Heart Failure: Nursing Assessment and Care
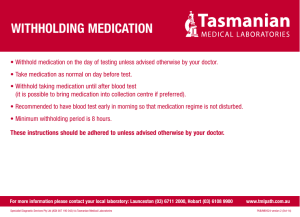
advertisement

Heart Failure: Nursing Assessment and Care Objectives 1. Understand the complexities of CHF and the care needs of a patient with CHF. 2. Employ critical components of diseases management into the care plan for frontline nursing care of the CHF patient Overview of CHF: The Problem One of most common causes of hospitalization, hospital readmission, and death. • Nearly 1.4 million hospitalizations (leading cause in > 64 y.o.) • 27% readmitted • Approximately 5.8 million Americans Outcomes suboptimal • 1 in 10 patients die within the first 30 days after hospitalization • 1 in 4 patients who survive are readmitted Financial burden $17 billion in total spending Overview of CHF …the inability or failure of the heart to provide sufficient forward output to meet the the perfusion and oxygenation requirements of the tissues will maintaining normal filling pressures Mechanisms: • Systolic dysfunction: Impaired cardiac contractile function • Diastolic dysfunction: Abnormal cardiac relaxation, stiffness or filling Anatomy: two pump system Functions: systole and diastole Cardiac output (CO) and ejection fraction (EF) CO = Stroke Volume X Heart Rate Normal 5.5 l/min (males) 5.0 l/min (females) EF = Stroke Volume / End Diastolic Volume X 100 Normal EF = 55-70% Systolic HF Abnormalities in systolic function • Reduced left ventricular ejection fraction (LVEF) • Usually with progressive chamber dilation and eccentric remodeling • HF with reduced LVEF (HFrEF) • EF < 50% Diastolic HF Abnormalities in diastolic function with symptoms • Normal LVEF • Normal LVEDV • Diastolic dysfunction • Usually with concentric remodeling or hypertrophy • HF with preserved LVEF (HFpEF) • EF > 50% Overview of CHF…Simplified Decrease in CO→ Increase in capillary pressure→ Symptoms Causes of Heart Failure? • Impairment of “filling it up or pumping it out” • • • • • • • Hypertension Cardiomyopathies Coronary artery disease Valvular disorders Dysrhythmias Diabetes Other….. Increased workload and end-diastolic volume enlarge the left ventricle. ►Increased heart rate, pale and cool skin, tingling in the extremities, decreased cardiac output, and arrhythmias. Blood pools in the ventricle and atrium and eventually backs up into the pulmonary veins and capillaries. ►Dyspnea on exertion, confusion, dizziness, orthostatic hypotension, decreased peripheral pulses and pulse pressure, cyanosis, and an S3 gallop. Rising capillary pressure pushes sodium (Na) and water (H2O) into the interstitial space, causing pulmonary edema. ►Coughing, subclavian retractions, crackles, tachypnea, elevated pulmonary artery pressure, diminished pulmonary compliance, and increased partial pressure of carbon dioxide. Because the left ventricle can’t handle the increased venous return, fluid pools in the pulmonary circulation, worsening pulmonary edema. ►Decreased breath sounds, dullness on percussion, crackles, and orthopnea. The right ventricle may now become stressed because it’s pumping against greater pulmonary vascular resistance and left ventricular pressure. ►Worsening symptoms. The stressed right ventricle enlarges with the formation of stretched tissue. ►Increased heart rate, cool skin, cyanosis, decreased cardiac output, dyspnea, and palpitations. Blood pools in the right ventricle and right atrium. The backed up blood causes pressure and congestion in the vena cava and systemic circulation. ►Increased central venous pressure, jugular vein distention, and hepatojugular reflux. Backed up blood distends the visceral veins, especially the hepatic vein. As the liver and spleen become engorged, their function is impaired. ►Anorexia, nausea, abdominal pain, palpable liver and spleen, weakness, and dyspnea secondary to abdominal distention. Rising capillary pressure forces excess fluid from the capillaries into the interstitial space. ►Edema, weight gain, and nocturia. Classification: ACC/AHA High risk of developing heart failure: • Hypertension diabetes, CAD, and family history of cardiomyopathy Asymptomatic heart failure: • Previous history of MI, left ventricular dysfunction, and valvular heart disease Symptomatic heart failure: • Structural heart failure, dyspnea and fatigue, and impaired exercise tolerance Refractory end-stage heart failure: • Marked symptoms at rest despite maximal medical therapy Classification: NYHA Class 1 (mild): • No limitation of physical activity; physical activity doesn’t cause tiredness, heart palpitations, or shortness of breath. Class II (mild): • Slight limitation of physical activity; the patient is comfortable at rest, but ordinary activity causes tiredness, heart palpitations, and/or shortness of breath. Class III (moderate): • Marked limitations of physical activity; the patient is comfortable at rest, but less than ordinary physical activity causes tiredness, heart palpitations, or shortness of breath. Class IV (severe): • Severe limitations of physical activity; the patient is unable to