Hamstring Injuries - Bulletin of the NYU Hospital for Joint Diseases

Bulletin of the NYU Hospital for Joint Diseases 2012;70(1):41-8 41
Hamstring Injuries
Christopher R. Ropiak, M.D., and Joseph A. Bosco, M.D.
Abstract
Hamstring injuries are a frequent injury in athletes. Proximal injuries are common, ranging from strain to complete tear. Strains are managed nonoperatively, with rest followed by progressive stretching and strengthening. Reinjury is a concern. High grade complete tears are better managed surgically, with reattachment to the injured tendon or ischial tuberosity. Distal hamstring injury is usually associated with other knee injuries, and isolated injury is rare.
T he hamstrings are amongst the most frequently injured muscle or tendon groups seen in athletes, particularly those participating in running, jumping, and kicking sports, as well as water skiing. Surgical intervention, however, is rarely indicated mainly because injury tends to occur at the musculotendinous junction and is amenable to nonoperative treatment.
Historically, the term “hamstring” is derived from the trade of butchering. Pig carcasses were hung up by these tendinous muscles in the thigh of the ham for slaughtering.
Additionally, the verb “to hamstring” means to disable or to render useless. This is testament to the importance of the hamstrings in both daily life and recreational activities.
1
As in all muscle-tendon groups, the hamstring injury spectrum ranges from mild strain to complete avulsion.
Strains occur in both the young and old, weekend warriors, and elite athletes. The focus of this article is to give an overview of injuries to the hamstrings and operative indications and outcomes, including a literature review of the rare isolated distal hamstring injury.
Christopher R. Ropiak, M.D., and Joseph A. Bosco, M.D., are in the Department of Orthopaedic Surgery, NYU Hospital for Joint
Diseases, New York, New York.
Correspondence: Christopher R. Ropiak, M.D., Union County
Orthopedic Group, 210 West St. Georges Avenue, Linden, New
Jersey 07036; ropiakc@gmail.com.
Anatomy
The hamstrings are made up of three separate muscles: semimembranosus, semitendinosus, and biceps femoris, the latter with a long and short head. The ischial tuberosity is the common origin for the three muscles that originate as an incompletely separated tendinous mass. The separate muscles become distinguishable 2 to 10 cm distal to the ischial tuberosity, with the semimembranosus splitting off first. The hamstrings span both the hip and knee joint.
During certain activities, these two joints may be moving in opposite directions, contributing to a predisposition to stretch injury of the hamstrings. The hamstrings have more abundant type II muscle fibers, which give explosive force compared to the quadriceps.
1-8
The semimembranosus originates on the ischial tuberosity and inserts through five distal expansions on the posteromedial aspect of the tibia: oblique popliteal ligament, posterior capsule and posterior horn of the medial meniscus, posterior oblique ligament, aponeurosis of the popliteus muscle, and an anterior portion, which passes beneath the medial collateral ligament. It is a significant contributor to the stability of the knee. Its action is to flex and medially rotate the calf at the knee as well as extending, adducting and medially rotating the thigh at the hip.
1,2,6,8
The semitendinosus also has its origin on the ischial tuberosity and inserts on the proximal medial metaphysis of the tibia with the gracilis and sartorius as the pes anserinus, overlying the medial collateral ligament. It functions as a flexor and internal rotator of the calf at the knee as well as provides rotatory valgus stability to the knee.
1,2,6,8
The biceps femoris has two heads: the long head and short head. The long head originates on the ischial tuberosity and sacrotuberous ligament; the short head originates distally on the posterolateral femur, just lateral to the linea aspera, the lateral supracondylar region, and the lateral intermuscular septum. The long head inserts through a complex tendinous
Ropiak CR, Bosco JA. Hamstring injuries. Bull NYU Hosp Jt Dis. 2012;70(1):41-8.
42 Bulletin of the NYU Hospital for Joint Diseases 2012;70(1):41-8X and fascial insertion to the fibular head and lateral condyle of the tibia. The short head attaches into the tendon of the long head of biceps as well as fascial and tendinous insertions to the posterolateral capsule, the capsulo-osseous layer of the iliotibial tract, the fibular head, and the proximal lateral tibia.
Its action is to provide flexion and lateral rotation of the leg at the knee and to extend, adduct, and laterally rotate the thigh at the hip. The short head is primarily a leg flexor with the thigh extended; the long head gives posterior stability to the pelvis and extends the pelvis on the hip.
1,2,6,8
All of the combined hamstrings also act as an agonist to the anterior cruciate ligament, providing rotatory and anterior stability to the knee by preventing forward displacement of the tibia on the femur during flexion.
1,2,6,8
The innervation of the hamstring is through the tibial branch of the sciatic nerve (L5, S1, S2, and S3) to the semimembranosus, semitendinosus, and long head of the biceps.
