH Research Profiles with the Partners Identity Management Project In 2015 we will adapt the work we have done on a centralized profile database of physicians, researchers, and staff to meet the needs of MGH research and integrate with the Partners Identity Management Project if feasible. Profile data are housed across diverse sources and each application built by MGH departments must request a feed from these sources, process the feed, and import into their own database. A centralized profile database with a granular “needs based” access layer would streamline the current process significantly and allow all groups to write integration code against a single source. SproutStudy – Electronic Data Capture Service for Research Registries We are prepared to add value to current (and future) Clinical Trials Management Systems and serve the MGH research community with Sprout. To complement institutional support for investigator data management provided via REDCap and commercial EDC products, we will extend our existing platform as detailed above to facilitate data collection from mobile devices, develop self-serve tools so that researchers make create their own forms and templates, and focus on the addition of features to comply with 21 CFR part 11 over the next year. CRP Program Review Information Technology Unit (ITU) 36 Translational Research Center (TRC) Mason W. Freeman, M.D., Director – formerly Translational Medicine Unit (TMU) GOALS The TRC’s overall goal is to facilitate the form of clinical research that moves basic scientific discoveries and new technologies toward the clinic to improve diagnostic capabilities and therapeutic interventions. Specifically, the TRC works with investigators to: Advance projects from pre-clinical findings that suggest clinical benefit through the required stages of development necessary to test the concepts in human trials. This work involves: • • • • • Clarifying the development pathway necessary for a given idea to be taken forward; Providing an assessment of the feasibility and cost of pre-clinical studies, including pharmacology, manufacturing, and toxicology; Preparing the electronic submission and obtaining an Investigation of a New Drug (IND) license from the FDA; Conducting meetings with relevant regulators at the FDA; and Assisting in the writing of clinical protocols for submission to the Partners IRB. These activities are typically time-intensive projects and require significant commitments on the part of the TRC staff to become familiar with the details of individual investigator’s projects in order to facilitate meaningful interactions with the FDA, external contract research organizations, or third part vendors whose expertise is needed to enable a translational project to advance. ACCOMPLISHMENTS • The TRC’s focus on advocating for more streamlined administrative processes that help clinical investigators expand their collaborations with outside groups and enhance grant revenue for the hospital achieved a notable milestone in 2014. Partners IRB policy was amended to allow the outsourcing of selected, multi-center clinical protocol reviews to independent, external IRB’s. The TRC has been a strong proponent of this approach and its advocacy work, in conjunction with the activities of the committee empowered to evaluate this change, the Partners Human Research/IRB office, as well as the staff and consultants brought into the evaluation process by the Partners Chief Academic Officer (Dr. Klibanski) has led to a significant change in IRB review policy that will benefit a wide array of MGH clinical investigators. • The Strategic Planning Process, initiated in April of 2012, was completed in 2014. The MGH hospital leadership and the MGH Scientific Advisory Committee strongly endorsed the recommendation to create the Translational Research Center (TRC). The TRC has been funded and recruitment of key staff is currently in progress. The TRC, which replaces the Translational Medicine Unit as the translational research-focused component of the new Clinical Research Division is directed by Dr. Freeman. The TRC will include an expanded in-patient clinical trial facility that will be combined with the existing Clinical Research Center to form a conjoined 18-bed inpatient unit on White 12. The space requirements for these combined programs have been delineated and architects have been engaged to draw up detailed renovation plans for White 12. Dr. Freeman and Michael Fisher of the Research Space Management office co-authored a grant application to the Massachusetts Life Sciences Center requesting $5 million to help defray the costs of the capital renovation of White 12 for the new unit. That application successfully passed the first stage of review by the MLSC review board in October and a more detailed MGH application was solicited by that review panel in November. Final word on whether the MGH will receive state funding for the new trial facility would be expected by the beginning of 2015. CRP Program Review Translational Research Center (TRC) 37 • A multi-year, multi-million dollar grant detailing the creation of a joint MIT-MGH innovation center for the development of novel medical devices and drugs was submitted to the NIH in