Ghrelin modulates baroreflex-regulation of sympathetic vasomotor
advertisement

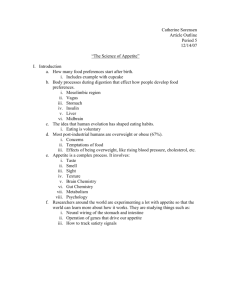
Articles in PresS. Am J Physiol Regul Integr Comp Physiol (April 4, 2012). doi:10.1152/ajpregu.00663.2011 1 Ghrelin modulates baroreflex-regulation of sympathetic vasomotor tone in healthy humans Alexander F. Krapalis1 – Jacqueline Reiter1 – Felix Machleidt1 – K. Alexander Iwen1 – Christoph Dodt2 – Hendrik Lehnert1 – Friedhelm Sayk1* 1 Dept. of Internal Medicine I, University Hospital of Schleswig-Holstein, Campus Luebeck 2 Dept. of Emergency Medicine, Bogenhausen Hospital, Munich Key terms: Ghrelin, muscle sympathetic nerve activity, baroreflex Running title: Ghrelin effects on baroreflex function Abstract: 244 words Body of text: 3822 words Number of figures: 4 Number of tables: 2 Sources of support: Grant of the German Research Foundation (DFG): SFB 654 Project B4 Disclosure summary: no conflict of interest * Correspondence to: Friedhelm Sayk, MD University of Luebeck Dept. of Internal Medicine I Ratzeburger Allee 160 D-23538 Luebeck Germany Phone: +49 451 500 6481 Fax: +45 451 500 2099 Email: friedhelm.sayk@uk-sh.de Copyright © 2012 by the American Physiological Society. 2 Abstract Ghrelin, a neuropeptide originally known for its growth hormone-releasing and orexigenic properties, exerts important pleiotropic effects on the cardiovascular system. Growing evidence suggests that these effects are mediated by the sympathetic nervous system. The present study aimed at elucidating the acute effect of ghrelin on sympathetic outflow to the muscle vascular bed (MSNA) and on baroreflex-mediated arterial blood pressure (BP) regulation in healthy humans. In a randomized double-blind cross-over design 12 lean young men were treated with a single dose of either ghrelin 2 µg/kg i.v. or placebo (isotonic saline). MSNA, heart rate (HR) and BP were recorded continuously from 30 minutes before until 90 minutes after substance administration. Sensitivity of arterial baroreflex was repeatedly tested by injection of vasoactive substances based on the modified Oxford protocol. Early, i.e. during the initial 30 minutes after ghrelin injection BP significantly decreased together with a transient increase of MSNA and HR. In the course of the experiment (>30 minutes) BP approached placebo level while MSNA and HR were significantly lower compared to placebo. The sensitivity of vascular arterial baroreflex significantly increased at 30-60 minutes after ghrelin i.v. compared to placebo, while HR response to vasoactive drugs was unaltered. Our findings suggest two distinct phases of ghrelin action: In the immediate phase BP is decreased presumably due to its vasodilating effects which trigger baroreflex-mediated counter-regulation with increases of HR and MSNA. In the delayed phase central nervous sympathetic activity is suppressed, accompanied by an increase of baroreflex-sensitivity. 3 Introduction Ghrelin is a peptide hormone mainly secreted from the stomach and small intestine with rapidly expanding experimental and clinical relevance. Although its growth-hormone (GH) secretagogue and energy-homeostatic properties are rather well characterized (14; 15), the effects of ghrelin on sympathetic nervous regulation of cardiovascular function are largely unexplored. The potential therapeutic use of ghrelin (3), its analogues and antagonists highlights the importance of further understanding its physiology. Thus, ghrelin proved beneficial for the treatment of cachexia due to malignancy (6), chronic heart failure (22) or COPD (19). Moreover, cardioprotective and anti-inflammatory properties were proclaimed in experimental models of myocardial infarction (26; 27), inflammatory bowel disease (7) and sepsis (35) . Previous results from human (20; 21) and animal studies (18; 26; 27) strongly suggest that ghrelin acts at central nervous baroreflex centers to reduce sympathetic activity, thereby decreasing blood pressure (BP). On the other side, ghrelin has specific binding sites within the peripheral vasculature (31) and was suggested to additionally exert direct vasodilating effects. Recently Lambert et al. observed a blood pressure (BP) decreasing effect of continuous intravenous infusion of ghrelin for one hour in human volunteers (16). This BP drop was combined with a significant increase of vasoconstrictive sympathetic outflow to the muscle vascular bed to counteract hypotension. Heart rate, however, remained unchanged compared to placebo, and sympathetic and hemodynamic responses to mental stress were blunted suggesting a combination of peripheral vasodilating and central sympathoneural effects of ghrelin. Our present placebo-controlled study aims at elucidating the effects of ghrelin on sympathetic nervous BP control in healthy humans. We hypothesize that 1) Ghrelin centrally decreases muscle sympathetic nerve activity (MSNA) and BP and that 2) Ghrelin modulates the sensitivity of baroreflex loops. Given the pulsatile nature of physiologic ghrelin secretion (4), we choose a placebo-controlled experimental design in which the effects of a single dose of ghrelin i.v. on MSNA, as well as hemodynamic and endocrine parameters were evaluated. Methods Subjects Twelve healthy lean male volunteers (BMI 20-25 kg/m2), aged