The short head of the biceps femoris alone is innervated by the peroneal branch of the sciatic nerve (L5, S1, and S2).
The biceps femoris, therefore, has a dual innervation, which some believe may predispose it to injury.
1,2,6,8-11
A cadaveric study by Miller in 2007 helped define the relevant surgical anatomy in this region. The inferior gluteal nerve and artery is 5 cm proximal to the inferior border of the gluteus maximus. So when retracting the gluteus maximus proximally, one should avoid placing a retractor excessively deep in this region. Also, the sciatic nerve was found to be 1.2 cm lateral to the most lateral aspect of the ischial tuberosity.
Regarding the footprint of the hamstring, the semitendinosus and biceps femoris share an oval shaped footprint that is 2.7 cm in diameter from proximal to distal and 1.8 cm from medial to lateral. The semimembranosus footprint is crescent shaped and lays lateral to the semitendinosus and biceps femoris footprint. It measures 3.1 cm from proximal to distal and 1.1 cm from medial to lateral.
7
Injuries
Incidence and Etiology
Injuries can be broadly classified into direct and indirect mechanisms and can be further categorized as lacerations, contusions, strains, delayed-onset muscle soreness, and cramps. The focus of this review is strains, which can be either complete or incomplete. Incomplete strains are commonly referred to as a “pulled muscle” by the general population, while a complete or grade III strain is a tear or rupture. An overwhelming majority of injuries results from indirect trauma. Previous reports in the literature cite that
12% of hamstring injuries may involve at least a partial tear or avulsion of the proximal origin. Nine percent of these may be complete tears.
2-6,8,10,12-14
Hamstring strains are commonly encountered in running, jumping, hurdling, and kicking sports. It is the most common injury in hurdling. A prospective Australian-rules football epidemiological study found that hamstring strains composed 13% of the almost 2,400 reported injuries over 2 seasons and led to a significant amount of missed play. The biceps femoris is the most commonly single strained muscle in the hamstring muscle group.
15 A study by Brubaker and
James in 1974 reviewed 109 injuries to runners. They found that hamstring strains accounted for 50% of strain injuries to sprinters, 20% of strain injuries in middle-distance and long-distance runners.
16 It can be inferred that hamstring injuries become more common with more explosive movements with greater limb range of motion.
Sprinting and hurdling commonly produce hamstring strains because range of motion of the limb is greatest and the forces involved are also at their maximum due to high angular velocities and acceleration of limb segments. If the musculotendinous unit elongates beyond its flexibility capacity, a tear will result. It is believed that the biceps femoris is most prone to injury during foot take-off phase of running, while the semitendinosus and semimembranosus are under the most stress during the swing phase.
16
Gait analyses during running demonstrate that the hamstrings undergo routine eccentric contraction during the last
25% of the swing phase to assist in proximal hip extension while decelerating knee extension distally, opposing the quadriceps activity. The hamstrings remain active during the first half of the stance phase to produce hip extension and resist knee extension through a concentric contraction.
2
Complete avulsions become more common with other activities, such as water skiing, dancing, weight lifting, and ice-skating. The most common mechanism of injury is through an eccentric contraction with the hip flexed and the knee extended, such as the motion involved commonly in water-skiing, doing splits, and doing hurdles.
3-6,8,10,14,16-18
Sallay and colleagues in 1996 published a series of 12 waterskiers with proximal hamstring ruptures and found that injuries in novice skiers occurs from an eccentric contraction while getting up from a submerged position, while the expert skier sustained their injuries from a fall. The novice skier is more likely to get up in a position with his hips flexed and knee extended, placing maximal tension on the hamstring.
5
There are several proposed factors that may predispose someone to a hamstring strain. One factor to consider is inadequate warm-up or stretching. An animal study by
Safran in 1988 demonstrated that warmer muscles have increased muscle length to failure ratio and that cold muscles tear at shorter lengths.
19 Another factor is poor endurance or strength. If the hamstring becomes fatigued or is disproportionately weak compared to the quadriceps, its ability to counteract the force of knee extension in the swing phase or to provide adequate hip extension torque in stance phase may result in overstretch injury. Both strength and flexibility decrease when muscle becomes fatigued. It relaxes more slowly and less completely and is, therefore, likely to be more prone to strain.
1-4,6,9-11,18-20
Other contributing factors include poor technique, poor posture, leg length inequality, and side to side muscle imbalance. The dual innervation of the biceps femoris has also
Bulletin of the NYU Hospital for Joint Diseases 2012;70(1):41-8 43 been speculated to play a role such that theoretically there may be asynchrony in activation of the two heads and predispose to injury. Brewer in 1960 and Craig in 1973 found that muscles that cross two joints are more commonly strained, for example the hamstrings, gastrocnemius, biceps brachii, triceps, and rectus femoris. In such situations, joints may be in motion in opposing directions, which makes the muscles that span the joints prone to injury.