June 2014 with Dr. Freeman and Drs. Arup Chakraborty and Elazer Edelman of MIT serving as the co-PIs of the grant. The grant, termed a REACH award, is currently under review by the NIH. This grant is very similar to the NHLBI-funded National Center for Accelerated Innovation award that was made to a Harvard-led Boston consortium last year, which is based at Partners and the Brigham and Women’s Hospital. Dr. Freeman continues to serve as a member of the 5-person oversight committee of that program (termed the Boston Biomedical Innovation Center or B-BIC) which awards pilot ($50,000) and drive ($250,000) grants to investigators in the B-BIC network. The first pilot and drive grant recipients will be announced before the end of 2014. • The TRC team, spearheaded by its Program Manager Dr. Yuan-Di Halvorsen, has continued to provide consultative services to a wide variety of MGH investigators whose research programs have needed input on clinical development, regulatory, or CMC issues of a wide variety. A sampling of some of that work is provided below: a. Dr. Steven Hersch of Neurology has pioneered the development of a ganglioside treatment for Huntington ’s disease. He is seeking additional NIH funding for his program and requested help from the TRC to prepare for a pre-IND meeting with the FDA, whose approval of Dr. Hersch’s therapeutic development plan will be required to ensure continued NIH support for his therapeutic studies. The TRC has worked extensively with Dr. Hersch to help plan his pre-clinical toxicology studies as well as several other components of the development plan that will be needed for the FDA interaction. The pre-IND meeting is expected to take place in February 2015. b. The TRC has continued to support the cholera vaccine program of Dr. Ed Ryan of the Infectious Disease Unit. It is serving as the CRO for the project, including supervision of the manufacturing development process. The NIH’s Division of Microbiology and Infectious Disease is supporting this work. c. Dr. John Stone of Rheumatology has defined a new disease that is termed IgG4-RD and shown that rituximab may be of considerable benefit to patients with that disorder. The TRC/Translational Medicine Group team helped Dr. Stone develop a clinical development program, budgetary plan, and coordinating center protocol for a multi-center, multi-national trial to treat this disorder using the Roche/Genentech antibody. A grant application to run this trial, with the TRC serving as the coordinating center, was submitted to the company and received strong endorsement. A final funding decision is pending commercial and budget priority determinations at Genentech. d. Dr. Ron Tompkins of Surgery has engaged the TRC on two projects, one devoted to support for an RO1 grant aimed at therapies for trauma patients and a second focused on a peptide with potential value in those suffering from extensive burns. e. Dr. Anders Naar of the Cancer Center has developed a locked nucleic acid inhibitor of a microRNA that controls key metabolic pathways in lipid and carbohydrate metabolism. The TRC team has worked closely with Dr. Naar and the Partners Innovation office to help devise an IND enabling pre-clinical program and to help identify a corporate sponsor for this work. LESSONS LEARNED • When the TMU was founded, the MGH was in danger of falling behind other academic health centers in its investment in the infrastructure required to support translational research. In the past few years, considerable progress has been made in closing this gap. With the creation of the TRC, the pending construction of a new in-patient clinical trial unit, and the development of a broader business development function for translational activity, the MGH is clearly emerging as a leader in the CRP Program Review Translational Research Center (TRC) 38 translational research field. There remain, however, key components of the clinical research enterprise that are not yet aligned with the requirements of a successful translational enterprise. One of these areas that will require considerable attention in 2015 is the timely execution of clinical research contracts. • Feedback from Boston’s local biopharmaceutical community makes clear that the MGH’s proximity to these organizations is a major competitive advantage for us. These relationships must be developed over time, building confidence between the MGH and its local partners in the commitment of each to the shared mission of bringing better treatments to those in need. Proximity is, however, not enough. A substantial effort must be made to create and solidify these relationships and this effort will depend not only on TRC personnel but also on the commitment of many of the hospitals most talented investigators. • The success of the new clinical trial facility, currently in the design phase of construction, will be highly dependent on the participation of key faculty in proposing and conducting new patient-based trials. Processes need to be put in place that streamline the effort the faculty must make to enable this participation and an appropriate incentive structure must be devised that will engage their energies. ADAPTATION PLANNED • With the approval and funding of the MGH