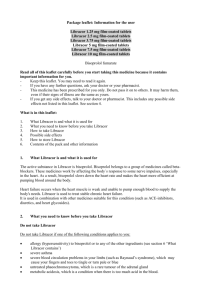
Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film
advertisement

UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 BISOPROLOL 1.25 MG, 2.5 MG, 3.75 MG, 5 MG, 7.5 MG AND 10 MG FILM-COATED TABLETS PL 21880/0127-32 UKPAR TABLE OF CONTENTS Lay Summary Page 2 Scientific discussion Page 3 Steps taken for assessment Page 12 Steps taken after authorisation – summary Page 13 Summary of Product Characteristics Page 14 Product Information Leaflet Page 62 Labelling Page 64 1 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 BISOPROLOL 1.25 MG, 2.5 MG, 3.75 MG, 5 MG, 7.5 MG AND 10 MG FILM-COATED TABLETS PL 21880/0127-32 LAY SUMMARY On 6th August 2012, the MHRA granted Medreich PLC Marketing Authorisations (licences) for Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets. Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets contain the active ingredient, bisoprolol fumarate. Bisoprolol belongs to a group of medicines called beta-blockers. Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets are used to treat stable chronic heart failure. It is used in combination with other medicines suitable for this condition (such as ACE (angiotensin-converting-enzyme) inhibitors, diuretics and heart glycosides). Heart failure occurs when the heart muscle is weak and unable to pump enough blood to supply the body’s needs. Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets work by affecting the body's response to some nerve impulses, especially in the heart. As a result, bisoprolol slows down the heart rate and makes the heart more efficient at pumping blood around the body. No new or unexpected safety concerns arose from these applications and it was, therefore, judged that the benefits of taking Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets outweigh the risks; hence Marketing Authorisations have been granted. 2 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 BISOPROLOL 1.25 MG, 2.5 MG, 3.75 MG, 5 MG, 7.5 MG AND 10 MG FILM-COATED TABLETS PL 21880/0127-32 SCIENTIFIC DISCUSSION TABLE OF CONTENTS Introduction Page 4 Pharmaceutical assessment Page 5 Non-clinical assessment Page 8 Clinical assessment (including statistical assessment) Page 9 Overall conclusions and risk benefit assessment Page 11 3 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 INTRODUCTION The UK granted Medreich PLC Marketing Authorisations for the medicinal products Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets (PL 21880/0127-32) on 6th August 2012. Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets are prescription only medicines (POM) and are indicated for the treatment of stable chronic heart failure with reduced systolic left ventricular function in addition to ACE inhibitors, and diuretics, and optionally cardiac glycosides These applications for Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets are submitted under Article 10.1 of Directive 2001/83/EC, claiming to be generic medicinal products to Cardicor 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets, authorised in the UK to E Merck Limited on 24th December 1999 (PL 00493/0179-84). These licences underwent changes of ownership to Merck Serono Limited on 2nd February 2010 (PL 11648/0071-6). Bisoprolol is a highly beta1-selective-adrenoceptor blocking agent, lacking intrinsic sympathomimetic and relevant membrane stabilising activity. It only shows low affinity to the beta2-receptor of the smooth muscles of bronchi and vessels as well as to the beta2receptors concerned with metabolic regulation. 4 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 PHARMACEUTICAL ASSESSMENT DRUG SUBSTANCE INN: Bisoprolol fumarate Chemical name: (RS)-1-[4-[[2-(1-Methylethoxy) ethoxy] methyl] phenoxy]-3-[(1methylethyl) amino] propan-2-ol fumarate Structure: Physical form: A white or almost white, slightly hygroscopic powder. Solubility: Very soluble in water and in methanol. Freely soluble in alcohol. Molecular formula: Molecular weight: C40H66N2O12 767 The bisoprolol fumarate used in the product complies with its European Pharmacopoeia monographs. The manufacturer of the drug substance holds a valid EDQM (European Directorate for the Quality of Medicines and Healthcare) Certificate of Suitability. The quality of the substance is suitably controlled in line with the current edition of the European Pharmacopoeia Monograph for bisprolol fumarate. The manufacturing process, control of materials, control of critical steps, validation and process development for bisprolol fumarate were assessed and approved by the EDQM in relation to the granting of the Certificate of Suitability and are therefore satisfactory. An appropriate specification with suitable test methods and limits has been provided for the drug substance. The methods of testing and limits for residual solvents are in compliance with current guidelines. Batch analysis data are provided and comply with the proposed specifications. Suitable specifications have been provided for all packaging used. The primary packaging has been shown to comply with current guidelines. Stability studies have been performed with the drug substance and no significant changes were observed. On the basis of the results, a suitable re-test period could be approved. 5 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 DRUG PRODUCT Other ingredients Other ingredients are pharmaceutical excipients microcrystalline cellulose (PH-102), maize starch, crospovidone (Type B), colloidal anhydrous silica, magnesium stearate, purified water, hypromellose, macrogol 400 and titanium dioxide. Bisoprolol 3.75 mg, 5 mg, 7.5 mg film-coated Tablets have the additional excipient ferric oxide yellow (E172). Bisoprolol 10 mg film-coated Tablets has the additional excipients ferric oxide yellow (E172) and ferric oxide red (E172). With the exception of ferric oxide yellow (E172) and ferric oxide red (E172), all the ingredients comply with their relevant European Pharmacopoeia monographs. Ferric oxide yellow (E172) and ferric oxide red (E172) comply with the United States Pharmacopoeia – National Forumulary. None of the excipients used contain material of animal or human origin. The magnesium stearate used in this product is of plant origin. Pharmaceutical Development The objective of the development programme was to produce safe, efficacious products containing bisoprolol fumarate that could be considered generic medicinal products of Cardicor 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets. Suitable product development information has been provided. Valid justifications for the use and amounts of each excipient have been provided. Comparative in vitro dissolution and impurity profiles have been provided for the proposed and reference products. Manufacturing Process Satisfactory batch formulae has been provided for the manufacture of the products, along with an appropriate account of the manufacturing process. The manufacturing process has been validated and has shown satisfactory results. In-process controls are satisfactory based on batch data and controls on the finished products. Process validation data on commercial-scale batches of each strength have been provided and are satisfactory. Finished Product Specification The finished product specifications are acceptable. Test methods have been described and adequately validated, as appropriate. Batch data have been provided and comply with the release specifications. Certificates of Analysis have been provided for any working standards used. Container-Closure System The products are packaged in blisters composed of aluminium, polyvinyl chloride (PVC) and polyvinylidene chloride (PVdC). The blisters are packed in cartons. Pack sizes are 20, 28, 30, 50, 56, 60, 90 and 100 film-coated tablets. Not all pack sizes are marketed. Satisfactory specifications and Certificates of Analysis have been provided for all packaging components. All primary product packaging complies with current legislation and the EU directives regarding contact with food stuffs. 6 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Stability of the product Stability studies were performed on batches of the finished products in the packaging proposed for marketing and in accordance with current guidelines. These data support a shelf-life of 24 months with no special requirements for storage. Summary of Product Characteristics (SmPCs), Patient Information Leaflet (PIL) and Labelling The SmPCs, PIL and labelling are pharmaceutically acceptable. The UK approved SmPCs, PIL and labelling are included in modules 2, 3 and 4 of this report. User testing results have been submitted for the PIL for these products. The results indicate that the PIL is in accordance with Article 59 of Council Directive 2001/83/EC, as amended and is well-structured and organised, easy to understand and written in a comprehensive manner. The test shows that the patients/users are able to act upon the information that it contains. MAA Forms These are pharmaceutically satisfactory. Quality Overall Summary The quality overall summary has been written by an appropriately qualified person and is a suitable summary of the pharmaceutical dossier. Conclusion From a quality point of view, it is recommended that Marketing Authorisations are granted for these applications. 7 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 NON-CLINICAL ASSESSMENT The pharmacodynamics, pharmacokinetics and toxicological properties of bisoprolol fumarate are well-known. As bisoprolol fumarate is a widely used, well-known drug substance, no new non-clinical data have been provided and none are required. An overview based on literature is therefore appropriate. Non-Clinical Overview The non-clinical overview has been written by an appropriately qualified person and is a suitable summary of the non-clinical aspects of the dossier. Environmental Risk Assessment A satisfactory justification for the absence of an Environmental Risk Assessment was provided. Conclusion From a non-clinical point of view, it is recommended that Marketing Authorisations are granted for these applications. 8 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 CLINICAL ASSESSMENT CLINICAL PHARMACOLOGY To support the applications, a single bioequivalence study has been provided: A single dose, two-period, crossover bioequivalence study comparing the pharmacokinetics of the test product Bisoprolol 10 mg film-coated Tablets versus the reference product Cardicor (bisoprolol fumarate) 10 mg film-coated Tablets (Merck Serono) in healthy volunteers under fasted conditions. Blood sampling was performed pre-dose and up to 72 hours post dose in each treatment period. There was a washout period of 8 days. Pharmacokinetic parameters were calculated and statistically analysed. Results from this study are presented below as log-transformed values: Geometric Least Mean Squares and 90% Confidence Interval Pharmacokinetic parameters of bisoprolol fumarate Treatment AUC0-t AUC0-∞ (ng.hr/ml) (ng.hr/ml) Cmax (ng/ml) 571.098 582.449 36.257 36.971 Test Reference 585.682 598.095 98.1 97.9 98.1 94.08 – 102.18 94.03 – 101.98 94.47 – 101.81 area under the plasma concentration-time curve from time zero to infinity area under the plasma concentration-time curve from time zero to t hours maximum plasma concentration Ratio (90% CI) AUC0-∞ AUC0-t Cmax The results for the primary variables indicated that the 90% confidence intervals test/reference ratio of geometric means for AUC0-t and Cmax for bisoprolol fumarate lie within the normal 80-125% limits. Thus, bioequivalence has been shown between the test and reference products. The applicant provided a satisfactory justification for the application of a biowaiver for the other strengths, which was accepted. Therefore, the results and conclusions of the bioequivalence study on the 10 mg tablet strength can be extrapolated to Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg and 7.5 mg film-coated Tablets. Efficacy These are generic applications based on demonstration of bioequivalence and new data relating to efficacy are not required as per EU legislation once bioequivalence has been demonstrated. Safety With the exception of the data submitted during the bioequivalence study, no new safety data were submitted with these generic applications and none were required. No new or unexpected safety concerns were raised during the bioequivalence study. 9 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 The Pharmacovigilance System and the Risk Management Plan The pharmacovigilance system as described by the Marketing Authorisation Holder (MAH) fulfils the requirements and provides adequate evidence that the MAH has the services of a qualified person responsible for pharmacovigilance and has the necessary means for the notification of any adverse reaction suspected of occurring. A satisfactory justification for the absence of a Risk Management Plan has been provided. Summary of Product Characteristics (SmPCs), Patient Information Leaflet (PIL) and Labelling The SmPCs, PIL and labelling are clinically satisfactory and consistent with those for the reference products. MAA Forms The MAA forms are clinically satisfactory. Clinical Overview The clinical overview has been written by a suitably qualified person and is satisfactory. Conclusion The bioequivalence study has shown that Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets can be considered as generic medicinal products to the reference products Cardicor 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets. From a clinical point of view, it is recommended that Marketing Authorisations are granted for these applications. 10 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 OVERALL CONCLUSIONS AND RISK BENEFIT ASSESSMENT QUALITY The important quality characteristics of Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg film-coated Tablets are well-defined and controlled. The specifications and batch analytical results indicate consistency from batch to batch. There are no outstanding quality issues that would have a negative impact on the benefit/risk balance. NON-CLINICAL No new non-clinical data were submitted and none are required for applications of this type. EFFICACY Bioequivalence has been demonstrated between the applicant’s Bisoprolol 10 mg film-coated Tablets and the reference product, Cardicor 10 mg film-coated Tablets. This conclusion can be extrapolated to Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg and 7.5 mg film-coated Tablets. No new or unexpected safety concerns arise from these applications. The SmPCs, PIL and labelling are satisfactory and consistent with those for the reference products. RISK BENEFIT ASSESSMENT The quality of the products is acceptable and no new non-clinical or clinical safety concerns have been identified. The bioequivalence studies support the claim that the applicant’s products and the reference products are interchangeable. Clinical experience with bisoprolol fumarate is considered to have demonstrated the therapeutic value of the compound. The benefit/risk is, therefore, considered to be positive. 11 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 BISOPROLOL 1.25 MG, 2.5 MG, 3.75 MG, 5 MG, 7.5 MG AND 10 MG FILM-COATED TABLETS PL 21880/0127-32 STEPS TAKEN FOR ASSESMENT 1 The MHRA received the Marketing Authorisation Applications on 9th June 2011. 2 Following standard checks and communication with the applicant the MHRA considered the applications valid on 7th July 2011. 3 The applicant responded to the MHRA’s requests, providing further information on 13th July 2012 and 30th July 2012 for the quality section. The applicant responded to the MHRA’s requests, providing further information on 1st June 2012 and 8th June 2012 for the clinical section. 4 The applications were determined on 6th August 2012. 12 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 BISOPROLOL 1.25 MG, 2.5 MG, 3.75 MG, 5 MG, 7.5 MG AND 10 MG FILM-COATED TABLETS PL 21880/0127-32 STEPS TAKEN AFTER AUTHORISATION - SUMMARY Date Application submitted type Scope Outcome 13 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 SUMMARY OF PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT Bisoprolol 1.25mg film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each Film coated tablet contains Bisoprolol Fumarate 1.25mg For list of excipients refer 6.1 3 PHARMACEUTICAL FORM Film-coated tablet. White colored round, biconvex, film coated tablets, plain on both sides 4 4.1 CLINICAL PARTICULARS THERAPEUTIC INDICATIONS Treatment of stable chronic heart failure with reduced systolic left ventricular function in addition to ACE inhibitors, and diuretics, and optionally cardiac glycosides (for additional information see section 5.1). 4.2 POSOLOGY AND METHOD OF ADMINISTRATION Standard treatment of CHF consists of an ACE inhibitor (or an angiotensin receptor blocker in case of intolerance to ACE inhibitors), a beta-blocker, diuretics, and when appropriate cardiac glycosides. Patients should be stable (without acute failure) when bisoprolol treatment is initiated. It is recommended that the treating physician should be experienced in the management of chronic heart failure. Transient worsening of heart failure, hypotension, or bradycardia may occur during the titration period and thereafter. Titration phase The treatment of stable chronic heart failure with bisoprolol requires a titration phase The treatment with bisoprolol is to be started with a gradual uptitration according to the following steps: - 1.25 mg once daily for 1 week, if well tolerated increase to - 2.5 mg once daily for a further week, if well tolerated increase to - 3.75 mg once daily for a further week, if well tolerated increase to - 5 mg once daily for the 4 following weeks, if well tolerated increase to - 7.5 mg once daily for the 4 following weeks, if well tolerated increase to - 10 mg once daily for the maintenance therapy. The maximum recommended dose is 10 mg once daily. Close monitoring of vital signs (heart rate, blood pressure) and symptoms of worsening heart failure is recommended during the titration phase. Symptoms may already occur within the first day after initiating the therapy. Treatment modification If the maximum recommended dose is not well tolerated, gradual dose reduction may be considered. In case of transient worsening of heart failure, hypotension, or bradycardia reconsideration of the dosage of the concomitant medication is recommended. It may also be necessary to temporarily lower the dose of bisoprolol or to consider discontinuation. The reintroduction and/or uptitration of bisoprolol should always be considered when the patient becomes stable again. If discontinuation is considered, gradual dose decrease is recommended, since abrupt withdrawal may lead to acute deterioration of the patients condition. Treatment of stable chronic heart failure with bisoprolol is generally a long-term treatment. 