21,22
In 1970, Burkett studied professional football player and track athletes and found two relationships that were significantly related to hamstring injuries. One was an imbalance in strength of quadriceps compared to ipsilateral hamstrings.
Another was a weak hamstring muscle group on one side compared to other side. For many years, a hamstring to quadriceps strength ratio of 0.5-0.6 was considered standard.
But in more recent years, this has been called into question.
More recent data found that that these ratios vary between male and females, between athletes in different sports, and even between athletes playing different positions on the same team.
2,6,9-11,18-21
Previous injury also may play a role. Hamstring injuries have a high rate of recurrence. A previously injured muscle is more prone to being injured again. If full recovery of flexibility, strength, endurance, and coordination is not achieved then there is the risk of recurrent or even more severe injury.
A prospective epidemiological study of injuries to English professional soccer players over 2 seasons found that re-injuries accounted for 48% of all strains, with hamstring injuries having the highest recurrence rate of all injuries.
13
Classification
A grade I or mild strain is characterized by a stretching of the musculotendinous unit with resulting tear of few muscle or tendon fibers and less than 5% disruption of structural integrity of the unit. An athlete may not even be aware of injury until after cooling down. Grade II strains are moderate strains or a partial tearing of the musculotendinous unit but without compete disruption. Grade III strains are severe, or a complete rupture of the musculotendinous unit with a resulting “rag mop” appearance macroscopically. These injuries are relatively rare, and it is this category in which surgical treatment may be recommended.
2-4,6,8,10,18,21,23,24
The general presentation of proximal hamstring strains includes a history of a tearing or pulling or, if severe, a
“pop” or sensation of being shot in the posterior thigh may be described. There will be complaints of generalized pain over the hamstring muscles. Depending on severity, there may be difficulty or inability to ambulate. Maximal pain is usually distal to the ischial tuberosity. Over the course of days, there will be ecchymosis that develops. The patient will have difficulty sitting due to pain at the tuberosity. Physical exam may reveal posterior thigh ecchymosis and swelling.
Tenderness over the insertion site is usually present, but palpation of a defect may or may not be easily established.
The patient may ambulate with a stiff-legged gait—avoiding hip and knee flexion. The examiner should palpate the entire length of suspected injured muscle, origin to insertion, with the patient prone and knee flexed 90°. One should document functional testing of the sciatic nerve, including the peroneal branch, which may be compressed or irritated by a hematoma. It is important to note any weakness of dorsiflexion of foot or eversion weakness of ankle. In the more chronic setting, physical exam findings are likely to be more subtle.
The patient may have weakness in knee flexion, functional impairment, and inability to sprint or participate in sports.
A straight leg raise to a position of maximum tolerance should be noted. This is also useful for guiding response to rehabilitation.
2-4,6,8,18,24
Proximal avulsions have been subclassified by Wood and coworkers in 2008 based on anatomic location, degree of avulsion (incomplete or complete), degree of muscle retraction (if complete), and presence or absence of sciatic nerve tethering. The classification is as follows: Type 1is an osseous avulsion (apophyseal injuries in skeletally immature); Type
2 is an avulsion at the musclotendonous junction; Type 3 is an incomplete tendon avulsions from bone, which may present late; Type 4 is a complete tendon avulsion with none to minimal retraction; and Type 5 is a complete tendon avulsion with retraction, subdivided into injury not associated with sciatic nerve involvement, Type 5a, and injury associated with sciatic nerve tethering, Type 5b.
4
The differential diagnosis for these injuries includes lumbosacral radiculopathy, piriformis syndrome, bursitis, and tumor (such as an osteochondroma) in chronic cases. These other entities need to be considered, especially with chronic cases where the history may be vague and presentation less dramatic.
6,8,18
Imaging
If the diagnosis of a mild strain is fairly certain, no imaging is usually necessary. With more severe injuries, a plain radiograph of the pelvis should be done to rule out ischial tuberosity avulsion. Magnetic resonance imaging has replaced other modalities, such as ultrasound, scintigraphy, and CT scans as the advanced modality of choice. When proximal avulsion is suspected, MRI is the most accurate imaging modality to evaluate the injury. With complete ruptures, there is often retraction of all three proximal tendons. One or two tendon avulsions are rare, and if present, the other tendons are usually at least partially involved. An MRI of a normal hamstring origin should demonstrate a homogeneously low signal on all pulse sequences. Acute injuries have high signal intensity on T2 as result of edema and hemorrhage and an intermediate intensity on T1. There will also be discontinuity of bone-tendon unit. The degree of retraction can be evaluated as well. Another finding suggestive of recent hamstring avulsion is a fluid collection around the tendon edge tracking distally within the investing fascia.