Strategic Plan and the re-organization of the Clinical Research Program into a Division of Clinical Research, the leadership is now in place to create an administrative structure that can build an outstanding translational research enterprise at the hospital. It is anticipated that much of this work will be initiated and significantly advanced in 2015. • With the creation of the MGH Research Institute and the filling of the key leadership positions in Research administration, the MGH should now be able to develop a sophisticated, integrated, and comprehensive program of translational research that opens up new opportunities for advancing patient care and for identifying novel sources of support for the clinical research mission of the hospital. CRP Program Review Translational Research Center (TRC) 39 Electronic Health Records (EHR) Research Unit Roy H. Perlis, M.D., M.Sc., Director GOALS The EHR Research Unit’s overall goal is facilitating investigations drawing on large clinical databases, most notably large-scale electronic health records (EHR). These studies run the gamut from pharmacovigilance and epidemiologic studies to small proof-of-concept or targeted biobanking efforts. Specific services offered by the EHR Research Unit include: a) Consultation with investigators to plan and refine investigations making use of large clinical datasets; b) Assistance in preparation of materials describing investigations of large clinical data sets for submission to IRB or other regulatory review; c) Assistance in generating descriptions of methods for incorporation in funding applications; d) Assistance in generating pilot data to motivate funding applications, and for incorporation in publications; e) Development of tools to allow researchers to address questions which would otherwise be difficult to study in large data sets; f) Assistance in accessing appropriate large data sets and integration of multiple data sets – for example, use of birth and death certificate data; g) Assistance in development of decision support tools which make use of results derived from large clinical data sets. These services require substantial investment of time by the director and staff to understand the specific project requirements and ensure that they are specified correctly prior to investing programmer and analyst resources in generating and analyzing data sets. ACCOMPLISHMENTS • The EHR Research Unit was constituted in the fall of 2014. Since then, it has completed approximately 1 consultation per week. The majority of these relate to grant submissions (K23/K99 or equivalent; R01 or equivalent). • The EHR Research Unit is developing a course for investigators interested in making use of EHR or other large data sets. • At the Partners Personalized Medicine meeting, EHR Research Unit leadership participated in a panel discussion to emphasize the role of EHR-linked biobanks in genetic discovery and translational research. LESSONS LEARNED • Based on initial consultations, it became apparent that a bottleneck in the use of Partners EHR resources is programmer time needed to move from a raw data set to a format amenable to analysis by investigators themselves. CRP leadership has agreed to provide support for this time to enable development of pilot data sets. • More generally, many investigators who are interested in using large clinical data sets are unfamiliar with the types of data available and the limitations and opportunities in using these data. Greater efforts at disseminating this knowledge – through formal courses but also by preparing introductory materials and examples – will be required. CRP Program Review Electronic Health Records (EHR) Research Unit 40 ADAPTATION PLANNED • To increase shared resources available for data generation and analysis, we will work with investigators to include some support for EHR Research Unit’s services in federal, foundation, and industry grants as appropriate. • Now that the Unit has been launched, we are increasing efforts to integrate with other CRP and nonCRP programs – for example, in translational research and statistics – to allow CRP to provide endto-end support for researchers. • In particular, Dr. Shawn Murphy, PHS Director of Research Information Systems, has agreed to serve as a senior advisor to EHR Research Unit, which will ensure bidirectional flow of ideas between CRP and Partners Research IT. CRP Program Review Electronic Health Records (EHR) Research Unit 41 Patient Centered Outcomes Research (PCOR) Unit Joshua P. Metlay, M.D., Ph.D. Director GOALS The PCOR Unit’s overall goal is to facilitate that form of clinical research that addresses the comparative effectiveness of different healthcare options from the perspective of patient outcomes. To a large extent, the PCOR Unit was established to address the research needs and funding opportunities provided by the creation of the Patient Centered Outcomes Research Institute (PCORI), which had a research budget of $650 million in 2014. Research supported by PCORI has three major components: 1) It tests the comparative effectiveness of a range of healthcare interventions, including treatments, diagnostic tests, and system-level strategies; 2) It focuses on outcomes that are experienced