14 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Administration Bisoprolol tablets should be taken in the morning and can be taken with food. They should be swallowed with liquid and should not be chewed. Special population Renal or hepatic impairment There is no information regarding pharmacokinetics of bisoprolol in patients with chronic heart failure and with impaired hepatic or renal function. Uptitration of the dose in these populations should therefore be made with additional caution. Elderly No dosage adjustment is required. Children There is no paediatric experience with bisoprolol, therefore its use cannot be recommended for children. 4.3 CONTRAINDICATIONS Bisoprolol is contraindicated in chronic heart failure patients with: - acute heart failure or during episodes of heart failure decompensation requiring i.v. inotropic therapy - cardiogenic shock - second or third degree AV block (without a pacemaker) - sick sinus syndrome - sinoatrial block - bradycardia with less than 60 beats/min before the start of therapy - hypotension (systolic blood pressure less than 100 mm Hg) - severe bronchial asthma or severe chronic obstructive pulmonary disease - late stages of peripheral arterial occlusive disease and Raynaud's syndrome - untreated phaeochromocytoma (see 4.4) - metabolic acidosis - hypersensitivity to bisoprolol or to any of the excipients 4.4 SPECIAL WARNINGS AND PRECAUTIONS FOR USE Bisoprolol must be used with caution in: - bronchospasm (bronchial asthma, obstructive airways diseases) - diabetes mellitus with large fluctuations in blood glucose values; symptoms of hypoglycaemia can be masked - strict fasting - ongoing desensitisation therapy - first degree AV block - Prinzmetal’s angina - peripheral arterial occlusive disease (intensification of complaints might happen especially during the start of therapy) - general anaesthesia In patients undergoing general anaesthesia beta-blockade reduces the incidence of arrhythmias and myocardial ischemia during induction and intubation, and the post-operative period. It is currently recommended that maintenance beta-blockade be continued peri-operatively. The anaesthesist must be aware of beta-blockade because of the potential for interactions with other drugs, resulting in bradyarrhythmias, attenuation of the reflex tachycardia and the decreased reflex ability to compensate for blood loss. If it is thought necessary to withdraw beta-blocker therapy before surgery, this should be done gradually and completed about 48 hours before anaesthesia. There is no therapeutic experience of bisoprolol treatment of heart failure in patients with the following diseases and conditions: - insulin dependent diabetes mellitus (type I) - severely impaired renal function - severely impaired hepatic function - restrictive cardiomyopathy 15 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 - congenital heart disease - haemodynamically significant organic valvular disease - myocardial infarction within 3 months Combination of bisoprolol with calcium antagonists of the verapamil or diltiazem type, with Class I antiarrhytmic drugs and with centrally acting antihypertensive drugs is generally not recommended, for details please refer to section 4.5. In bronchial asthma or other chronic obstructive lung diseases, which may cause symptoms, bronchodilating therapy should be given concomitantly. Occasionally an increase of the airway resistance may occur in patients with asthma, therefore the dose of beta2-stimulants may have to be increased. As with other beta-blockers, bisoprolol may increase both the sensitivity towards allergens and the severity of anaphylactic reactions. Adrenaline treatment does not always give the expected therapeutic effect. Patients with psoriasis or with a history of psoriasis should only be given beta-blockers (e.g. bisoprolol) after carefully balancing the benefits against the risks. In patients with phaeochromocytoma bisoprolol must not be administered until after alpha-receptor blockade. Under treatment with bisoprolol the symptoms of a thyreotoxicosis may be masked. The initiation of treatment with bisoprolol necessitates regular monitoring. For the posology and method of administration please refer to section 4.2. The cessation of therapy with bisoprolol should not be done abruptly unless clearly indicated. For further information please refer to section 4.2. 4.5 INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION Combinations not recommended Calcium antagonists of the verapamil type and to a lesser extent of the diltiazem type: Negative influence on contractility and atrio-ventricular conduction. Intravenous administration of verapamil in patients on β-blocker treatment may lead to profound hypotension and atrioventricular block. Class I antiarrhythmic drugs (e.g. quinidine, disopyramide; lidocaine, phenytoin; flecainide, propafenone): Effect on atrio-ventricular conduction time may be potentiated and negative inotropic effect increased. Centrally acting antihypertensive drugs such as clonidine and others (e.g. methyldopa, moxonodine, rilmenidine): Concomitant use of centrally acting antihypertensive drugs may worsen heart failure by a decrease in the central sympathetic tonus (reduction of heart rate and cardiac output, vasodilation). Abrupt withdrawal, particularly if prior to beta-blocker discontinuation, may increase risk of “rebound hypertension”. Combinations to be used with caution Calcium antagonists of the dihydropyridine type such as felodipine and amlodipine: Concomitant use may increase the risk of hypotension, and an increase in the risk of a further deterioration of the ventricular pump function in patients with heart failure cannot be excluded. Class-III antiarrhythmic drugs (e.g. amiodarone): Effect on atrio-ventricular conduction time may be potentiated. Topical beta-blockers (e.g. eye drops for glaucoma treatment) may add to the systemic effects of bisoprolol. Parasympathomimetic drugs: Concomitant use may increase atrio-ventricular conduction time and the risk of bradycardia. 16 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Insulin and oral antidiabetic drugs: Intensification of blood sugar lowering effect. Blockade of betaadrenoreceptors may mask symptoms of hypoglycaemia. Anaesthetic agents: Attenuation of the reflex tachycardia and increase of the risk of hypotension (for further information on general anaesthesia see also section 4.4.). Digitalis glycosides: Reduction of heart rate, increase of atrio-ventricular conduction time. Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs may reduce the hypotensive effect of bisoprolol. β-Sympathomimetic agents (e.g. isoprenaline, dobutamine): Combination with bisoprolol may reduce the effect of both agents. Sympathomimetics that activate both β- and α-adrenoceptors (e.g. noradrenaline, adrenaline): Combination with bisoprolol may unmask the α-adrenoceptor-mediated vasoconstrictor effects of these agents leading to blood pressure increase and exacerbated intermittent claudication. Such interactions are considered to be more likely with nonselective β-blockers. Concomitant use with antihypertensive agents as well as with other drugs with blood pressure lowering potential (e.g. tricyclic antidepressants, barbiturates, phenothiazines) may increase the risk of hypotension. Combinations to be considered Mefloquine: increased risk of bradycardia Monoamine oxidase inhibitors (except MAO-B inhibitors): Enhanced hypotensive effect of the betablockers but also risk for hypertensive crisis. 4.6 PREGNANCY AND LACTATION Pregnancy: Bisoprolol has pharmacological effects that may cause harmful effects on pregnancy and/or the fetus/newborn. In general, beta-adrenoceptor blockers reduce placental perfusion, which has been associated with growth retardation, intrauterine death, abortion or early labour. Adverse effects (e.g. hypoglycaemia and bradycardia) may occur in the fetus and newborn infant. If treatment with betaadrenoceptor blockers is necessary, beta1-selective adrenoceptor blockers are preferable. Bisoprolol should not be used during pregnancy unless clearly necessary. If treatment with bisoprolol is considered necessary, the uteroplacental blood flow and the fetal growth should be monitored. In case of harmful effects on pregnancy or the fetus alternative treatment should be considered. The newborn infant must be closely monitored. Symptoms of hypoglycaemia and bradycardia are generally to be expected within the first 3 days. Lactation: It is not known whether this drug is excreted in human milk. Therefore, breastfeeding is not recommended during administration of bisoprolol. Fertility: In reproduction toxicology studies Bisoprolol had no influence on fertility or on general reproduction performance (see section 5.3). 4.7 EFFECTS ON ABILITY TO DRIVE AND USE MACHINES In a study with coronary heart disease patients bisoprolol did not impair driving performance. However, due to individual variations in reactions to the drug, the ability to drive a vehicle or to operate machinery may be impaired. This should be considered particularly at start of treatment and upon change of medication as well as in conjunction with alcohol. 4.8 UNDESIRABLE EFFECTS The following definitions apply to the frequency terminology used hereafter: Very common ( 1/10) Common ( 1/100, < 1/10) Uncommon ( 1/1,000, < 1/100) Rare ( 1/10,000, < 1/1,000) Very rare (< 1/10,000) 17 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Cardiac disorders: Very common: bradycardia. Common: worsening of heart failure. Uncommon: AV-conduction disturbances. Investigations: Rare: increased triglycerides, increased liver enzymes (ALAT, ASAT). Nervous system disorders: Common: dizziness, headache. Eye disorders: Rare: reduced tear flow (to be considered if the patient uses lenses). Very rare: conjunctivitis. Ear and labyrinth disorders: Rare: hearing impairment. Respiratory, thoracic and mediastinal disorders: Uncommon: bronchospasm in patients with bronchial asthma or a history of obstructive airways disease. Rare: allergic rhinitis. Gastrointestinal disorders: Common: gastrointestinal complaints such as nausea, vomiting, diarrhoea, constipation. Skin and subcutaneous tissue disorders: Rare: hypersensitivity reactions (itching, flush, rash). Very rare: beta-blockers may provoke or worsen psoriasis or induce psoriasis-like rash, alopecia. Musculoskeletal and connective tissue disorders: Uncommon: muscular weakness and cramps. Vascular disorders: Common: feeling of coldness or numbness in the extremities, hypotension. Uncommon: orthostatic hypotension. General disorders: Common: asthenia, fatigue. Hepatobiliary disorders: Rare: hepatitis. Reproductive system and breast disorders: Rare: potency disorders. Psychiatric disorders: Uncommon: sleep disorders, depression. Rare: nightmares, hallucinations. 4.9 OVERDOSE With overdose (e.g. daily dose of 15 mg instead of 7.5 mg) third degree AV-block, bradycardia, and dizziness have been reported. In general the most common signs expected with overdosage of a betablocker are bradycardia, hypotension, bronchospasm, acute cardiac insufficiency and hypoglycaemia. To date a few cases of overdose (maximum: 2000 mg) with bisoprolol have been reported in patients suffering from hypertension and/or coronary heart disease showing bradycardia and/or hypotension; all patients recovered. There is a wide interindividual variation in sensitivity to one single high dose of bisoprolol and patients with heart failure are probably very sensitive. Therefore it is mandatory to initiate the treatment of these patients with a gradual uptitration according to the scheme given in section 4.2. 18 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 If overdose occurs, bisoprolol treatment should be stopped and supportive and symptomatic treatment should be provided. Limited data suggest that bisoprolol is hardly dialysable. Based on the expected pharmacologic actions and recommendations for other beta-blockers, the following general measures should be considered when clinically warranted. Bradycardia: Administer intravenous atropine. If the response is inadequate, isoprenaline or another agent with positive chronotropic properties may be given cautiously. Under some circumstances, transvenous pacemaker insertion may be necessary. Hypotension: Intravenous fluids and vasopressors should be administered. Intravenous glucagon may be useful. AV block (second or third degree): Patients should be carefully monitored and treated with isoprenaline infusion or transvenous cardiac pacemaker insertion. Acute worsening of heart failure: Administer i.v. diuretics, inotropic agents, vasodilating agents. Bronchospasm: Administer bronchodilator therapy such as isoprenaline, beta2-sympathomimetic drugs and/or aminophylline. Hypoglycaemia: Administer i.v. glucose. 5 5.1 PHARMACOLOGICAL PROPERTIES PHARMACODYNAMIC PROPERTIES Pharmacotherapeutic group: Beta blocking agents, selective ATC Code: C07AB07 Bisoprolol is a highly beta1-selective-adrenoceptor blocking agent, lacking intrinsic stimulating and relevant membrane stabilising activity. It only shows low affinity to the beta2-receptor of the smooth muscles of bronchi and vessels as well as to the beta2-receptors concerned with metabolic regulation. Therefore, bisoprolol is generally not to be expected to influence the airway resistance and beta2mediated metabolic effects. Its beta1-selectivity extends beyond the therapeutic dose range. In total 2647 patients were included in the CIBIS II trial. 83% (n = 2202) were in NYHA class III and 17% (n = 445) were in NYHA class IV. They had stable symptomatic systolic heart failure (ejection fraction <35%, based on echocardiography). Total mortality was reduced from 17.3% to 11.8% (relative reduction 34%). A decrease in sudden death (3.6% vs 6.3%, relative reduction 44%) and a reduced number of heart failure episodes requiring hospital admission (12% vs 17.6%, relative reduction 36%) was observed. Finally, a significant improvement of the functional status according to NYHA classification has been shown. During the initiation and titration of bisoprolol hospital admission due to bradycardia (0.53%), hypotension (0.23%), and acute decompensation (4.97%) were observed, but they were not more frequent than in the placebo-group (0%, 0.3% and 6.74%). The numbers of fatal and disabling strokes during the total study period were 20 in the bisoprolol group and 15 in the placebo group. The CIBIS III trial investigated 1010 patients aged 65 years with mild to moderate chronic heart failure (CHF; NYHA class II or III) and left ventricular ejection fraction 35%, who had not been treated previously with ACE inhibitors, beta-blockers, or angiotensin receptor blockers. The trial compared the efficacy and safety of an initial six-month monotherapy with bisoprolol (target dose 10 mg once daily), to which the ACE inhibitor enalapril (target dose 10 mg twice daily) was added for further 6 to 24 months, with the opposite sequence of treatment initiation. Each group comprised 505 patients. The two strategies were blindly compared with regard to the combined primary endpoint of all-cause mortality or hospitalisation, and each of these components individually. In the intention-to-treat population the primary endpoint occurred in 178 patients (35.2%) in the bisoprolol-first group vs. 186 (36.8%) in the enalapril-first group, showing bisoprolol-first treatment to be comparably effective (non-inferior) as enalapril-first treatment. With bisoprolol-first, 65 patients died vs. 73 with enalaprilfirst (between-group difference p=0.44), and 151 vs. 157 patients were hospitalisised (p=0.66). The number of serious and total adverse events was similar in the two groups. Analysis of data from the 19 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 first year showed a non-significant trend of the bisoprolol-first strategy to reduce all-cause mortality by 31% compared with the enalapril-first strategy. Mainly the statistically significant risk-reduction of sudden death by 46% (p=0.049) during the first year contributed to the better survival in the bisoprololfirst group. The two strategies for initiation of CHF treatment showed a similar rate of combined death and hospitalization, and a trend towards prolonged survival, particularly by reduction of sudden death, was observed in the bisoprolol-first group. The results indicate that it is as safe and efficacious to initiate treatment for CHF with bisoprolol as with enalapril. Bisoprolol is also used for the treatment of hypertension and angina. In acute administration in patients with coronary heart disease without chronic heart failure bisoprolol reduces the heart rate and stroke volume and thus the cardiac output and oxygen consumption. In chronic administration the initially elevated peripheral resistance decreases. 5.2 PHARMACOKINETIC PROPERTIES Bisoprolol is absorbed and has a biological availability of about 90% after oral administration. The plasma protein binding of bisoprolol is about 30%. The distribution volume is 3.5 l/kg. Total clearance is approximately 15 l/h. The half-life in plasma of 10-12 hours gives a 24 hour effect after dosing once daily. Bisoprolol is excreted from the body by two routes. 50% is metabolised by the liver to inactive metabolites which are then excreted by the kidneys. The remaining 50% is excreted by the kidneys in an unmetabolised form. Since the elimination takes place in the kidneys and the liver to the same extent a dosage adjustment is not required for patients with impaired liver function or renal insufficiency. The pharmacokinetics in patients with stable chronic heart failure and with impaired liver or renal function has not been studied. The kinetics of bisoprolol are linear and independent of age. In patients with chronic heart failure (NYHA stage III) the plasma levels of bisoprolol are higher and the half-life is prolonged compared to healthy volunteers. Maximum plasma concentration at steady state is 64+21 ng/ml at a daily dose of 10 mg and the half-life is 17+5 hours. 5.3 PRECLINICAL SAFETY DATA Preclinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity or carcinogenicity. Like other beta-blockers, bisoprolol caused maternal (decreased food intake and decreased body weight) and embryo/fetal toxicity (increased incidence of resorptions, reduced birth weight of the offspring, retarded physical development) at high doses but was not teratogenic. 6 6.1 PHARMACEUTICAL PARTICULARS LIST OF EXCIPIENTS Microcrystalline Cellulose (PH-102) Maize Starch Crospovidone (Type B) Colloidal Anhydrous Silica Magnesium Stearate Purified Water Film coating (1.25mg tablets and 2.5mg tablets): Hypromellose, Macrogol 400 and Titanium dioxide (E171). Film coating (3.75mg tablets, 5 mg tablets and 7.5mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171) and Ferric oxide yellow (E172) Film coating (10 mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171), Ferric oxide yellow (E172), Ferric oxide red (E172) 6.2 INCOMPATIBILITIES Not applicable. 