0021-972X/04/$15.00/0
Printed in U.S.A.
The Journal of Clinical Endocrinology & Metabolism 89(9):4422– 4427
Copyright © 2004 by The Endocrine Society
doi: 10.1210/jc.2004-0160
Factors That Affect Final Height and Change in Height
Standard Deviation Scores in Survivors of Childhood
Cancer Treated with Growth Hormone: A Report from
the Childhood Cancer Survivor Study
CARRIE M. BROWNSTEIN, ANN C. MERTENS, PAULINE A. MITBY, MARILYN STOVALL, JING QIN,
GLENN HELLER, LESLIE L. ROBISON, AND CHARLES A. SKLAR
Departments of Pediatrics (C.M.B., C.A.S.) and Epidemiology and Biostatistics (J.Q., G.H.), Memorial Sloan-Kettering
Cancer Center, New York, New York 10021; Department of Pediatrics (A.C.M., P.A.M., L.L.R.), University of Minnesota
School of Medicine, Minneapolis, Minnesota 55455; and Department of Radiation Physics (M.S.), University of Texas M. D.
Anderson Cancer Center, Houston, Texas 77030
GH deficiency is a common late complication in survivors of
pediatric malignancies, particularly those who are treated
with radiation (RT) to the hypothalamic-pituitary region.
Nonetheless, few reports have assessed final height outcomes
in survivors treated with GH. In the present study, we investigated which patient and treatment variables correlate with
final height and change in height SD score (SDS) in a large
cohort of cancer survivors treated with GH.
We previously identified 361 participants in the multicenter Childhood Cancer Survivor Study who were treated
with GH. Final height data were available in 183 survivors
(120 males). Diagnoses included: central nervous system tumors (n ⴝ 90), acute leukemia (n ⴝ 64), soft tissue sarcomas
(n ⴝ 23), and miscellaneous (n ⴝ 6). The median age at diagnosis of the primary cancer was 4.6 yr, and the median age at
start of GH treatment was 11.3 yr. Mean height SDS at start of
D
UE TO IMPROVEMENTS in therapies and supportive
care, the survival rates for children and adolescents
with a malignancy have increased dramatically over the
last 30 yr (1). Because most pediatric cancer patients now can
be expected to survive into adulthood, it has become increasingly important to study the long-term consequences
and delayed effects of pediatric malignancies and their
treatments.
At least one endocrine disturbance can be documented in
approximately 40% of survivors, including GH deficiency
(GHD). GHD is most often seen after radiation (RT) to the
hypothalamic-pituitary region or as a consequence of a tumor in that region of the brain (2). Although GHD is common
among survivors of certain pediatric cancers and contributes
to adult short stature in this population (3, 4), the determinants of final height in survivors are multifactorial and include both hormonal (e.g. GHD, precocious puberty) and
nonhormonal factors (e.g. RT injury to the growth plates of
Abbreviations: CCSS, Childhood Cancer Survivor Study; CI, confidence interval; GHD, GH deficiency; GnRHa, GnRH agonist; IGHD,
idiopathic GHD; RT, radiation; SDS, sd score.
JCEM is published monthly by The Endocrine Society (http://www.
endo-society.org), the foremost professional society serving the endocrine community.
GH therapy was ⴚ2.03 ⴞ 0.8, and the mean final height SDS
was ⴚ1.48 ⴞ 0.10 (P < 0.001). Final height SDS was positively
associated with target height and dose of GH but negatively
associated with the presence of concomitant endocrinopathies and dose of spinal RT. Change in height SDS (start of
GH-final height) was positively associated with male gender,
younger bone age at start of GH, and dose of GH; presence of
concomitant endocrinopathies and dose of spinal RT were
negatively associated with change in height SDS. Risk factors
associated with a final height of ⴚ2.0 SD or less included lower
doses of GH and exposure to higher doses of spinal RT. Thus,
to maximize final height, our findings emphasize the importance of beginning GH therapy at the earliest bone age that is
clinically feasible; treating with conventional higher doses of
GH; and, when possible, minimizing the dose of spinal RT.
(J Clin Endocrinol Metab 89: 4422– 4427, 2004)
spine, midparental height). Despite the fact that GH has been
used in survivors of childhood cancers for more than 25 yr,
data on the final height of survivors treated with GH are
quite limited (5–9). Moreover, because of the small size and
homogenous nature of most series, it has not been possible
to determine the interaction among various patient (e.g. age,
gender) and treatment (e.g. spinal RT) variables and how
they impact the response to GH.
In the present study, we attempted to overcome some of
the aforementioned limitations by determining the variables
that contribute to final height and change in height sd score
(SDS) (start of GH-final height) in a large and heterogeneous
cohort of survivors of childhood cancer treated with GH.
Patients and Methods
Childhood Cancer Survivor Study (CCSS)
The cohort of patients evaluated in this study is a subset of the
patients who are participants in the CCSS, also known to study participants as the Long-Term Follow-Up Study. The methods, objectives,
eligibility criteria, and characteristics of study participants for the CCSS
have been published in detail previously (10). In brief, the CCSS is a
multiinstitutional (see Acknowledgments) retrospective study of 5-yr survivors of childhood cancer diagnosed before age 21 yr, between 1970 and
1986. Subjects with benign tumors, including craniopharyngioma, were
excluded from the study. The study was aimed primarily at determining
late adverse outcomes that follow treatment for childhood and adoles-
4422
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 14:55 For personal use only. No other uses without permission. . All rights reserved.
