Cefazolin Drug Monograph: Uses, Dosage, Side Effects
advertisement

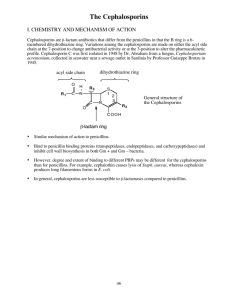
Name /bks_53161_deglins_md_disk/cefazolin 02/19/2014 01:01PM Plate # 0-Composite pg 1 # 1 Contraindications/Precautions Contraindicated in: Hypersensitivity to cephalosporins; Serious hypersensitivity 1 ceFAZolin (sef-a-zoe-lin) to penicillins. Use Cautiously in: Renal impairment (dosepand/orqdosing interval recom- Ancef Classification Therapeutic: anti-infectives Pharmacologic: first-generation cephalosporins Pregnancy Category B mended if CCr ⬍30 mL/min); Hepatic impairment; History of GI disease, especially colitis; OB: Half-life is shorter and blood levels lower during pregnancy; has been used safely; Lactation: Low concentrations of drug appear in breast milk; Geri: Dose adjustment due to age-relatedpin renal function may be necessary. Indications Treatment of the following infections due to susceptible organisms: Skin and skin structure infections (including burn wounds), Pneumonia, Urinary tract infections, Biliary tract infections, Genital infections, Bone and joint infections, Septicemia, Bacterial endocarditis prophylaxis for dental and upper respiratory procedures. Perioperative prophylaxis. Not suitable for the treatment of meningitis. Action Binds to bacterial cell wall membrane, causing cell death. Therapeutic Effects: Bactericidal action against susceptible bacteria. Spectrum: Active against many gram-positive cocci including: Streptococcus pneumoniae, Group A beta-hemolytic streptococci, Penicillinase-producing staphylococci. Not active against: Methicillinresistant staphylococci, Bacteroides fragilis, Enterococcus. Active against some gram-negative rods including: Proteus mirabilis, Escherichia coli. Pharmacokinetics Absorption: Well absorbed after IM administration. Distribution: Widely distributed. Penetrates bone and synovial fluid well. Crosses the placenta and enters breast milk in low concentrations. Minimal CSF penetration. Protein Binding: 74— 86%. Metabolism and Excretion: Excreted almost entirely unchanged by the kidneys. Half-life: Neonates: 3– 5 hrs; Adults: 90– 150 min (qin renal impairment). TIME/ACTION PROFILE (blood levels) Adverse Reactions/Side Effects CNS: SEIZURES (high doses). GI: PSEUDOMEMBRANOUS COLITIS, diarrhea, nausea, vomiting, cramps. Derm: STEVENS-JOHNSON SYNDROME, rash, pruritis, urticaria. Hemat: leukopenia, neutropenia, thrombocytopenia. Local: pain at IM site, phlebitis at IV site. Misc: allergic reactions including anaphylaxis and serum sickness, superinfection. Interactions Drug-Drug: Probenecidpexcretion andqblood levels of renally excreted cephalosporins. Route/Dosage IM, IV (Adults): Moderate-to-severe infections— 500 mg-2 g every 6– 8 hr; maximum 12 g/day. Mild infections with Gram-positive cocci— 250– 500 mg every 8 hr. Uncomplicated urinary tract infection— 1 g every 12 hr. Pneumococcal pneumonia— 500 mg every 12 hr. Infective endocarditis or septicemia— 1– 1.5 g every 6 hr. Perioperative prophylaxis— 1 g within 30– 60 min prior to incision (an additional 500 mg– 1 g should be given for surgeries ⱖ 2 hr). 