differentiating antihistamine efficacy from potency
advertisement
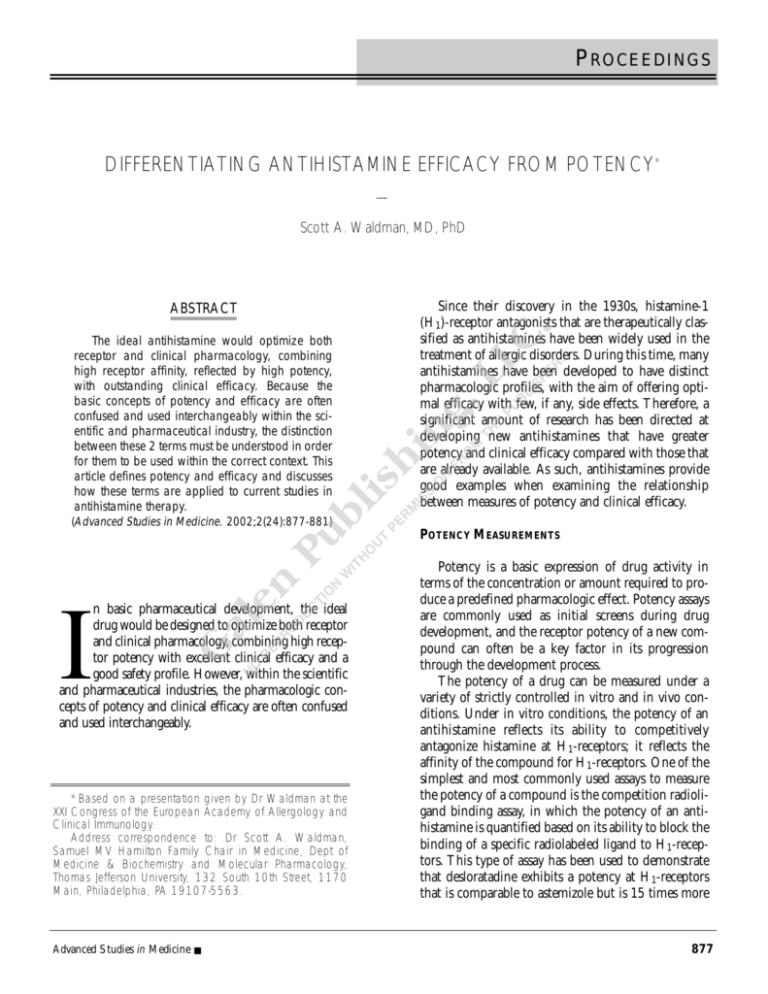
PROCEEDINGS DIFFERENTIATING ANTIHISTAMINE EFFICACY FROM POTENCY* — Scott A. Waldman, MD, PhD ABSTRACT The ideal antihistamine would optimize both receptor and clinical pharmacology, combining high receptor affinity, reflected by high potency, with outstanding clinical efficacy. Because the basic concepts of potency and efficacy are often confused and used interchangeably within the scientific and pharmaceutical industry, the distinction between these 2 terms must be understood in order for them to be used within the correct context. This article defines potency and efficacy and discusses how these terms are applied to current studies in antihistamine therapy. Since their discovery in the 1930s, histamine-1 (H1)-receptor antagonists that are therapeutically classified as antihistamines have been widely used in the treatment of allergic disorders. During this time, many antihistamines have been developed to have distinct pharmacologic profiles, with the aim of offering optimal efficacy with few, if any, side effects. Therefore, a significant amount of research has been directed at developing new antihistamines that have greater potency and clinical efficacy compared with those that are already available. As such, antihistamines provide good examples when examining the relationship between measures of potency and clinical efficacy. (Advanced Studies in Medicine. 2002;2(24):877-881) POTENCY MEASUREMENTS n basic pharmaceutical development, the ideal drug would be designed to optimize both receptor and clinical pharmacology, combining high receptor potency with excellent clinical efficacy and a good safety profile. However, within the scientific and pharmaceutical industries, the pharmacologic concepts of potency and clinical efficacy are often confused and used interchangeably. I *Based on a presentation given by Dr Waldman at the XXI Congress of the European Academy of Allergology and Clinical Immunology. Address correspondence to: Dr Scott A. Waldman, Samuel MV Hamilton Family Chair in Medicine, Dept of Medicine & Biochemistry and Molecular Pharmacology, Thomas Jefferson University, 132 South 10th Street, 1170 Main, Philadelphia, PA 19107-5563. Advanced Studies in Medicine ■ Potency is a basic expression of drug activity in terms of the concentration or amount required to produce a predefined pharmacologic effect. Potency assays are commonly used as initial screens during drug development, and the receptor potency of a new compound can often be a key factor in its progression through the development process. The potency of a drug can be measured under a variety of strictly controlled in vitro and in vivo conditions. Under in vitro conditions, the potency of an antihistamine reflects its ability to competitively antagonize histamine at H1-receptors; it reflects the affinity of the compound for H1-receptors. One of the simplest and most commonly used assays to measure the potency of a compound is the competition radioligand binding assay, in which the potency of an antihistamine is quantified based on its ability to block the binding of a specific radiolabeled ligand to H1-receptors. This type of assay has been used to demonstrate that desloratadine exhibits a potency at H1-receptors that is comparable to astemizole but is 15 times more 877 PROCEEDINGS potent than its parent molecule, loratadine. 