carry out any physical activity without discomfort. Symptoms are present at rest, and any physical activity increases that discomfort. Diagnosis • History and physical examination • Symptoms • Tests • EKG, Chest X-ray • Labs • • • • • CBC Electrolytes Glucose BUN and Creatinine B-type natriuretic peptide (BNP) • Echocardiogram Prognosis • If decompensated and hospitalization required: • Significant mortality risk of more than 20% at one year • NYHA stage IV have mortality rate of up to 50% at one year Treatment • Lifestyle modification • • • • • • Smoking cessation Limited alcohol consumption Low sodium diet Fluid restrictions Daily weight / symptom monitoring Medication compliance Treatment • Medications • Beta-blockers • Angiotensin-converting enzyme inhibitors (ACEI) • Angiotensin II receptor blocker (ARB) • Diuretic (1 liter of urine output = 1 Kg weight lost) Treatment • Procedures • • • • • Cardioversion Ablation Cardiac resynchronization therapy (CRT) Implantable cardioverter defibrillator (ICD) Transplant Caring for the HF Patient • Assess • Teach/Coach Self Management • Advocate Self Management for HF •Assess ability to self manage • Self Care of Heart Failure Index • European Heart Failure Selfcare Behavior Scale Self Management for HF • Assess ability to self manage • Self Care of Heart Failure Index • European Heart Failure Self-care Behavior Scale • Medication management • Daily monitoring for signs/symptoms • Adherence to a low sodium diet • Routine exercise Self Management: Meds Obtaining initial and refill prescriptions Incorporating meds into daily routine Adhering to the daily medication schedule Understanding and implementing prescription changes • Recognizing common side effects of medications • Managing changes of routine (travel, illness) • • • • Patient Medication Instruction • Take each medication each day at the times indicated by using a system (list, pill box, etc) • Do not allow prescriptions to expire of bottels to become empty before refilling • Use same pharmacy each time • Bring all medications to each doctor’s visit • Contact their doctor immediately if they feel they are having side effects from medications (rather than stopping them without telling anyone). Medication Management Skills • Know which pill is their diuretic • Know how to change the dose of the diuretic according to the HF action plan • Be able to carry out any additional changes that should accompany diuretic dosage changes • i.e. need for earlier refills, addition of potassium supplementation Daily Monitoring of Signs/Symptoms Daily Weights • Use scale with large enough print to be readily visible • Use a scale that is big enough for the patient to stand on easily • Use a scale that is easy to “zero,” such as a digital scale • Weigh themselves at the same time every morning • After urinating but before eating or drinking • Before getting dressed or in the same amount of clothing each day Heart Failure Signs • • • • • • • Edema/swelling Ankle/leg edema Palpitations Abdominal edema Irregular pulse Sudden weight gain Change in urine output compared to normal • Weight loss • Low blood pressure or orthostatic blood pressure • Heart rate <60/min or >120/min • Cool, pale or mottled skin Heart Failure Symptoms Shortness of breath Exercise intolerance Orthopnea Profound fatigue with exertion or generalized weakness • Dizziness/lightheadedness • Nausea/vomiting: diarrhea or loss of appetite • • • • • Paroxysmal nocturnal dyspnea • Restlessness, confusion or fainting • Right-sided abdominal fullness, discomfort or tenderness • Severe cough • Chest pain • Wheezing Daily Monitoring of Signs/Symptoms • Record the results in a log book or other permanent record (calendar) • May be telemonitored • Compare results to previous day and to previous week • Know their target weight • 2 to 5 lb. weight gain in one week, diet/medications changes should be made • >5 lb. weight gain in one week requires immediate call to physician/nurse Daily Monitoring of Signs/Symptoms Daily Checks for Edema • Examine their legs each day for swelling or an increase in existing swelling • Describe how far up the leg the swelling reaches (ankle, shin, knee) or measure ankle circumference • Worsening edema requires diet/medication changes Daily Monitoring of Signs/Symptoms Daily Check of Symptom Severity • Monitor exercise tolerance • Using a scale ranging from no shortness of breath, SOB after moderate exertion, SOB after mild exertion, SOB at rest • Monitor their breathing at night • Using a scale ranging from no SOB lying flat, needing two or more pillows, sleeping upright or awakening with sudden SOB • Watch for dizziness or lightheadedness • Using a scale ranging from not dizzy, dizzy, dizzy for a while after standing, near syncope/syncope or fall • Less severe needs diet/medication modification • Severe symptoms needs immediate call to physician/nurse Self Management: Diet • Adherence to low sodium (2 gram) diet • No clinical trials demonstrating benefit • Patients hospitalized with acute