SARASOTA MEMORIAL HOSPITAL NURSING PROCEDURE
advertisement
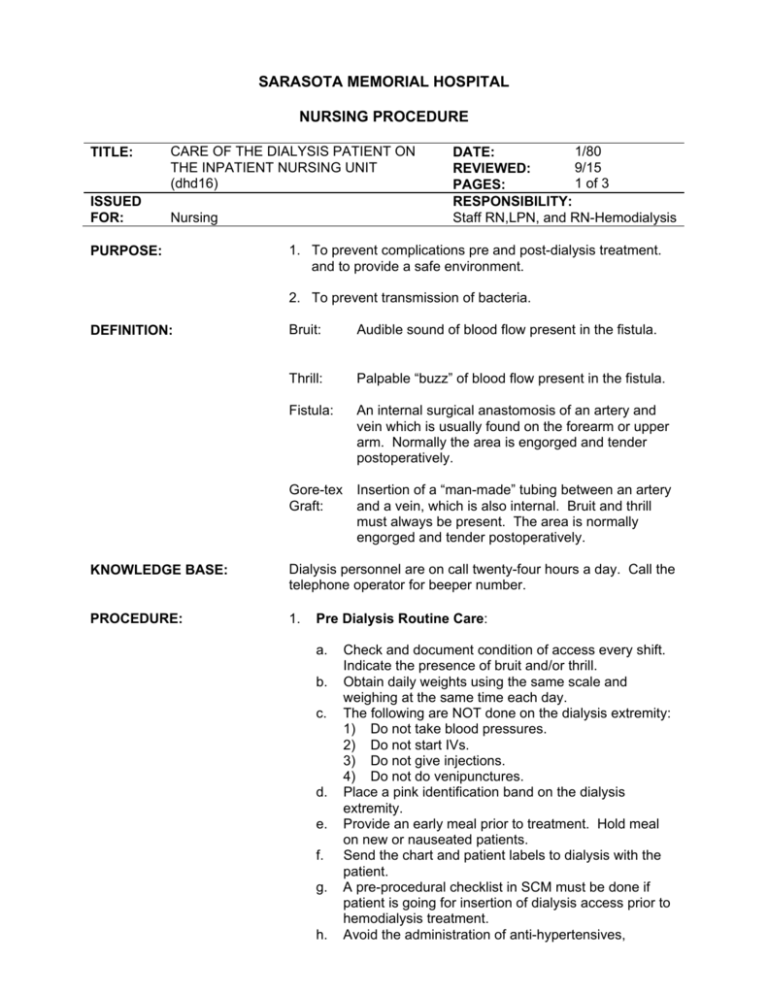
SARASOTA MEMORIAL HOSPITAL NURSING PROCEDURE TITLE: ISSUED FOR: CARE OF THE DIALYSIS PATIENT ON THE INPATIENT NURSING UNIT (dhd16) Nursing PURPOSE: 1/80 DATE: 9/15 REVIEWED: 1 of 3 PAGES: RESPONSIBILITY: Staff RN,LPN, and RN-Hemodialysis 1. To prevent complications pre and post-dialysis treatment. and to provide a safe environment. 2. To prevent transmission of bacteria. DEFINITION: Bruit: Audible sound of blood flow present in the fistula. Thrill: Palpable “buzz” of blood flow present in the fistula. Fistula: An internal surgical anastomosis of an artery and vein which is usually found on the forearm or upper arm. Normally the area is engorged and tender postoperatively. Gore-tex Graft: Insertion of a “man-made” tubing between an artery and a vein, which is also internal. Bruit and thrill must always be present. The area is normally engorged and tender postoperatively. KNOWLEDGE BASE: Dialysis personnel are on call twenty-four hours a day. Call the telephone operator for beeper number. PROCEDURE: 1. Pre Dialysis Routine Care: a. b. c. d. e. f. g. h. Check and document condition of access every shift. Indicate the presence of bruit and/or thrill. Obtain daily weights using the same scale and weighing at the same time each day. The following are NOT done on the dialysis extremity: 1) Do not take blood pressures. 2) Do not start IVs. 3) Do not give injections. 4) Do not do venipunctures. Place a pink identification band on the dialysis extremity. Provide an early meal prior to treatment. Hold meal on new or nauseated patients. Send the chart and patient labels to dialysis with the patient. A pre-procedural checklist in SCM must be done if patient is going for insertion of dialysis access prior to hemodialysis treatment. Avoid the administration of anti-hypertensives, TITLE: CARE OF THE DIALYSIS PATIENT ON AN INPATIENT NURSING UNIT (dhd16) PAGE: 2 of 3 narcotics, or antibiotics prior to treatment. If any questions about withholding medications, consult with the Dialysis nurse. i. If it is necessary for the Dialysis RN to draw lab work, notification should be given in the form of a pretreatment report. Send any Labels from the lab with the patient. j. Use “Hand off” communication guidelines to discuss medications/labs/isolation precautions/etc. k. The patient will be taken to dialysis by the transport team, via wheelchair, stretcher or bed when the unit is called. If the patient meets criteria as established in the SMH policy 01.PAT.23, then a nurse must accompany the patient on the transport. If