1 However, an important consideration is that the relative potency of a compound will depend on the particular assay system and tissue type used. For example, the rank order of potency of various antihistamines in a calcium ion (Ca2+) flux assay, using Chinese hamster ovary cells transfected with H1receptors, indicated that desloratadine was more potent than chlorpheniramine.2 In contrast, comparing the potency of the same antihistamines by their ability to antagonize histamine-induced contractions of guinea pig ileum showed that chlorpheniramine was 30 times more potent than desloratadine.1 This exemplifies that in vitro potency data may vary depending on the type of assay, the conditions used, and the tissue in which potency is measured. In vivo, the potency of antihistamines reflects the relationship between dose or concentration and a targeted pathophysiologic response. For example, a popular in vivo test for antihistamine potency is the epicutaneous histamine-induced wheal and flare assay. This test assesses the potential for clinical effectiveness by measuring in vivo potency at peripheral receptors. It relies on the ability of epicutaneously injected histamine to bring about the wheal and flare, a neurovascular response that involves reflex vasodilation (flare) and local swelling caused by plasma extravasation (wheal). In this assay, the potency of an antihistamine is judged by the degree with which it suppresses the wheal and flare response. A recent wheal and flare study in healthy adult volunteers demonstrated that fexofenadine was more effective at fully inhibiting the wheal and flare responses compared with both loratadine and desloratadine, with a faster onset of action.3 Interestingly, desloratadine was not as effective at inhibiting the wheal response compared with loratadine, which is in contrast to earlier radioligand binding studies using cellular membranes where desloratadine was found to be 15 times more potent than loratadine.1 Similarly, although the radioligand binding profiles of the antihistamines astemizole, chlorpheniramine, cetirizine, and terfenadine show that astemizole and chlorpheniramine are more potent than cetirizine and terfenadine, the results of the histamine-induced wheal and flare assay show that cetirizine, at regular dosing, and terfenadine, at double dosing, are more potent than astemizole and chlorpheniramine (Figure 1).4 Thus, when using potency data to differentiate between drugs, both the endpoint 878 selected for measurement and the protocol used must be taken into consideration. DOES POTENCY REFLECT CLINICAL EFFICACY? Many examples of discrepancy can be found between antihistamine potency and clinical efficacy. For example, although loratadine and fexofenadine have been demonstrated to have equal H1-receptor potency,2 a large randomized, double-blind clinical study found that fexofenadine was significantly better than loratadine in relieving eye symptoms and nasal congestion in patients with seasonal allergic rhinitis (P ≤ .05).5 In pharmaceutical development, the in vitro and in vivo potency of the drug candidate is only one of the factors involved when considering whether to progress the drug into clinical trials. Clinical efficacy measures the magnitude (quantity) and profile (quality) of clinical disease improvement following drug administration in human populations. The ability of a drug to interact with effector systems in humans is influenced by pharmacokinetic parameters, such as absorption and metabolism, which determine the bioavailability of the drug at sites of action in the body. The clinical usefulness of a drug may be limited by undesired adverse effects and by interactions at sites other than target receptors that may or may not be characterized. Thus, in contrast to potency, which quantifies a single endpoint in relation to drug dose or concentration, clinical efficacy measures the therapeutic benefit brought about by the integration of