24
Chronic injuries are less predictable in appearance. Absence of fluid collection at margins of tendon edge, fatty
44 Bulletin of the NYU Hospital for Joint Diseases 2012;70(1):41-8X infiltration, reduction in volume of hamstring muscles, and scarring of tendon to adjacent structures are all suggestive of chronic hamstring injury.
24
Ischial Tuberosity Avulsion
When discussing proximal hamstring injuries, one must also consider apophyseal avulsions of the ischial tuberosity.
These injuries occur with the same mechanism of proximal hamstring tendon ruptures but with a predisposition to adolescents or young adults. The peak incidence is in the
15 to18 year range.
The ischial apophysis appears at 13 to 15 years old and fuses with the pelvis at 20 to 25 years old. The presentation and history is similar to that of strains, which will be discussed at more length later in the review. An x-ray of the pelvis will show asymmetry of the ischial tuberosity with possibly some displacement of the fragment.
18,25
In general, the treatment algorithm and details of treatment follow that of strains. Minimally displaced avulsions are treated conservatively with rest, ice, and immobilization with bed rest and a hinged knee brace. Protected weight bearing is recommended until painless ambulation is possible.
This is followed by gentle stretching and strengthening as pain tolerates. Isometric exercises are done before isokinetic exercises. Running and jogging may be introduced when tolerated. Return to competition is allowed after flexibility, strength, power, endurance, coordination, and agility return to pre-injury level.
25
Surgical indications include greater than 2 cm of displacement, or any displacement in an elite athlete, and symptomatic nonunion, which may manifest itself as a painful deformity. Nonunions of displaced avulsions can occur in up to two-thirds of cases, but not all of these are necessarily symptomatic. A displaced untreated avulsion may become scarred to the sciatic nerve and cause neurologic symptoms.
Alternatively, an avulsion in which the athlete was unable to regain adequate function may be indicated for surgical intervention. The surgical intervention would include, typically, excision of the nonunion and re-insertion of the proximal hamstring to the ischium, with suture anchors or through bone tunnels.
25
Treatment
Grade I and II strains are treated conservatively with rest, ice packs, relative immobilization, compression, non-steroidal anti-inflammatory drugs, and analgesics as needed. In the first 3 to 5 days the goal of treatment is control of hemorrhage, edema, and pain. Progressive ambulation is begun when swelling and tenderness begin to subside, assisted with crutches until pain-free walking is possible. Gentle painless stretching should be initiated. Strengthening is progressed as long as it remains pain-free (starting with isometric exercise, then progressing to isokinetic). Jogging and running are increased as tolerated. Return to competition is permitted after full recovery from the injury.
1-3,6,8,17,20
There is some controversy regarding the use and timing of
NSAIDs in the treatment of hamstring strains. Some suggest use only for initial pain relief as an animal study showed an NSAID (flurbiprofen) used for 2 to 3 days produced short-term gains in contractile and histologic properties of healing muscle, but after longer use, it showed detrimental effects.
25-27
Nonsurgical treatment for Grade III injuries are generally reserved for isolated single tendon avulsions with less than 2 cm of retraction, which is very rare. It is felt that the single tendon will scar to the intact tendons and allow for full return of strength and return to sports in about 6 weeks.
Literature indicates that nonsurgical treatment for complete tendon ruptures with retraction results in unsatisfactory outcomes including inability to resume an active lifestyle or sports, chronic knee flexion weakness, mild hip extension weakness, sciatic neuralgia, pain with sitting, and deformity.
It is for these reasons that for Grade III injuries surgical reattachment is commonly recommended. Surgical treatment is also recommended for those with delayed presentation or unsatisfactory results with nonoperative treatment.
2-8,12,14,17,28-31
Acute repair is recommended over delayed repair because it is easier to mobilize tendons acutely, and there is less chance of sciatic nerve involvement. Chronic or delayed repairs have less predictable results. There is potential for scarring of the stump to the sciatic nerve, which would require neurolysis at time of repair. Retraction may require allograft augmentation, commonly with Achilles tendon.
In Wood’s article, it was recommended that the ideal time to surgery is 4 to 6 weeks post injury. Injuries treated after
3 months had tendons that were retracted and indistinct, along with scarring around the nerve. Neurolysis at the time of surgery for chronic cases may be performed with the aid of a nerve stimulator depending on the surgeon’s comfort level, with the aid of a hand surgeon and loupe magnification.