and reported by patients; and 3) Research progresses in a model with substantial stakeholder engagement including input from patients, caregivers and providers. The PCOR Unit seeks to facilitate research by providing support in each of these domains. Specifically, the PCOR Unit advances work through four complimentary strategies: a. Working with the CRP Education Unit to host a series of educational seminars and workshops to prepare investigators to submit PCORI applications. b. Providing project specific consultative services through review of investigator-initiated proposals in the pre-award phase. c. Supporting the expansion and evaluation of methods for collecting patient reported outcome measures, specifically as routine components in clinical care settings. d. Establishing best practices for patient and community engagement strategies and disseminating these resources to investigators. ACCOMPLISHMENTS • The PCOR Unit was formed in September 2014. Dr. Josh Metlay was named the inaugural director. • PCOR Unit worked with CRP staff to create web site additions that allowed investigators to rapidly access current resources, including prior PCORI educational presentations, PCORI web based tools (including methodological guidance documents), and links for creating project consultations. Examples of such initial consultations include: 1. Marlene Freeman, MD submitted a PCORI proposal under the “Assessment of Prevention, Diagnosis, or Treatment Options” RFA. Her proposal linked with a national advocacy organization to study use of prophylactic antidepressant medication in woman with prior history of postpartum depression. Key methodological questions related to options for nonrandomized study designs to study treatment effectiveness. Proposal submitted in October 2014. 2. Brian Skotko, MD submitted a PCORI proposal under their “Addressing Disparities” RFA to study “Virtual evidence based healthcare for underserved patients with Down syndrome.” Key questions related to the choice of the best outcome measures for the study and based ways to engage providers in the study rollout and implementation. Proposal submitted in October 2014. • The PCOR Unit, in collaboration with Dr. Andrew Nierenberg and the Education Unit, has developed a proposal for a seminar series, which will include lectures and workshops designed to support both CRP Program Review Patient Centered Outcomes Research (PCOR) Unit 42 new and established investigators who are planning to submit applications to PCORI. The training program will be launched in the spring of 2015, specifically designed to support investigators who are planning to submit letters of intent for applications during the second half of 2015. • PCOR Unit hired a part-time research assistant, Emily Wendell, who is working with Dr. Metlay and Susan Edgman-Levitan to accelerate the implementation of new patient reported outcome measures (PROMs) into primary care settings. Partners Healthcare System is supporting widespread adoption of PROMs as a component of meaningful use goals and population health management strategies. The primary PHS strategy involves the use of an electronic tool, which is supported on tablet devices and allows patients to report clinical outcomes, health status, preferences, and other self-reported measures while they are in ambulatory care settings. The PCOR Unit is collaborating with this PHS program to help accelerate adoption of these tools into routine clinical practice in order to create greater availability of patient reported measures for clinical investigators. A first project will implement a health assessment PROM in a series of MGH primary care practices this winter with an evaluation strategy developed to validate the measures and identify opportunities for further scale up. • PCOR Unit is partnering with investigators at Chelsea Health Center to build and evaluate a model of stakeholder engagement for clinical researchers. The Chelsea Health Center Research Roundtable, formed in 2013, is a monthly gathering of a diverse group of health professionals and researchers based in Chelsea who are conducting community-based and community-partnered research studies. The roundtable provides a forum for sharing of best practice, feedback on protocols in development, and facilitation of new collaborations. With support from the PCOR Unit, a Chelsea-based community research will be responsible for expanding this model to provide increased support for MGH researchers exploring research opportunities at this site as well as developing standardized approaches for building engagement strategies in other communities where MGH researchers are interested in launching research projects. LESSONS LEARNED • There is a relatively large community of junior and established clinical investigators at MGH who are actively exploring funding opportunities through PCORI and are seeking more training and research support. • While PCORI has adopted an approach to assure that research funding is equitably distributed on a national level, there are already several notable examples of successful PCORI applications from MGH (either as the prime applicant or subcontractor). The community of funded PCORI investigators is growing at MGH