Brownstein et al. • Height in GH-Treated Childhood Cancer Survivors
cent cancer. The study was reviewed and approved by the Institutional
Review Board at each of the 25 participating clinical centers.
Each participant was required to fill out an extensive baseline questionnaire (complete questionnaire is available at www.cancer.umn.edu/
ccss). In addition, detailed medical information was abstracted from the
medical record of each participant. Data collected included all treatments for the primary diagnosis, including the initial treatment, treatment for any relapse, and preparatory regimens for bone marrow transplant. Information about cancer treatment included qualitative
information on 42 chemotherapeutic agents; quantitative information on
22 selected agents; surgeries performed from the time of diagnosis; and
quantitative radiation data on field size, site, and dose.
Survivors treated with GH
From among the first 13,539 participants of the CCSS, we were able
to verify that 361 had received treatment with GH (11). From among
those 361 subjects treated with GH, 183 had completed their growing
and had documented final height data. Final height was defined as the
height achieved when serial heights revealed a change of 2 cm or less
over a 12-month period or the height recorded when the bone age was
14.5 yr or more for girls and 16 yr or more for boys. Additionally, the
charts were reviewed for parental heights, dose of GH, duration of GH
therapy, preparation of GH prescribed, bone age at commencement of
GH treatment, peak GH value during provocative testing, and treatment
with other hormones including GnRH agonists (GnRHa). Results of
provocative GH testing were available on 163 of the 183 participants. The
peak GH response to provocative testing was less than 10 ng/ml in 156
subjects (68 subjects tested with two agents; 88 subjects tested with one
agent) and more than 10 ng/ml in the remaining seven.
A total of 177 patients were known to have received RT; complete
radiotherapy records were available for 165 of these patients. Eighty-six
received cranial irradiation, 72 craniospinal irradiation, and seven received total body irradiation. Treatment volumes were determined for
each patient, based on diagrams and photographs of the patients in
treatment position, as found in the records. The absorbed radiation dose
was estimated to the hypothalamus-pituitary and the spine; the spine
was considered to have been irradiated if at least three fourths of the
spine was included in a radiation beam. Standard radiotherapy depth
dose data (12) were used to estimate doses to anatomic sites in a beam,
and data measured in a water phantom were used for out-of-beam sites
(13). For analysis, hypothalamic-pituitary and spinal doses were placed
in six categories: 0 –10, more than 10 –20, more than 20 –30, more than
30 – 40, more than 40 –50, and more than 50⫹ Gy.
Statistical analysis
This was an observational study intended to determine the factors
that contribute to final height in survivors of childhood cancer treated
with GH, which factors put these children at greatest risk for significant
short stature. The covariates, age at diagnosis, age at commencement of
GH therapy, bone age at commencement of GH therapy, duration of GH
therapy, dose of GH, target height, gender, treatment with chemotherapy, treatment with a GnRHa, treatment with other hormonal agents,
dose of pituitary RT, and dose of direct spinal RT were used to explain
the variability in the response variables: final height SDS, change in
height SDS, and final height SDS dichotomized at ⫺2.0. A linear regression model was used to model the relationship for the first two
response variables, and a logistic regression model was used for the third
response variable. Stepwise regression was used to find the most significant factors. Pearson’s correlation coefficient was used to measure
the association between the self-reported final heights and the documented final heights. The t-statistic was used to test the difference
between groups univariately.
Results
The clinical characteristics of the 183 GH-treated survivors with documented final height data are summarized
in Table 1.
J Clin Endocrinol Metab, September 2004, 89(9):4422– 4427 4423
TABLE 1. Patient characteristics
Gender (male:female)
Median age (yr) at cancer diagnosis
(range)
Diagnoses
Tumors of the CNS
Medulloblastomaa
Astroglial
Ependymoma
Germ cell
Miscellaneous
Acute leukemiab
Soft tissue sarcoma
Rhabdomyosarcoma
Neuroblastoma
Other
Median age (yr) at start of GH
(range)
Median duration (yr) of GH
therapy (range)
GH preparation
Human pituitary only
Recombinant only
Both
Unknown
Other hormones
T4
Glucocorticoids
DDAVP/vasopressin
Sex hormones
GnRH agonist
120:63
4.6 (0 –13.9)
90
42
31
7
9
1
64
23
22
5
1
11.3 (3.1–18.6)
4.5 (0.55–13.1)
18
139
19
7
108
21
8
47
14
CNS, Central nervous system; DDAVP, 1-desamino-8-D-arginine
vasopressin.
a
Includes cases of primitive neuroectodermal tumors (PNET).
b
Includes cases of non-Hodgkin’s lymphoma (NHL).