2-5,8,12,14,23,28-32
Surgical Technique
Surgical repair or reconstruction is most commonly performed with the patient in a prone position. Most investigators recommend a longitudinal incision starting at ischial tuberosity, although a more cosmetic transverse incision has been described. The drawback to the transverse incision is that it is not an extensile approach and is contraindicated in chronic cases where scarring and retraction are likely to be a factor.
Dissection is carried down to the gluteal fascia, with care to avoid the posterior femoral cutaneous nerve, which crosses the hamstring from lateral proximal to medial distal. Damage to this nerve causes hypesthesia to the posterior thigh. Next, a transverse incision is made in the gluteal fascia at the inferior border of the gluteus maximus. The gluteus maximus is then elevated and retracted superiorly to expose the hamstring fascia, with care not to
Bulletin of the NYU Hospital for Joint Diseases 2012;70(1):41-8 45 place a retractor too deep on the ischium because of risk to the inferior gluteal nerve, which is about 5 cm proximal to the inferior edge of the gluteus maximus. Slight flexion of the hip aids exposure by moving the gluteus maximus more proximally.
A longitudinal incision of the hamstring fascia is then made. This is where fibrous scar tissue and hematoma may be encountered. The sciatic nerve can be palpated in this plane and is protected by lateral retraction of tendons (keeping in mind that it passes in close proximity deep and lateral to the proximal hamstring origin).
Fibrotic tissue is debrided from the tendon ends until normal tendon is encountered, avoiding excessive shortening of the tendons. The tendons are mobilized and tagged with a heavy suture. The ischial tuberosity is identified, and the lateral aspect is cleared with a periosteal elevator to expose the anatomic origin (remembering that the semimembranosus is most lateral and the semitendinosus and long head of biceps femoris are more medial).
The tuberosity is then prepared or curetted. Repair can then be commenced with transosseous repair or now more commonly with use of suture anchor repair. The repair should be done with the hip extended and knee flexed about
30° to 90°.
Anchor configuration and number vary in the literature, but most commonly a range of two to five anchors are used. Suture technique varies as well, with some surgeons preferring horizontal mattress, while others preferring to do a Bunnel, Kessler or Mason-Allen technique repair. Once the repair is complete the fascia and wound are closed in layers.
2-5,7,8,12,14,23,28-32
Postoperative
Postoperatively the repair should be protected from tension. This can be done with a custom fitted hip orthosis to restrict hip flexion and knee extension. However, other investigators have found that a hinged knee brace locked in flexion is adequate and well tolerated. The patient is allowed to ambulate with crutches over the next few weeks as the brace is brought into increasing knee extension. The brace is usually discontinued at about 6 weeks, at which point progressive stretching, range of motion, and strengthening is commenced. The average time to return to sports is about
6 to 9 months.
2-5,7,8,12,14,23,28-32
Outcomes
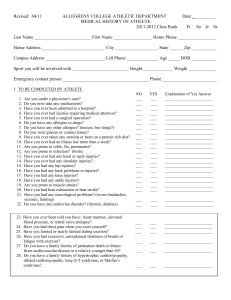
There are no large outcome studies in the literature. There are several case series or cohorts without control groups, and most have small numbers so they are underpowered. Table
1 summarizes the studies.
2-5,7,8,12,14,23,28-32
The study by Sallay is the most commonly cited in support of surgical treatment of complete tears. Patients were all water-skiers that presented to the investigator at an average of 5.6 months following the injury with a high level of dissatisfaction with nonoperative treatment of complete tears, and delayed surgical reconstruction was necessary in these cases. Some of studies have a large number of chronic cases, generally defined as greater than 3 months after the injury, though variable in the papers. Of note, chronic cases often required neurolysis and had a trend toward worse outcomes, although results were still largely satisfactory. It is also important to point out that with delayed presentations or chronic cases, it is unknown how many complete tears have occurred but never presented to a surgeon or physician for treatment. Presumably only those patients that are not happy with their progress or function after a hamstring tear are the ones that would come in for treatment several months after the injury.
The Sarimo study from Finland reported 70% good to excellent results and 30% moderate to poor results. Worse outcomes correlated to a significantly greater time to surgery. Wood’s study is the largest series in the literature. The investigators report very good outcomes with surgical repair, but they noted that in the case of chronic repairs there was a much greater need for neurolysis, there was more retraction and scarring of the tendons, and a greater need for post-op bracing. They also commented that when those chronic cases were associated with significant retraction there was a trend toward decreased postoperative hamstring strength and endurance. When considering the papers that report on a high percentage of acute repairs, it becomes evident that outcomes are generally favorable with surgical repair. Return to pre-injury level was high and strength measurements and patient satisfaction was high.