20 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 6.3 SHELF LIFE 24 months. 6.4 SPECIAL PRECAUTIONS FOR STORAGE No special requirements 6.5 NATURE AND CONTENTS OF CONTAINER 20, 28, 30, 50, 56, 60, 90, or 100 tablets Not all pack sizes are marketed. Tablets are packed in Aluminium (0.02mm thickness) and PVC (0.25mm)/ PVDC (120 gsm) blisters. Blisters are packed in cartons. 6.6 SPECIAL PRECAUTIONS FOR DISPOSAL No special requirements. 7 MARKETING AUTHORISATION HOLDER Medreich Plc 9 Royal Parade Kew Gardens Surrey TW9 3QD UK 8 MARKETING AUTHORISATION NUMBER(S) PL 21880/0127 9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION 06/08/2012 10 DATE OF REVISION OF THE TEXT 06/08/2012 21 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 1 NAME OF THE MEDICINAL PRODUCT Bisoprolol 2.5 mg film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each Film coated tablet contains Bisoprolol Fumarate 2.5mg For list of excipients refer 6.1 3 PHARMACEUTICAL FORM Film-coated tablet. White and heart-shaped with a break-line on both sides. 4 4.1 CLINICAL PARTICULARS THERAPEUTIC INDICATIONS Treatment of stable chronic heart failure with reduced systolic left ventricular function in addition to ACE inhibitors, and diuretics, and optionally cardiac glycosides (for additional information see section 5.1). 4.2 POSOLOGY AND METHOD OF ADMINISTRATION Standard treatment of CHF consists of an ACE inhibitor (or an angiotensin receptor blocker in case of intolerance to ACE inhibitors), a beta-blocker, diuretics, and when appropriate cardiac glycosides. Patients should be stable (without acute failure) when bisoprolol treatment is initiated. It is recommended that the treating physician should be experienced in the management of chronic heart failure. Transient worsening of heart failure, hypotension, or bradycardia may occur during the titration period and thereafter. Titration phase The treatment of stable chronic heart failure with bisoprolol requires a titration phase The treatment with bisoprolol is to be started with a gradual uptitration according to the following steps: - 1.25 mg once daily for 1 week, if well tolerated increase to - 2.5 mg once daily for a further week, if well tolerated increase to - 3.75 mg once daily for a further week, if well tolerated increase to - 5 mg once daily for the 4 following weeks, if well tolerated increase to - 7.5 mg once daily for the 4 following weeks, if well tolerated increase to - 10 mg once daily for the maintenance therapy. The maximum recommended dose is 10 mg once daily. Close monitoring of vital signs (heart rate, blood pressure) and symptoms of worsening heart failure is recommended during the titration phase. Symptoms may already occur within the first day after initiating the therapy. Treatment modification If the maximum recommended dose is not well tolerated, gradual dose reduction may be considered. In case of transient worsening of heart failure, hypotension, or bradycardia reconsideration of the dosage of the concomitant medication is recommended. It may also be necessary to temporarily lower the dose of bisoprolol or to consider discontinuation. The reintroduction and/or uptitration of bisoprolol should always be considered when the patient becomes stable again. If discontinuation is considered, gradual dose decrease is recommended, since abrupt withdrawal may lead to acute deterioration of the patients condition. Treatment of stable chronic heart failure with bisoprolol is generally a long-term treatment. 22 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Administration Bisoprolol tablets should be taken in the morning and can be taken with food. They should be swallowed with liquid and should not be chewed. Special population Renal or hepatic impairment There is no information regarding pharmacokinetics of bisoprolol in patients with chronic heart failure and with impaired hepatic or renal function. Uptitration of the dose in these populations should therefore be made with additional caution. Elderly No dosage adjustment is required. Children There is no paediatric experience with bisoprolol, therefore its use cannot be recommended for children. 4.3 CONTRAINDICATIONS Bisoprolol is contraindicated in chronic heart failure patients with: - acute heart failure or during episodes of heart failure decompensation requiring i.v. inotropic therapy - cardiogenic shock - second or third degree AV block (without a pacemaker) - sick sinus syndrome - sinoatrial block - bradycardia with less than 60 beats/min before the start of therapy - hypotension (systolic blood pressure less than 100 mm Hg) - severe bronchial asthma or severe chronic obstructive pulmonary disease - late stages of peripheral arterial occlusive disease and Raynaud's syndrome - untreated phaeochromocytoma (see 4.4) - metabolic acidosis - hypersensitivity to bisoprolol or to any of the excipients 4.4 SPECIAL WARNINGS AND PRECAUTIONS FOR USE Bisoprolol must be used with caution in: - bronchospasm (bronchial asthma, obstructive airways diseases) - diabetes mellitus with large fluctuations in blood glucose values; symptoms of hypoglycaemia can be masked - strict fasting - ongoing desensitisation therapy - first degree AV block - Prinzmetal’s angina - peripheral arterial occlusive disease (intensification of complaints might happen especially during the start of therapy) - general anaesthesia In patients undergoing general anaesthesia beta-blockade reduces the incidence of arrhythmias and myocardial ischemia during induction and intubation, and the post-operative period. It is currently recommended that maintenance beta-blockade be continued peri-operatively. The anaesthesist must be aware of beta-blockade because of the potential for interactions with other drugs, resulting in bradyarrhythmias, attenuation of the reflex tachycardia and the decreased reflex ability to compensate for blood loss. If it is thought necessary to withdraw beta-blocker therapy before surgery, this should be done gradually and completed about 48 hours before anaesthesia. There is no therapeutic experience of bisoprolol treatment of heart failure in patients with the following diseases and conditions: - insulin dependent diabetes mellitus (type I) - severely impaired renal function - severely impaired hepatic function - restrictive cardiomyopathy 23 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 - congenital heart disease - haemodynamically significant organic valvular disease - myocardial infarction within 3 months Combination of bisoprolol with calcium antagonists of the verapamil or diltiazem type, with Class I antiarrhytmic drugs and with centrally acting antihypertensive drugs is generally not recommended, for details please refer to section 4.5. In bronchial asthma or other chronic obstructive lung diseases, which may cause symptoms, bronchodilating therapy should be given concomitantly. Occasionally an increase of the airway resistance may occur in patients with asthma, therefore the dose of beta2-stimulants may have to be increased. As with other beta-blockers, bisoprolol may increase both the sensitivity towards allergens and the severity of anaphylactic reactions. Adrenaline treatment does not always give the expected therapeutic effect. Patients with psoriasis or with a history of psoriasis should only be given beta-blockers (e.g. bisoprolol) after carefully balancing the benefits against the risks. In patients with phaeochromocytoma bisoprolol must not be administered until after alpha-receptor blockade. Under treatment with bisoprolol the symptoms of a thyreotoxicosis may be masked. The initiation of treatment with bisoprolol necessitates regular monitoring. For the posology and method of administration please refer to section 4.2. The cessation of therapy with bisoprolol should not be done abruptly unless clearly indicated. For further information please refer to section 4.2. 4.5 INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION Combinations not recommended Calcium antagonists of the verapamil type and to a lesser extent of the diltiazem type: Negative influence on contractility and atrio-ventricular conduction. Intravenous administration of verapamil in patients on β-blocker treatment may lead to profound hypotension and atrioventricular block. Class I antiarrhythmic drugs (e.g. quinidine, disopyramide; lidocaine, phenytoin; flecainide, propafenone): Effect on atrio-ventricular conduction time may be potentiated and negative inotropic effect increased. Centrally acting antihypertensive drugs such as clonidine and others (e.g. methyldopa, moxonodine, rilmenidine): Concomitant use of centrally acting antihypertensive drugs may worsen heart failure by a decrease in the central sympathetic tonus (reduction of heart rate and cardiac output, vasodilation). Abrupt withdrawal, particularly if prior to beta-blocker discontinuation, may increase risk of “rebound hypertension”. Combinations to be used with caution Calcium antagonists of the dihydropyridine type such as felodipine and amlodipine: Concomitant use may increase the risk of hypotension, and an increase in the risk of a further deterioration of the ventricular pump function in patients with heart failure cannot be excluded. Class-III antiarrhythmic drugs (e.g. amiodarone): Effect on atrio-ventricular conduction time may be potentiated. Topical beta-blockers (e.g. eye drops for glaucoma treatment) may add to the systemic effects of bisoprolol. Parasympathomimetic drugs: Concomitant use may increase atrio-ventricular conduction time and the risk of bradycardia. 24 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Insulin and oral antidiabetic drugs: Intensification of blood sugar lowering effect. Blockade of betaadrenoreceptors may mask symptoms of hypoglycaemia. Anaesthetic agents: Attenuation of the reflex tachycardia and increase of the risk of hypotension (for further information on general anaesthesia see also section 4.4.). Digitalis glycosides: Reduction of heart rate, increase of atrio-ventricular conduction time. Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs may reduce the hypotensive effect of bisoprolol. β-Sympathomimetic agents (e.g. isoprenaline, dobutamine): Combination with bisoprolol may reduce the effect of both agents. Sympathomimetics that activate both β- and α-adrenoceptors (e.g. noradrenaline, adrenaline): Combination with bisoprolol may unmask the α-adrenoceptor-mediated vasoconstrictor effects of these agents leading to blood pressure increase and exacerbated intermittent claudication. Such interactions are considered to be more likely with nonselective β-blockers. Concomitant use with antihypertensive agents as well as with other drugs with blood pressure lowering potential (e.g. tricyclic antidepressants, barbiturates, phenothiazines) may increase the risk of hypotension. Combinations to be considered Mefloquine: increased risk of bradycardia Monoamine oxidase inhibitors (except MAO-B inhibitors): Enhanced hypotensive effect of the betablockers but also risk for hypertensive crisis. 4.6 PREGNANCY AND LACTATION Pregnancy: Bisoprolol has pharmacological effects that may cause harmful effects on pregnancy and/or the fetus/newborn. In general, beta-adrenoceptor blockers reduce placental perfusion, which has been associated with growth retardation, intrauterine death, abortion or early labour. Adverse effects (e.g. hypoglycaemia and bradycardia) may occur in the fetus and newborn infant. If treatment with betaadrenoceptor blockers is necessary, beta1-selective adrenoceptor blockers are preferable. Bisoprolol should not be used during pregnancy unless clearly necessary. If treatment with bisoprolol is considered necessary, the uteroplacental blood flow and the fetal growth should be monitored. In case of harmful effects on pregnancy or the fetus alternative treatment should be considered. The newborn infant must be closely monitored. Symptoms of hypoglycaemia and bradycardia are generally to be expected within the first 3 days. Lactation: It is not known whether this drug is excreted in human milk. Therefore, breastfeeding is not recommended during administration of bisoprolol. Fertility: In reproduction toxicology studies Bisoprolol had no influence on fertility or on general reproduction performance (see section 5.3). 4.7 EFFECTS ON ABILITY TO DRIVE AND USE MACHINES In a study with coronary heart disease patients bisoprolol did not impair driving performance. However, due to individual variations in reactions to the drug, the ability to drive a vehicle or to operate machinery may be impaired. This should be considered particularly at start of treatment and upon change of medication as well as in conjunction with alcohol. 4.8 UNDESIRABLE EFFECTS The following definitions apply to the frequency terminology used hereafter: Very common ( 1/10) Common ( 1/100, < 1/10) Uncommon ( 1/1,000, < 1/100) Rare ( 1/10,000, < 1/1,000) Very rare (< 1/10,000) 25 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Cardiac disorders: Very common: bradycardia. Common: worsening of heart failure. Uncommon: AV-conduction disturbances. Investigations: Rare: increased triglycerides, increased liver enzymes (ALAT, ASAT). Nervous system disorders: Common: dizziness, headache. Eye disorders: Rare: reduced tear flow (to be considered if the patient uses lenses). Very rare: conjunctivitis. Ear and labyrinth disorders: Rare: hearing impairment. Respiratory, thoracic and mediastinal disorders: Uncommon: bronchospasm in patients with bronchial asthma or a history of obstructive airways disease. Rare: allergic rhinitis. Gastrointestinal disorders: Common: gastrointestinal complaints such as nausea, vomiting, diarrhoea, constipation. Skin and subcutaneous tissue disorders: Rare: hypersensitivity reactions (itching, flush, rash). Very rare: beta-blockers may provoke or worsen psoriasis or induce psoriasis-like rash, alopecia. Musculoskeletal and connective tissue disorders: Uncommon: muscular weakness and cramps. Vascular disorders: Common: feeling of coldness or numbness in the extremities, hypotension. Uncommon: orthostatic hypotension. General disorders: Common: asthenia, fatigue. Hepatobiliary disorders: Rare: hepatitis. Reproductive system and breast disorders: Rare: potency disorders. Psychiatric disorders: Uncommon: sleep disorders, depression. Rare: nightmares, hallucinations. 4.9 OVERDOSE With overdose (e.g. daily dose of 15 mg instead of 7.5 mg) third degree AV-block, bradycardia, and dizziness have been reported. In general the most common signs expected with overdosage of a betablocker are bradycardia, hypotension, bronchospasm, acute cardiac insufficiency and hypoglycaemia. To date a few cases of overdose (maximum: 2000 mg) with bisoprolol have been reported in patients suffering from hypertension and/or coronary heart disease showing bradycardia and/or hypotension; all patients recovered. There is a wide interindividual variation in sensitivity to one single high dose of bisoprolol and patients with heart failure are probably very sensitive. Therefore it is mandatory to initiate the treatment of these patients with a gradual uptitration according to the scheme given in section 4.2. 26 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 If overdose occurs, bisoprolol treatment should be stopped and supportive and symptomatic treatment should be provided. Limited data suggest that bisoprolol is hardly dialysable. Based on the expected pharmacologic actions and recommendations for other beta-blockers, the following general measures should be considered when clinically warranted. Bradycardia: Administer intravenous atropine. If the response is inadequate, isoprenaline or another agent with positive chronotropic properties may be given cautiously. Under some circumstances, transvenous pacemaker insertion may be necessary. Hypotension: Intravenous fluids and vasopressors should be administered. Intravenous glucagon may be useful. AV block (second or third degree): Patients should be carefully monitored and treated with isoprenaline infusion or transvenous cardiac pacemaker insertion. Acute worsening of heart failure: Administer i.v. diuretics, inotropic agents, vasodilating agents. Bronchospasm: Administer bronchodilator therapy such as isoprenaline, beta2-sympathomimetic drugs and/or aminophylline. Hypoglycaemia: Administer i.v. glucose. 5 5.1 PHARMACOLOGICAL PROPERTIES PHARMACODYNAMIC PROPERTIES Pharmacotherapeutic group: Beta blocking agents, selective ATC Code: C07AB07 Bisoprolol is a highly beta1-selective-adrenoceptor blocking agent, lacking intrinsic stimulating and relevant membrane stabilising activity. It only shows low affinity to the beta2-receptor of the smooth muscles of bronchi and vessels as well as to the beta2-receptors concerned with metabolic regulation. Therefore, bisoprolol is generally not to be expected to influence the airway resistance and beta2mediated metabolic effects. Its beta1-selectivity extends beyond the therapeutic dose range. In total 2647 patients were included in the CIBIS II trial. 83% (n = 2202) were in NYHA class III and 17% (n = 445) were in NYHA class IV. They had stable symptomatic systolic heart failure (ejection fraction <35%, based on echocardiography). Total mortality was reduced from 17.3% to 11.8% (relative reduction 34%). A decrease in sudden death (3.6% vs 6.3%, relative reduction 44%) and a reduced number of heart failure episodes requiring hospital admission (12% vs 17.6%, relative reduction 36%) was observed. Finally, a significant improvement of the functional status according to NYHA classification has been shown. During the initiation and titration of bisoprolol hospital admission due to bradycardia (0.53%), hypotension (0.23%), and acute decompensation (4.97%) were observed, but they were not more frequent than in the placebo-group (0%, 0.3% and 6.74%). The numbers of fatal and disabling strokes during the total study period were 20 in the bisoprolol group and 15 in the placebo group. The CIBIS III trial investigated 1010 patients aged 65 years with mild to moderate chronic heart failure (CHF; NYHA class II or III) and left ventricular ejection fraction 35%, who had not been treated previously with ACE inhibitors, beta-blockers, or angiotensin receptor blockers. The trial compared the efficacy and safety of an initial six-month monotherapy with bisoprolol (target dose 10 mg once daily), to which the ACE inhibitor enalapril (target dose 10 mg twice daily) was added for further 6 to 24 months, with the opposite sequence of treatment initiation. Each group comprised 505 patients. The two strategies were blindly compared with regard to the combined primary endpoint of all-cause mortality or hospitalisation, and each of these components individually. In the intention-to-treat population the primary endpoint occurred in 178 patients (35.2%) in the bisoprolol-first group vs. 186 (36.8%) in the enalapril-first group, showing bisoprolol-first treatment to be comparably effective (non-inferior) as enalapril-first treatment. With bisoprolol-first, 65 patients died vs. 73 with enalaprilfirst (between-group difference p=0.44), and 151 vs. 157 patients were hospitalisised (p=0.66). The number of serious and total adverse events was similar in the two groups. Analysis of data from the 27 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 first year showed a non-significant trend of the bisoprolol-first strategy to reduce all-cause mortality by 31% compared with the enalapril-first strategy. Mainly the statistically significant risk-reduction of sudden death by 46% (p=0.049) during the first year contributed to the better survival in the bisoprololfirst group. The two strategies for initiation of CHF treatment showed a similar rate of combined death and hospitalization, and a trend towards prolonged survival, particularly by reduction of sudden death, was observed in the bisoprolol-first group. The results indicate that it is as safe and efficacious to initiate treatment for CHF with bisoprolol as with enalapril. Bisoprolol is also used for the treatment of hypertension and angina. In acute administration in patients with coronary heart disease without chronic heart failure bisoprolol reduces the heart rate and stroke volume and thus the cardiac output and oxygen consumption. In chronic administration the initially elevated peripheral resistance decreases. 