Variables associated with final height and change in
height SDS
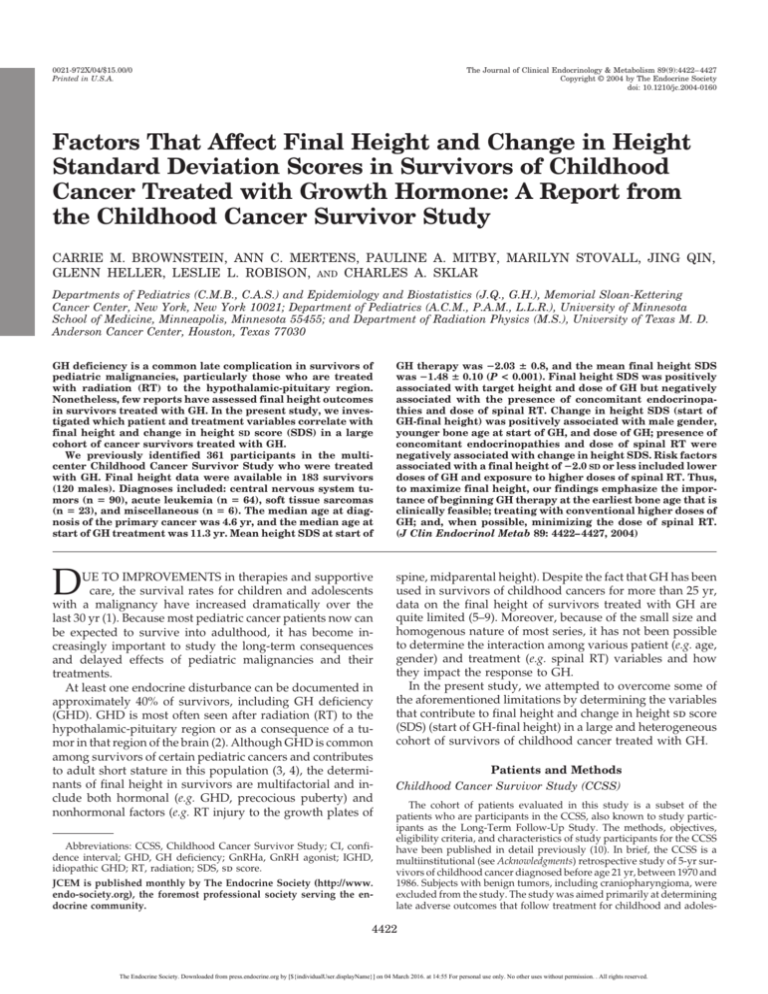
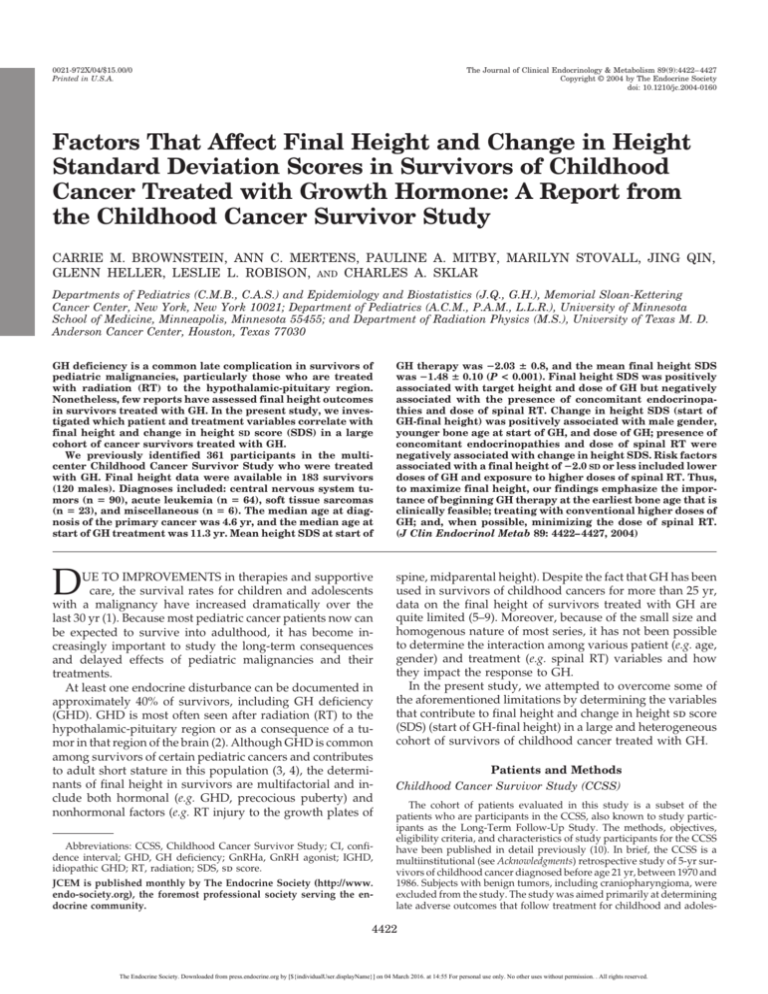
The change in height SDS from the start of GH therapy to
final height was significant (⫺2.08 ⫾ 0.08 vs. ⫺1.48 ⫾ 0.10,
P ⬍ 0.0001) (Fig. 1). The variables associated with change in
height SDS and final height SDS for the multivariate models
are summarized in Table 2. In the multivariate model, change
in height SDS was positively associated with male gender
and dose of GH but negatively associated with bone age at
start of GH, treatment with other hormones in addition to
GH, and dose of spinal RT.
In the multivariate model, final height was positively associated with target height and dose of GH but negatively
associated with treatment with other hormones in addition
to GH and dose of spinal RT (Table 2 and Fig. 2).
Risk of final height ⫺2.0
SD
or less
We calculated the odds ratio for final height ⫺2.0 sd or less
for GH-treated survivors stratified by GH dose, bone age at
start of GH therapy, dose of spinal RT, and gender (Table 3).