2-5,7,8,12,14,23,28-32
Reviews of the outcome studies conclude that surgical repair results in acceptable outcomes with 75% to 88% return to most sporting activities, 8% to 17% objective residual hamstring strength deficit, and a return to sports in about
6 to 12 months, with a high rate of patient satisfaction. If treatment is delayed, good results may still be obtained with chronic repair or reconstruction; however, a trend to larger dissection, more difficult surgery, need for allograft augmentation, and need for sciatic nerve neurolysis does exist.
The natural history and true denominator of patients never diagnosed or never seeking treatment and functioning well remains unclear. There are no studies with a control group of nonoperative treatment. Ultimately, the available literature supports that active patients do not tolerate the sequelae of complete proximal hamstring rupture and should consider repair or reconstruction, and they can expect fairly good results.
2-5,7,8,12,14,23,28-32
Distal Hamstring Tendon Injuries
Distal hamstring injuries are very rare in isolation of a significant ligamentous injury to the knee. Discussion of distal hamstring injuries in the setting of multiligamentous knee injuries is beyond the scope of this review. Included here is a review of isolated distal hamstring injuries. These injuries occur in sprinting sports or with hyper-extension of the knee.
33-37
46 Bulletin of the NYU Hospital for Joint Diseases 2012;70(1):41-8X
Table 1 Summaries of Studies on Proximal Hamstring Repair
Study
No. of patients
(No. acutely injured) Method of Repair
Sallay et al (1996)
Cross et al (1998)
Kilingele and Sallay
(2002)
12 (0)
9 (0)
11 (7)
Not specified (5 of 12 patients required late surgical repair)
Longitudinal incision with and without anchors
Longitudinal incision with 2-3 anchors
Average
Follow-up
7.5 yrs
(6 mos – 18 yrs)
48 mos
34 mos
Chakravarthy et al
(2005)
Brucker and Imhoff
(2005)
Cohen and Bradley
(2007)
Sarimo et al (2008)
Wood et al (2008)
Folsom and Larson
(2008)
Konan and Haddad
(2009)
4 (1)
8 (6)
8 (8)
41 (14)
72 (32)
26 (21)
10 (10)
Longitudinal incision with metal anchors or primary repair
Repair with average of
3.5 anchors
Transverse incision with
5 sutures anchors in “X” configuration
Longitudinal incision with 2-4 anchors
Longitudinal incision with 3 anchors
Chronic – Achilles allograft
Acute – suture anchors
3-5 suture anchors
12 mos
20 mos
6 mos
37 mos
(12-72mos)
24 mos
20 mos
12 mos
Outcome
58% returned to sports (all partial tears)
42% unable to return to sports at same level
(all complete tears)
Hamstring strength 60% at follow-up
All required neurolysis of the sciatic nerve
91% satisfaction
73% pain free or mild pain with activity
43% moderate limitations
85% return of strength with Cybex
75% returned to sport
All regained strength and near normal motion
All sciatic nerve symptoms resolved
75% returned to sport
10% deficit on isokinetic muscle testing
All satisfied
85% returned to sports at average of 8.5 mos
70% excellent to good (2.4 mos to surgery)
30% moderate to poor (11.7 mos to surgery)
84% isotonic HS strength (worse w/ delay)
89% HS endurance (worse w/ delay)
79% return to pre-injury level of sports
76% returned to sports
96% would have surgery again
No difference in acute vs chronic
(underpowered)
100% satisfied
HS strength 85% at 6 months
There are few published reports that focus on this topic.
The most significant paper is by Lempainen and associates from Finland with a series of 18 distal hamstring tears, with other papers confined to single case reports or very small case series. The paper out of Finland consisted of
6 professional athletes, 10 competitive-level athletes, and
2 recreational athletes. Injuries most commonly occurred during sprinting. Very few injuries are symptomatic, except in high level athletes in sports that rely on optimum function of the hamstrings. All reported athletes had symptoms including weakness of knee flexion, pain, stiffness, sense of instability of the knee, cramps, and spasms. The biceps femoris was injured in 11 patients, the semimembranosus was injured in 5 patients, and the semitendinosus was injured in 2 patients. Most of the injuries (15 to18) were located at the musculotendinous junction, 2 were avulsions, and 1 was a longitudinal tear. Of the 15 that were tears at the musculotendinous junction, 13 were repaired using sutures and excision of scar tissue. The other two had a distal tenotomy preformed to the ruptured part of the semimembranosus.
33-37
In the cases of avulsions, one injury was a biceps femoris avulsion that was re-attached to the fibular head with a suture anchor. In the other case, the avulsed semitendinosus was not able to be reattached at its insertion site and was then reinserted with sutures to the sartorius tendon. Follow-up averaged 37 months, and 13 excellent results were obtained,
1 good, 3 fair, and 1 poor result. The 13 excellent results were asymptomatic and able to return to pre-injury level of sport.