and provides an important opportunity to mentor new investigators and create valuable collaborations in order to expand our PCOR activities. • Stakeholder engagement strategies are challenging. Many stakeholder groups have limited research experience and we will need to develop standardized training options for patient and caregivers who are participating in PCORI applications and funded projects. Collaboration with BWH may be critical in this regard. • The emergence of clinical research networks, including both patient powered research networks and clinical data research networks with direct ties to MGH, provide an important opportunity for MGH investigators to partner with these networks to launch large scale comparative effectiveness trials and other clinical studies. CRP Program Review Patient Centered Outcomes Research (PCOR) Unit 43 Biostatistics Unit Dianne Finkelstein, Ph.D., Director Hang Lee, Ph.D., Lead Statistician GOALS The broad goal of the CRP’s Biostatistics Unit is to support the biostatistical needs of the MGH’s clinical research community by providing timely and onsite consultative biostatistical expertise. Specifically, the Biostatistics Unit’s faculty: • Assist in the study design for clinical research grant applications prior to submission, and join grant research teams to ensure sufficient statistical support of research once funded; • Guide MGH’s clinical investigators in the selection of the appropriate biostatistical methodology and interpretation of data for papers intended for submission to journals; • Serve the CRP’s educational mission via a biostatistics Lecture Series and individual tutorials in collaboration with the Education Unit; • Serve on the IRB to provide statistical review of submitted protocols; and • Provide statistical, database, and web software for applications needed to conduct clinical research. ACCOMPLISHMENTS Overview of Principal Activities: In addition to Unit Chief, Dianne Finkelstein, Ph.D., seven other biostatistics faculty members from the MGH Biostatistics Center participate in the Unit supported by the CRP: David Schoenfeld, Ph.D., Hang Lee, Ph.D., Douglas Hayden, Ph.D., Eric Macklin, Ph.D., Hui Zheng, Ph.D., Brian Healy, Ph.D, and Lily Altstein, Ph.D. Our pool of MGH faculty statisticians provides a full spectrum of local biostatistical expertise to match the broad range of needs of the MGH clinical research community. CRP offers free initial consultations of 4-6 hours to all MGH clinical investigators planning an IRB approved human study. Dr. Lee, Assistant Professor of Medicine and Director of the CRP’s Biostatistical Consulting Laboratory, triages each initial inquiry from MGH physician scientists, taking into consideration the nature of the investigator’s need, in-house biostatistical expertise, and time required. The Unit ensures statistical expertise on grants by providing FTE support to each researcher who requests a statistician on his/her grant, guaranteeing that the research will have adequate statistical support for study design, development, conduct, analysis and dissemination. To outreach further to clinical investigators, CRP statisticians now serve on the MGH IRB, providing statistical review and guidance on protocols reviewed biweekly. When requested, Data Monitoring Committee statistical support is provided as well. The Unit offers both formal lecture series in biostatistics and selective biostatistics workshop sessions within the CRP’s Education Unit. This year, the Biostatistics Unit brgan to offer new support options: • K-awardees, who have no funding for statistical analysis within their K award grant, are now offered free biostatistical support for their projects. • Some investigators require a one-time extended statistical analysis. Newly developed Biostatistics Core provides short-term fee-for-service statistical support for more sophisticated data analysis. CRP Program Review Biostatistics Unit 44 • • For junior investigators, who seek assistance and statistical computing support to learn and then complete their own analyses, we provide a computing laboratory with statistical software and personnel and library support. The lab is accessible at all hours to MGH investigators. In response to requests for support in submitting trial results to www.clinicaltrials.gov, the Unit has developed a lecture and online tutorials as well as statistical computing support to allow investigators to retrieve the summary measures required by the website. Individual Consultations: The CRP supported 51 consultations, which were directed to the Unit exclusively through the CRP. The majority (60%) of the consultations were with junior investigators (Instructors, Assistant Professors, or Fellows, working in collaboration with senior faculty). The remaining were primarily consultations with residents, medical students, research associates, and research nurses and pharmacists, which is a notable increase in volume and proportion of these three categories (38%) compared to 12% in 2013. The major areas of the investigator requests came from Medicine (29%), Surgery (21%), Psychiatry (16%), and other areas included Neurology, Ob/Gyn, Cardiology, Emergency Medicine, Anesthesia, Pediatrics, Radiology, Graduate