between 22 and 30 years participated in the experiments. Participants were non-smokers and free of any medication. They were asked to abstain from alcohol and caffeinated beverages for 24 h and to have their last meal 4 in the evening prior to the experiments. In a randomized double-blind placebo-controlled crossover design, subjects either received a bolus of human ghrelin or isotonic saline. The study was conducted on two experimental days, i.e. ghrelin or placebo, separated by at least one week. Each subject was assigned to a sequence of experiments randomly. The study was approved by the local ethics committee and all participants gave their written informed consent. Experimental setting Experiments were performed in our neurophysiological laboratory starting at 7:30 a.m. and lasting until 12:30 p.m. Participants were investigated in a comfortable supine position and equipped for continuous ECG- and BP monitoring (Finometer, Finapres Medical Systems, Amsterdam, Netherlands). In addition BP was measured oscillometrically (Vital Signs Monitor 300, Welch Allyn, Skaneateles Falls, NY), and Finometer BP was calibrated according to the oscillometric readings. An intravenous cannula was inserted into an antecubital vein for repeated blood sampling. A second cannula was placed into the antecubital vein of the opposite arm for bolus administration of either ghrelin (2 µg/kg body wt, Clinalfa basic, Bachem, Bubendorf, Switzerland) (19; 22) or isotonic saline (placebo), as well as application of vasoactive substances for baroreflex testing. The respective substance was prepared by a team member not involved in the current session in a lab room apart and was provided in a neutral syringe. Microneurographic Recordings MSNA was recorded from the peroneal nerve using tungsten microelectrodes as reported previously (8) . In brief, the recording electrode was percutaneously inserted into a sympathetic fascicle of the peroneal muscle nerve. A reference electrode was positioned subcutaneously at a distance of 2 to 3 cm. Signals were amplified, filtered, and passed through an amplitude discriminator to obtain a mean voltage display of the multiunit nerve activity. Technical details and evidence that the recorded activity is of sympathetic origin have been published before (33). Analog curves of all parameters (MSNA neurogram, ECG, respiration movements, finometer BP) were digitized online and stored on a computer disk for subsequent computer analysis (PowerLab, ADInstruments, Colorado Springs, CO). Experimental protocol Recordings of hemodynamic parameters and MSNA were started about 30 min. (t -30 min) prior to the bolus injection of either ghrelin or isotonic saline (t +0 min) and were continued throughout the experiment. To determine the baroreflex setpoint MSNA, BP and heart rate (HR) were repeatedly measured during 5-10 minute periods of unaffected rest (baseline) according to 5 the protocol presented in Figure 1. In brief, the first baseline period was timed before injection of the test substance (10 minute period starting at t -25 min, pre-injection baseline). Similar recording periods of baseline MSNA, BP and HR were placed immediately (t +2 and t +7 min, early post-injection baseline 1 and 2) and later after administration of the respective test substance (t +85 min, delayed post-injection baseline). In order to document constant MSNA recording quality, microelectrodes remained in an intraneural position during the entire experiment. Subjective sensations were repeatedly assessed with a simple questionnaire. Baroreflex assessment Additionally, baroreflex sensitivity was assessed using a novel simplified approach combining the steady-state vasoactive-drug protocol used by our group before (24) with the modified Oxford protocol (MOP) (23). In brief, each cycle of baroreflex assessment consisted of 3 parts: 1) a brief resting period, followed by 2) an i.v. bolus of 150µg sodium-nitroprusside, a shortacting direct vasodilator, and 3) an i.v. bolus of 150µg phenylephrine, a short-acting vasoconstrictor, 60 seconds later. Cycles for pharmacologic baroreflex assessment were performed before (t – 5 min) and after administration of the test substance (t + 15 min, t + 35 min and t + 65 min; see Figure 1, MOP 1-4). Biochemistry Blood samples were taken at t -10 min, t +10 min, t +30 min, t +60 min and at the end of the experiment (t +110 min). They were centrifuged and stored at -80°C for analysis of ghrelin (total ghrelin RIA Kit, Millipore, Billerica, MA), renin (renin III generation, Cisbio, Codolet, France), catecholamines (HPLC, Chromsystems, Munich, Germany), GH, ACTH, cortisol (all IMMULITE, Siemens, Llanberis, United Kingdom) and Copeptin (Thermo Fisher Scientific BRAHMS GmbH, Henningsdorf, Germany). Data analysis Sympathetic bursts were visually identified by inspecting the mean voltage neurogram, and MSNA was quantified with the aid of analytical software that also analyzed heart rate from the ECG (Chart 5.02, ADInstruments). A recording was considered suitable for analysis when the signal-to-noise ratio was >3. Additionally, bursts were controlled for the coupling to the cardiac cycle, typically found at sinusrhythm. Moreover, recording quality was scrutinized by comparison of the burst characteristics (morphology, amplitude) during sympathoexcitatory apnoea at both, the pre- and delayed post-injection phase – a manoeuvre which regularly stimulates MSNA even in sympathosuppressive conditions. A difficulty for comparison of 6 intraneural MSNA recordings retrieved at different experimental days is the fact that burstamplitude and area-under-curve are critically affected by the position of the electrode in relation to the sympathetic fascicle and might considerably differ between sessions. Burst rate (number of bursts/min.) at rest, in contrast, is highly reproducible over long periods in healthy subjects. Therefore, nerve activity was expressed as burst rate (number of bursts/min). All recordings were analyzed by the same observer, who was unaware of the substance (ghrelin or placebo) administered. Due to physiological considerations discussed in detail below, we distinguished the preinjection phase from an immediate (< 30 minutes) and a delayed (> 30 minutes) response phase after injection of ghrelin or placebo, respectively. Previous studies have shown distinct hemodynamic and endocrine changes within this time scale (20). BP, HR and MSNA were analyzed during pre-injection baseline (t -25 min), immediate (t +2 min and t +7 min) and delayed post-injection baseline (t +85 min). For assessment of baroreflex sensitivity the modified Oxford protocol (MOP) cycles were analyzed. MSNA, HR and mean arterial BP were measured for 60 second intervals 1) before injection of vasoactive substances, 2) from 30 to 90 seconds after bolus injection of 150 µg sodium-nitroprusside and 3) from 90 to 150 seconds after injection of 150 µg phenylephrine. For each cycle of measurement BP was plotted against MSNA or HR (vascular or cardial baroreflex, respectively), and a linear regression analysis was performed using the ordinary leastsquares method. A cycle of measurement was accepted if the coefficient of determination R2 was equal to or greater than 0.7. Resulting slopes of model linear functions were used to characterize baroreflex sensitivity and subjected to further statistical analysis. An example of MSNA recording during baseline as well as during baroreflex challenge with nitroprusside and phenylephrine are shown in Figure 2. Statistics Data are expressed as means +/- SEM. Statistical analysis of data was based on analysis of variance (ANOVA) with group factor treatment (ghrelin vs. placebo) and the repeated-measures factor time. A Greenhouse-Geisser corrected P value < 0.05 was considered significant. Post hoc testing was performed using paired Student´s T-test as appropriate (PASW Statistics 18). In addition to comparison between both conditions, i.e. ghrelin vs. placebo, within-condition comparison was calculated for the recording periods defined above, prior to vs. after respective bolus injection. Sample size calculations (power and effect size) were performed with G*Power 3.1.3 (Franz Faul, University of Kiel, Germany). 7 Results Clinical observations Intravenous administration of ghrelin was generally well tolerated. Under ghrelin condition, subjects reported sensations of hunger (n=6), flush (n=3), dizziness (n=2), sleepiness (n=3) and borborygmi (n=4). Sweating occurred in 5 subjects. Subjects’ ratings of ‘physical discomfort’ were transiently increased during the early phase after ghrelin injection. All ghrelin-related sensations resolved within the first 30 minutes after administration, except hunger, which persisted for the whole experiment. Under placebo condition, one subject reported sleepiness. Hormonal response to ghrelin In the placebo condition plasma levels of total ghrelin remained at pre-injection level throughout the experiment. Following ghrelin injection, however, plasma levels increased about 18-fold after 10 minutes, followed by an exponential decline. As expected, growth hormone (GH) significantly increased with short latency (peak at t +30 min, 15-fold compared to preinjection), while a slight decrease of GH was observed under placebo. In accordance with previous studies (20) administration of ghrelin was answered by a highly significant increase in ACTH, cortisol and epinephrine, but not norepinephrine. Moreover, levels of copeptin, an unspecific marker of circulatory stress, were increased and plasma renin tended to be higher early after ghrelin i.v. (peak at t +30 min). (See table 2.) Blood pressure, heart rate and MSNA BP and HR were analyzed for all 12 participants while MSNA data was complete for 10, but incomplete for two subjects due to loss of electrode position from the sympathetic fascicle at delayed ghrelin phase. Results are reported in detail in table 1 and figure 3 A)-C). For the whole experiment, ANOVA for interaction between group factor ghrelin/placebo and time of measurement was significant concerning MSNA (P=0.037) and HR (P<0.001). It indicated a strong trend regarding BP (P=0.057). In detail, resting BP, HR and MSNA did not differ between both conditions during the preinjection period (t -25 min, t -5 min). After ghrelin injection (t +15 min and subsequent), mean arterial BP was persistently decreased as compared to the pre-injection period. Compared to the corresponding placebo data, BP was significantly lower early after ghrelin (t +7 to +35 min; P=0.014, ANOVA for factor