The odds of final height ⫺2.0 sd or less for survivors treated
with spinal RT at a dose of 10 ⫺30 Gy or less were 2.1 times
[95% confidence interval (CI), 0.921, 5.095] and those treated
with a dose more than 30 Gy were 3.4 times (95% CI, 1.595–
7.279; P ⫽ 0.004) the odds of final height ⫺2.0 sd or less for
survivors treated with spinal doses less than 10 Gy. The odds
of final height ⫺2.0 sd or less for survivors treated with GH
at a dose greater than 0.3 mg/kg䡠wk were 0.22 times (95% CI,
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 14:55 For personal use only. No other uses without permission. . All rights reserved.
4424
J Clin Endocrinol Metab, September 2004, 89(9):4422– 4427
0.109, 0.442; P ⬍ 0.0001) the odds of final height ⫺2.0 sd or
less, compared with those treated with a dose less than 0.25
mg/kg䡠wk.
Discussion
Studies of final height in childhood cancer survivors
treated with GH are important to determine the effectiveness
FIG. 1. The height SDS at start of GH and final height. Solid white
line represents median height SDS. The boxes represent the 25th and
75th quartiles. Whiskers extend to the upper and lower adjacent
values that are 1.5 times or less the interquartile range. *, P ⬍ 0.0001.
Brownstein et al. • Height in GH-Treated Childhood Cancer Survivors
of GH therapy and identify areas in which physicians can
intervene to improve final height outcome. Our study provides final height data on the largest cohort of childhood
cancer survivors treated with GH reported to date. We were
able to identify five variables that were independently associated with an improvement in height SDS: use of lower
doses of spinal RT, use of higher doses of GH, initiation of
GH therapy at a younger bone age, male gender, and the
absence of additional endocrinopathies. Dose of pituitary
irradiation, use of GnRHa, exposure to chemotherapy, and
duration of GH treatment were not found to have an independent effect on change in height SDS. We found that target
height did contribute to final height SDS but not to change
in height SDS.
Our results confirm the earlier findings of smaller studies
demonstrating the efficacy of GH treatment in survivors of
childhood cancer (5, 6, 8, 14 –16). Most recently, Gleeson et al.
(9) demonstrated improvements in final height outcomes
over 25 yr in childhood brain tumor survivors. These improvements were presumably secondary to more standardized GH schedules, superior dosing regimens (i.e. higher
doses spread over 6 –7 d/wk), and the use of GnRHa in
selected groups of patients.
Additionally, our results concur with the findings of previous studies evaluating children with idiopathic GHD
(IGHD), which demonstrated the use of higher doses of GH
to be beneficial in maximizing final height (17–20). We observed an inverse correlation between risk of final height SDS
⫺2.0 or less and GH dose. Previously Radetti et al. (20)
observed significantly higher final height SDS and growth
velocity SDS in patients treated with GH at 0.3 mg/kg䡠wk as
compared with 0.15 mg/kg䡠wk. Blethen et al. (18) demon-
TABLE 2. Results of multivariate analysis for change in height SDS and final height SDS
Change in height SDS (start GH-final)
Log-bone age at start of GH
Female gender
Other hormone treatment
Dose of GH (⬍0.25 vs. ⱖ0.25 mg/kg䡠wk)
Spinal RT (⬍20 vs. ⱖ20 Gy)
Final height SDS
Target height
Other hormone treatment
Dose of GH (⬍0.25 vs. ⱖ0.25 mg/kg䡠wk)
Spinal RT (⬍20 vs. ⱖ20 Gy)
Estimated coefficient (95% CI)
P
⫺0.804 (⫺1.288, ⫺0321)
⫺0.462 (⫺0.774, ⫺0.150)
⫺0.397 (⫺0.707, ⫺0.086)
0.402 (0.090, 0.715)
⫺0.611 (⫺0.936, ⫺0.286)
0.001
0.004
0.013
0.013
0.0003
0.402 (0.195, 0.608)
⫺0.620 (⫺1.017, ⫺0.224)
0.739 (0.343, 1.134)
⫺0.772 (⫺1.194, ⫺0.351)
0.0002
0.003
0.0004
0.0005
FIG. 2. Final height SDS according to
original diagnosis and exposure to direct spinal RT. Solid white line represents median height SDS. The boxes
represent the 25th and 75th quartiles.
Whiskers extend to the upper and lower
adjacent values that are 1.5 times or
less the interquartile range. Outliers
are individually plotted (horizontal
lines). CNS, Central nervous system. *,
P ⬍ 0.05; **, P ⬍ 0.0001.
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 14:55 For personal use only. No other uses without permission. . All rights reserved.
Brownstein et al. • Height in GH-Treated Childhood Cancer Survivors
TABLE 3. Risk factors associated with final height ⫺2.0 SDS
or less
Factor
GH dose (mg/kg䡠wk)
⬍0.25
0.25– 0.3
⬎0.3
Bone age at start of GH (yr)
⬍4
4–8
⬎8
Dose of spinal RT (Gy)
⬍10
10 to ⱕ30
⬎30
Gender
Male
Female
Odds ratio (95% CI)
P
⬍0.0001
1.000
0.553 (0.205–1.491)
0.220 (0.109 – 0.442)
0.627
1.000
1.020 (0.474 –2.194)
0.720 (0.307–1.688)
0.004
1.000
2.167 (0.921–5.095)
3.408 (1.595–7.279)
0.281
1.000
1.411 (0.756 –2.632)
strated higher final height SDS in IGHD patients treated with
recombinant human GH at 0.3 mg/kg䡠wk, compared with
historical controls treated with 0.15– 0.19 mg/kg䡠wk. More
recently Cohen et al. (21) reported a dose-response effect of
GH both on growth and the serum levels of the growth
factors IGF-I and IGF binding protein-3. In the latter study,
it appeared that the dose-response curve reached a plateau
at around 0.35 mg/kg䡠wk. At higher doses, there was a
greater chance of an elevated IGF-I level but without additional benefit in terms of growth (21).