complex interactions among various tissues, receptors, effector mechanisms, and physiologic processes. PHARMACOKINETIC AND PHARMACODYNAMIC FACTORS The potency of a drug is evaluated by assessing the response to the direct application or administration of the drug to a particular tissue under strictly defined conditions. Therefore, it does not take into account the extent to which a drug reaches its sites of action; that is, the bioavailability of the drug at the target organ. The molecular size, shape, and solubility of a drug are key factors determining bioavailability, as these properties affect the distribution of the drug around the body. Accordingly, an effective drug will easily penetrate its site of action, increasing the bioavailability of the drug to its target receptors. A recent study of healthy volunteers found that, com- Vol. 2, No. 24 ■ November 2002 PROCEEDINGS pared with an equivalent dose of diphenhydramine, fexofenadine penetrated the skin to a greater extent. The clinical relevance of this was reflected in the significantly greater suppression of both wheals and flares by fexofenadine following epicutaneous injection of histamine into the skin.6 trate this point, although cetirizine has an apparently greater ability to inhibit histamine-induced wheal and flare responses compared with loratadine, nasal challenge studies have failed to show any difference in efficacy between cetirizine and loratadine.7 Whereas it is clear that histamine is the primary mediator in pruritus and sneezing, other agents such as neuropeptides, sulfidopeptide leukotrienes, or even prostaglandin D2 may contribute to other symptoms such as rhinorrhea and nasal congestion. Furthermore, while antihistamines clearly exert their main pharmacologic effects by competitive antagonism of histamine for H1-receptors present in smooth muscles, nerve endings, and glandular cells, some of the newer antihistamines, such as cetirizine, loratadine, desloratadine, and fexofenadine, also exhibit significant anti-inflammatory effects. As an example, fexofenadine has been shown to significantly reduce the release of numerous late-phase inflammatory mediators and adhesion molecules such as granulocyte macrophage-colony stimulating DIFFERENCES IN TARGET ORGAN CELLULAR MECHANISMS The comparative ability, or potency, of various antihistamines to block histamine-induced wheal and flare in the skin has often been used to predict the global antiallergic clinical efficacy of various antihistamines in allergic rhinitis. However, the allergic response is not simply the consequence of one mediator, but results from a complex cascade of interactions among specialized cells and mediators. Thus, an important point to note is that unlike the clinical situation, the histamine-induced wheal and flare reaction involves neither mast cell degranulation nor activation of the complex cascade of cellular events that are observed in the late-phase allergic response. To illus- Figure 1. Comparison of Effects of Antihistamines in Receptor Binding Assays and Histamine-Induced Wheal and Flare Assays Astemizole Chlorpheniramine > Cetirizine 10 mg Terfenadine 120 mg Cetirizine Terfenadine Chlorpheniramine, Astemizole 80 Cetirizine, Terfenadine 60 50 40 20 Mean Wheal Area (cm2) Receptor Occupancy (%) 100 > Astemizole 10 mg Chlorpheniramine 4 mg Placebo Astemizole Cetirizine 0.2 Terfenadine Chlorpheniramine 0.1 0 0 log [Antihistamine] 0 0.5 1 2 3 4 5 6 7 8 9 10 11 12 24 Time (h) Modified with permission from: Simons FE, McMillan JL, Simons KJ. A double-blind, single-dose, crossover comparison of cetirizine, terfenadine, loratadine, astemizole, and chlorpheniramine versus placebo: suppressive effects on histamine-induced wheals and flares during 24 hours in normal subjects. J Allergy Clin Immunol. 