5.2 PHARMACOKINETIC PROPERTIES Bisoprolol is absorbed and has a biological availability of about 90% after oral administration. The plasma protein binding of bisoprolol is about 30%. The distribution volume is 3.5 l/kg. Total clearance is approximately 15 l/h. The half-life in plasma of 10-12 hours gives a 24 hour effect after dosing once daily. Bisoprolol is excreted from the body by two routes. 50% is metabolised by the liver to inactive metabolites which are then excreted by the kidneys. The remaining 50% is excreted by the kidneys in an unmetabolised form. Since the elimination takes place in the kidneys and the liver to the same extent a dosage adjustment is not required for patients with impaired liver function or renal insufficiency. The pharmacokinetics in patients with stable chronic heart failure and with impaired liver or renal function has not been studied. The kinetics of bisoprolol are linear and independent of age. In patients with chronic heart failure (NYHA stage III) the plasma levels of bisoprolol are higher and the half-life is prolonged compared to healthy volunteers. Maximum plasma concentration at steady state is 64+21 ng/ml at a daily dose of 10 mg and the half-life is 17+5 hours. 5.3 PRECLINICAL SAFETY DATA Preclinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity or carcinogenicity. Like other beta-blockers, bisoprolol caused maternal (decreased food intake and decreased body weight) and embryo/fetal toxicity (increased incidence of resorptions, reduced birth weight of the offspring, retarded physical development) at high doses but was not teratogenic. 6 6.1 PHARMACEUTICAL PARTICULARS LIST OF EXCIPIENTS Microcrystalline Cellulose (PH-102) Maize Starch Crospovidone (Type B) Colloidal Anhydrous Silica Magnesium Stearate Purified Water Film coating (1.25mg tablets and 2.5mg tablets): Hypromellose, Macrogol 400 and Titanium dioxide (E171). Film coating (3.75mg tablets, 5 mg tablets and 7.5mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171) and Ferric oxide yellow (E172) Film coating (10 mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171), Ferric oxide yellow (E172), Ferric oxide red (E172) 6.2 INCOMPATIBILITIES Not applicable. 28 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 6.3 SHELF LIFE 24 months. 6.4 SPECIAL PRECAUTIONS FOR STORAGE No special requirements 6.5 NATURE AND CONTENTS OF CONTAINER 20, 28, 30, 50, 56, 60, 90, or 100 tablets Not all pack sizes are marketed. Tablets are packed in Aluminium (0.02mm thickness) and PVC (0.25mm)/ PVDC (120 gsm) blisters. Blisters are packed in cartons. 6.6 SPECIAL PRECAUTIONS FOR DISPOSAL No special requirements. 7 MARKETING AUTHORISATION HOLDER Medreich Plc 9 Royal Parade Kew Gardens Surrey TW9 3QD UK 8 MARKETING AUTHORISATION NUMBER(S) PL 21880/0128 9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION 06/08/2012 10 DATE OF REVISION OF THE TEXT 06/08/2012 29 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 1 NAME OF THE MEDICINAL PRODUCT Bisoprolol 3.75mg film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each Film coated tablet contains Bisoprolol Fumarate 3.75mg For list of excipients refer 6.1 3 PHARMACEUTICAL FORM Film-coated tablet. Off-white and heart-shaped with a break-line on both sides 4 4.1 CLINICAL PARTICULARS THERAPEUTIC INDICATIONS Treatment of stable chronic heart failure with reduced systolic left ventricular function in addition to ACE inhibitors, and diuretics, and optionally cardiac glycosides (for additional information see section 5.1). 4.2 POSOLOGY AND METHOD OF ADMINISTRATION Standard treatment of CHF consists of an ACE inhibitor (or an angiotensin receptor blocker in case of intolerance to ACE inhibitors), a beta-blocker, diuretics, and when appropriate cardiac glycosides. Patients should be stable (without acute failure) when bisoprolol treatment is initiated. It is recommended that the treating physician should be experienced in the management of chronic heart failure. Transient worsening of heart failure, hypotension, or bradycardia may occur during the titration period and thereafter. Titration phase The treatment of stable chronic heart failure with bisoprolol requires a titration phase The treatment with bisoprolol is to be started with a gradual uptitration according to the following steps: - 1.25 mg once daily for 1 week, if well tolerated increase to - 2.5 mg once daily for a further week, if well tolerated increase to - 3.75 mg once daily for a further week, if well tolerated increase to - 5 mg once daily for the 4 following weeks, if well tolerated increase to - 7.5 mg once daily for the 4 following weeks, if well tolerated increase to - 10 mg once daily for the maintenance therapy. The maximum recommended dose is 10 mg once daily. Close monitoring of vital signs (heart rate, blood pressure) and symptoms of worsening heart failure is recommended during the titration phase. Symptoms may already occur within the first day after initiating the therapy. Treatment modification If the maximum recommended dose is not well tolerated, gradual dose reduction may be considered. In case of transient worsening of heart failure, hypotension, or bradycardia reconsideration of the dosage of the concomitant medication is recommended. It may also be necessary to temporarily lower the dose of bisoprolol or to consider discontinuation. The reintroduction and/or uptitration of bisoprolol should always be considered when the patient becomes stable again. If discontinuation is considered, gradual dose decrease is recommended, since abrupt withdrawal may lead to acute deterioration of the patients condition. Treatment of stable chronic heart failure with bisoprolol is generally a long-term treatment. 30 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Administration Bisoprolol tablets should be taken in the morning and can be taken with food. They should be swallowed with liquid and should not be chewed. Special population Renal or hepatic impairment There is no information regarding pharmacokinetics of bisoprolol in patients with chronic heart failure and with impaired hepatic or renal function. Uptitration of the dose in these populations should therefore be made with additional caution. Elderly No dosage adjustment is required. Children There is no paediatric experience with bisoprolol, therefore its use cannot be recommended for children. 4.3 CONTRAINDICATIONS Bisoprolol is contraindicated in chronic heart failure patients with: - acute heart failure or during episodes of heart failure decompensation requiring i.v. inotropic therapy - cardiogenic shock - second or third degree AV block (without a pacemaker) - sick sinus syndrome - sinoatrial block - bradycardia with less than 60 beats/min before the start of therapy - hypotension (systolic blood pressure less than 100 mm Hg) - severe bronchial asthma or severe chronic obstructive pulmonary disease - late stages of peripheral arterial occlusive disease and Raynaud's syndrome - untreated phaeochromocytoma (see 4.4) - metabolic acidosis - hypersensitivity to bisoprolol or to any of the excipients 4.4 SPECIAL WARNINGS AND PRECAUTIONS FOR USE Bisoprolol must be used with caution in: - bronchospasm (bronchial asthma, obstructive airways diseases) - diabetes mellitus with large fluctuations in blood glucose values; symptoms of hypoglycaemia can be masked - strict fasting - ongoing desensitisation therapy - first degree AV block - Prinzmetal’s angina - peripheral arterial occlusive disease (intensification of complaints might happen especially during the start of therapy) - general anaesthesia In patients undergoing general anaesthesia beta-blockade reduces the incidence of arrhythmias and myocardial ischemia during induction and intubation, and the post-operative period. It is currently recommended that maintenance beta-blockade be continued peri-operatively. The anaesthesist must be aware of beta-blockade because of the potential for interactions with other drugs, resulting in bradyarrhythmias, attenuation of the reflex tachycardia and the decreased reflex ability to compensate for blood loss. If it is thought necessary to withdraw beta-blocker therapy before surgery, this should be done gradually and completed about 48 hours before anaesthesia. There is no therapeutic experience of bisoprolol treatment of heart failure in patients with the following diseases and conditions: - insulin dependent diabetes mellitus (type I) - severely impaired renal function - severely impaired hepatic function - restrictive cardiomyopathy 31 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 - congenital heart disease - haemodynamically significant organic valvular disease - myocardial infarction within 3 months Combination of bisoprolol with calcium antagonists of the verapamil or diltiazem type, with Class I antiarrhytmic drugs and with centrally acting antihypertensive drugs is generally not recommended, for details please refer to section 4.5. In bronchial asthma or other chronic obstructive lung diseases, which may cause symptoms, bronchodilating therapy should be given concomitantly. Occasionally an increase of the airway resistance may occur in patients with asthma, therefore the dose of beta2-stimulants may have to be increased. As with other beta-blockers, bisoprolol may increase both the sensitivity towards allergens and the severity of anaphylactic reactions. Adrenaline treatment does not always give the expected therapeutic effect. Patients with psoriasis or with a history of psoriasis should only be given beta-blockers (e.g. bisoprolol) after carefully balancing the benefits against the risks. In patients with phaeochromocytoma bisoprolol must not be administered until after alpha-receptor blockade. Under treatment with bisoprolol the symptoms of a thyreotoxicosis may be masked. The initiation of treatment with bisoprolol necessitates regular monitoring. For the posology and method of administration please refer to section 4.2. The cessation of therapy with bisoprolol should not be done abruptly unless clearly indicated. For further information please refer to section 4.2. 4.5 INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION Combinations not recommended Calcium antagonists of the verapamil type and to a lesser extent of the diltiazem type: Negative influence on contractility and atrio-ventricular conduction. Intravenous administration of verapamil in patients on β-blocker treatment may lead to profound hypotension and atrioventricular block. Class I antiarrhythmic drugs (e.g. quinidine, disopyramide; lidocaine, phenytoin; flecainide, propafenone): Effect on atrio-ventricular conduction time may be potentiated and negative inotropic effect increased. Centrally acting antihypertensive drugs such as clonidine and others (e.g. methyldopa, moxonodine, rilmenidine): Concomitant use of centrally acting antihypertensive drugs may worsen heart failure by a decrease in the central sympathetic tonus (reduction of heart rate and cardiac output, vasodilation). Abrupt withdrawal, particularly if prior to beta-blocker discontinuation, may increase risk of “rebound hypertension”. Combinations to be used with caution Calcium antagonists of the dihydropyridine type such as felodipine and amlodipine: Concomitant use may increase the risk of hypotension, and an increase in the risk of a further deterioration of the ventricular pump function in patients with heart failure cannot be excluded. Class-III antiarrhythmic drugs (e.g. amiodarone): Effect on atrio-ventricular conduction time may be potentiated. Topical beta-blockers (e.g. eye drops for glaucoma treatment) may add to the systemic effects of bisoprolol. Parasympathomimetic drugs: Concomitant use may increase atrio-ventricular conduction time and the risk of bradycardia. 32 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Insulin and oral antidiabetic drugs: Intensification of blood sugar lowering effect. Blockade of betaadrenoreceptors may mask symptoms of hypoglycaemia. Anaesthetic agents: Attenuation of the reflex tachycardia and increase of the risk of hypotension (for further information on general anaesthesia see also section 4.4.). Digitalis glycosides: Reduction of heart rate, increase of atrio-ventricular conduction time. Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs may reduce the hypotensive effect of bisoprolol. β-Sympathomimetic agents (e.g. isoprenaline, dobutamine): Combination with bisoprolol may reduce the effect of both agents. Sympathomimetics that activate both β- and α-adrenoceptors (e.g. noradrenaline, adrenaline): Combination with bisoprolol may unmask the α-adrenoceptor-mediated vasoconstrictor effects of these agents leading to blood pressure increase and exacerbated intermittent claudication. Such interactions are considered to be more likely with nonselective β-blockers. Concomitant use with antihypertensive agents as well as with other drugs with blood pressure lowering potential (e.g. tricyclic antidepressants, barbiturates, phenothiazines) may increase the risk of hypotension. Combinations to be considered Mefloquine: increased risk of bradycardia Monoamine oxidase inhibitors (except MAO-B inhibitors): Enhanced hypotensive effect of the betablockers but also risk for hypertensive crisis. 4.6 PREGNANCY AND LACTATION Pregnancy: Bisoprolol has pharmacological effects that may cause harmful effects on pregnancy and/or the fetus/newborn. In general, beta-adrenoceptor blockers reduce placental perfusion, which has been associated with growth retardation, intrauterine death, abortion or early labour. Adverse effects (e.g. hypoglycaemia and bradycardia) may occur in the fetus and newborn infant. If treatment with betaadrenoceptor blockers is necessary, beta1-selective adrenoceptor blockers are preferable. Bisoprolol should not be used during pregnancy unless clearly necessary. If treatment with bisoprolol is considered necessary, the uteroplacental blood flow and the fetal growth should be monitored. In case of harmful effects on pregnancy or the fetus alternative treatment should be considered. The newborn infant must be closely monitored. Symptoms of hypoglycaemia and bradycardia are generally to be expected within the first 3 days. Lactation: It is not known whether this drug is excreted in human milk. Therefore, breastfeeding is not recommended during administration of bisoprolol. Fertility: In reproduction toxicology studies Bisoprolol had no influence on fertility or on general reproduction performance (see section 5.3). 4.7 EFFECTS ON ABILITY TO DRIVE AND USE MACHINES In a study with coronary heart disease patients bisoprolol did not impair driving performance. However, due to individual variations in reactions to the drug, the ability to drive a vehicle or to operate machinery may be impaired. This should be considered particularly at start of treatment and upon change of medication as well as in conjunction with alcohol. 4.8 UNDESIRABLE EFFECTS The following definitions apply to the frequency terminology used hereafter: Very common ( 1/10) Common ( 1/100, < 1/10) Uncommon ( 1/1,000, < 1/100) Rare ( 1/10,000, < 1/1,000) Very rare (< 1/10,000) 33 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Cardiac disorders: Very common: bradycardia. Common: worsening of heart failure. Uncommon: AV-conduction disturbances. Investigations: Rare: increased triglycerides, increased liver enzymes (ALAT, ASAT). Nervous system disorders: Common: dizziness, headache. Eye disorders: Rare: reduced tear flow (to be considered if the patient uses lenses). Very rare: conjunctivitis. Ear and labyrinth disorders: Rare: hearing impairment. Respiratory, thoracic and mediastinal disorders: Uncommon: bronchospasm in patients with bronchial asthma or a history of obstructive airways disease. Rare: allergic rhinitis. Gastrointestinal disorders: Common: gastrointestinal complaints such as nausea, vomiting, diarrhoea, constipation. Skin and subcutaneous tissue disorders: Rare: hypersensitivity reactions (itching, flush, rash). Very rare: beta-blockers may provoke or worsen psoriasis or induce psoriasis-like rash, alopecia. Musculoskeletal and connective tissue disorders: Uncommon: muscular weakness and cramps. Vascular disorders: Common: feeling of coldness or numbness in the extremities, hypotension. Uncommon: orthostatic hypotension. General disorders: Common: asthenia, fatigue. Hepatobiliary disorders: Rare: hepatitis. Reproductive system and breast disorders: Rare: potency disorders. Psychiatric disorders: Uncommon: sleep disorders, depression. Rare: nightmares, hallucinations. 4.9 OVERDOSE With overdose (e.g. daily dose of 15 mg instead of 7.5 mg) third degree AV-block, bradycardia, and dizziness have been reported. In general the most common signs expected with overdosage of a betablocker are bradycardia, hypotension, bronchospasm, acute cardiac insufficiency and hypoglycaemia. To date a few cases of overdose (maximum: 2000 mg) with bisoprolol have been reported in patients suffering from hypertension and/or coronary heart disease showing bradycardia and/or hypotension; all patients recovered. There is a wide interindividual variation in sensitivity to one single high dose of bisoprolol and patients with heart failure are probably very sensitive. Therefore it is mandatory to initiate the treatment of these patients with a gradual uptitration according to the scheme given in section 4.2. 