ghrelin/placebo) but approached placebo level later (t +65 min and subsequent). HR transiently increased immediately after ghrelin administration (t +2 min: 8 P=0.018 compared to pre-injection (t -25 min); P=0.117 compared to placebo, T-test). In the delayed post-injection phase (t +35 min and subsequent) HR significantly decreased after ghrelin, but increased in the placebo condition compared to pre-injection data. Therefore HR was significantly lower after ghrelin as compared to placebo in the delayed phase (P=0.043, ANOVA for factor ghrelin/placebo; Fig. 3 B). MSNA significantly increased immediately after the ghrelin bolus, but not after placebo compared to pre-injection levels (t +2 min vs. t -25 min: P=0.005, TTest). Though this immediate increase persisted for more than 15 minutes it did not reach significance as compared to the corresponding placebo data (t +2 min: P=0.088, T-test), and was less than expected with regard to the prevailing BP decrease. After ghrelin, during the delayed phase, MSNA had returned to pre-injection levels until the end of the experiment (t +85 min). After placebo, in contrast, MSNA remained constant in the immediate post-injection phase, but increased during the later periods to become significantly higher at t +85 min compared to ghrelin (28.4 vs. 32.7 bpm, P=0.047, T-test) or to placebo pre-injection levels (P=0.016, T-test). Baroreflex To identify differential effects on baroreflex performance, vasoactive substances were administered (MOP cycles) and slopes of baroreflex were derived from linear regression as illustrated in Figure 4. Pre-injection (t –5 min) slopes were comparable under both conditions. Due to poor correlation immediate post-injection phase data (t +15 min) did not meet the statistical requirements mentioned above. In the delayed post-injection phase (t +35 min and t +65 min, pooled data) sensitivity of MSNA-related vascular baroreflex showed a significant increase following ghrelin i.v. (mean slope -2.25 vs. -1.66 after ghrelin or placebo i.v., respectively; ANOVA: P=0.036 for interaction between factors ghrelin/placebo and time of measurement, N=10). Statistical analysis of sensitivity of HR-related cardiac baroreflex did not show any significant difference between ghrelin and placebo condition (ANOVA: n.s.; N=8). However, in contrast to MSNA-related baroreflex data, this aspect was underpowered according to post hoc power analysis. 9 Discussion Immediate and delayed phase of ghrelin action In the present study two distinct phases of ghrelin action could be distinguished over the experimental time course: immediately after ghrelin injection, a decrease of BP combined with an increase of MSNA and a transient increase of HR was observed (immediate ghrelin phase). After 30 minutes, MSNA had returned to placebo level while BP and HR were decreased. Finally, blood pressure was on placebo level combined with a decreased HR and a MSNA which was significantly lower compared to placebo (delayed ghrelin phase). According to the broadly accepted baroreflex paradigm a reduced BP should trigger the arterial baroreflex to increase sympathetic outflow towards the heart and vasculature in order to restore the preset BP level. Vice versa a BP above the setpoint level should be followed by a decrease of MSNA and HR, unless the setpoint itself was altered (5; 11). Therefore, our findings in the immediate ghrelin phase can be explained by a direct vasodilation leading to an immediate blood pressure decrease which results in a compensatory increase of MSNA and a short transient increase of HR mediated by the arterial baroreflex. Ghrelin is known to decrease systemic vascular resistance (21), which might result from NO-dependent (36) or –independent (34) vasodilatory mechanisms. However, the reflex-increase of resting MSNA at this phase was modest with regard to the significant BP decrease (e.g. t +15 min; s. Table 1). In previous studies, NO-related BP decreases of similar degree yielded much stronger sympathoexcitation (25; 30). This observation might indicate a rapid central sympatholytic ghrelin effect already during the immediate phase. During the delayed ghrelin phase, at first MSNA remained on placebo level and HR was decreased during a state of reduced BP (t +35 min). Subsequently MSNA and HR were lower during a state of unchanged BP (t +65 min, t +85 min) compared to placebo. Therefore, one potential explanation might involve a shift of the setpoint of sympathetic BP control towards lower BP levels during the delayed ghrelin phase. This interpretation is in accordance with previous findings concerning interactions of ghrelin with the sympathetic nervous system (SNS). Thus, in healthy men ghrelin was found to decrease mean arterial BP without any significant change of HR but with an increase of cardiac index (20). In patients with chronic heart failure ghrelin i.v. twice a day for three weeks resulted in a significant decrease of plasma norepinephrine, a global marker of overall SNS activity (22). Moreover, the intracerebroventricular administration of ghrelin decreased BP, HR and renal SNS activity and increased the sensitivity of baroreflex in conscious rabbits (18). Ghrelin i.v. suppressed cardiac 10 SNS activation following myocardial infarction in rats (26; 