1990;86(suppl 4, pt 1):540-547. Advanced Studies in Medicine ■ 879 PROCEEDINGS factor, soluble intracellular adhesion molecule 1, interleukin-8, and leukotriene-C4.8 These additional anti-inflammatory effects cannot be explained purely on the basis of classic H1-receptor blockade and therefore cannot be predicted from the results of potency measurements. The clinical significance of these effects is currently unknown. TARGET ORGAN SELECTIVITY In addition to receptor selectivity, the ideal drug will only affect its target sites of action. The first-generation antihistamines are small, lipophilic molecules, which enables them to easily cross the blood-brain barrier and bind to central H1-recep- 880 P<.001 AMP = adenosine monophosphate; CHO = Chinese hamster ovary. Adapted from: Ellis J, Seidenberg M. Desloratadine interacts with muscarinic acetylcholine receptors with high affinity and antagonizes the cyclic AMP response at the M2 subtype. J Allergy Clin Immunol. 2001;107(2):S160. Figure 3. Effect of Desloratadine on Heart Rate in Conscious Dogs Heart Rate (% change from control) RECEPTOR SELECTIVITY Only a few drugs can be said to be fully selective for their target receptor, and often they possess additional pharmacologic effects. In some cases, such as the anti-inflammatory effects described above, these additional effects can be beneficial. However, nonselective effects are often unwanted, and are related to the drug’s affinity for nontarget receptors. For example, the H1-receptor shares close sequence homology with muscarinic acetylcholine M2-receptors, and many of the first-generation antihistamines, such as hydroxylamine and promethazine, possess a high affinity for both H1-receptors and the muscarinic receptors M1, M2, and M3. Antagonism of M2receptors by nonselective antihistamines can result in adverse effects since M2-receptors are involved in maintaining vagal tone, and blockade of these receptors causes an increase in heart rate.9 Recent experiments have shown that the antihistamine desloratadine exhibits a high affinity for cardiac M2-receptors; it is 5 times more selective for H1receptors compared with M2-receptors.10 This study also showed that desloratadine was able to antagonize the effects of the muscarinic agonist, carbachol, on the inhibition of adenyl cyclase (Figure 2). In contrast, the selectivity ratio of fexofenadine for these 2 receptors is 2 orders of magnitude higher: fexofenadine is 600-fold more selective for H1-receptors compared with M2receptors.10 Moreover, in a recent study, the antimuscarinic effect of desloratadine was shown to increase the resting heart rate of conscious dogs both under normal conditions and following heart failure (Figures 2 and 3).11 Figure 2. Effects of Desloratadine (DCL) and Fexofenadine (FEX) on Cyclic AMP Levels in CHO Cells Expressing M2 Muscarinic Receptors Adapted from: Igawa A, Cheg CP, Little W. Desloratadine, but not fexofenadine, increases the heart rate in dogs before and after heart failure. Allergy. 2001;56(suppl 68):203-204. Vol. 2, No. 24 ■ November 2002 PROCEEDINGS tors. Indeed, positron-emission tomography studies demonstrate a strong positive correlation between the degree of central H1-receptor binding and the level of sedation caused by some antihistamines.12 The high levels of sedation and subsequent performance deficits seen with the first-generation antihistamines led to the development of new lipophobic H1-receptor antagonists, which do not cross into the central nervous system.13 This lack of central effects means that, compared with their forerunners, the newer antihistamines are more