34 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 If overdose occurs, bisoprolol treatment should be stopped and supportive and symptomatic treatment should be provided. Limited data suggest that bisoprolol is hardly dialysable. Based on the expected pharmacologic actions and recommendations for other beta-blockers, the following general measures should be considered when clinically warranted. Bradycardia: Administer intravenous atropine. If the response is inadequate, isoprenaline or another agent with positive chronotropic properties may be given cautiously. Under some circumstances, transvenous pacemaker insertion may be necessary. Hypotension: Intravenous fluids and vasopressors should be administered. Intravenous glucagon may be useful. AV block (second or third degree): Patients should be carefully monitored and treated with isoprenaline infusion or transvenous cardiac pacemaker insertion. Acute worsening of heart failure: Administer i.v. diuretics, inotropic agents, vasodilating agents. Bronchospasm: Administer bronchodilator therapy such as isoprenaline, beta2-sympathomimetic drugs and/or aminophylline. Hypoglycaemia: Administer i.v. glucose. 5 5.1 PHARMACOLOGICAL PROPERTIES PHARMACODYNAMIC PROPERTIES Pharmacotherapeutic group: Beta blocking agents, selective ATC Code: C07AB07 Bisoprolol is a highly beta1-selective-adrenoceptor blocking agent, lacking intrinsic stimulating and relevant membrane stabilising activity. It only shows low affinity to the beta2-receptor of the smooth muscles of bronchi and vessels as well as to the beta2-receptors concerned with metabolic regulation. Therefore, bisoprolol is generally not to be expected to influence the airway resistance and beta2mediated metabolic effects. Its beta1-selectivity extends beyond the therapeutic dose range. In total 2647 patients were included in the CIBIS II trial. 83% (n = 2202) were in NYHA class III and 17% (n = 445) were in NYHA class IV. They had stable symptomatic systolic heart failure (ejection fraction <35%, based on echocardiography). Total mortality was reduced from 17.3% to 11.8% (relative reduction 34%). A decrease in sudden death (3.6% vs 6.3%, relative reduction 44%) and a reduced number of heart failure episodes requiring hospital admission (12% vs 17.6%, relative reduction 36%) was observed. Finally, a significant improvement of the functional status according to NYHA classification has been shown. During the initiation and titration of bisoprolol hospital admission due to bradycardia (0.53%), hypotension (0.23%), and acute decompensation (4.97%) were observed, but they were not more frequent than in the placebo-group (0%, 0.3% and 6.74%). The numbers of fatal and disabling strokes during the total study period were 20 in the bisoprolol group and 15 in the placebo group. The CIBIS III trial investigated 1010 patients aged 65 years with mild to moderate chronic heart failure (CHF; NYHA class II or III) and left ventricular ejection fraction 35%, who had not been treated previously with ACE inhibitors, beta-blockers, or angiotensin receptor blockers. The trial compared the efficacy and safety of an initial six-month monotherapy with bisoprolol (target dose 10 mg once daily), to which the ACE inhibitor enalapril (target dose 10 mg twice daily) was added for further 6 to 24 months, with the opposite sequence of treatment initiation. Each group comprised 505 patients. The two strategies were blindly compared with regard to the combined primary endpoint of all-cause mortality or hospitalisation, and each of these components individually. In the intention-to-treat population the primary endpoint occurred in 178 patients (35.2%) in the bisoprolol-first group vs. 186 (36.8%) in the enalapril-first group, showing bisoprolol-first treatment to be comparably effective (non-inferior) as enalapril-first treatment. With bisoprolol-first, 65 patients died vs. 73 with enalaprilfirst (between-group difference p=0.44), and 151 vs. 157 patients were hospitalisised (p=0.66). The number of serious and total adverse events was similar in the two groups. Analysis of data from the 35 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 first year showed a non-significant trend of the bisoprolol-first strategy to reduce all-cause mortality by 31% compared with the enalapril-first strategy. Mainly the statistically significant risk-reduction of sudden death by 46% (p=0.049) during the first year contributed to the better survival in the bisoprololfirst group. The two strategies for initiation of CHF treatment showed a similar rate of combined death and hospitalization, and a trend towards prolonged survival, particularly by reduction of sudden death, was observed in the bisoprolol-first group. The results indicate that it is as safe and efficacious to initiate treatment for CHF with bisoprolol as with enalapril. Bisoprolol is also used for the treatment of hypertension and angina. In acute administration in patients with coronary heart disease without chronic heart failure bisoprolol reduces the heart rate and stroke volume and thus the cardiac output and oxygen consumption. In chronic administration the initially elevated peripheral resistance decreases. 5.2 PHARMACOKINETIC PROPERTIES Bisoprolol is absorbed and has a biological availability of about 90% after oral administration. The plasma protein binding of bisoprolol is about 30%. The distribution volume is 3.5 l/kg. Total clearance is approximately 15 l/h. The half-life in plasma of 10-12 hours gives a 24 hour effect after dosing once daily. Bisoprolol is excreted from the body by two routes. 50% is metabolised by the liver to inactive metabolites which are then excreted by the kidneys. The remaining 50% is excreted by the kidneys in an unmetabolised form. Since the elimination takes place in the kidneys and the liver to the same extent a dosage adjustment is not required for patients with impaired liver function or renal insufficiency. The pharmacokinetics in patients with stable chronic heart failure and with impaired liver or renal function has not been studied. The kinetics of bisoprolol are linear and independent of age. In patients with chronic heart failure (NYHA stage III) the plasma levels of bisoprolol are higher and the half-life is prolonged compared to healthy volunteers. Maximum plasma concentration at steady state is 64+21 ng/ml at a daily dose of 10 mg and the half-life is 17+5 hours. 5.3 PRECLINICAL SAFETY DATA Preclinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity or carcinogenicity. Like other beta-blockers, bisoprolol caused maternal (decreased food intake and decreased body weight) and embryo/fetal toxicity (increased incidence of resorptions, reduced birth weight of the offspring, retarded physical development) at high doses but was not teratogenic. 6 6.1 PHARMACEUTICAL PARTICULARS LIST OF EXCIPIENTS Microcrystalline Cellulose (PH-102) Maize Starch Crospovidone (Type B) Colloidal Anhydrous Silica Magnesium Stearate Purified Water Film coating (1.25mg tablets and 2.5mg tablets): Hypromellose, Macrogol 400 and Titanium dioxide (E171). Film coating (3.75mg tablets, 5 mg tablets and 7.5mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171) and Ferric oxide yellow (E172) Film coating (10 mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171), Ferric oxide yellow (E172), Ferric oxide red (E172) 6.2 INCOMPATIBILITIES Not applicable. 36 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 6.3 SHELF LIFE 24 months. 6.4 SPECIAL PRECAUTIONS FOR STORAGE No special requirements 6.5 NATURE AND CONTENTS OF CONTAINER 20, 28, 30, 50, 56, 60, 90, or 100 tablets Not all pack sizes are marketed. Tablets are packed in Aluminium (0.02mm thickness) and PVC (0.25mm)/ PVDC (120 gsm) blisters. Blisters are packed in cartons. 6.6 SPECIAL PRECAUTIONS FOR DISPOSAL No special requirements. 7 MARKETING AUTHORISATION HOLDER Medreich Plc 9 Royal Parade Kew Gardens Surrey TW9 3QD UK 8 MARKETING AUTHORISATION NUMBER(S) PL 21880/0129 9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION 06/08/2012 10 DATE OF REVISION OF THE TEXT 06/08/2012 37 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 1 NAME OF THE MEDICINAL PRODUCT Bisoprolol 5mg film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each Film coated tablet contains Bisoprolol Fumarate 5mg For list of excipients refer 6.1 3 PHARMACEUTICAL FORM Film-coated tablet. White-yellow, heart-shaped with a break-line on both sides. 4 4.1 CLINICAL PARTICULARS THERAPEUTIC INDICATIONS Treatment of stable chronic heart failure with reduced systolic left ventricular function in addition to ACE inhibitors, and diuretics, and optionally cardiac glycosides (for additional information see section 5.1). 4.2 POSOLOGY AND METHOD OF ADMINISTRATION Standard treatment of CHF consists of an ACE inhibitor (or an angiotensin receptor blocker in case of intolerance to ACE inhibitors), a beta-blocker, diuretics, and when appropriate cardiac glycosides. Patients should be stable (without acute failure) when bisoprolol treatment is initiated. It is recommended that the treating physician should be experienced in the management of chronic heart failure. Transient worsening of heart failure, hypotension, or bradycardia may occur during the titration period and thereafter. Titration phase The treatment of stable chronic heart failure with bisoprolol requires a titration phase The treatment with bisoprolol is to be started with a gradual uptitration according to the following steps: - 1.25 mg once daily for 1 week, if well tolerated increase to - 2.5 mg once daily for a further week, if well tolerated increase to - 3.75 mg once daily for a further week, if well tolerated increase to - 5 mg once daily for the 4 following weeks, if well tolerated increase to - 7.5 mg once daily for the 4 following weeks, if well tolerated increase to - 10 mg once daily for the maintenance therapy. The maximum recommended dose is 10 mg once daily. Close monitoring of vital signs (heart rate, blood pressure) and symptoms of worsening heart failure is recommended during the titration phase. Symptoms may already occur within the first day after initiating the therapy. Treatment modification If the maximum recommended dose is not well tolerated, gradual dose reduction may be considered. In case of transient worsening of heart failure, hypotension, or bradycardia reconsideration of the dosage of the concomitant medication is recommended. It may also be necessary to temporarily lower the dose of bisoprolol or to consider discontinuation. The reintroduction and/or uptitration of bisoprolol should always be considered when the patient becomes stable again. If discontinuation is considered, gradual dose decrease is recommended, since abrupt withdrawal may lead to acute deterioration of the patients condition. Treatment of stable chronic heart failure with bisoprolol is generally a long-term treatment. 38 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Administration Bisoprolol tablets should be taken in the morning and can be taken with food. They should be swallowed with liquid and should not be chewed. Special population Renal or hepatic impairment There is no information regarding pharmacokinetics of bisoprolol in patients with chronic heart failure and with impaired hepatic or renal function. Uptitration of the dose in these populations should therefore be made with additional caution. Elderly No dosage adjustment is required. Children There is no paediatric experience with bisoprolol, therefore its use cannot be recommended for children. 4.3 CONTRAINDICATIONS Bisoprolol is contraindicated in chronic heart failure patients with: - acute heart failure or during episodes of heart failure decompensation requiring i.v. inotropic therapy - cardiogenic shock - second or third degree AV block (without a pacemaker) - sick sinus syndrome - sinoatrial block - bradycardia with less than 60 beats/min before the start of therapy - hypotension (systolic blood pressure less than 100 mm Hg) - severe bronchial asthma or severe chronic obstructive pulmonary disease - late stages of peripheral arterial occlusive disease and Raynaud's syndrome - untreated phaeochromocytoma (see 4.4) - metabolic acidosis - hypersensitivity to bisoprolol or to any of the excipients 4.4 SPECIAL WARNINGS AND PRECAUTIONS FOR USE Bisoprolol must be used with caution in: - bronchospasm (bronchial asthma, obstructive airways diseases) - diabetes mellitus with large fluctuations in blood glucose values; symptoms of hypoglycaemia can be masked - strict fasting - ongoing desensitisation therapy - first degree AV block - Prinzmetal’s angina - peripheral arterial occlusive disease (intensification of complaints might happen especially during the start of therapy) - general anaesthesia In patients undergoing general anaesthesia beta-blockade reduces the incidence of arrhythmias and myocardial ischemia during induction and intubation, and the post-operative period. It is currently recommended that maintenance beta-blockade be continued peri-operatively. The anaesthesist must be aware of beta-blockade because of the potential for interactions with other drugs, resulting in bradyarrhythmias, attenuation of the reflex tachycardia and the decreased reflex ability to compensate for blood loss. If it is thought necessary to withdraw beta-blocker therapy before surgery, this should be done gradually and completed about 48 hours before anaesthesia. There is no therapeutic experience of bisoprolol treatment of heart failure in patients with the following diseases and conditions: - insulin dependent diabetes mellitus (type I) - severely impaired renal function - severely impaired hepatic function - restrictive cardiomyopathy 39 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 - congenital heart disease - haemodynamically significant organic valvular disease - myocardial infarction within 3 months Combination of bisoprolol with calcium antagonists of the verapamil or diltiazem type, with Class I antiarrhytmic drugs and with centrally acting antihypertensive drugs is generally not recommended, for details please refer to section 4.5. In bronchial asthma or other chronic obstructive lung diseases, which may cause symptoms, bronchodilating therapy should be given concomitantly. Occasionally an increase of the airway resistance may occur in patients with asthma, therefore the dose of beta2-stimulants may have to be increased. As with other beta-blockers, bisoprolol may increase both the sensitivity towards allergens and the severity of anaphylactic reactions. Adrenaline treatment does not always give the expected therapeutic effect. Patients with psoriasis or with a history of psoriasis should only be given beta-blockers (e.g. bisoprolol) after carefully balancing the benefits against the risks. In patients with phaeochromocytoma bisoprolol must not be administered until after alpha-receptor blockade. Under treatment with bisoprolol the symptoms of a thyreotoxicosis may be masked. The initiation of treatment with bisoprolol necessitates regular monitoring. For the posology and method of administration please refer to section 4.2. The cessation of therapy with bisoprolol should not be done abruptly unless clearly indicated. For further information please refer to section 4.2. 4.5 INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION Combinations not recommended Calcium antagonists of the verapamil type and to a lesser extent of the diltiazem type: Negative influence on contractility and atrio-ventricular conduction. Intravenous administration of verapamil in patients on β-blocker treatment may lead to profound hypotension and atrioventricular block. Class I antiarrhythmic drugs (e.g. quinidine, disopyramide; lidocaine, phenytoin; flecainide, propafenone): Effect on atrio-ventricular conduction time may be potentiated and negative inotropic effect increased. Centrally acting antihypertensive drugs such as clonidine and others (e.g. methyldopa, moxonodine, rilmenidine): Concomitant use of centrally acting antihypertensive drugs may worsen heart failure by a decrease in the central sympathetic tonus (reduction of heart rate and cardiac output, vasodilation). Abrupt withdrawal, particularly if prior to beta-blocker discontinuation, may increase risk of “rebound hypertension”. Combinations to be used with caution Calcium antagonists of the dihydropyridine type such as felodipine and amlodipine: Concomitant use may increase the risk of hypotension, and an increase in the risk of a further deterioration of the ventricular pump function in patients with heart failure cannot be excluded. Class-III antiarrhythmic drugs (e.g. amiodarone): Effect on atrio-ventricular conduction time may be potentiated. Topical beta-blockers (e.g. eye drops for glaucoma treatment) may add to the systemic effects of bisoprolol. Parasympathomimetic drugs: Concomitant use may increase atrio-ventricular conduction time and the risk of bradycardia. 40 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Insulin and oral antidiabetic drugs: Intensification of blood sugar lowering effect. Blockade of betaadrenoreceptors may mask symptoms of hypoglycaemia. Anaesthetic agents: Attenuation of the reflex tachycardia and increase of the risk of hypotension (for further information on general anaesthesia see also section 4.4.). Digitalis glycosides: Reduction of heart rate, increase of atrio-ventricular conduction time. Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs may reduce the hypotensive effect of bisoprolol. β-Sympathomimetic agents (e.g. isoprenaline, dobutamine): Combination with bisoprolol may reduce the effect of both agents. Sympathomimetics that activate both β- and α-adrenoceptors (e.g. noradrenaline, adrenaline): Combination with bisoprolol may unmask the α-adrenoceptor-mediated vasoconstrictor effects of these agents leading to blood pressure increase and exacerbated intermittent claudication. Such interactions are considered to be more likely with nonselective β-blockers. Concomitant use with antihypertensive agents as well as with other drugs with blood pressure lowering potential (e.g. tricyclic antidepressants, barbiturates, phenothiazines) may increase the risk of hypotension. Combinations to be considered Mefloquine: increased risk of bradycardia Monoamine oxidase inhibitors (except MAO-B inhibitors): Enhanced hypotensive effect of the betablockers but also risk for hypertensive crisis. 4.6 PREGNANCY AND LACTATION Pregnancy: Bisoprolol has pharmacological effects that may cause harmful effects on pregnancy and/or the fetus/newborn. In general, beta-adrenoceptor blockers reduce placental perfusion, which has been associated with growth retardation, intrauterine death, abortion or early labour. Adverse effects (e.g. hypoglycaemia and bradycardia) may occur in the fetus and newborn infant. If treatment with betaadrenoceptor blockers is necessary, beta1-selective adrenoceptor blockers are preferable. Bisoprolol should not be used during pregnancy unless clearly necessary. If treatment with bisoprolol is considered necessary, the uteroplacental blood flow and the fetal growth should be monitored. In case of harmful effects on pregnancy or the fetus alternative treatment should be considered. The newborn infant must be closely monitored. Symptoms of hypoglycaemia and bradycardia are generally to be expected within the first 3 days. Lactation: It is not known whether this drug is excreted in human milk. Therefore, breastfeeding is not recommended during administration of bisoprolol. Fertility: In reproduction toxicology studies Bisoprolol had no influence on fertility or on general reproduction performance (see section 5.3). 