Nancy Bouchard DDS, MHP
advertisement

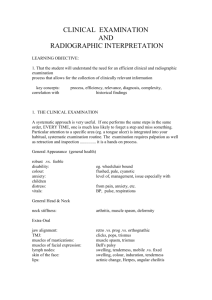
Nancy Bouchard DDS, MHP RADIATION SAFETY Operator Safety Patient Safety Maximum Permissible Dose: 2rem/year ALARA: As Low As Reasonably Achievable 1) Do Not Take Films When Pregnant 1) Take Films by Prescription: Only When Necessary 2) Do Not Hold the Film in the Patient’s Mouth 3) Achieve Certification and Continuing Education 2) Use Fast Speed Film 3) Use Proper Processing Procedures and Adhere to Quality Assurance Measures 4) Wear Radiation Badges 5) Install Adequate Barriers: Lead Lined Walls, Leaded Windows, Adequately Thick Cement or Brick Walls Movable Lead Barriers 6) Obey the Position and Distance Rule: 6 Feet from the Patient 90º - 135º to the Central Beam 4) Place Lead Apron and Thyroid Collar on Every Patient 5) Have Adequate Filtration 6) Use Collimation Patient Category Child Primary Dentition (prior to eruption of first permanent tooth) New Patient Posterior bitewing examination if proximal surfaces of primary teeth cannot be visualized or probed All new patients to assess dental diseases and growth and development Recall Patient Adolescent Adult Transitional Dentition (following eruption of permanent tooth Permanent Dentition (prior to eruption of third molars) Dentate Individualized radiographic examination consisting of periapical/occlusal views and posterior bitewings or panoramic examination and posterior bitewings Individualized radiographic examination consisting of posterior bitewings and selected periapicals. A full mouth intraoral radiographic examination is appropriate when the patient presents with clinical evidence of generalized dental disease or a history of extensive dental treatment. Full mouth intraoral radiographic examination or panoramic examination Posterior bitewing examination at 6-month intervals or until no carious lesions are evident Posterior bitewing Posterior bitewing examination at 6-to 12examination at12-to 18month intervals or until no month intervals carious lesions are evident Not applicable Posterior bitewing Posterior bitewing examination at 12-to 24- examination at12-to 24month intervals if proximal month intervals surfaces of primary teeth cannot be visualized or probe Posterior bitewing examination at 18-to 36month intervals Posterior bitewing examination at24-to 36month Intervals Not applicable Individualized radiographic examination consisting of selected periapical and/or bitewing radiographs for areas where periodontal disease (other than nonspecific gingivitis) can be demonstrated clinically Not applicable Periapical or panoramic examination to assess developing third molars Usually not indicated Clinical caries or high-risk factors for caries** No clinical caries and no high-risk factors for caries** Periodontal disease or a Individualized radiographic examination consisting of selected periapical and/or bitewing radiographs for history of periodontal areas where periodontal disease (other than nonspecific treatment gingivitis) can be demonstrated clinically Growth and development assessment Usually not indicated /www.fda.gov/cdrh/radhealth/adaxray-1.html Individualized radiographic examination consisting of a periapical/occlusal or panoramic examination Usually not indicated Edentulous EQUIVALENT BACKGROUND EXPOSURE FROM DENTAL RADIOGRAPHY EXAMINATION FULL MOUTH (20 films) BITEWINGS (4 films) Panoramic FILM COLLIMATION D Round E Round D Rectangular E Rectangular D Round E Round D Rectangular E Rectangular Rare Earth Tungstate Screens BACKGROUND EQUIVALENT 10 days 5 days 4 days 2 days 2 days 1 day 1 day 10 hours 10 hours Background Radiation (or Natural) Largest contributor 83% of the radiation exposure of people living in the United States today -3.6 mSV per year EXTERNAL SOURCES: cosmic (e.g.: altitude, airline travel) and terrestrial (that found in soil) radiation or that originating from the environment. INTERNAL SOURCES: radionuclides that are taken up from the external environment by inhalation and ingestion (e.g.: radon) Artificial Radiation: Medical diagnosis and treatment Consumer and industrial products (i.e. televisions and airport