27) and suppressed sympathetically mediated cytokine release in experimental sepsis (35). Alternatively, Ghrelin might have blunted stress-induced sympathetic feed-forward commands in contrast to placebo. In the present study, MSNA increased in the course of time under placebo condition. Such increases of sympathetic activity are a well-known phenomenon during recording protocols of long duration and are commonly explained as reaction to urinary bladder filling or discomfort due to restricted body position – though subjective ratings for these categories were not increased in the present study at the end of the placebo condition (25). Ghrelin in contrast, finally (t +85 min) resulted in an unchanged BP combined with a significantly lower MSNA and HR compared to placebo. MSNA is a direct measure of central nervous sympathetic outflow. Therefore our findings might indicate that ghrelin prevented stressrelated sympathoactivation. This is in accordance with recent findings in humans showing mitigated response to mental stress under ghrelin (16) – an aspect that may have distinct clinical implication on individual hypertensive pressor responses. Microneurographic approaches to assess baroreflex gain represent a simplified input-output relationship of blood pressure and MSNA, which may potentially be modulated by ghrelin independently from its mere baroreflex effects. In accordance with previous findings, we observed that following ghrelin plasma levels of various hemodynamically active hormones like cortisol, copeptin and epinephrine were strongly increased, transiently (20). These increases can be attributed to the presence of specific GH-secretagogue binding sites within the hypothalamus, pituitary gland and adrenal medulla (10; 16). In contrast to epinephrine, norepinephrine was not elevated – a pattern similarly observed even after injection of much higher ghrelin doses of 10 µg/kg (20). When injected repeatedly over 3 weeks at doses comparable to our study ghrelin even decreased plasma norepinephrine levels (19). Plasma norepinephrine originates from multiple sympathetic branches by spill-over. Therefore, this rather crude marker indicates that overall sympathetic activity was not increased in our study, corroborating the above mentioned MSNA-findings. Blood pressure resetting and Sensitivity of baroreflex In the present study, baroreflex assessment yielded a steepening of the MSNA-BP slope at 35 and 65 minutes after ghrelin administration. Thus, ghrelin i.v. increased the sensitivity of arterial baroreflex. In consistency, a similar effect was found for renal sympathetic nerve activity in an animal model (18). This finding provides additional support for the hypothesis that peripheral ghrelin modulates circulation control at central nervous levels including hypothalamic and 11 brainstem centers (17). There is evidence that ghrelin can pass the blood brain barrier (2). These mechanisms, however, warrant further investigation. Ghrelin is well-known for its GH-secretagogue function. Since in states of GH-deficiency an increased sympathetic outflow was described (29), whereas GH-replacement therapy led to a decrease of MSNA (28), one might hypothesize that GH should inhibit sympathetic outflow. Moreover, ghrelin i.v. increases cortisol plasma levels. Glucocorticoids have been shown to acutely decrease MSNA (8). Hence, as an alternative to the mechanism mentioned above, the delayed decrease of sympathetic outflow observed in our study following ghrelin i.v. could be mediated by GH or cortisol. Recently, Lambert et al. found that the continuous intravenous infusion of ghrelin for one hour significantly decreased BP compared to preceding or subsequent placebo infusion (16). This decrease was accompanied by a modest but significant increase of MSNA indicating a baroreflex-mediated sympathetic counterregulation. The experimental bolus design of the present study differs substantially from the continuous infusion model chosen by Lambert et al. Moreover, conducting the ghrelin and placebo experiment on separate days reduced the effects of substance interaction in our study. Under physiological conditions, ghrelin is secreted following a pulsatile pattern (4) and inactivated by deacylation with a halflife of only about 9-13 minutes (1). In the present study the bolus application of ghrelin produced two distinct phases. Presumably, in Lambert’s experiment the physiologic mechanisms are comparable to those prevailing during the immediate phase of our study. Absence of a significant increase of HR as well as the blunted sympathoexcitation in response to stressful stimuli described by Lambert et al. suggested an additional central nervous effect of ghrelin as proposed for the delayed phase of the present study. Clinical implications We found new evidence in human subjects that high circulating levels of the gut-hormone ghrelin can decrease both BP and SNS activity while increasing baroreflex sensitivity. Low ghrelin levels, in contrast, as found in obese subjects (32), might contribute to obesity related SNS activation (9), a hallmark of obesity hypertension. On the other hand, physiologically high ghrelin levels during slow wave sleep might play a role in nocturnal BP dipping and resetting of the baroreflex during