35 There was no nonoperative arm of this study to compare outcomes; therefore, it is difficult to draw conclusions from this paper or the other literature about when to operate and when not to operate on distal hamstring injuries in the acute setting. Operative intervention, in general, should be reserved for cases in which extended conservative treatment has failed to yield satisfactory results in a high functioning patient and when there is a high expectation of an improved outcome compared to nonoperative treatment.
Bulletin of the NYU Hospital for Joint Diseases 2012;70(1):41-8 47
An article by Schilders and coworkers reported a series of four professional athletes with partial rupture of the distal semitendinosus tendon. These patients failed nonoperative treatment and had debilitating pain that rendered them unable to participate in anything other than light training. All four patients underwent a tenotomy of the distal semitendinosus tendon and, at 2-year follow-up, all four were pain free and had been able to return to professional sports following surgery. This demonstrates that if a partial distal semitendinosus rupture fails conservative treatment, then a tenotomy is a reasonable option and may have good outcomes.
36
Some conclusions must be drawn from experience with hamstring autograft harvesting. Isolated distal hamstring injuries are “created” when harvesting the distal portion of the semitendinosus tendon as part of the hamstring autograft for surgeries, such as anterior cruciate ligament reconstruction. In general, harvesting the semitendinosus tendon and gracilis is well tolerated. The current literature base addressing the fate of the hamstrings after semitendinosus harvest is far from conclusive, and many questions remain to be answered. However, there is no doubt that distal hamstring tendons have the capability to regenerate to a “tendon-like” structure after harvesting. The question of full recovery of the natural hamstring function remains less clear. Studies addressing this are conflicting, controversial, and inconclusive. Some report almost full recovery of knee flexor strength, possibly through hypertrophy of the other hamstring muscles. Other studies have demonstrated significant reduction in isokinetic strength in the hamstring of the operated leg versus the nonoperative leg.
38,39 The fact is that harvesting the semitendinosus is well tolerated by the general population, and one might conclude that likewise isolated injuries to the distal hamstring tendons are well tolerated.
This is likely because the general population rarely, if ever, stress their hamstrings close to their maximum capacity in regards to endurance, flexibility, and power.
Ultimately, the literature is scarce about the incidence and treatment and outcomes of isolated distal hamstring injuries, and decisions have to be made on a case by case basis. Surgery is rarely necessary, but when it is performed the few reported outcomes are generally positive.
Conclusion
Hamstring injuries are a common injury among athletes.
The literature strongly suggests that operative management of complete, retracted proximal injuries offers improved outcomes compared to those managed nonsurgically. Both nonoperatively managed low grade injuries and surgically repaired high grade injuries produce good results, however, retearing is a concern. Isolated distal hamstring injuries are rare.
Disclosure Statement
The authors have no financial or proprietary interest in the subject matter or materials discussed, including, but not limited to, employment, consultancies, stock ownership, honoraria, and paid expert testimony.
References
1. Morris A. Sports medicine: prevention of athletic injuries. In:
Sports Medicine . Dubuque, Iowa: Em C. Brown Publishers,
1984, pp. 162-163.
2. Agre JC. Hamstring injuries: Proposed aetiological factors, prevention, and treatment. Sports Med. 1985 Jan-
Feb;2(1):21-33.
3. Cohen S, Bradley J. Acute proximal Hamstring Rupture. J
Am Acad Orthop Surg. 2007 Jun;15(6):350-5.
4. Wood D, Packham I, Trikha S, Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008
Nov;90(11):2365-74.
5. Sallay PI, Friedman RL, Coogan PG, Garret WE. Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med. 1996 Mar-Apr;24(2):130-6.
6. Mann G, Shabat S, Friedman A, et al. Hamstring Injuries.
Orthopedics. 2007 Jul;30(7):536-40;quiz 541-2.
7. Miller S, Gill J, Webb G. The proximal origin of the hamstring and surrounding anatomy encountered during repair: a cadaveric study. J Bone Joint Surg Am. 2007;89(1):44-8.
8. Clanton T, Coupe K. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998 Jun-
Aug;6(4):237-48.
9. Burkett LN. Causative factors in hamstring strains. Med Sci
Sports. 1970 Spring;2(1):39-42.
10. Burkett LN. Investigation into hamstring strains: the case of the hybrid muscle. J Sports Med. 1975 Sept-Oct;3(5):228-31.
11. Croisier JL. Factors associated with recurrent hamstring injuries. Sports Med. 2004;24(10):681-95.
12. Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998 Nov-Dec;26(6):785-8.
13. Hawkins RD, Hulse MA, Wilkinson C, et al. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. 2001 Feb;35(1):43-7.
14. Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008 Jun;36(6):1110-5.