500 mg-1 g should then be given for all surgeries every 6– 8 hr for 24 hr following the surgery. IM, IV (Children and Infants ⬎1 mo): 50– 100 mg/kg/day divided every 8 hr; maximum: 6 g/day Bacterial endocarditis prophylaxis in penicillin-allergic patients— 25 mg/kg 30 minutes prior to procedure; maximum dose: 1 g. IM, IV (Neonates ⱕ 7 days): 40 mg/kg/day divided q 12 hr. IM, IV (Neonates ⬎ 7 days and ⱕ 2 kg): 40 mg/kg/day divided q 12 hr. IM, IV (Neonates ⬎ 7 days and ⬎ 2 kg): 60 mg/kg/day divided q 8 hr. ROUTE ONSET PEAK DURATION Renal Impairment IM IV rapid rapid 0.5–2 hr 5 min 6–12 hr 6–12 hr IM, IV (Adults): CCr 10– 30 mL/min— Administer dose every 12 hr; CCr ⱕ10 mL/ min— Administer every 24 hr. ⫽ Canadian drug name. ⫽ Genetic Implication. CAPITALS indicate life-threatening, underlines indicate most frequent. Strikethrough ⫽ Discontinued. PDF Page #1 Name /bks_53161_deglins_md_disk/cefazolin 02/19/2014 01:01PM Plate # 0-Composite pg 2 # 2 2 ● IM: Reconstitute IM doses with 2 mL or 2.5 mL of with sterile water for injection to NURSING IMPLICATIONS Assessment ● Inject deep into a well-developed muscle mass; massage well. a achieve a final concentration of 225– 330 mg/mL. ● Assess for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC) at beginning of and throughout therapy. ● Before initiating therapy, obtain a history to determine previous use of and reac● ● ● ● ● ● ● tions to penicillins or cephalosporins. Persons with a negative history of penicillin sensitivity may still have an allergic response. Obtain specimens for culture and sensitivity before initiating therapy. First dose may be given before receiving results. Observe patient for signs and symptoms of anaphylaxis (rash, pruritus, laryngeal edema, wheezing). Discontinue drug and notify health care professional immediately if these problems occur. Keep epinephrine, an antihistamine, and resuscitation equipment close by in case of an anaphylactic reaction. Monitor bowel function. Diarrhea, abdominal cramping, fever, and bloody stools should be reported to health care professional promptly as a sign of pseudomembranous colitis. May begin up to several weeks following cessation of therapy. Assess patient for skin rash frequently during therapy. Discontinue at first sign of rash; may be life-threatening. Stevens-Johnson syndrome may develop. Treat symptomatically; may recur once treatment is stopped. Lab Test Considerations: May cause positive results for Coombs’ test in patients receiving high doses or in neonates whose mothers were given cephalosporins before delivery. May causeqserum AST, ALT, alkaline phosphatase, bilirubin, LDH, BUN, and creatinine. May rarely cause leukopenia, neutropenia, thrombocytopenia, and eosinophilia. Potential Nursing Diagnoses Risk for infection (Indications) (Side Effects) Diarrhea (Adverse Reactions) Implementation ● Do not confuse cefazolin with cefotetan, cefoxitin, ceftazidime, or cef- triaxone. IV Administration ● pH: 4.5– 7.0. ● IV: Monitor site frequently for thrombophlebitis (pain, redness, swelling). Change sites every 48– 72 hr to prevent phlebitis. ● Do not use solutions that are cloudy or contain a precipitate. ● If aminoglycosides are administered concurrently, administer in separate sites, if ● ● ● ● possible, at least 1 hr apart. If second site is unavailable, flush line between medications. Direct IV: Diluent: Dilute with sterile water for injection. Do not use preparations containing benzyl alcohol for neonates. Concentration: ⱕ100 mg/mL. Rate: Administer slowly over 3– 5 min. Intermittent Infusion: Diluent: Reconstituted solution may be further diluted with 0.9% NaCl, D5W, D10W, D5/0.25% NaCl, D5/0.45% NaCl, D5/09% NaCl, D5/ LR, or LR solution. Solution is stable for 24 hr at room temperature and 10 days if refrigerated. Concentration: ⱕ20 mg/mL. Rate: Administer over 30– 60 min. Y-Site Compatibility: acyclovir, alfentanil, allopurinol, alprostadil, amifostine, aminocaproic acid, aminophylline, amphotericin B lipid complex, amphotericin