nighttime sleep (24). Moreover, ghrelin therapy was beneficial in humans suffering from chronic heart failure (22) or pulmonary cachexia (19), i.e. conditions strongly associated with chronically increased SNS activity. In these studies ghrelin was injected intravenously twice per day for 3 weeks at doses equivalent to our study (2 µg/kg). The 12 therapeutic ghrelin effect might at least partially be mediated by central nervous sympathoinhibition. Limitations Our experimental model focussed on the acute effects of ghrelin on baroreflex-mediated BP control. Recordings of MSNA, being the most important vasoconstrictive stimulus, provide a direct measure of sympathetic outflow to resistance arteries. This allows us to draw very specific conclusions concerning this branch of the baroreflex arch, whereas other aspects, particularly concerning cardiac baroreflex function, cannot be answered with similar specificity. Though the number of subjects was small in our study, the solid placebo-controlled design permitting within subject comparison is an important strength of our study. Statistical tests were sufficiently powered to detect an alteration of sympathetic baroreflex function, whereas analysis of the cardiac baroreflex-slope was underpowered. The baroreflex-test chosen in our study represents a simplified method providing basic insight. Other more sophisticated dynamic techniques might provide more detailed information, but will not alter our key findings (12; 13). Perspective Our study suggests a two-phase model of ghrelin effect on sympathetic cardiovascular control: an immediate phase of direct peripheral vasodilation with baroreflex-mediated sympathoactivation, followed by a delayed neurohumoral phase. The latter was characterized by decreased vasoconstrictive sympathetic activity combined with increased baroreflex sensitivity as compared to placebo. Our results could offer a new understanding of seemingly conflicting findings in previous studies. To further elucidate long-lasting ghrelin-baroreflex interactions, experimental models of chronic ghrelin administration are desirable. We would expect that under this regimen an even more distinct central nervous inhibition of vasoconstrictive SNS activity might occur. Subsequently it would be most interesting to investigate the potentially beneficial effects of ghrelin on MSNA under pathological conditions associated with permanently increased sympathetic activity, like chronic heart failure, liver cirrhosis, morbid obesity or sleep disordered breathing. Acknowledgements We thank Martina Grohs and Heidi Ruf for their excellent technical assistance. 13 Source of funding This study was financially supported by a Grant of the Deutsche Forschungsgemeinschaft (SFB 654/B4) without influencing the study design, data collection, analysis or interpretation. Reference List 1. Akamizu T, Takaya K, Irako T, Hosoda H, Teramukai S, Matsuyama A, Tada H, Miura K, Shimizu A, Fukushima M, Yokode M, Tanaka K and Kangawa K. Pharmacokinetics, safety, and endocrine and appetite effects of ghrelin administration in young healthy subjects. Eur J Endocrinol 150: 447-455, 2004. 2. Banks WA, Tschop M, Robinson SM and Heiman ML. Extent and direction of ghrelin transport across the blood-brain barrier is determined by its unique primary structure. J Pharmacol Exp Ther 302: 822-827, 2002. 3. Cheyuo C, Jacob A and Wang P. Ghrelin-mediated Sympathoinhibition and Suppression of Inflammation in Sepsis. Am J Physiol Endocrinol Metab 2011. 4. Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE and Weigle DS. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 50: 1714-1719, 2001. 5. Dampney RA, Coleman MJ, Fontes MA, Hirooka Y, Horiuchi J, Li YW, Polson JW, Potts PD and Tagawa T. Central mechanisms underlying short- and long-term regulation of the cardiovascular system. Clin Exp Pharmacol Physiol 29: 261-268, 2002. 6. DeBoer MD. Emergence of ghrelin as a treatment for cachexia syndromes. Nutrition 24: 806-814, 2008. 7. DeBoer MD. Use of ghrelin as a treatment for inflammatory bowel disease: mechanistic considerations. Int J Pept 2011: 189242, 2011. 8. Dodt C, Keyser B, Molle M, Fehm HL and Elam M. Acute suppression of muscle sympathetic nerve activity by hydrocortisone in humans. Hypertension 35: 758-763, 2000. 14 9. Esler M, Straznicky N, Eikelis N, Masuo K, Lambert G and Lambert E. Mechanisms of sympathetic activation in obesity-related hypertension. Hypertension 48: 787-796, 2006. 10. Ghigo E, Arvat E, Broglio F, Giordano R, Gianotti L, Muccioli G, Papotti M, Graziani A, Bisi G, Deghenghi R and Camanni F. Endocrine and non-endocrine activities of growth hormone secretagogues in humans. Horm Res 51 Suppl 3: 9-15, 1999. 11. Guyenet PG. The sympathetic control of blood pressure. Nat Rev Neurosci 7: 335-346, 2006. 12. Hart EC, Joyner MJ, Wallin BG, Karlsson T, Curry TB and Charkoudian N. Baroreflex control of muscle sympathetic nerve activity: a nonpharmacological measure of baroreflex sensitivity. Am J Physiol (Heart Circ Physiol ) 298: H816-H822, 2010. 13. Kienbaum P, Karlsson T, Sverrisdottir YB, Elam M and Wallin BG. Two sites for modulation of human sympathetic activity by arterial baroreceptors? J Physiol 531: 861869, 2001. 14. Kojima M and Kangawa K. Ghrelin: structure and function. Physiol Rev 85: 495-522, 2005. 