In the current study, patients were treated with both
pituitary-derived GH as well as the recombinant forms of
GH. Moreover, the doses used were often lower than the
doses that are routinely used currently. Thus, we would
anticipate that the height outcomes achieved in the future are
likely to be superior to those described in this report.
Our study confirms the well-documented detrimental effect of spinal RT on growth and final height (7, 14, 22). In our
study, patients who received more than 30 Gy to the spine
had a 3.5 times greater risk of achieving a final height ⫺2.0
sd or less, compared with those treated with less than 10 Gy.
Furthermore, when patients were stratified by diagnosis and
exposure to direct spinal RT, patients with acute leukemia
and central nervous system tumors treated with direct spinal
RT had a statistically significant shorter final height SDS than
those who did not get spinal RT as part of their treatment.
In the present study, males appeared to have a better
response to GH, compared with females. The reasons for this
are not clear, but age and bone age at start of GH therapy
were similar between males and females (data not shown).
In review of the literature on the affect of gender on height
outcome after GH therapy, the data are conflicting and confounded by whether puberty was spontaneous or induced
(23, 24). It has been previously demonstrated that females are
more likely to develop precocious puberty after cranial irradiation than similarly treated males (25, 26). Thus, it is
possible that the propensity for females to enter puberty
prematurely may account, at least in part, for their poorer
height outcomes. Furthermore, the smaller number of females in this and most other studies make comparisons between males and females difficult. Whereas it is possible that
male survivors may respond better to GH, further studies are
needed.
J Clin Endocrinol Metab, September 2004, 89(9):4422– 4427 4425
The use of a GnRHa has been shown to enhance final
height in patients with central precocious puberty (27), those
with IGHD without precocious puberty (28 –30), and normal
short children with normally timed puberty (31). Recent
studies have suggested an augmentation in final height in
childhood cancer survivors who were treated with both GH
and a GnRHa (5, 9). We did not find that GnRHa therapy was
associated with an increase in height SDS in this cohort. It is
possible that we did not find an affect of GnRHa on change
in final height SDS due to the small number of patients (14
of 183) who received GnRHa in the current study and the fact
that GnRHa therapy was not prescribed in a uniform manner
in this retrospective study.
Treatment with chemotherapy has been reported to have
a significant negative impact on final height (7, 25, 32–35). In
our cohort of survivors, we did not find chemotherapy to
independently contribute to final height and change in
height SDS. Similarly, in a recent study by Gurney et al. (36),
the addition of adjuvant chemotherapy to surgery and cranial irradiation or surgery alone did not impart a greater risk
of adult short stature in survivors of childhood brain cancer.
This disparity may be due, in part, to the fact that the patients
in the present study were treated with GH, as opposed to
some of the earlier studies in which patients were not so
treated (25, 32–35). Furthermore, in the study of OgilvyStuart and Shalet (7) in which the subjects were treated with
GH, the dose of GH was relatively low and lower than the
dose employed in many of the subjects in the present cohort.
Thus, it is possible that larger doses of GH may overcome
some of the detrimental effects of chemotherapy on growing
bones.
Although we did not find that the dose of radiation to the
hypothalamus and pituitary was predictive of final height or
change in height SDS as documented by earlier studies (37),
we did find that the presence of concomitant endocrinopathies was associated with reduced final height and less
change in height SDS. Because patients treated with higher
doses of hypothalamic-pituitary irradiation are at increased
risk of developing more profound GHD and additional anterior pituitary hormone deficiencies (4, 37), the presence of
concomitant endocrinopathies is likely a surrogate for radiation dose to the hypothalamic-pituitary axis. Additionally,
it is conceivable that suboptimal replacement therapy with
other hormones, especially glucocorticoids and sex steroids,
independently interferes with growth, as demonstrated by
superior final height outcomes in patients with isolated
GHD, compared with those with multiple congenital pituitary deficiencies (38).
Whereas recent data support the safety of GH replacement
therapy in survivors of childhood cancer in terms of risk of
disease recurrence, the issue of risk of subsequent new malignancies remains unresolved (11, 16, 39, 40). Given the data
on a possible link between the serum concentrations of IGF-I
and IGF binding protein-3 and the common cancers of adulthood (41, 42), the recommendation to monitor serum levels
of these growth factors in all children treated with GH seems
justified (21). This may be especially important when using
doses in the higher ranges.
In conclusion, our data from a large cohort of cancer survivors suggest that improvements in final height can be
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 14:55 For personal use only. No other uses without permission. . All rights reserved.
4426
J Clin Endocrinol Metab, September 2004, 89(9):4422– 4427
achieved by initiating GH therapy at the earliest bone age
that is clinically feasible, using conventional higher doses of
GH and, when possible, minimizing the dose of spinal RT.
Brownstein et al. • Height in GH-Treated Childhood Cancer Survivors
4.
5.