Medical Education, Pharmacy, Rehabilitation, Ophthalmology, and Nursing. A notable change in trend was the increase in the requested consultations from Psychiatry, Ophthalmology, Nursing, and Pharmacy. The typical consultations involved study design or analysis advice for manuscript preparation, handling IRB submissions, and education on special statistical method topics. The usage statistics (total of 51 consultations with 340 hours) by faculty ranks, departments/specialty, and service types are presented in Figs. 1–3. Figure 1: Percent of Projects by Faculty Ranks Assoc./Full Professor 2% Fellow 16% Assistant Professor 20% Instructor 24% Other (Residents, RN, etc) 38% N = 51 Figure 2: Percent of Projects by Department Specialty MEEI 2% Radiology 2% Pediatrics 2% Other 4% Nursing 4% Neurology 6% Anesthesia 6% Orthopaedics 8% Psychiatry 16% Surgery 21% Medicine 29% N = 51 CRP Program Review Biostatistics Unit 45 Figure 3: Percent of Projects by Project Types IRB Resubmission Grant Submission Education on Stats Methods 2% 12% 13% Study Design 26% Analysis Advice 47% N = 51 Grant Submissions: An important aspect of the CRP support of investigators is the collaboration on research grants. This includes a range of discussions from study design, contributing the statistical considerations to the application to committing a portion of their time to the grant research if it is funded. During the past year, members of the Biostatistics Unit were included as personnel for 92 grants (Figure 4 shows breakdown by Department). This represents a large increase compared to 82 in 2013. If the grant is funded, the MGH statistician will then shift a portion of their activities to new personnel to make their time available to the new project. Figure 4: Percent of Submitted NIH Grants by PI Departments Other Surgery 3% 4% Radiology 15% Neurology 15% Psychiatry 25% Medicine 37% N = 92 K-Awardees Mentoring: Since August 2014, the Unit has begun providing increased effort to the MGH K-Awardees for extensive consulting and mentoring, which requires more than typical CRP consulting. In this period, there are 11 junior investigators (accounting for about 50 hours) who have been receiving this support. Statistical Computing Lab: We provide junior investigators open access to a computing laboratory with statistical software and personnel and library support. The average usage was 1-3 hour long one visit per week. The lab computers provide common statistical IT packages, including SAS, STATA, PASS (power and sample size), with newly added Graphad/Prizm, JMP, and SPSS to meet the requests of laboratory and pharmacokinetics investigators who needed Prizm, and clinical investigators needing factor- and item analyses, ROC analysis, and general linear mixed effects model JMP and SPSS), The lab also provided updated educational material including on-line tutorial books, and lecture notes developed by Dr. Healy, http://hedwig.mgh.harvard.edu/biostatistics/software and http://hedwig.mgh.harvard.edu/biostatistics/stathelp. CRP Program Review Biostatistics Unit 46 www.Clinicaltrials.gov statistical software and support: The Unit has developed a lecture and online tutorial as well as statistical computing support to allow investigators to retrieve the summary measures required by the www.clinicaltrials.gov website. This input must be entered directly by the PIs. These summary statistics include target- and accomplished recruitment sizes, efficacy measures with 95% confidence intervals and p-values, adverse event rates, and an indication (or narrative summary) of the statistical methods used. The tutorial is a step-by-step demonstration of calculation of these summary measures. The computing support includes standard preprogrammed modules to access the trial data files and produce the statistics, write them in the correct field, check the completeness, and submit the report. In the case of the trials that require more complex programming beyond this module, the Unit offers special consultations. Education: Drs. Lee and Zheng participated in delivering the CRP lecture “Study Design: Statistical Perspective session of the Conquering the K: Submitting an NIH Career Development Award Proposal. Dr. Healy offered the annual CRP lecture, “Basic Biostatistics for Clinical Research”, as well as the Harvard Catalyst Certificate in Applied Biostatistics which was offered to the local MGH investigators. Dr. Lee offered biostatistics tutorials to MGH-THI resident training program, and served as a preceptor of the CRP’s Design and Conduct of Clinical Trials course. The aforementioned computing lab is used in conjunction with formal course and was used by 54 researchers (vs. 30 in previous year) who received consultation for sessions averaging one hour in length. The level of CRP tutoring topics have become more advanced, including longitudinal data, genetic analysis, and the multiple imputation technique to deal with missing data arising from randomized clinical trials. LESSONS LEARNED From Consulting Activities • Proximity Matters: A crucial function of the program is to provide MGH’s clinical investigative community with local statisticians as interactive collaborators and/or co-investigators on their grant proposals