4.7 EFFECTS ON ABILITY TO DRIVE AND USE MACHINES In a study with coronary heart disease patients bisoprolol did not impair driving performance. However, due to individual variations in reactions to the drug, the ability to drive a vehicle or to operate machinery may be impaired. This should be considered particularly at start of treatment and upon change of medication as well as in conjunction with alcohol. 4.8 UNDESIRABLE EFFECTS The following definitions apply to the frequency terminology used hereafter: Very common ( 1/10) Common ( 1/100, < 1/10) Uncommon ( 1/1,000, < 1/100) Rare ( 1/10,000, < 1/1,000) Very rare (< 1/10,000) 41 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Cardiac disorders: Very common: bradycardia. Common: worsening of heart failure. Uncommon: AV-conduction disturbances. Investigations: Rare: increased triglycerides, increased liver enzymes (ALAT, ASAT). Nervous system disorders: Common: dizziness, headache. Eye disorders: Rare: reduced tear flow (to be considered if the patient uses lenses). Very rare: conjunctivitis. Ear and labyrinth disorders: Rare: hearing impairment. Respiratory, thoracic and mediastinal disorders: Uncommon: bronchospasm in patients with bronchial asthma or a history of obstructive airways disease. Rare: allergic rhinitis. Gastrointestinal disorders: Common: gastrointestinal complaints such as nausea, vomiting, diarrhoea, constipation. Skin and subcutaneous tissue disorders: Rare: hypersensitivity reactions (itching, flush, rash). Very rare: beta-blockers may provoke or worsen psoriasis or induce psoriasis-like rash, alopecia. Musculoskeletal and connective tissue disorders: Uncommon: muscular weakness and cramps. Vascular disorders: Common: feeling of coldness or numbness in the extremities, hypotension. Uncommon: orthostatic hypotension. General disorders: Common: asthenia, fatigue. Hepatobiliary disorders: Rare: hepatitis. Reproductive system and breast disorders: Rare: potency disorders. Psychiatric disorders: Uncommon: sleep disorders, depression. Rare: nightmares, hallucinations. 4.9 OVERDOSE With overdose (e.g. daily dose of 15 mg instead of 7.5 mg) third degree AV-block, bradycardia, and dizziness have been reported. In general the most common signs expected with overdosage of a betablocker are bradycardia, hypotension, bronchospasm, acute cardiac insufficiency and hypoglycaemia. To date a few cases of overdose (maximum: 2000 mg) with bisoprolol have been reported in patients suffering from hypertension and/or coronary heart disease showing bradycardia and/or hypotension; all patients recovered. There is a wide interindividual variation in sensitivity to one single high dose of bisoprolol and patients with heart failure are probably very sensitive. Therefore it is mandatory to initiate the treatment of these patients with a gradual uptitration according to the scheme given in section 4.2. 42 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 If overdose occurs, bisoprolol treatment should be stopped and supportive and symptomatic treatment should be provided. Limited data suggest that bisoprolol is hardly dialysable. Based on the expected pharmacologic actions and recommendations for other beta-blockers, the following general measures should be considered when clinically warranted. Bradycardia: Administer intravenous atropine. If the response is inadequate, isoprenaline or another agent with positive chronotropic properties may be given cautiously. Under some circumstances, transvenous pacemaker insertion may be necessary. Hypotension: Intravenous fluids and vasopressors should be administered. Intravenous glucagon may be useful. AV block (second or third degree): Patients should be carefully monitored and treated with isoprenaline infusion or transvenous cardiac pacemaker insertion. Acute worsening of heart failure: Administer i.v. diuretics, inotropic agents, vasodilating agents. Bronchospasm: Administer bronchodilator therapy such as isoprenaline, beta2-sympathomimetic drugs and/or aminophylline. Hypoglycaemia: Administer i.v. glucose. 5 5.1 PHARMACOLOGICAL PROPERTIES PHARMACODYNAMIC PROPERTIES Pharmacotherapeutic group: Beta blocking agents, selective ATC Code: C07AB07 Bisoprolol is a highly beta1-selective-adrenoceptor blocking agent, lacking intrinsic stimulating and relevant membrane stabilising activity. It only shows low affinity to the beta2-receptor of the smooth muscles of bronchi and vessels as well as to the beta2-receptors concerned with metabolic regulation. Therefore, bisoprolol is generally not to be expected to influence the airway resistance and beta2mediated metabolic effects. Its beta1-selectivity extends beyond the therapeutic dose range. In total 2647 patients were included in the CIBIS II trial. 83% (n = 2202) were in NYHA class III and 17% (n = 445) were in NYHA class IV. They had stable symptomatic systolic heart failure (ejection fraction <35%, based on echocardiography). Total mortality was reduced from 17.3% to 11.8% (relative reduction 34%). A decrease in sudden death (3.6% vs 6.3%, relative reduction 44%) and a reduced number of heart failure episodes requiring hospital admission (12% vs 17.6%, relative reduction 36%) was observed. Finally, a significant improvement of the functional status according to NYHA classification has been shown. During the initiation and titration of bisoprolol hospital admission due to bradycardia (0.53%), hypotension (0.23%), and acute decompensation (4.97%) were observed, but they were not more frequent than in the placebo-group (0%, 0.3% and 6.74%). The numbers of fatal and disabling strokes during the total study period were 20 in the bisoprolol group and 15 in the placebo group. The CIBIS III trial investigated 1010 patients aged 65 years with mild to moderate chronic heart failure (CHF; NYHA class II or III) and left ventricular ejection fraction 35%, who had not been treated previously with ACE inhibitors, beta-blockers, or angiotensin receptor blockers. The trial compared the efficacy and safety of an initial six-month monotherapy with bisoprolol (target dose 10 mg once daily), to which the ACE inhibitor enalapril (target dose 10 mg twice daily) was added for further 6 to 24 months, with the opposite sequence of treatment initiation. Each group comprised 505 patients. The two strategies were blindly compared with regard to the combined primary endpoint of all-cause mortality or hospitalisation, and each of these components individually. In the intention-to-treat population the primary endpoint occurred in 178 patients (35.2%) in the bisoprolol-first group vs. 186 (36.8%) in the enalapril-first group, showing bisoprolol-first treatment to be comparably effective (non-inferior) as enalapril-first treatment. With bisoprolol-first, 65 patients died vs. 73 with enalaprilfirst (between-group difference p=0.44), and 151 vs. 157 patients were hospitalisised (p=0.66). The number of serious and total adverse events was similar in the two groups. Analysis of data from the 43 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 first year showed a non-significant trend of the bisoprolol-first strategy to reduce all-cause mortality by 31% compared with the enalapril-first strategy. Mainly the statistically significant risk-reduction of sudden death by 46% (p=0.049) during the first year contributed to the better survival in the bisoprololfirst group. The two strategies for initiation of CHF treatment showed a similar rate of combined death and hospitalization, and a trend towards prolonged survival, particularly by reduction of sudden death, was observed in the bisoprolol-first group. The results indicate that it is as safe and efficacious to initiate treatment for CHF with bisoprolol as with enalapril. Bisoprolol is also used for the treatment of hypertension and angina. In acute administration in patients with coronary heart disease without chronic heart failure bisoprolol reduces the heart rate and stroke volume and thus the cardiac output and oxygen consumption. In chronic administration the initially elevated peripheral resistance decreases. 5.2 PHARMACOKINETIC PROPERTIES Bisoprolol is absorbed and has a biological availability of about 90% after oral administration. The plasma protein binding of bisoprolol is about 30%. The distribution volume is 3.5 l/kg. Total clearance is approximately 15 l/h. The half-life in plasma of 10-12 hours gives a 24 hour effect after dosing once daily. Bisoprolol is excreted from the body by two routes. 50% is metabolised by the liver to inactive metabolites which are then excreted by the kidneys. The remaining 50% is excreted by the kidneys in an unmetabolised form. Since the elimination takes place in the kidneys and the liver to the same extent a dosage adjustment is not required for patients with impaired liver function or renal insufficiency. The pharmacokinetics in patients with stable chronic heart failure and with impaired liver or renal function has not been studied. The kinetics of bisoprolol are linear and independent of age. In patients with chronic heart failure (NYHA stage III) the plasma levels of bisoprolol are higher and the half-life is prolonged compared to healthy volunteers. Maximum plasma concentration at steady state is 64+21 ng/ml at a daily dose of 10 mg and the half-life is 17+5 hours. 5.3 PRECLINICAL SAFETY DATA Preclinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity or carcinogenicity. Like other beta-blockers, bisoprolol caused maternal (decreased food intake and decreased body weight) and embryo/fetal toxicity (increased incidence of resorptions, reduced birth weight of the offspring, retarded physical development) at high doses but was not teratogenic. 6 6.1 PHARMACEUTICAL PARTICULARS LIST OF EXCIPIENTS Microcrystalline Cellulose (PH-102) Maize Starch Crospovidone (Type B) Colloidal Anhydrous Silica Magnesium Stearate Purified Water Film coating (1.25mg tablets and 2.5mg tablets): Hypromellose, Macrogol 400 and Titanium dioxide (E171). Film coating (3.75mg tablets, 5 mg tablets and 7.5mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171) and Ferric oxide yellow (E172) Film coating (10 mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171), Ferric oxide yellow (E172), Ferric oxide red (E172) 6.2 INCOMPATIBILITIES Not applicable. 44 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 6.3 SHELF LIFE 24 months. 6.4 SPECIAL PRECAUTIONS FOR STORAGE No special requirements 6.5 NATURE AND CONTENTS OF CONTAINER 20, 28, 30, 50, 56, 60, 90, or 100 tablets Not all pack sizes are marketed. Tablets are packed in Aluminium (0.02mm thickness) and PVC (0.25mm)/ PVDC (120 gsm) blisters. Blisters are packed in cartons. 6.6 SPECIAL PRECAUTIONS FOR DISPOSAL No special requirements. 7 MARKETING AUTHORISATION HOLDER Medreich Plc 9 Royal Parade Kew Gardens Surrey TW9 3QD UK 8 MARKETING AUTHORISATION NUMBER(S) PL 21880/0130 9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION 06/08/2012 10 DATE OF REVISION OF THE TEXT 06/08/2012 45 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 1 NAME OF THE MEDICINAL PRODUCT Bisoprolol 7.5mg film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each Film coated tablet contains Bisoprolol Fumarate 7.5mg For list of excipients refer 6.1 3 PHARMACEUTICAL FORM Film-coated tablet. Pale yellow and heart-shaped with a break-line on both sides. 4 4.1 CLINICAL PARTICULARS THERAPEUTIC INDICATIONS Treatment of stable chronic heart failure with reduced systolic left ventricular function in addition to ACE inhibitors, and diuretics, and optionally cardiac glycosides (for additional information see section 5.1). 4.2 POSOLOGY AND METHOD OF ADMINISTRATION Standard treatment of CHF consists of an ACE inhibitor (or an angiotensin receptor blocker in case of intolerance to ACE inhibitors), a beta-blocker, diuretics, and when appropriate cardiac glycosides. Patients should be stable (without acute failure) when bisoprolol treatment is initiated. It is recommended that the treating physician should be experienced in the management of chronic heart failure. Transient worsening of heart failure, hypotension, or bradycardia may occur during the titration period and thereafter. Titration phase The treatment of stable chronic heart failure with bisoprolol requires a titration phase The treatment with bisoprolol is to be started with a gradual uptitration according to the following steps: - 1.25 mg once daily for 1 week, if well tolerated increase to - 2.5 mg once daily for a further week, if well tolerated increase to - 3.75 mg once daily for a further week, if well tolerated increase to - 5 mg once daily for the 4 following weeks, if well tolerated increase to - 7.5 mg once daily for the 4 following weeks, if well tolerated increase to - 10 mg once daily for the maintenance therapy. The maximum recommended dose is 10 mg once daily. Close monitoring of vital signs (heart rate, blood pressure) and symptoms of worsening heart failure is recommended during the titration phase. Symptoms may already occur within the first day after initiating the therapy. Treatment modification If the maximum recommended dose is not well tolerated, gradual dose reduction may be considered. In case of transient worsening of heart failure, hypotension, or bradycardia reconsideration of the dosage of the concomitant medication is recommended. It may also be necessary to temporarily lower the dose of bisoprolol or to consider discontinuation. The reintroduction and/or uptitration of bisoprolol should always be considered when the patient becomes stable again. If discontinuation is considered, gradual dose decrease is recommended, since abrupt withdrawal may lead to acute deterioration of the patients condition. Treatment of stable chronic heart failure with bisoprolol is generally a long-term treatment. 46 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Administration Bisoprolol tablets should be taken in the morning and can be taken with food. They should be swallowed with liquid and should not be chewed. Special population Renal or hepatic impairment There is no information regarding pharmacokinetics of bisoprolol in patients with chronic heart failure and with impaired hepatic or renal function. Uptitration of the dose in these populations should therefore be made with additional caution. Elderly No dosage adjustment is required. Children There is no paediatric experience with bisoprolol, therefore its use cannot be recommended for children. 4.3 CONTRAINDICATIONS Bisoprolol is contraindicated in chronic heart failure patients with: - acute heart failure or during episodes of heart failure decompensation requiring i.v. inotropic therapy - cardiogenic shock - second or third degree AV block (without a pacemaker) - sick sinus syndrome - sinoatrial block - bradycardia with less than 60 beats/min before the start of therapy - hypotension (systolic blood pressure less than 100 mm Hg) - severe bronchial asthma or severe chronic obstructive pulmonary disease - late stages of peripheral arterial occlusive disease and Raynaud's syndrome - untreated phaeochromocytoma (see 4.4) - metabolic acidosis - hypersensitivity to bisoprolol or to any of the excipients 4.4 SPECIAL WARNINGS AND PRECAUTIONS FOR USE Bisoprolol must be used with caution in: - bronchospasm (bronchial asthma, obstructive airways diseases) - diabetes mellitus with large fluctuations in blood glucose values; symptoms of hypoglycaemia can be masked - strict fasting - ongoing desensitisation therapy - first degree AV block - Prinzmetal’s angina - peripheral arterial occlusive disease (intensification of complaints might happen especially during the start of therapy) - general anaesthesia In patients undergoing general anaesthesia beta-blockade reduces the incidence of arrhythmias and myocardial ischemia during induction and intubation, and the post-operative period. It is currently recommended that maintenance beta-blockade be continued peri-operatively. The anaesthesist must be aware of beta-blockade because of the potential for interactions with other drugs, resulting in bradyarrhythmias, attenuation of the reflex tachycardia and the decreased reflex ability to compensate for blood loss. If it is thought necessary to withdraw beta-blocker therapy before surgery, this should be done gradually and completed about 48 hours before anaesthesia. There is no therapeutic experience of bisoprolol treatment of heart failure in patients with the following diseases and conditions: - insulin dependent diabetes mellitus (type I) - severely impaired renal function - severely impaired hepatic function - restrictive cardiomyopathy 47 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 - congenital heart disease - haemodynamically significant organic valvular disease - myocardial infarction within 3 months Combination of bisoprolol with calcium antagonists of the verapamil or diltiazem type, with Class I antiarrhytmic drugs and with centrally acting antihypertensive drugs is generally not recommended, for details please refer to section 4.5. In bronchial asthma or other chronic obstructive lung diseases, which may cause symptoms, bronchodilating therapy should be given concomitantly. Occasionally an increase of the airway resistance may occur in patients with asthma, therefore the dose of beta2-stimulants may have to be increased. As with other beta-blockers, bisoprolol may increase both the sensitivity towards allergens and the severity of anaphylactic reactions. Adrenaline treatment does not always give the expected therapeutic effect. Patients with psoriasis or with a history of psoriasis should only be given beta-blockers (e.g. bisoprolol) after carefully balancing the benefits against the risks. In patients with phaeochromocytoma bisoprolol must not be administered until after alpha-receptor blockade. Under treatment with bisoprolol the symptoms of a thyreotoxicosis may be masked. The initiation of treatment with bisoprolol necessitates regular monitoring. For the posology and method of administration please refer to section 4.2. The cessation of therapy with bisoprolol should not be done abruptly unless clearly indicated. For further information please refer to section 4.2. 