clinically useful in the practical daily treatment of common allergies. CONCLUSION Although potency is often mistakenly equated with efficacy, drugs with greater potency do not necessarily have greater clinical efficacy, as therapeutic behavior is modulated by pharmacokinetic and pharmacodynamic parameters, and by further interactions at sites other than the target receptor, which may or may not be characterized. This is exemplified in the case of antihistamines by studies demonstrating that agents with a similar potency may differ dramatically in clinical efficacy. Potency is certainly a useful marker of the potential therapeutic actions of a drug at the preliminary stages of drug development, but beyond this stage, clinical efficacy can only be assessed within the patient population. Moreover, relative potency has been shown to vary across various investigative models. Taken together, these observations emphasize the importance of clearly distinguishing between potency and efficacy when analyzing the results of clinical outcomes of studies comparing drugs in a particular therapeutic class, such as antihistamines. Advanced Studies in Medicine ■ REFERENCES 1. Kreutner W, Hey JA, Anthes J, Barnett A, Tozzi S. Preclinical studies of desloratadine, a nonsedating selective histamine H1-receptor antagonist with anti-allergic activity. Allergy. 2000;55(suppl 63):278. 2. Anthes J, Richard C, West RE, et al. Functional characterization of desloratadine and other antihistamines in human histamine H1 receptors. Allergy. 2000;55(suppl 63):277. 3. Fossard N, Purohit A, Kovacs S et al. Fexofenadine is superior to loratadine and desloratadine in onset of action of histamine-induced wheal and flare inhibition. Ann Allergy Asthma Immunol 2002 (Abstr). In Press. 4. Simons FE, McMillan JL, Simons KJ. A double-blind, singledose, crossover comparison of cetirizine, terfenadine, loratadine, astemizole, and chlorpheniramine versus placebo: suppressive effects on histamine-induced wheals and flares during 24 hours in normal subjects. J Allergy Clin Immunol. 1990;86(suppl 4, pt 1):540-547. 5. Van Cauwenberge P, Juniper EF. Comparison of the efficacy, safety and quality of life provided by fexofenadine hydrochloride 120 mg, loratadine 10 mg and placebo administered once daily for the treatment of seasonal allergic rhinitis. Clin Exp Allergy. 2000;30(6):891-899. 6. Simons FE, Silver NA, Gu X, Simons KJ. Skin concentrations of H1-receptor antagonists. J Allergy Clin Immunol. 2001;107(3):526-530. 7. Persi L, Demoly P, Harris AG, Tisserand B, Michel FB, Bousquet J. Comparison between nasal provocation tests and skin tests in patients treated with loratadine and cetirizine. J Allergy Clin Immunol. 1999;103(4):591-594. 8. Abdelaziz MM, Khair OA, Devalia JL. The potential of active metabolites of antihistamines in the management of allergic disease. Allergy. 2000;55(5):425-434. 9. Goyal RK. Muscarinic receptor subtypes. Physiology and clinical implications. N Engl J Med. 1989;321(15):1022-1029. 10. Ellis J, Seidenberg M. Desloratadine interacts with muscarinic acetylcholine receptors with high affinity and antagonizes the cyclic AMP response at the M2 subtype. J Allergy Clin Immunol. 2001;107(2):S160. 11. Igawa A, Cheg CP, Little W. Desloratadine, but not fexofenadine, increases the heart rate in dogs before and after heart failure. Allergy. 2001;56(suppl 68):203-204. 12. Okamura N, Yanai K, Higuchi M, et al. Functional neuroimaging of cognition impaired by a classical antihistamine, d-chlorpheniramine. Br J Pharmacol. 2000; 129(1):115-123. 13. Gonzalez M, Estes K. Pharmacokinetic overview of oral second-generation H1 antihistamines. Int J Clin Pharmacol Ther. 1998;36(5):292-300. 881