through the consulting activities and laboratory serially over time. As evidenced by the markedly increased number of submitted grants in collaboration with Biostatistics Unit increased (from 82 in 2013 to 92 in 2014), it is essential that these collaborations lead to the statistician becoming an active member in the research. Such close and evolving interactions are facilitated by the singular and onsite commitment of the CRP Biostatistics Unit to the investigators of the MGH. During the year, Biostatistics Unit offered PhD or MA statistician support (more than .5 FTE) to the research programs of several investigators in the MGH, including Drs. James Perrin (Pediatrics), Maurizio Fava and Andrew Nierenberg (Psychiatry), Donna Felsenstein (Infectious Disease), Kenneth Freedberg (Infectious Disease/MPEC) and Steven Safren (Psychiatry). In response to a rising demand for short-term fee-for service consults for data analysis we developed a Biostatistics Core. This service partners with the CRP service as we are able to offer free CRP consults for Statistical Analysis Plans, which are then carried out by the Core statisticians. This has been especially useful to departments like psychiatry or nursing who have funding to support a limited but substantial portion of a statistician's (FTE) time, but do not have a stable funding support for statistics as a grant would provide. • CRP goes beyond Harvard Catalyst: Harvard Catalyst also provides a consulting service for Harvard investigators and some of our statisticians provide consultations for both Catalyst and CRP. However the CRP efforts summarized above are distinct from those offered by Catalyst in several ways. First, the CRP consultations are guided to the statistical group by CRP faculty and staff who are assisting with other aspects of supporting their individual projects (such as IRB submission, budget preparation etc): Thus these efforts are tightly coordinated by the complete support that is unique to the CRP. Second, both the educational milieu and technological support for the biostatistics support services CRP Program Review Biostatistics Unit 47 offered by the CRP is local. Thus, courses and computer lab offered by CRP statisticians are available on-site at MGH and at times that are convenient for physician scientists with complex patient care and clinical responsibilities (in contrast to Catalyst courses which reside solely at the Longwood campus and during the daytimes only). Finally, statisticians working with investigators on preparation of their individual grant applications are then available to commit their time to the eventual execution of the grant and research effort as a member of the research team in contrast to Catalyst collaborations where only limited consultations for design or analysis plans are supported and there is no commitment to future collaboration. Thus, the spectrum of support provided by CRP’s Biostatistical Unit is complete, local (onsite), and comes with a commitment to be part of the research team – unique features that cover the full spectrum of services made available to MGH investigators that distinguish these efforts from the Catalyst supported functions. From the educational mission • The Need is Expanding: The annual CRP Basic Biostatistics Course has been received very well and enrolled approximately r200 clinical investigators. Many of the MGH’s evolving clinical investigative community are now alumni and have developed a collegial relationship with the Biostatistics Unit through our consultative support activities or tutorials. In many cases, these alumni have become part of ongoing research teams that fully integrates the MGH’s biostatistics faculty and results in vastly improved applications as well as quality of ultimate outcomes. There are also educational components within the individual biostatistical consulting projects, several of which have become crucial and now required components of NIH career development awards (K series) that often require statistician co-mentors, a role particularly facilitated by our onsite presence. In response to this expanding demand for biostatistics education, we will expand the biostatics offerings in the coming year in collaboration with the CRP’s Education Unit. This collaborative support was launched with a very successful short course in Biostatistics given by Dr. Brian Healy. The course has expanded to offer online homework and blogs for communication between faculty and students. A particularly popular unique aspect of his program is the open office hours where investigators are invited to drop in and discuss their research proposals and analyses. This service also includes standing statistical computing and consult lab in dedicated space contiguous to the Biostatistics Unit. • There is an interest in providing additional online lectures and tools to allow investigators to learn statistics at their own timing and pace. In the context of consultations on study design, we recently identified a need for a new education module that could focus on “Developing a Study Proposal and Statistical Design”. This short course will benefit early career Fellows who plan to propose a clinical study but have not had sufficient clinical