4.5 INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION Combinations not recommended Calcium antagonists of the verapamil type and to a lesser extent of the diltiazem type: Negative influence on contractility and atrio-ventricular conduction. Intravenous administration of verapamil in patients on β-blocker treatment may lead to profound hypotension and atrioventricular block. Class I antiarrhythmic drugs (e.g. quinidine, disopyramide; lidocaine, phenytoin; flecainide, propafenone): Effect on atrio-ventricular conduction time may be potentiated and negative inotropic effect increased. Centrally acting antihypertensive drugs such as clonidine and others (e.g. methyldopa, moxonodine, rilmenidine): Concomitant use of centrally acting antihypertensive drugs may worsen heart failure by a decrease in the central sympathetic tonus (reduction of heart rate and cardiac output, vasodilation). Abrupt withdrawal, particularly if prior to beta-blocker discontinuation, may increase risk of “rebound hypertension”. Combinations to be used with caution Calcium antagonists of the dihydropyridine type such as felodipine and amlodipine: Concomitant use may increase the risk of hypotension, and an increase in the risk of a further deterioration of the ventricular pump function in patients with heart failure cannot be excluded. Class-III antiarrhythmic drugs (e.g. amiodarone): Effect on atrio-ventricular conduction time may be potentiated. Topical beta-blockers (e.g. eye drops for glaucoma treatment) may add to the systemic effects of bisoprolol. Parasympathomimetic drugs: Concomitant use may increase atrio-ventricular conduction time and the risk of bradycardia. 48 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Insulin and oral antidiabetic drugs: Intensification of blood sugar lowering effect. Blockade of betaadrenoreceptors may mask symptoms of hypoglycaemia. Anaesthetic agents: Attenuation of the reflex tachycardia and increase of the risk of hypotension (for further information on general anaesthesia see also section 4.4.). Digitalis glycosides: Reduction of heart rate, increase of atrio-ventricular conduction time. Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs may reduce the hypotensive effect of bisoprolol. β-Sympathomimetic agents (e.g. isoprenaline, dobutamine): Combination with bisoprolol may reduce the effect of both agents. Sympathomimetics that activate both β- and α-adrenoceptors (e.g. noradrenaline, adrenaline): Combination with bisoprolol may unmask the α-adrenoceptor-mediated vasoconstrictor effects of these agents leading to blood pressure increase and exacerbated intermittent claudication. Such interactions are considered to be more likely with nonselective β-blockers. Concomitant use with antihypertensive agents as well as with other drugs with blood pressure lowering potential (e.g. tricyclic antidepressants, barbiturates, phenothiazines) may increase the risk of hypotension. Combinations to be considered Mefloquine: increased risk of bradycardia Monoamine oxidase inhibitors (except MAO-B inhibitors): Enhanced hypotensive effect of the betablockers but also risk for hypertensive crisis. 4.6 PREGNANCY AND LACTATION Pregnancy: Bisoprolol has pharmacological effects that may cause harmful effects on pregnancy and/or the fetus/newborn. In general, beta-adrenoceptor blockers reduce placental perfusion, which has been associated with growth retardation, intrauterine death, abortion or early labour. Adverse effects (e.g. hypoglycaemia and bradycardia) may occur in the fetus and newborn infant. If treatment with betaadrenoceptor blockers is necessary, beta1-selective adrenoceptor blockers are preferable. Bisoprolol should not be used during pregnancy unless clearly necessary. If treatment with bisoprolol is considered necessary, the uteroplacental blood flow and the fetal growth should be monitored. In case of harmful effects on pregnancy or the fetus alternative treatment should be considered. The newborn infant must be closely monitored. Symptoms of hypoglycaemia and bradycardia are generally to be expected within the first 3 days. Lactation: It is not known whether this drug is excreted in human milk. Therefore, breastfeeding is not recommended during administration of bisoprolol. Fertility: In reproduction toxicology studies Bisoprolol had no influence on fertility or on general reproduction performance (see section 5.3). 4.7 EFFECTS ON ABILITY TO DRIVE AND USE MACHINES In a study with coronary heart disease patients bisoprolol did not impair driving performance. However, due to individual variations in reactions to the drug, the ability to drive a vehicle or to operate machinery may be impaired. This should be considered particularly at start of treatment and upon change of medication as well as in conjunction with alcohol. 4.8 UNDESIRABLE EFFECTS The following definitions apply to the frequency terminology used hereafter: Very common ( 1/10) Common ( 1/100, < 1/10) Uncommon ( 1/1,000, < 1/100) Rare ( 1/10,000, < 1/1,000) Very rare (< 1/10,000) 49 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Cardiac disorders: Very common: bradycardia. Common: worsening of heart failure. Uncommon: AV-conduction disturbances. Investigations: Rare: increased triglycerides, increased liver enzymes (ALAT, ASAT). Nervous system disorders: Common: dizziness, headache. Eye disorders: Rare: reduced tear flow (to be considered if the patient uses lenses). Very rare: conjunctivitis. Ear and labyrinth disorders: Rare: hearing impairment. Respiratory, thoracic and mediastinal disorders: Uncommon: bronchospasm in patients with bronchial asthma or a history of obstructive airways disease. Rare: allergic rhinitis. Gastrointestinal disorders: Common: gastrointestinal complaints such as nausea, vomiting, diarrhoea, constipation. Skin and subcutaneous tissue disorders: Rare: hypersensitivity reactions (itching, flush, rash). Very rare: beta-blockers may provoke or worsen psoriasis or induce psoriasis-like rash, alopecia. Musculoskeletal and connective tissue disorders: Uncommon: muscular weakness and cramps. Vascular disorders: Common: feeling of coldness or numbness in the extremities, hypotension. Uncommon: orthostatic hypotension. General disorders: Common: asthenia, fatigue. Hepatobiliary disorders: Rare: hepatitis. Reproductive system and breast disorders: Rare: potency disorders. Psychiatric disorders: Uncommon: sleep disorders, depression. Rare: nightmares, hallucinations. 4.9 OVERDOSE With overdose (e.g. daily dose of 15 mg instead of 7.5 mg) third degree AV-block, bradycardia, and dizziness have been reported. In general the most common signs expected with overdosage of a betablocker are bradycardia, hypotension, bronchospasm, acute cardiac insufficiency and hypoglycaemia. To date a few cases of overdose (maximum: 2000 mg) with bisoprolol have been reported in patients suffering from hypertension and/or coronary heart disease showing bradycardia and/or hypotension; all patients recovered. There is a wide interindividual variation in sensitivity to one single high dose of bisoprolol and patients with heart failure are probably very sensitive. Therefore it is mandatory to initiate the treatment of these patients with a gradual uptitration according to the scheme given in section 4.2. 50 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 If overdose occurs, bisoprolol treatment should be stopped and supportive and symptomatic treatment should be provided. Limited data suggest that bisoprolol is hardly dialysable. Based on the expected pharmacologic actions and recommendations for other beta-blockers, the following general measures should be considered when clinically warranted. Bradycardia: Administer intravenous atropine. If the response is inadequate, isoprenaline or another agent with positive chronotropic properties may be given cautiously. Under some circumstances, transvenous pacemaker insertion may be necessary. Hypotension: Intravenous fluids and vasopressors should be administered. Intravenous glucagon may be useful. AV block (second or third degree): Patients should be carefully monitored and treated with isoprenaline infusion or transvenous cardiac pacemaker insertion. Acute worsening of heart failure: Administer i.v. diuretics, inotropic agents, vasodilating agents. Bronchospasm: Administer bronchodilator therapy such as isoprenaline, beta2-sympathomimetic drugs and/or aminophylline. Hypoglycaemia: Administer i.v. glucose. 5 5.1 PHARMACOLOGICAL PROPERTIES PHARMACODYNAMIC PROPERTIES Pharmacotherapeutic group: Beta blocking agents, selective ATC Code: C07AB07 Bisoprolol is a highly beta1-selective-adrenoceptor blocking agent, lacking intrinsic stimulating and relevant membrane stabilising activity. It only shows low affinity to the beta2-receptor of the smooth muscles of bronchi and vessels as well as to the beta2-receptors concerned with metabolic regulation. Therefore, bisoprolol is generally not to be expected to influence the airway resistance and beta2mediated metabolic effects. Its beta1-selectivity extends beyond the therapeutic dose range. In total 2647 patients were included in the CIBIS II trial. 83% (n = 2202) were in NYHA class III and 17% (n = 445) were in NYHA class IV. They had stable symptomatic systolic heart failure (ejection fraction <35%, based on echocardiography). Total mortality was reduced from 17.3% to 11.8% (relative reduction 34%). A decrease in sudden death (3.6% vs 6.3%, relative reduction 44%) and a reduced number of heart failure episodes requiring hospital admission (12% vs 17.6%, relative reduction 36%) was observed. Finally, a significant improvement of the functional status according to NYHA classification has been shown. During the initiation and titration of bisoprolol hospital admission due to bradycardia (0.53%), hypotension (0.23%), and acute decompensation (4.97%) were observed, but they were not more frequent than in the placebo-group (0%, 0.3% and 6.74%). The numbers of fatal and disabling strokes during the total study period were 20 in the bisoprolol group and 15 in the placebo group. The CIBIS III trial investigated 1010 patients aged 65 years with mild to moderate chronic heart failure (CHF; NYHA class II or III) and left ventricular ejection fraction 35%, who had not been treated previously with ACE inhibitors, beta-blockers, or angiotensin receptor blockers. The trial compared the efficacy and safety of an initial six-month monotherapy with bisoprolol (target dose 10 mg once daily), to which the ACE inhibitor enalapril (target dose 10 mg twice daily) was added for further 6 to 24 months, with the opposite sequence of treatment initiation. Each group comprised 505 patients. The two strategies were blindly compared with regard to the combined primary endpoint of all-cause mortality or hospitalisation, and each of these components individually. In the intention-to-treat population the primary endpoint occurred in 178 patients (35.2%) in the bisoprolol-first group vs. 186 (36.8%) in the enalapril-first group, showing bisoprolol-first treatment to be comparably effective (non-inferior) as enalapril-first treatment. With bisoprolol-first, 65 patients died vs. 73 with enalaprilfirst (between-group difference p=0.44), and 151 vs. 157 patients were hospitalisised (p=0.66). The number of serious and total adverse events was similar in the two groups. Analysis of data from the 51 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 first year showed a non-significant trend of the bisoprolol-first strategy to reduce all-cause mortality by 31% compared with the enalapril-first strategy. Mainly the statistically significant risk-reduction of sudden death by 46% (p=0.049) during the first year contributed to the better survival in the bisoprololfirst group. The two strategies for initiation of CHF treatment showed a similar rate of combined death and hospitalization, and a trend towards prolonged survival, particularly by reduction of sudden death, was observed in the bisoprolol-first group. The results indicate that it is as safe and efficacious to initiate treatment for CHF with bisoprolol as with enalapril. Bisoprolol is also used for the treatment of hypertension and angina. In acute administration in patients with coronary heart disease without chronic heart failure bisoprolol reduces the heart rate and stroke volume and thus the cardiac output and oxygen consumption. In chronic administration the initially elevated peripheral resistance decreases. 5.2 PHARMACOKINETIC PROPERTIES Bisoprolol is absorbed and has a biological availability of about 90% after oral administration. The plasma protein binding of bisoprolol is about 30%. The distribution volume is 3.5 l/kg. Total clearance is approximately 15 l/h. The half-life in plasma of 10-12 hours gives a 24 hour effect after dosing once daily. Bisoprolol is excreted from the body by two routes. 50% is metabolised by the liver to inactive metabolites which are then excreted by the kidneys. The remaining 50% is excreted by the kidneys in an unmetabolised form. Since the elimination takes place in the kidneys and the liver to the same extent a dosage adjustment is not required for patients with impaired liver function or renal insufficiency. The pharmacokinetics in patients with stable chronic heart failure and with impaired liver or renal function has not been studied. The kinetics of bisoprolol are linear and independent of age. In patients with chronic heart failure (NYHA stage III) the plasma levels of bisoprolol are higher and the half-life is prolonged compared to healthy volunteers. Maximum plasma concentration at steady state is 64+21 ng/ml at a daily dose of 10 mg and the half-life is 17+5 hours. 5.3 PRECLINICAL SAFETY DATA Preclinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity or carcinogenicity. Like other beta-blockers, bisoprolol caused maternal (decreased food intake and decreased body weight) and embryo/fetal toxicity (increased incidence of resorptions, reduced birth weight of the offspring, retarded physical development) at high doses but was not teratogenic. 6 6.1 PHARMACEUTICAL PARTICULARS LIST OF EXCIPIENTS Microcrystalline Cellulose (PH-102) Maize Starch Crospovidone (Type B) Colloidal Anhydrous Silica Magnesium Stearate Purified Water Film coating (1.25mg tablets and 2.5mg tablets): Hypromellose, Macrogol 400 and Titanium dioxide (E171). Film coating (3.75mg tablets, 5 mg tablets and 7.5mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171) and Ferric oxide yellow (E172) Film coating (10 mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171), Ferric oxide yellow (E172), Ferric oxide red (E172) 6.2 INCOMPATIBILITIES Not applicable. 52 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 6.3 SHELF LIFE 24 months. 6.4 SPECIAL PRECAUTIONS FOR STORAGE No special requirements 6.5 NATURE AND CONTENTS OF CONTAINER 20, 28, 30, 50, 56, 60, 90, or 100 tablets Not all pack sizes are marketed. Tablets are packed in Aluminium (0.02mm thickness) and PVC (0.25mm)/ PVDC (120 gsm) blisters. Blisters are packed in cartons. 6.6 SPECIAL PRECAUTIONS FOR DISPOSAL No special requirements. 7 MARKETING AUTHORISATION HOLDER Medreich Plc 9 Royal Parade Kew Gardens Surrey TW9 3QD UK 8 MARKETING AUTHORISATION NUMBER(S) PL 21880/0131 9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION 06/08/2012 10 DATE OF REVISION OF THE TEXT 06/08/2012 53 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 1 NAME OF THE MEDICINAL PRODUCT Bisoprolol 10mg film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each Film coated tablet contains Bisoprolol Fumarate 10mg For list of excipients refer 6.1 3 PHARMACEUTICAL FORM Film-coated tablet. Pale to light orange, heart-shaped with a break-line on both sides. 4 4.1 CLINICAL PARTICULARS THERAPEUTIC INDICATIONS Treatment of stable chronic heart failure with reduced systolic left ventricular function in addition to ACE inhibitors, and diuretics, and optionally cardiac glycosides (for additional information see section 5.1). 4.2 POSOLOGY AND METHOD OF ADMINISTRATION Standard treatment of CHF consists of an ACE inhibitor (or an angiotensin receptor blocker in case of intolerance to ACE inhibitors), a beta-blocker, diuretics, and when appropriate cardiac glycosides. Patients should be stable (without acute failure) when bisoprolol treatment is initiated. It is recommended that the treating physician should be experienced in the management of chronic heart failure. Transient worsening of heart failure, hypotension, or bradycardia may occur during the titration period and thereafter. Titration phase The treatment of stable chronic heart failure with bisoprolol requires a titration phase The treatment with bisoprolol is to be started with a gradual uptitration according to the following steps: - 1.25 mg once daily for 1 week, if well tolerated increase to - 2.5 mg once daily for a further week, if well tolerated increase to - 3.75 mg once daily for a further week, if well tolerated increase to - 5 mg once daily for the 4 following weeks, if well tolerated increase to - 7.5 mg once daily for the 4 following weeks, if well tolerated increase to - 10 mg once daily for the maintenance therapy. The maximum recommended dose is 10 mg once daily. Close monitoring of vital signs (heart rate, blood pressure) and symptoms of worsening heart failure is recommended during the titration phase. Symptoms may already occur within the first day after initiating the therapy. Treatment modification If the maximum recommended dose is not well tolerated, gradual dose reduction may be considered. In case of transient worsening of heart failure, hypotension, or bradycardia reconsideration of the dosage of the concomitant medication is recommended. It may also be necessary to temporarily lower the dose of bisoprolol or to consider discontinuation. The reintroduction and/or uptitration of bisoprolol should always be considered when the patient becomes stable again. If discontinuation is considered, gradual dose decrease is recommended, since abrupt withdrawal may lead to acute deterioration of the patients condition. Treatment of stable chronic heart failure with bisoprolol is generally a long-term treatment. 54 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Administration Bisoprolol tablets should be taken in the morning and can be taken with food. They should be swallowed with liquid and should not be chewed. Special population Renal or hepatic impairment There is no information regarding pharmacokinetics of bisoprolol in patients with chronic heart failure and with impaired hepatic or renal function. Uptitration of the dose in these populations should therefore be made with additional caution. Elderly No dosage adjustment is required. Children There is no paediatric experience with bisoprolol, therefore its use cannot be recommended for children. 