Acknowledgments
Following is the list of CCSS institutions and investigators: Arthur
Ablin, M.D.* (University of California-San Francisco, California); Roger
Berkow, M.D.* (University of Alabama, Birmingham, Alabama); John
Boice, Sc.D.‡ (International Epidemiology Institute, Rockville, Maryland); Norman Breslow, Ph.D.‡ (University of Washington, Seattle,
Washington); George R. Buchanan, M.D.*, Kevin Oeffinger, M.D.‡ (University of Texas Southwestern Medical Center at Dallas, Dallas, Texas);
Lisa Diller, M.D.*, Holcombe Grier, M.D.†, Frederick Li, M.D.‡ (DanaFarber Cancer Institute, Boston, Massachusetts); Zoann Dreyer, M.D.*
(Texas Children’s Center, Houston, Texas); Debra Friedman, M.D.,
M.P.H.*, Thomas Pendergass, M.D.‡ (Children’s Hospital and Medical
Center, Seattle, Washington); Daniel M. Green, M.D.*‡ (Roswell Park
Cancer Institute, Buffalo, New York); Mark Greenberg, M.B., Ch.B.*
(Hospital for Sick Children, Toronto, Canada); Robert Hayashi, M.D.*,
Teresa Vietti, M.D.† (St. Louis Children’s Hospital, St. Louis, Missouri);
Melissa Hudson, M.D.*‡ (St. Jude Children’s Research Hospital, Memphis, Tennessee); Raymond Hutchinson, M.D.* (University of Michigan,
Ann Arbor, Michigan); Michael P. Link, M.D.*, Sarah S. Donaldson,
M.D.‡ (Stanford University School of Medicine, Stanford, California);
Anna Meadows, M.D.*‡, Bobbie Bayton‡ (Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania); John Mulvihill, M.D.‡ (Children’s
Hospital, Oklahoma City, Oklahoma); Brian Greffe*, Lorrie Odom,
M.D.† (Children’s Hospital, Denver, Colorado); Maura O’Leary, M.D.*
(Children’s Health Care-Minneapolis, Minneapolis, Minnesota);
Amanda Termuhlen, M.D.*, Frederick Ruymann, M.D.†, Stephen
Qualman, M.D.‡ (Columbus Children’s Hospital, Columbus, Ohio);
Gregory Reaman, M.D.*, Roger Packer, M.D.‡ (Children’s National Medical Center, Washington, DC); A. Kim Ritchey, M.D.*, Julie Blatt, M.D.†
(Children’s Hospital of Pittsburgh, Pittsburgh, Pennsylvania); Leslie L.
Robison, Ph.D.*‡, Ann Mertens, Ph.D.‡, Joseph Neglia, M.D., M.P.H.‡,
Mark Nesbit, M.D.‡ (University of Minnesota, Minneapolis, Minnesota);
Stella Davies, M.D., Ph.D.‡ (Cincinnati Children’s Hospital Medical
Center, Cincinnati, Ohio); Kathy Ruccione, R.N., M.P.H.* (Children’s
Hospital Los Angeles, Los Angeles, California); Charles Sklar, M.D.*‡
(Memorial Sloan-Kettering Cancer Center, New York, New York);
Malcolm Smith, M.D.‡, Peter Inskip, Sc.D.‡ (National Cancer Institute,
Bethesda, Maryland); W. Anthony Smithson, M.D.*, Gerald Gilchrist,
M.D.† (Mayo Clinic, Rochester, Minnesota); Louise Strong, M.D.*‡,
Marilyn Stovall, Ph.D.‡ (University of Texas M. D. Anderson Cancer
Center, Houston, Texas); Terry A. Vik, M.D.*, Robert Weetman, M.D.†
(Riley Hospital for Children, Indianapolis, Indiana); Yutaka Yasui,
Ph.D.*‡, John Potter, M.D., Ph.D.†‡ (Fred Hutchinson Cancer Research
Center, Seattle, Washington); Lonnie Zeltzer, M.D.*‡ (University of California-Los Angeles, Los Angeles, California). *, Institutional principal
investigator; †, former institutional principal investigator; ‡, CCSS Steering Committee.
Received February 3, 2004. Accepted May 27, 2004.
Address all correspondence and requests for reprints to: Charles A.
Sklar, M.D., Memorial Sloan-Kettering Cancer Center, Department of
Pediatrics, 1275 York Avenue, New York, New York 10021. E-mail:
sklarc@mskcc.org.
This work was supported by National Institutes of Health Grant
(U24-CA55727), the Genentech Foundation for Growth and Development, and the University of Minnesota funding provided by the Children’s Cancer Research Fund.