15. Kojima M and Kangawa K. Ghrelin: more than endogenous growth hormone secretagogue. Ann N Y Acad Sci 1200: 140-148, 2010. 16. Lambert E, Lambert G, Ika-Sari C, Dawood T, Lee K, Chopra R, Straznicky N, Eikelis N, Drew S, Tilbrook A, Dixon J, Esler M and Schlaich MP. Ghrelin Modulates Sympathetic Nervous System Activity and Stress Response in Lean and Overweight Men. Hypertension 2011. 17. Lin Y, Matsumura K, Fukuhara M, Kagiyama S, Fujii K and Iida M. Ghrelin acts at the nucleus of the solitary tract to decrease arterial pressure in rats. Hypertension 43: 977982, 2004. 18. Matsumura K, Tsuchihashi T, Fujii K, Abe I and Iida M. Central ghrelin modulates sympathetic activity in conscious rabbits. Hypertension 40: 694-699, 2002. 15 19. Nagaya N, Itoh T, Murakami S, Oya H, Uematsu M, Miyatake K and Kangawa K. Treatment of cachexia with ghrelin in patients with COPD. Chest 128: 1187-1193, 2005. 20. Nagaya N, Kojima M, Uematsu M, Yamagishi M, Hosoda H, Oya H, Hayashi Y and Kangawa K. Hemodynamic and hormonal effects of human ghrelin in healthy volunteers. Am J Physiol Regul Integr Comp Physiol 280: R1483-R1487, 2001. 21. Nagaya N, Miyatake K, Uematsu M, Oya H, Shimizu W, Hosoda H, Kojima M, Nakanishi N, Mori H and Kangawa K. Hemodynamic, renal, and hormonal effects of ghrelin infusion in patients with chronic heart failure. J Clin Endocrinol Metab 86: 58545859, 2001. 22. Nagaya N, Moriya J, Yasumura Y, Uematsu M, Ono F, Shimizu W, Ueno K, Kitakaze M, Miyatake K and Kangawa K. Effects of ghrelin administration on left ventricular function, exercise capacity, and muscle wasting in patients with chronic heart failure. Circulation 110: 3674-3679, 2004. 23. Rudas L, Crossman AA, Morillo CA, Halliwill JR, Tahvanainen KU, Kuusela TA and Eckberg DL. Human sympathetic and vagal baroreflex responses to sequential nitroprusside and phenylephrine. Am J Physiol 276: H1691-H1698, 1999. 24. Sayk F, Becker C, Teckentrup C, Fehm HL, Struck J, Wellhoener JP and Dodt C. To dip or not to dip: on the physiology of blood pressure decrease during nocturnal sleep in healthy humans. Hypertension 49: 1070-1076, 2007. 25. Sayk F, Vietheer A, Schaaf B, Wellhoener P, Weitz G, Lehnert H and Dodt C. Endotoxemia causes central downregulation of sympathetic vasomotor tone in healthy humans. Am J Physiol Regul Integr Comp Physiol 295: R891-R898, 2008. 26. Schwenke DO, Tokudome T, Kishimoto I, Horio T, Shirai M, Cragg PA and Kangawa K. Early ghrelin treatment after myocardial infarction prevents an increase in cardiac sympathetic tone and reduces mortality. Endocrinology 149: 5172-5176, 2008. 16 27. Soeki T, Kishimoto I, Schwenke DO, Tokudome T, Horio T, Yoshida M, Hosoda H and Kangawa K. Ghrelin suppresses cardiac sympathetic activity and prevents early left ventricular remodeling in rats with myocardial infarction. Am J Physiol Heart Circ Physiol 294: H426-H432, 2008. 28. Sverrisdottir YB, Elam M, Caidahl K, Soderling AS, Herlitz H and Johannsson G. The effect of growth hormone (GH) replacement therapy on sympathetic nerve hyperactivity in hypopituitary adults: a double-blind, placebo-controlled, crossover, shortterm trial followed by long-term open GH replacement in hypopituitary adults. J Hypertens 21: 1905-1914, 2003. 29. Sverrisdottir YB, Elam M, Herlitz H, Bengtsson BA and Johannsson G. Intense sympathetic nerve activity in adults with hypopituitarism and untreated growth hormone deficiency. J Clin Endocrinol Metab 83: 1881-1885, 1998. 30. Tank J, Diederich A, Szchech E, Luft FC and Jordan J. Baroreflex Regulation of Heart Rate and Sympathetic Vasomotor Tone in Women and Men. Hypertension 45: 1159-1164, 2005. 31. Tesauro M, Schinzari F, Caramanti M, Lauro R and Cardillo C. Cardiovascular and metabolic effects of ghrelin. Curr Diabetes Rev 6: 228-235, 2010. 32. Tschop M, Weyer C, Tataranni PA, Devanarayan V, Ravussin E and Heiman ML. Circulating ghrelin levels are decreased in human obesity. Diabetes 50: 707-709, 2001. 33. Vallbo AB, Hagbarth KE, Torebjork HE and Wallin BG. Somatosensory, proprioceptive, and sympathetic activity in human peripheral nerves. Physiol Rev 59: 919957, 1979. 34. Wiley KE and Davenport AP. Comparison of vasodilators in human internal mammary artery: ghrelin is a potent physiological antagonist of endothelin-1. Br J Pharmacol 136: 1146-1152, 2002. 17 35. Wu R, Zhou M, Das P, Dong W, Ji Y, Yang D, Miksa M, Zhang F, Ravikumar TS and Wang P. Ghrelin inhibits sympathetic nervous activity in sepsis. Am J Physiol Endocrinol Metab 293: E1697-E1702, 2007. 