the patient is from a critical care unit, they need to be transported with a cardiac monitor and an RN. 2. Post-Dialysis Routine Care: a. b. c. d. e. f. g. h. 3. Post-dialysis: The dialysis nurse will give a patient report to the receiving nurse. In the event the patient does have to go to another procedure, a nurse from Hemo will accompany the patient if criteria met as per 01.PAT.23. Otherwise, the patient may be transported to the next procedural area via Transport Services after a nurse-to-nurse communication. Check the access upon returning to the unit postdialysis. Document condition of the patient including any changes from pre-dialysis condition. Thrill and bruit will be checked each shift. Check the access each shift for hematoma, swelling or oozing. Apply direct pressure for 5-10 minutes if there is oozing or slight bleeding from the fistula. DO NOT apply pressure dressings! Notify the dialysis physician immediately for profuse bleeding or absence of thrill. Apply direct pressure for bleeding. Band-aids covering dialysis sites can be removed eight hours after dialysis. All medications will be resumed post treatment including daily medication dosages unless new orders are written. Post-Surgical: a. b. c. Moderate pain and edema of extremity is common. Elevate with pillow and check fingers for good circulation. Severe pain is unusual. Check bruit and thrill before medicating. (Clotting may be occurring.) Slight oozing of blood is common. Note amount and TITLE: CARE OF THE DIALYSIS PATIENT ON AN INPATIENT NURSING UNIT (dhd16) d. e. PAGE: 3 of 3 reinforce dressing. Do not apply a pressure dressing. Do not use ice on access. Temperature change may cause clotting. Observe for bruit and thrill and bleeding with routine postop vital signs, eventually tapering to an every-shift check. Call surgeon if there are any problems. DOCUMENTATION: Assessment/Reassessment flowsheet (under the Peripheral/Vascular section) (or forms appropriate to special care areas): Document the access checks and reassessments. REFERENCE: SMH Policy. Handoff Communication Guidelines. (01.PAT.25). SMH: Author. SMH Policy. Transportation and Monitoring of Patients (01.PAT.23). SMH: Author. SMH Nursing Department Policy. Guidelines for Intra-hospital Transporting of Adult Special Care Patient. (126.442). SMH: Author. REVIEWING AUTHOR(S): B. Kruger RN, CCRN, CNN, CPS, Critical Care/Hemodialysis S. Olsen RN,BS,CCRN, CM, Hemodialysis Jackie Bland, BSN, RN Medical Wound Care Doris Cahueque, MS, RN, CNL APN, Medical-Surgical Division Wendy Kline, MSN, RN, PCCN, Clinical Manager, 7WT APPROVAL: Clinical Practice Council 9/3/15