References
1. Ries LAG, Smith MA, Gurney JG, Linet M, Tamra T, Young JL, Bunin GR,
eds 1999 Cancer incidence and survival among children and adolescents:
United States SEER Program 1975–1995. NIH Publication 99 – 4649. Bethesda,
MD: NIH, National Cancer Institute, SEER Program
2. Sklar CA 1999 Overview of the effects of cancer therapies: the nature, scale and
breadth of the problem. Acta Paediatr Suppl 88:1– 4
3. Robison LL, Nesbit Jr ME, Sather HN, Meadows AT, Ortega JA, Hammond
GD 1985 Height of children successfully treated for acute lymphoblastic leu-
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
kemia: a report from the Late Effects Study Committee of Children’s Cancer
Study Group. Med Pediatr Oncol 13:14 –21
Sklar CA 1997 Growth and neuroendocrine dysfunction following therapy for
childhood cancer. Pediatr Clin North Am 44:489 –503
Adan L, Sainte-Rose C, Souberbielle JC, Zucker JM, Kalifa C, Brauner R 2000
Adult height after growth hormone (GH) treatment for GH deficiency due to
cranial irradiation. Med Pediatr Oncol 34:14 –19
Vassilopoulou S, Klein MJ, Moore 3rd BD, Reid HL, Ater J, Zietz HA 1995
Efficacy of growth hormone replacement therapy in children with organic
growth hormone deficiency after cranial irradiation. Horm Res 43:188 –193
Ogilvy-Stuart AL, Shalet SM 1995 Growth and puberty after growth hormone
treatment after irradiation for brain tumours. Arch Dis Child 73:141–146
Herber SM, Dunsmore IR, Milner RD 1985 Final stature in brain tumours
other than craniopharyngioma: effect of growth hormone. Horm Res 22:63– 67
Gleeson HK, Stoeter R, Ogilvy-Stuart AL, Gattamaneni HR, Brennan BM,
Shalet SM 2003 Improvements in final height over 25 years in growth hormone
(GH)-deficient childhood survivors of brain tumors receiving GH replacement.
J Clin Endocrinol Metab 88:3682–3689
Robison LL, Mertens AC, Boice JD, Breslow NE, Donaldson SS, Green DM,
Li FP, Meadows AT, Mulvihill JJ, Neglia JP, Nesbit ME, Packer RJ, Potter
JD, Sklar CA, Smith MA, Stoval MA, Strong LC, Yasui Y, Zelter LK 2002
Study design and cohort characteristics of the Childhood Cancer Survivor
Study: a multi-institutional collaborative project. Med Pediatr Oncol 38:229 –
239
Sklar CA, Mertens AC, Mitby P, Occhigrosso G, Qin J, Heller G, Yasui Y,
Robison LL 2002 Risk of disease recurrence and second neoplasms in survivors
of childhood cancer treated with growth hormone: a report from the Childhood Cancer Survivor Study. J Clin Endocrinol Metab 87:3136 –3141
Aird EGA, Burns JE, Day MJ, Duane S, Jordan TJ, Kacperek A, Klevenhagen
SC, Harrison RM, Lillicrap SC, McKenzie AL, Pitchford WG, Shaw JE, Smith
CW 1996 Central axis depth dose data for use in radiotherapy: 1996. A survey
of depth doses and related data measured in water or equivalent media. Br J
Radiol Suppl 25:1–188
Stovall M, Smith SA, Rosenstein M 1989 Tissue doses from radiotherapy of
cancer of the uterine cervix. Med Phys 16:726 –733
Xu W, Janss A, Moshang T 2003 Adult height and adult sitting height in
childhood medulloblastoma survivors. J Clin Endocrinol Metab 88:4677– 4681
Lannering B, Albertsson-Wikland K 1989 Improved growth response to GH
treatment in irradiated children. Acta Paediatr Scand 78:562–567
Leung W, Rose SR, Zhou Y, Hancock ML, Burstein S, Schriock EA, Lustig
R, Danish RK, Evans WE, Hudson MM, Pui CH 2002 Outcomes of growth
hormone replacement therapy in survivors of childhood acute lymphoblastic
leukemia. J Clin Oncol 20:2959 –2964
MacGillivray MH, Baptista J, Johanson A 1996 Outcome of a four-year randomized study of daily versus three times weekly somatropin treatment in
prepubertal naive growth hormone-deficient children. Genentech Study
Group. J Clin Endocrinol Metab 81:1806 –1809
Blethen SL, Baptista J, Kuntze J, Foley T, LaFranchi S, Johanson A 1997 Adult
height in growth hormone (GH)-deficient children treated with biosynthetic
GH. The Genentech Growth Study Group. J Clin Endocrinol Metab 82:418 – 420
Blethen SL, Compton P, Lippe BM, Rosenfeld RG, August GP, Johanson A
1993 Factors predicting the response to growth hormone (GH) therapy in
prepubertal children with GH deficiency. J Clin Endocrinol Metab 76:574 –579
Radetti G, Buzi F, Paganini C, Pilotta A, Felappi B 2003 Treatment of GHdeficient children with two different GH doses: effect on final height and
cost-benefit implications. Eur J Endocrinol 148:515–518
Cohen P, Bright GM, Rogol AD, Kappelgaard AM, Rosenfeld RG 2002
Effects of dose and gender on the growth and growth factor response to GH
in GH-deficient children: implications for efficacy and safety. J Clin Endocrinol
Metab 87:90 –98
Sulmont V, Brauner R, Fontoura M, Rappaport R 1990 Response to growth
hormone treatment and final height after cranial or craniospinal irradiation.
Acta Paediatr Scand 79:542–549
Carel JC, Ecosse E, Nicolino M, Tauber M, Leger J Cabrol ST, Bastie-Sigeac
I, Chaussain JL, Coste J 2002 Adult height after long term treatment with
recombinant growth hormone for idiopathic isolated growth hormone deficiency: observational follow up study of the French population based registry.