4.3 CONTRAINDICATIONS Bisoprolol is contraindicated in chronic heart failure patients with: - acute heart failure or during episodes of heart failure decompensation requiring i.v. inotropic therapy - cardiogenic shock - second or third degree AV block (without a pacemaker) - sick sinus syndrome - sinoatrial block - bradycardia with less than 60 beats/min before the start of therapy - hypotension (systolic blood pressure less than 100 mm Hg) - severe bronchial asthma or severe chronic obstructive pulmonary disease - late stages of peripheral arterial occlusive disease and Raynaud's syndrome - untreated phaeochromocytoma (see 4.4) - metabolic acidosis - hypersensitivity to bisoprolol or to any of the excipients 4.4 SPECIAL WARNINGS AND PRECAUTIONS FOR USE Bisoprolol must be used with caution in: - bronchospasm (bronchial asthma, obstructive airways diseases) - diabetes mellitus with large fluctuations in blood glucose values; symptoms of hypoglycaemia can be masked - strict fasting - ongoing desensitisation therapy - first degree AV block - Prinzmetal’s angina - peripheral arterial occlusive disease (intensification of complaints might happen especially during the start of therapy) - general anaesthesia In patients undergoing general anaesthesia beta-blockade reduces the incidence of arrhythmias and myocardial ischemia during induction and intubation, and the post-operative period. It is currently recommended that maintenance beta-blockade be continued peri-operatively. The anaesthesist must be aware of beta-blockade because of the potential for interactions with other drugs, resulting in bradyarrhythmias, attenuation of the reflex tachycardia and the decreased reflex ability to compensate for blood loss. If it is thought necessary to withdraw beta-blocker therapy before surgery, this should be done gradually and completed about 48 hours before anaesthesia. There is no therapeutic experience of bisoprolol treatment of heart failure in patients with the following diseases and conditions: - insulin dependent diabetes mellitus (type I) - severely impaired renal function - severely impaired hepatic function - restrictive cardiomyopathy 55 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 - congenital heart disease - haemodynamically significant organic valvular disease - myocardial infarction within 3 months Combination of bisoprolol with calcium antagonists of the verapamil or diltiazem type, with Class I antiarrhytmic drugs and with centrally acting antihypertensive drugs is generally not recommended, for details please refer to section 4.5. In bronchial asthma or other chronic obstructive lung diseases, which may cause symptoms, bronchodilating therapy should be given concomitantly. Occasionally an increase of the airway resistance may occur in patients with asthma, therefore the dose of beta2-stimulants may have to be increased. As with other beta-blockers, bisoprolol may increase both the sensitivity towards allergens and the severity of anaphylactic reactions. Adrenaline treatment does not always give the expected therapeutic effect. Patients with psoriasis or with a history of psoriasis should only be given beta-blockers (e.g. bisoprolol) after carefully balancing the benefits against the risks. In patients with phaeochromocytoma bisoprolol must not be administered until after alpha-receptor blockade. Under treatment with bisoprolol the symptoms of a thyreotoxicosis may be masked. The initiation of treatment with bisoprolol necessitates regular monitoring. For the posology and method of administration please refer to section 4.2. The cessation of therapy with bisoprolol should not be done abruptly unless clearly indicated. For further information please refer to section 4.2. 4.5 INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION Combinations not recommended Calcium antagonists of the verapamil type and to a lesser extent of the diltiazem type: Negative influence on contractility and atrio-ventricular conduction. Intravenous administration of verapamil in patients on β-blocker treatment may lead to profound hypotension and atrioventricular block. Class I antiarrhythmic drugs (e.g. quinidine, disopyramide; lidocaine, phenytoin; flecainide, propafenone): Effect on atrio-ventricular conduction time may be potentiated and negative inotropic effect increased. Centrally acting antihypertensive drugs such as clonidine and others (e.g. methyldopa, moxonodine, rilmenidine): Concomitant use of centrally acting antihypertensive drugs may worsen heart failure by a decrease in the central sympathetic tonus (reduction of heart rate and cardiac output, vasodilation). Abrupt withdrawal, particularly if prior to beta-blocker discontinuation, may increase risk of “rebound hypertension”. Combinations to be used with caution Calcium antagonists of the dihydropyridine type such as felodipine and amlodipine: Concomitant use may increase the risk of hypotension, and an increase in the risk of a further deterioration of the ventricular pump function in patients with heart failure cannot be excluded. Class-III antiarrhythmic drugs (e.g. amiodarone): Effect on atrio-ventricular conduction time may be potentiated. Topical beta-blockers (e.g. eye drops for glaucoma treatment) may add to the systemic effects of bisoprolol. Parasympathomimetic drugs: Concomitant use may increase atrio-ventricular conduction time and the risk of bradycardia. 56 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Insulin and oral antidiabetic drugs: Intensification of blood sugar lowering effect. Blockade of betaadrenoreceptors may mask symptoms of hypoglycaemia. Anaesthetic agents: Attenuation of the reflex tachycardia and increase of the risk of hypotension (for further information on general anaesthesia see also section 4.4.). Digitalis glycosides: Reduction of heart rate, increase of atrio-ventricular conduction time. Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs may reduce the hypotensive effect of bisoprolol. β-Sympathomimetic agents (e.g. isoprenaline, dobutamine): Combination with bisoprolol may reduce the effect of both agents. Sympathomimetics that activate both β- and α-adrenoceptors (e.g. noradrenaline, adrenaline): Combination with bisoprolol may unmask the α-adrenoceptor-mediated vasoconstrictor effects of these agents leading to blood pressure increase and exacerbated intermittent claudication. Such interactions are considered to be more likely with nonselective β-blockers. Concomitant use with antihypertensive agents as well as with other drugs with blood pressure lowering potential (e.g. tricyclic antidepressants, barbiturates, phenothiazines) may increase the risk of hypotension. Combinations to be considered Mefloquine: increased risk of bradycardia Monoamine oxidase inhibitors (except MAO-B inhibitors): Enhanced hypotensive effect of the betablockers but also risk for hypertensive crisis. 4.6 PREGNANCY AND LACTATION Pregnancy: Bisoprolol has pharmacological effects that may cause harmful effects on pregnancy and/or the fetus/newborn. In general, beta-adrenoceptor blockers reduce placental perfusion, which has been associated with growth retardation, intrauterine death, abortion or early labour. Adverse effects (e.g. hypoglycaemia and bradycardia) may occur in the fetus and newborn infant. If treatment with betaadrenoceptor blockers is necessary, beta1-selective adrenoceptor blockers are preferable. Bisoprolol should not be used during pregnancy unless clearly necessary. If treatment with bisoprolol is considered necessary, the uteroplacental blood flow and the fetal growth should be monitored. In case of harmful effects on pregnancy or the fetus alternative treatment should be considered. The newborn infant must be closely monitored. Symptoms of hypoglycaemia and bradycardia are generally to be expected within the first 3 days. Lactation: It is not known whether this drug is excreted in human milk. Therefore, breastfeeding is not recommended during administration of bisoprolol. Fertility: In reproduction toxicology studies Bisoprolol had no influence on fertility or on general reproduction performance (see section 5.3). 4.7 EFFECTS ON ABILITY TO DRIVE AND USE MACHINES In a study with coronary heart disease patients bisoprolol did not impair driving performance. However, due to individual variations in reactions to the drug, the ability to drive a vehicle or to operate machinery may be impaired. This should be considered particularly at start of treatment and upon change of medication as well as in conjunction with alcohol. 4.8 UNDESIRABLE EFFECTS The following definitions apply to the frequency terminology used hereafter: Very common ( 1/10) Common ( 1/100, < 1/10) Uncommon ( 1/1,000, < 1/100) Rare ( 1/10,000, < 1/1,000) Very rare (< 1/10,000) 57 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 Cardiac disorders: Very common: bradycardia. Common: worsening of heart failure. Uncommon: AV-conduction disturbances. Investigations: Rare: increased triglycerides, increased liver enzymes (ALAT, ASAT). Nervous system disorders: Common: dizziness, headache. Eye disorders: Rare: reduced tear flow (to be considered if the patient uses lenses). Very rare: conjunctivitis. Ear and labyrinth disorders: Rare: hearing impairment. Respiratory, thoracic and mediastinal disorders: Uncommon: bronchospasm in patients with bronchial asthma or a history of obstructive airways disease. Rare: allergic rhinitis. Gastrointestinal disorders: Common: gastrointestinal complaints such as nausea, vomiting, diarrhoea, constipation. Skin and subcutaneous tissue disorders: Rare: hypersensitivity reactions (itching, flush, rash). Very rare: beta-blockers may provoke or worsen psoriasis or induce psoriasis-like rash, alopecia. Musculoskeletal and connective tissue disorders: Uncommon: muscular weakness and cramps. Vascular disorders: Common: feeling of coldness or numbness in the extremities, hypotension. Uncommon: orthostatic hypotension. General disorders: Common: asthenia, fatigue. Hepatobiliary disorders: Rare: hepatitis. Reproductive system and breast disorders: Rare: potency disorders. Psychiatric disorders: Uncommon: sleep disorders, depression. Rare: nightmares, hallucinations. 4.9 OVERDOSE With overdose (e.g. daily dose of 15 mg instead of 7.5 mg) third degree AV-block, bradycardia, and dizziness have been reported. In general the most common signs expected with overdosage of a betablocker are bradycardia, hypotension, bronchospasm, acute cardiac insufficiency and hypoglycaemia. To date a few cases of overdose (maximum: 2000 mg) with bisoprolol have been reported in patients suffering from hypertension and/or coronary heart disease showing bradycardia and/or hypotension; all patients recovered. There is a wide interindividual variation in sensitivity to one single high dose of bisoprolol and patients with heart failure are probably very sensitive. Therefore it is mandatory to initiate the treatment of these patients with a gradual uptitration according to the scheme given in section 4.2. 58 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 If overdose occurs, bisoprolol treatment should be stopped and supportive and symptomatic treatment should be provided. Limited data suggest that bisoprolol is hardly dialysable. Based on the expected pharmacologic actions and recommendations for other beta-blockers, the following general measures should be considered when clinically warranted. Bradycardia: Administer intravenous atropine. If the response is inadequate, isoprenaline or another agent with positive chronotropic properties may be given cautiously. Under some circumstances, transvenous pacemaker insertion may be necessary. Hypotension: Intravenous fluids and vasopressors should be administered. Intravenous glucagon may be useful. AV block (second or third degree): Patients should be carefully monitored and treated with isoprenaline infusion or transvenous cardiac pacemaker insertion. Acute worsening of heart failure: Administer i.v. diuretics, inotropic agents, vasodilating agents. Bronchospasm: Administer bronchodilator therapy such as isoprenaline, beta2-sympathomimetic drugs and/or aminophylline. Hypoglycaemia: Administer i.v. glucose. 5 5.1 PHARMACOLOGICAL PROPERTIES PHARMACODYNAMIC PROPERTIES Pharmacotherapeutic group: Beta blocking agents, selective ATC Code: C07AB07 Bisoprolol is a highly beta1-selective-adrenoceptor blocking agent, lacking intrinsic stimulating and relevant membrane stabilising activity. It only shows low affinity to the beta2-receptor of the smooth muscles of bronchi and vessels as well as to the beta2-receptors concerned with metabolic regulation. Therefore, bisoprolol is generally not to be expected to influence the airway resistance and beta2mediated metabolic effects. Its beta1-selectivity extends beyond the therapeutic dose range. In total 2647 patients were included in the CIBIS II trial. 83% (n = 2202) were in NYHA class III and 17% (n = 445) were in NYHA class IV. They had stable symptomatic systolic heart failure (ejection fraction <35%, based on echocardiography). Total mortality was reduced from 17.3% to 11.8% (relative reduction 34%). A decrease in sudden death (3.6% vs 6.3%, relative reduction 44%) and a reduced number of heart failure episodes requiring hospital admission (12% vs 17.6%, relative reduction 36%) was observed. Finally, a significant improvement of the functional status according to NYHA classification has been shown. During the initiation and titration of bisoprolol hospital admission due to bradycardia (0.53%), hypotension (0.23%), and acute decompensation (4.97%) were observed, but they were not more frequent than in the placebo-group (0%, 0.3% and 6.74%). The numbers of fatal and disabling strokes during the total study period were 20 in the bisoprolol group and 15 in the placebo group. The CIBIS III trial investigated 1010 patients aged 65 years with mild to moderate chronic heart failure (CHF; NYHA class II or III) and left ventricular ejection fraction 35%, who had not been treated previously with ACE inhibitors, beta-blockers, or angiotensin receptor blockers. The trial compared the efficacy and safety of an initial six-month monotherapy with bisoprolol (target dose 10 mg once daily), to which the ACE inhibitor enalapril (target dose 10 mg twice daily) was added for further 6 to 24 months, with the opposite sequence of treatment initiation. Each group comprised 505 patients. The two strategies were blindly compared with regard to the combined primary endpoint of all-cause mortality or hospitalisation, and each of these components individually. In the intention-to-treat population the primary endpoint occurred in 178 patients (35.2%) in the bisoprolol-first group vs. 186 (36.8%) in the enalapril-first group, showing bisoprolol-first treatment to be comparably effective (non-inferior) as enalapril-first treatment. With bisoprolol-first, 65 patients died vs. 73 with enalaprilfirst (between-group difference p=0.44), and 151 vs. 157 patients were hospitalisised (p=0.66). The number of serious and total adverse events was similar in the two groups. Analysis of data from the 59 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 first year showed a non-significant trend of the bisoprolol-first strategy to reduce all-cause mortality by 31% compared with the enalapril-first strategy. Mainly the statistically significant risk-reduction of sudden death by 46% (p=0.049) during the first year contributed to the better survival in the bisoprololfirst group. The two strategies for initiation of CHF treatment showed a similar rate of combined death and hospitalization, and a trend towards prolonged survival, particularly by reduction of sudden death, was observed in the bisoprolol-first group. The results indicate that it is as safe and efficacious to initiate treatment for CHF with bisoprolol as with enalapril. Bisoprolol is also used for the treatment of hypertension and angina. In acute administration in patients with coronary heart disease without chronic heart failure bisoprolol reduces the heart rate and stroke volume and thus the cardiac output and oxygen consumption. In chronic administration the initially elevated peripheral resistance decreases. 5.2 PHARMACOKINETIC PROPERTIES Bisoprolol is absorbed and has a biological availability of about 90% after oral administration. The plasma protein binding of bisoprolol is about 30%. The distribution volume is 3.5 l/kg. Total clearance is approximately 15 l/h. The half-life in plasma of 10-12 hours gives a 24 hour effect after dosing once daily. Bisoprolol is excreted from the body by two routes. 50% is metabolised by the liver to inactive metabolites which are then excreted by the kidneys. The remaining 50% is excreted by the kidneys in an unmetabolised form. Since the elimination takes place in the kidneys and the liver to the same extent a dosage adjustment is not required for patients with impaired liver function or renal insufficiency. The pharmacokinetics in patients with stable chronic heart failure and with impaired liver or renal function has not been studied. The kinetics of bisoprolol are linear and independent of age. In patients with chronic heart failure (NYHA stage III) the plasma levels of bisoprolol are higher and the half-life is prolonged compared to healthy volunteers. Maximum plasma concentration at steady state is 64+21 ng/ml at a daily dose of 10 mg and the half-life is 17+5 hours. 5.3 PRECLINICAL SAFETY DATA Preclinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity or carcinogenicity. Like other beta-blockers, bisoprolol caused maternal (decreased food intake and decreased body weight) and embryo/fetal toxicity (increased incidence of resorptions, reduced birth weight of the offspring, retarded physical development) at high doses but was not teratogenic. 6 6.1 PHARMACEUTICAL PARTICULARS LIST OF EXCIPIENTS Microcrystalline Cellulose (PH-102) Maize Starch Crospovidone (Type B) Colloidal Anhydrous Silica Magnesium Stearate Purified Water Film coating (1.25mg tablets and 2.5mg tablets): Hypromellose, Macrogol 400 and Titanium dioxide (E171). Film coating (3.75mg tablets, 5 mg tablets and 7.5mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171) and Ferric oxide yellow (E172) Film coating (10 mg tablets): Hypromellose, Macrogol 400, Titanium dioxide (E171), Ferric oxide yellow (E172), Ferric oxide red (E172) 6.2 INCOMPATIBILITIES Not applicable. 60 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 6.3 SHELF LIFE 24 months. 6.4 SPECIAL PRECAUTIONS FOR STORAGE No special requirements 6.5 NATURE AND CONTENTS OF CONTAINER 20, 28, 30, 50, 56, 60, 90, or 100 tablets Not all pack sizes are marketed. Tablets are packed in Aluminium (0.02mm thickness) and PVC (0.25mm)/ PVDC (120 gsm) blisters. Blisters are packed in cartons. 6.6 SPECIAL PRECAUTIONS FOR DISPOSAL No special requirements. 7 MARKETING AUTHORISATION HOLDER Medreich Plc 9 Royal Parade Kew Gardens Surrey TW9 3QD UK 8 MARKETING AUTHORISATION NUMBER(S) PL 21880/0132 9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION 06/08/2012 10 DATE OF REVISION OF THE TEXT 06/08/2012 61 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 PATIENT INFORMATION LEAFLET 62 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 63 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 LABELLING 64 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 65 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 66 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 67 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 68 UKPAR Bisoprolol 1.25 mg, 2.5 mg, 3.75 mg, 5 mg, 7.5 mg and 10 mg Film-Coated Tablets PL 21880/0127-32 69