15. Verrall G, Slavotinek J, Barnes P. The effect of sports specific training on reducing the incidence of hamstring injuries in professional Australian Rules football players. Br J Sports
Med. 2005 Jun;39:363-8.
16. Brubaker CE, James SL. Injuries to runners. J Sports Med.
1974 Jul-Aug;2(4):189-98.
17. Ishikawa K, Kai K, Mizuta H. Avulsion of the hamstring muscles from the ischial tuberosity. A report of two cases.
Clin Orthop Relat Res. 1988Jul;(232):153-5.
18. Zarins B, Ciullo JV. ACute muscle and tendon injuries in athletes. Clin Sports Med. 1983 Mar;2(1):167-82.
19. Safran MR, Seaber AV, Garrett WE. Warm-up and muscular injury prevention. An update. Sports Med. 1989 Oct;894):239-
49.
20. Knapik J, Jones B, Bauman C, Harris J. Strength, flexibility, and athletic injuries. Sports Med. 1992 Nov;14(5):277-88.
21. Brewer B. Mechanism of injury to the musculotendinous unit: Instructional Course Lectures. Am Acad Orthop Surg.
1960;17:354-8.
48 Bulletin of the NYU Hospital for Joint Diseases 2012;70(1):41-8X
22. Craig T. American Medical Association Comments in Sports
Medicine. In: Craig T (ed): American Medical Association
Comments in Sports Medicine . Chicago: American Medical
Association, 1973, pp. 25-27.
23. Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons.
Knee Surg Sports Traumatol Arthrosc. 2005 Jul;13(5):411-8.
24. Koulouris G, Connel D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003
Oct;32(10):582-9.
25. Kujala U, Orava S. Ischial apophysis injuries in athletes.
Sports Med. 1993;16(4):290-4.
26. Mishra DK, Fridén J, Schmitz MC, Lieber RL. Anti-imflammatory medication after muscle injury. A treatment resulting in short-term improvement but subsequent loss of muscle function. J Bone Joint Surg Am. 1995;77(10):1510-9.
27. Obremsky WT, Seaber AV, Ribbeck BN, Garrett WE Jr. Biochemical and histological assessment of a controlled muscle strain injury treated with piroxicam. Am J Sports Med. 1994
Jul-Aug;22(4):558-61.
28. Chakravarthy J, Ramisetty N, Pimpalnerkar A, Mohtadi N.
Surgical repair of complete proximal hamstring ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med. 2005 Aug;39(8):569-72.
29. Folsom GJ, Larson CM. Surgical treatment of acute versus chronic complete proximal hamstring ruptures: results of a new allograft technique for chronic reconstructions. Am J
Sports Med. 2008 Jan;36(1):104-9.
30. Klingele KE, Sallay PI. Surgical Repair of Complete Proximal
Hamstring Tendon Rupture. Am J Sports Med. 2002 Sep-
Oct;30(5):742-7.
31. Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010 Feb;34(1):119-23.
32. Marx RG, Fives G, Chu SK, et al. Allograft reconstruction for symptomatic chronic complete proximal hamstring tendon avulsion. Knee Surg Sports Traumatol Arthrosc. 2009
Jan;17(1):19-23.
33. Aliota RJ, Browne JE, Barnthouse CD, Scott AR. Complete rupture of the distal semimembranosus complex in a professional athlete. Clin Orthop Relat Res. 1997 Mar;(336):162-5.
34. Kusma M, Seil R, Kohn D. Isolated avulsion of the biceps femoris insertion-injury patterns and treatment options: a case report and literature review. Arch Orthop Trauma Surg. 2007
Nov;127(9):777-80.
35. Lempainen L, Sarimo J, Mattila K, et al. Distal tears of the hamstring muscles: review of the literature and our results of surgical treatment. Br J Sports Med. 2007 Feb;41(2):80-3.
36. Schilders E, Bismil Q, Sidham S, et al. Partial rupture of the distal semitendinosus tendon treated by tenotomy-a previous undescribed entity. Knee. 2006 Jan;13(1):45-7.
37. Sebastianelli WJ, Hanks GA, Kalenak A. Isolated avulsion of the biceps femoris insertion. A case report. Clin Orthop Relat
Res. 1990 Oct;(259):200-3.
38. Okahashi K, Sugimoto K, Iwai M, et al. Regeneration of the hamstring tendons after harvesting for arthroscopic anterior cruciate ligament reconstruction: a histological study in 11 patients. Knee Surg Sports Traumatol Arthrosc. 2006
Jun;14(6):542-5.
39. Nikolaou VS, Efstathopoulos N, Wredmark T. Hamstring tendons regeneration after ACL reconstruction : an overview.
Knee Surg Sports Traumatol Arthrosc. 2007 Feb;1592):153-
60.