research and statistical training. This will be a “light” abridged version of the “Basic Biostatistics for Clinical Research” to cover issues of how to translate medical questions into the framework of testable statistical hypotheses and adequate research design. ADAPTATION PLANNED Many MGH investigators would benefit from more statistical support on their grant proposals. Hence, it would be useful if the MGH could establish a new mechanism whereby the CRP’s biostatistical review could be inserted into the grant submission process, allowing at least 2-4 weeks prior to submission. This additional support would be especially useful for grants that are availing themselves of the MGH’s bridge funding to improve the yield on this institutional investment. Similarly, a mandatory statistical review prior to any IRB approval of all clinical studies coincident with that of IRB review or even required prior to it would ensure that study designs are compatible with research goals and might streamline use of valuable committee time. Finally, the Biostatistics Unit is becoming more visible to MGH researchers with Dr. Finkelstein’s regular attendance at ECOR meetings and Drs. Lee and Hayden’s attendance at MGH IRB Panel A. Expansion of such a role in the review of research grants, awards, and infrastructure decisions could raise awareness of the Unit further. CRP Program Review Biostatistics Unit 48 Appendix CRP Website and Evaluation Tools Liz Salomon, Ed.M., Sr. Project Manager GOALS During this year of transition for the CRP, the goals were • • To continue making the CRP’s website responsive to the new features of the Program: and Enhance the ability to evaluate existing and new courses, consultations and services. ACCOMPLISHMENTS Website With the introduction of new faculty, courses, consultations and services, the CRP website and marketing materials have been continuously updated to reflect the increasing breadth of its offerings. Of particular note, were the introductions of Epic support services and the CRP’s Patient Centered Outcomes Research (PCOR), Imaging Biomarkers, Biostatistics for K Awardees and Electronic Health Record Research consultations. The CRP’s website continues to serve as both a training tool and a resource guide for the MGH clinical research community. Since its launch on Clinical Research Day in October of 2012, the site has consistently shown increases in use from previous years. Figure A illustrates visits per month for November 1 – October 31, 2011- 12, 2012 - 13 and 2013 - 14. As in years past, this figure points to steady improvements in use throughout the year with particularly heavy website usage during the time leading up to and following Clinical Research Day. CRP Website Visits Per Month November 1 - October 31, 2011-12, 2012-2013 & 2013-14 Number of Visits/Month 8,000 2013-2014 6,000 2012-2013 2011-2012 4,000 2,000 0 Nov Dec Jan Feb Mar Apr May Jun Jul Aug Sep Oct Evaluations The CRP’s online evaluation system for courses continues to facilitate the evaluation process for those attending Education Unit offerings and those seeking to learn from their feedback. Evaluations throughout the past year have been overwhelmingly positive with the overall rating for all courses (with a scale that places 1 as poor and 4 as excellent) averaging 3.5. Getting this feedback from course participants has allowed the Education Unit staff greater ability to provide feedback to course faculty in real-time and a more expeditious way to be responsive to participant feedback for future course offerings. This year, the CRP has continued to use its online evaluation tools to seek and receive feedback about its consultation and support services. Feedback provided from these surveys have been shared with CRP CRP Program Review CRP Website and Evaluation Tools 49 faculty and staff to inform their continued growth and learning and has also been posted on the CRP website to provide consumers with insight from their peers about the value of the CRP’s offerings. Examples of feedback received via this mechanism are available on the CRP website. LESSONS LEARNED Resources like the CRP’s website and its online course, consultation and service evaluations have continued to provide the CRP with easy ways to educate and support the MGH clinical research community to help shape its current and future vision and goals. These mechanisms provide important insights into the CRP’s successes and challenges and help the Program be responsive in real time to the needs of the MGH clinical research community. ADAPTATION PLANNED In the coming year, the CRP will: 1. Work with the MGH marketing department to fold the CRP’s website content into the MGH Research Website. 2. Ensure that the content of this site will address not only the needs of the MGH clinical research community, but also the interests of MGH patients and potential collaborators. 3. Continue to make the website’s content dynamic and responsive to the changes as the CRP becomes part of the larger MGH Research Institute infrastructure. 4. Continue to enhance its online evaluation tools to assist in the consolidation of feedback about CRP consultations, courses and services. CRP Program Review CRP Website and Evaluation Tools 50