B liposome, anidulafungin, argatroban, ascorbic acid, atracurium, atropine, azithromycin, aztreonam, benztropine, bivalirudin, bleomycin, bumetanide, buprenorphine, butorphanol, calcium gluconate, carboplatin, carmustine, cefoperazone, cefotetan, cefoxitin, ceftazidime, ceftriaxone, cefuroxime, chlorampheniocol, cisplatin, clindamycin, cyanocobalamin, cyclophosphamide, cyclosporine, cytarabine, dactinomycin, daptomycin, dexamethasone, dexmedetomidine, digoxin, diltiazem, docetaxel, doxacurium, doxapram, doxorubicin liposome, enalaprilat, ephedrine, epinephrine, epirubicin, epoetin alfa, eptifibatide, esmolol, etoposide, etoposide phosphate, fenoldopam, fentanyl, filgrastim, fluconazole, fludarabine, fluorouracil, folic acid, foscarnet, furosemide, gemcitabine, glycopyrrolate, granisetron, heparin, hydrocortisone, ifosfamide, imipenem/cilastatin, indomethacin, insulin, irinotecan, isoproterenol, ketamine, ketorolac, leucovorin, lidocaine, linezolid, lorazepam, mannitol, mechlorethamine, melphalan, meperidine, metaraminol, methotrexate, methyldopate, methylprednisolone, metoclopramide, metoprolol, metronidazole, midazolam, milrinone, morphine, 䉷 2015 F.A. Davis Company CONTINUED PDF Page #2 Name /bks_53161_deglins_md_disk/cefazolin 02/19/2014 01:01PM Plate # 0-Composite pg 3 # 3 3 PDF Page #3 CONTINUED ceFAZolin multivitamins, nafcillin, nalbuphine, naloxone, nesiritide, nicardipine, nitroglycerin, nitroprusside, norepinephrine, octreotide, ondansetron, oxacillin, oxaliplatin, oxytocin, paclitaxel, palonosetron, pamidronate, pancuronium, penicillin G, perphenazine, phenobarbital, phenylephrine, phytonadione, potassium acetate, potassium chloride, procainamide, propofol, propranolol, ranitidine, remifentanil, rituximab, sargramostim, sodium acetate, sodium bicarbonate, streptokinase, succinylcholine, sufentanil, tacrolimus, teniposide, theophylline , thiamine, thiotepa, ticarcillin/clavulanate, tigecycline, tirofiban, tolazoline, trastuzumab, vasopressin, vecuronium, verapamil, vinblastine, vincristine, vitamin B complex with C, voriconazole, warfarin, zoledronic acid. ● Y-Site Incompatibility: alemtuzumab, amphotericin B cholesteryl, azathioprine, calcium chloride, caspofungin, cefotaxime, chlorpromazine, dantrolene, diazepam, diazoxide, diphenhydramine, dobutamine, dolasetron, dopamine, doxorubicin hydrochloride, doxycycline, erythromycin, ganciclovir, haloperidol, hydralazine, hydroxyzine, idarubicin, levofloxacin, mitoxantrone, mycophenolate, papaverine, pemetrexed, pentamidine, pentazocine, pentobarbital, phentolamine, phenytoin, prochlorperazine, promethazine, protamine, pyridoxime, quinupristin/dalfopristin, sodium citrate, tobramycin, trimethoprim/sulfamethoxazole, vinorelbine. Patient/Family Teaching ● Advise patient to report signs of superinfection (furry overgrowth on the tongue, vaginal itching or discharge, loose or foul-smelling stools) and allergy. ● Instruct patient to notify health care professional if rash, or fever and di- arrhea develop, especially if diarrhea contains blood, mucus, or pus. Advise patient not to treat diarrhea without consulting health care professional. Evaluation/Desired Outcomes ● Resolution of signs and symptoms of infection. Length of time for complete resolu- tion depends on the organism and site of infection. ● Decreased incidence of infection when used for prophylaxis. Why was this drug prescribed for your patient? ⫽ Canadian drug name. ⫽ Genetic Implication. CAPITALS indicate life-threatening, underlines indicate most frequent. Strikethrough ⫽ Discontinued.