inspection systems) LEVELS OF RISK FOR X-RAY EXAMINATIONS X-Ray Exam Equivalent Period of Natural Background Radiation Lifetime Additional Risk of Cancer per Examination Chest / Teeth / Hands and Feet A few days Skull / Head / Neck A few weeks Breast / Hip / Spine / CT Scan of Head / Lung Isotope Kidneys and Bladder / Colon—Barium Enema / CT Scan of Chest A few months to a year NEGLIGIBLE Less than 1 in 1,000,000 MINIMAL 1 in 1,000,000 to 1 in 100,000 VERY LOW 1 in 100,000 to 1 in 10,000 A few years LOW RISK 1 in 10,000 to 1 in 1,000 DENTAL RADIOGRAPH EXPOSURE mSV Bitewings (4 films) Full-mouth series (about 19 films) Panorex (panoramic jaw film) 0.038 MEDICAL RADIOGRAPHS EXPOSURE mSV Lower GI series Upper GI series Chest Average radiation from outer space in Denver, CO (per year) Average radiation in the U.S. from Natural sources (per year) 4.060 0.150 0.019 2.440 0.080 0.510 3.600 Radiographic Interpretation When interpreting radiographs, remember that we are viewing a two-dimensional picture of a three-dimensional object. Therefore, some items which are in front of or behind the object may not show on the radiograph; some items may make the object appear different than expected. For instance, imagine that the tooth is a box: If the x-ray beam strikes the tooth/box straight on, there will only be one shade on the film. If the x-ray beam is not parallel to the tooth/box or If the tooth is misaligned, then the edges of the tooth/ the corners of the box will appear more radiolucent on the film because there is less material for the beam to go through. Cervical Burnout This is diffuse radiolucent areas with ill-defined borders in the area of the CEJ. These shadows are caused from the contrast of adjacent materials (enamel, bone, metals). When the x-ray beam hits all these materials, the photons bounce and seek a less dense area or an opening to go through. The area then appears dark. CARIES Occlusal decay is not seen on radiographs unless it is large due to the thickness of the enamel. Interproximal decay is found right in the contact area. Do not look more coronally as the cusps may appear like decay. Root decay is difficult to distinguish from cervical burnout. First, check if there is any bone loss. If there is not, any shadow see at the cervical area is probably burnout. Root caries appear as defined, half-moon shaped shadows. Long vertical shadows are often cervical burnout or the grooves of the roots. PERIODONTAL EVALUATION When we examine radiographs, we estimate the periodontal support of the teeth. This will be an approximation because we are viewing the teeth on the film and not in their three-dimensional space. Lamina Dura / Periodontal Ligament Space The lamina dura is a white line around the roots of the teeth. The periodontal ligament space is radiolucent. When either appears thickened, it may be a sign of occlusal trauma. Crestal Irregularities The crest of alveolar bone between teeth should appear solid sometimes having a white line. There should be no loss of density at the ridge. When the crest appears thin, has lost its whiteness, or has cupping, then the bone is undergoing breakdown the day the radiograph was taken. This is NOT an indication of the severity of loss. Someone who has no bone loss may exhibit crestal irregularities if the bone is beginning to break down. Someone who has bone loss may show solid crestal bone is he/she has had corrective treatment and has been seeking adequate maintenance. Severity of Bone Loss 20 % bone loss from the CEJ to the apex = slight 30% bone loss from the CEJ to the apex = moderate 40 % bone loss from the CEJ to the apex = severe What is moderate on one tooth may be severe on another. Type of Bone Loss Comparing the bone to the CEJs, horizontal bone loss is when adjacent teeth have lost the same amount of bone; vertical loss is when adjacent teeth have differing amounts of loss. Calculus Appears as radiopaque spicules or spurs in the interproximal regions or as a line along the CEJ region on mandibular anteriors when there is a ridge present. Furcations There is a radiolucency in the furcation area. slight moderate severe