BMJ 325:70 –76
Ranke MB, Price DA, Albertsson-Wikland K, Maes M, Lindberg A 1997
Factors determining pubertal growth and final height in growth hormone
treatment of idiopathic growth hormone deficiency. Analysis of 195 patients
of the Kabi Pharmacia International Growth Study. Horm Res 48:62–71
Sklar C, Mertens A, Walter A, Mitchell D, Nesbit M, O’Leary M, Hutchinson
R, Meadows A, Robison L 1993 Final height after treatment for childhood
acute lymphoblastic leukemia: comparison of no cranial irradiation with 1800
and 2400 centigrays of cranial irradiation. J Pediatr 123:59 – 64
Oberfield SE, Soranno D, Nirenberg A, Heller G, Allen JC, David R, Levine
LS, Sklar CA 1996 Age at onset of puberty following high-dose central nervous
system radiation therapy. Arch Pediatr Adolesc Med 150:589 –592
Klein KO, Barnes KM, Jones JV, Feuillan PP, Cutler Jr GB 2001 Increased
final height in precocious puberty after long-term treatment with LHRH ago-
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 14:55 For personal use only. No other uses without permission. . All rights reserved.
Brownstein et al. • Height in GH-Treated Childhood Cancer Survivors
28.
29.
30.
31.
32.
33.
34.
35.
nists: the National Institutes of Health experience. J Clin Endocrinol Metab
86:4711– 4716
Mericq MV, Eggers M, Avila A, Cutler Jr GB, Cassorla F 2000 Near final
height in pubertal growth hormone (GH)-deficient patients treated with GH
alone or in combination with luteinizing hormone-releasing hormone analog:
results of a prospective, randomized trial. J Clin Endocrinol Metab 85:569 –573
Mul D, Wit JM, Oostdijk W, Van den Broeck J 2001 The effect of pubertal
delay by GnRH agonist in GH-deficient children on final height. J Clin Endocrinol Metab 86:4655– 4656
Saggese G, Federico G, Barsanti S, Fiore L 2001 The effect of administering
gonadotropin-releasing hormone agonist with recombinant-human growth
hormone (GH) on the final height of girls with isolated GH deficiency: results
from a controlled study. J Clin Endocrinol Metab 86:1900 –1904
Yanovski JA, Rose SR, Municchi G, Pescovitz OH, Hill SC, Cassorla FG,
Cutler Jr GB 2003 Treatment with a luteinizing hormone-releasing hormone
agonist in adolescents with short stature. N Engl J Med 348:908 –917
Clayton PE, Shalet SM, Morris-Jones PH, Price DA 1988 Growth in children
treated for acute lymphoblastic leukaemia. Lancet 1:460 – 462
Caruso-Nicoletti M, Mancuso M, Spadaro G, Dibenedetto SP, DiCataldo A,
Schiliro G 1993 Growth and growth hormone in children during and after
therapy for acute lymphoblastic leukaemia. Eur J Pediatr 152:730 –733
Cicognani A, Cacciari E, Rosito P, Mancini AF, Carla G, Mandini M, Paolucci
G 1994 Longitudinal growth and final height in long-term survivors of childhood leukaemia. Eur J Pediatr 153:726 –730
Mohnike K, Dorffel W, Timme J, Kluba U, Aumann V, Vorwerk P, Mittler
J Clin Endocrinol Metab, September 2004, 89(9):4422– 4427 4427
36.
37.
38.
39.
40.
41.
42.
U 1997 Final height and puberty in 40 patients after antileukaemic treatment
during childhood. Eur J Pediatr 156:272–276
Gurney JG, Ness KK, Stovall M, Wolden S, Punyko JA, Neglia JP, Mertens
AC, Packer RJ, Robison LL, Sklar CA 2003 Final height and body mass index
among adult survivors of childhood brain cancer: Childhood Cancer Survivor
Study. J Clin Endocrinol Metab 88:4731– 4739
Rappaport R, Brauner R 1989 Growth and endocrine disorders secondary to
cranial irradiation. Pediatr Res 25:561–567
Pertzelan A, Kauli R, Assa S, Greenberg D, Laron Z 1976 Intermittent treatment with human growth hormone (GH) in isolated GH deficiency and in
multiple pituitary hormone deficiencies. Clin Endocrinol (Oxf) 5:15–24
Swerdlow AJ, Reddingius RE, Higgins CD, Spoudeas HA, Phipps K, Qiao
Z, Ryder WD, Brada M, Hayward RD, Brook CG, Hindmarsh PC, Shalet SM
2000 Growth hormone treatment of children with brain tumors and risk of
tumor recurrence. J Clin Endocrinol Metab 85:4444 – 4449
Packer RJ, Boyett JM, Janss AJ, Stavrou T, Kun LE, Wisoff J, Russo C, Geyer
R, Phillips P, Kieran M, Greenber M, Goldman S, Hyder D, Heideman R,
Jones-Wallace D, August GP, Smith SH, Moshang T 2001 Growth hormone
replacement therapy in children with medulloblastoma: use and effect on
tumor control. J Clin Oncol 19:480 – 487
Chan JM, Stampfer MJ, Ma J, Gann P, Gaziano JM, Giovannucci E 1998
Plasma insulin-like growth factor-I and prostate cancer risk: a prospective
study. Science 279:563–566
Hankinson SE, Willett WC, Colditz GA, Hunter DJ, Michaud DS, Deroo B,
Rosner B, Speizer FE, Pollak M 1998 Circulating concentrations of insulin-like
growth factor-I and risk of breast cancer. Lancet 351:1393–1396
JCEM is published monthly by The Endocrine Society (http://www.endo-society.org), the foremost professional society serving the
endocrine community.
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 14:55 For personal use only. No other uses without permission. . All rights reserved.