exacerbation of HF found that excess dietary sodium to be a precipitating event in 1/5 of patients • Sodium restriction can reduce BP and enhance the response to antihypertensive drugs Patient Diet Instruction • Understand the relationship between sodium intake and edema • Know that salt and “sodium” are the same • Demonstrate ability to read a nutrition label • Demonstrate ability to calculate total sodium intake in a day • Recognize “hidden” sources of salt intake Dietary Management Skills • Select low-salt foods and avoid high-salt foods, including processed meats, hot cereals, condiments • Reduce salt added during home cooking • Ask for reduced-salt meals at restaurants and avoid known sources of salt • Rinse canned goods before cooking and/or eating • Avoid instant foods and salty snacks Self Management: Exercise • Screen for absence of significant ischemia or arrhythmias using exercise testing prior to training • Generally safe for NYHA class II and • Cardiac rehabilitation program Self Management: Smoking Cessation • Current smoking independent predictor of mortality in patients with HF Self Management: Limited Alcohol • < 2 standard drinks per day or < 1 standard drink per day in women Barriers to Self Care • Inability to afford medications • Generics • Medication Assistance Programs • Good Rx • Therapy-related factors • Common adverse effects / benefits • Minimize pill quantity • Side effects (impotence, depression, incontinence) • Low health literacy • Screen patients at risk • Document learning preferences • Integrate strategies to facility health understanding Barriers to Self Care • Multimorbidity • Multiple clinicians • Confusing or conflicting recommendations • Aspiring in patient with CAD, Hx GI bleeding, and HF • Depression and anxiety • Highly prevalent in HF patients • Effects cognition, social support, motivation and engagement • Higher rates of medication nonadherence, hospitalization and mortality • Healthcare team/system factors • Clinicians unable to provide self-care education, monitoring and reinforcement • Ancillary resources unavailable • Rare reimbursement for counseling, follow-up and monitoring Promoting Effective Self Care •Knowledge •Skills •Behavior change/patient engagement Promoting Knowledge • Utilize teach-back techniques to assure patient understands the materials • Ask specific questions to ensure the patient understands the materials • Limit teaching point to no more than 3 or 4 per session • Repeat, reinforce and review teaching points at regular intervals Promoting Skill Development • Experimental teaching • have pt. read Rx label and take out correct amount of medications, calculate the amount of salt in a food product, etc. • Role playing • have pt. practice telling provider about worsening symptoms • Group sessions • allows patients to learn from the experience of other, similarly situated patients Behavior Change/Pt Engagement • Use motivational interviewing techniques • Question patients explicitly about their beliefs in disease etiology and efficacy of treatment • Engage patients in developing a plan, and in filling out a notebook or monitoring materials • Use brainstorming with patients to help them incorporate self-management into their lives: build on patient’s own experience and routines • Help patients identify one or two concrete actions they can do for each self-care • Have patients describe their self-management practices and offer feedback to improve them, rather than suggesting or imposing self-management practices Heart Failure Action Plan • Developed between patient /family and provider • Essential Discussion • Completed Early in Course • “Hope for the best and prepare for the worst” Heart Failure Action Plan • Identification of an approach to care • Hospital vs home care or hospice for example • Identification of goals • Continued interventions to maximize function or length of life versus simplifying treatment and focusing on managing symptoms • A plan to manage current interventions to achieve goals, including each medication and device • Assistance for family and care givers in delivering care • Resources for spiritual and emotional support for patient and family Heart Failure Action Plan • Developed between patient and provider • Divided into zones: • Green – STABLE state • Maintain plan as is • Yellow – WORSENING status • Additional diuretic intake • Renewed vigilance to diet and medication compliance • Orange – ACUTE EXACERBATION • Immediate call to provider • Rapid evaluation • Red – CARDIAC EMERGENCY • Call 911 Heart Failure Disease Management • Multidisciplinary disease management • • • • • • • • • • Physician Nurse Pharmacist Case Manager Exercise Specialist Dietitian Social Worker Spiritual Care Palliative Care Family End of Life Considerations • Symptom management • • • • • Treatment of HF Fatigue Dyspnea Pain Anorexia and cachexia • Emotional, spiritual, psychological and social support • ICD deactivation • Hospice care Summary All patients deserve to know… it is a terminal disease.