36. Xu X, Jhun BS, Ha CH and Jin ZG. Molecular mechanisms of ghrelin-mediated endothelial nitric oxide synthase activation. Endocrinology 149: 4183-4192, 2008. Legends Table 1. Circulation parameters and MSNA. For the whole course of the experiment, ANOVA for interaction between group factor ghrelin/placebo and time of measurement was significant concerning MSNA (P=0.037) and heart rate (P<0.001), and indicated a strong trend regarding BP (P=0.057). Ghrelin/placebo i.v. bolus injection at time +0 min. Data are means +/- SEM. * = P<0.05 for post-hoc comparison between ghrelin and placebo, † = P<0.05, †† = P<0.01 for comparison between pre-injection and respective post-injection data (T-test). Table 2. Hormone levels before and after bolus injection of ghrelin/placebo i.v. (t +0 min) in 12 subjects (Copeptin: n=9, t +110 min n=7). Data are means +/- SEM. * = P<0.05, ** = P<0.01 for comparison between ghrelin and placebo, † = P<0.05, †† = P<0.01 for comparison between pre-injection and respective post-injection data (T-test). Figure 1. Protocol of the present study. Hemodynamic parameters and muscle sympathetic nerve activity (MSNA) were measured before (pre-injection), as well as immediately and delayed after injection of ghrelin i.v. or placebo (post-injection). Baroreflex performance was assessed by vasoactive-substance mediated modulation of blood pressure (modified Oxford protocol, MOP). Additionally, biochemical studies were conducted. Figure 2. Exemplary combined recording of MSNA and BP from a representative subject during A) baseline and during baroreflex challenge (modified Oxford protocol) with B) nitroprusside (NP) and C) phenylephrine (PE). Timescale represents 2 second intervals. 18 Figure 3. A) Muscle sympathetic nerve activity (MSNA), B) heart rate, and C) mean arterial blood pressure before and after intravenous bolus injection (dotted line) of either ghrelin (black symbols) or placebo (white symbols). Values are means +/- SEM. A) § = P<0.05 for interaction between group factor ghrelin/placebo and time of measurement (ANOVA, N=10); * = P<0.05 for comparison between ghrelin and placebo (T-Test); †† = P<0.01 for comparison between preinjection and respective post-injection data (T-test). B) §§ = P<0.001 for interaction between group factor ghrelin/placebo and time of measurement (ANOVA, N=12); * = P<0.05 for factor ghrelin/placebo, t +35 min to t + 85 min (ANOVA); † = P<0.05 for comparison between preinjection and respective post-injection data (T-test). C) P=0.057 for interaction between group factor ghrelin/placebo and time of measurement (ANOVA, N=12); * = P<0.05 for factor ghrelin/placebo, t +7 min to t +35 min (ANOVA). Figure 4. Slope of vascular (MSNA) arterial baroreflex performance during bolus challenges of nitroprusside and phenylephrine i.v. (modified Oxford protocol, MOP) before and after injection of ghrelin or placebo. A linear regression was performed for each individual cycle of measurement. Slopes were accepted if R2 ≥ 0.7. Post-injection data was pooled from MOP 3 and 4 (delayed phase of ghrelin action). A) Exemplary data of one individual participant. Black/white symbols: Ghrelin/placebo condition. Circles/triangles: Pre-/post-injection phase. Linear regression lines for ghrelin pre-/post-injection (dotted/solid), placebo pre-/post-injection (short/long dashes). B) Statistics for slope of baroreflex. Values are means +/- SEM; black/white circles: Ghrelin/placebo condition. * = P<0.05 for interaction between group factor ghrelin/placebo and time of measurement (ANOVA; N=10). The greater negative increment indicates the increased baroreflex sensitivity under ghrelin condition. 19 Table 1. Time (min) Ghrelin mean SEM Placebo mean SEM MSNA (bursts per minute) -25 -5 +2 +7 +15 +35 +65 +85 27.3 27.8 32.9 31.9 31.6 29.8 28.3 28.4 ± ± ± ± ± ± ± ± 3.5 3.0 3.8 †† 4.1 3.8 3.0 4.0 3.8 * 27.6 28.3 28.8 28.9 27.8 28.7 30.2 32.7 ± ± ± ± ± ± ± ± 3.7 2.7 4.1 4.0 3.2 2.9 3.9 5,2 † Heart rate (1/min) -25 -5 +2 +7 +15 +35 +65 +85 60.2 60.3 64.5 60.5 60.3 57.2 56.5 57.8 ± ± ± ± ± ± ± ± 2.2 2.2 2.6 2.2 2.4 2.0 1.9 1.9 † *, †† * 59.7 61.5 60.7 61.4 59.9 61.5 61.9 64.2 ± ± ± ± ± ± ± ± 2.2 2.5 1.9 2.2 2.1 2.4 2.0 † 2.2 †† -25 -5 +2 +7 +15 +35 +65 +85 83.9 83.5 87.3 81.7 79.8 77.7 80.8 77.7 ± ± ± ± ± ± ± ± 1.8 1.5 3.0 3.2 2.2 2.0 1.8 1.5 *, † †† † †† 83.8 85.4 85.4 87.7 85.6 84.1 82.3 79.6 ± ± ± ± ± ± ± ± 2.2 1.9 2.5 3.1 2.1 1.8 1.5 2.1 † Mean arterial pressure (mmHg) † 20 Table 2. Time (min) Ghrelin (total, pg/ml) GH (ng/ml) ACTH (pg/ml) Cortisol (µg/dl) Copeptin (pmol/l) Renin (pg/ml) Epinephrine (pg/ml) Norepinephrine (pg/ml) -5 +15 +30 +60 +110 -5 +15 +30 +60 +110 -5 +15 +30 +60 +110 -5 +15 +30 +60 +110 -5 +15 +30 +60 +110 -5 +15 +30 +60 +110 -5 +15 +30 +60 +110 -5 +15 +30 +60 +110 Ghrelin mean SEM 819.4 13449.7 7549.1 4710.8 2716.2 2.4 16.7 37.5 32.8 13.7 26.6 154.9 163.5 76.5 31.2 10.5 13.5 21.0 21.1 15.1 5.0 6.9 8.6 6.5 7.1 7.8 7.8 11.2 10.1 9.1 25.6 165.9 123.9 66.4 27.5 235.5 218.0 212.1 204.5 212.3 ± 61.8 ± 1639.8 **, †† ± 499.7 **, †† ± 247.2 **, †† ± 264.6 **, †† ± 1.3 ± 3.8 **, †† ± 1.8 **, †† ± 3.3 **, †† ± 4.1 *, † ± 2.4 ± 31.8 **, † ± 34.7 **, † ± 13.2 **, † ± 3.0 ± 1.2 ± 1.2 ± 1.1 **, †† ± 1.5 **, †† ± 1.4 ** ± 1.3 ± 1.7 †† ± 1.9 *, † ± 1.5 ± 2.2 ± 0.8 * ± 1.1 ± 2.3 ± 1.1 † ± 1.1 ± 9.1 ± 44.3 *, †† ± 21.0 **, †† ± 12.8 **, †† ± 8.3 ± 25.8 ± 23.1 ± 24.0 ± 19.0 †† ± 22.0 † Placebo mean SEM 739.8 739.2 732.6 733.5 710.9 2.2 1.0 0.7 0.3 0.2 33.0 27.8 27.3 25.3 25.6 12.4 11.2 10.5 8.9 8.7 5.7 4.7 4.5 4.1 6.2 10.3 10.0 10.2 9.8 10.2 33.8 32.1 26.6 28.0 26.3 250.4 234.4 236.4 219.3 237.5 ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± 48.2 51.6 50.2 48.7 41.1 0.9 0.5 0.3 0.1 0.1 5.5 3.5 2.8 2.5 1.9 1.2 1.2 1.1 0.8 0.8 1.2 1.0 0.8 0.8 1.9 1.3 1.2 1.2 1.1 1.1 15.5 9.9 9.4 10.7 9.3 46.8 40.3 39.9 37.8 44.1 † †† †† † † † † Figure 1. Figure 2. Modified Oxford protocol (MOP) MSNA (V) A) Baseline 2 1 BP (mmHg) 0 150 0 time 2 BP (mmHg) MSNA (V) B) NP 1 0 150 0 time 2 BP (mmHg) MSNA (V) C) PE 1 0 150 0 time Figure 3. Figure 4.