SuggeSted empiric AntimicrobiAl AgentS of choice Aspirus Wausau
advertisement
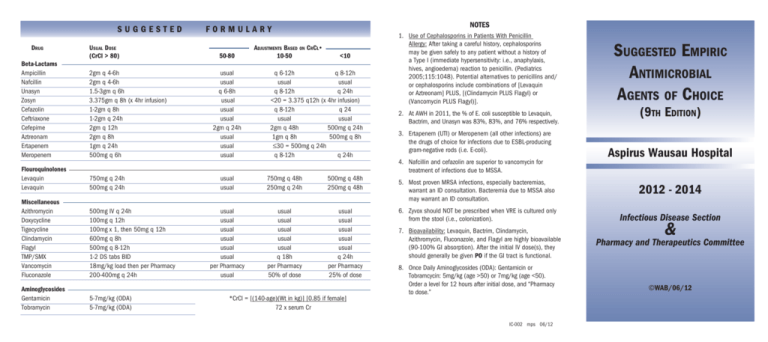
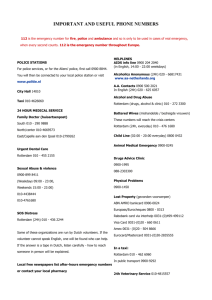
SUGGESTED DrugUsual Dose (CrCl > 80) Beta-Lactams Ampicillin 2gm q 4-6h Nafcillin 2gm q 4-6h Unasyn 1.5-3gm q 6h Zosyn 3.375gm q 8h (x 4hr infusion) Cefazolin 1-2gm q 8h Ceftriaxone 1-2gm q 24h Cefepime 2gm q 12h Aztreonam 2gm q 8h Ertapenem 1gm q 24h Meropenem 500mg q 6h Flouroquinolones Levaquin Levaquin 750mg q 24h 500mg q 24h Miscellaneous Azithromycin Doxycycline Tigecycline Clindamycin Flagyl TMP/SMX Vancomycin Fluconazole 500mg IV q 24h 100mg q 12h 100mg x 1, then 50mg q 12h 600mg q 8h 500mg q 8-12h 1-2 DS tabs BID 18mg/kg load then per Pharmacy 200-400mg q 24h Aminoglycosides Gentamicin Tobramycin 5-7mg/kg (ODA) 5-7mg/kg (ODA) NOTES FORMULARY 50-80 usual usual q 6-8h usual usual usual 2gm q 24h usual usual usual Adjustments Based on CrCl• 10-50 <10 q 6-12h q 8-12h usual usual q 8-12h q 24h <20 = 3.375 q12h (x 4hr infusion) q 8-12h q 24 usual usual 2gm q 48h 500mg q 24h 1gm q 8h 500mg q 8h ≤30 = 500mg q 24h q 8-12h q 24h usual usual 750mg q 48h 250mg q 24h 500mg q 48h 250mg q 48h usual usual usual usual usual usual per Pharmacy usual usual usual usual usual usual q 18h per Pharmacy 50% of dose usual usual usual usual usual q 24h per Pharmacy 25% of dose * CrCl = [(140-age)(Wt in kg)] [0.85 if female] 72 x serum Cr 1. Use of Cephalosporins in Patients With Penicillin Allergy: After taking a careful history, cephalosporins may be given safely to any patient without a history of a Type I (immediate hypersensitivity: i.e., anaphylaxis, hives, angioedema) reaction to penicillin. (Pediatrics 2005;115:1048). Potential alternatives to penicillins and/ or cephalosporins include combinations of [Levaquin or Aztreonam] PLUS, [(Clindamycin PLUS Flagyl) or (Vancomycin PLUS Flagyl)]. 2. At AWH in 2011, the % of E. coli susceptible to Levaquin, Bactrim, and Unasyn was 83%, 83%, and 76% respectively. 3.Ertapenem (UTI) or Meropenem (all other infections) are the drugs of choice for infections due to ESBL-producing gram-negative rods (i.e. E-coli). 4.Nafcillin and cefazolin are superior to vancomycin for treatment of infections due to MSSA. Suggested Empiric Antimicrobial Agents of Choice (9th Edition) Aspirus Wausau Hospital 5.Most proven MRSA infections, especially bacteremias, warrant an ID consultation. Bacteremia due to MSSA also may warrant an ID consultation. 2012 - 2014 6.Zyvox should NOT be prescribed when VRE is cultured only from the stool (i.e., colonization). Infectious Disease Section 7. Bioavailability: Levaquin, Bactrim, Clindamycin, Azithromycin, Fluconazole, and Flagyl are highly bioavailable (90-100% GI absorption). After the initial IV dose(s), they should generally be given PO if the GI tract is functional. 8. Once Daily Aminoglycosides (ODA): Gentamicin or Tobramcycin: 5mg/kg (age >50) or 7mg/kg (age <50). Order a level for 12 hours after initial dose, and “Pharmacy to dose.” IC-002 mps 06/12 & Pharmacy and Therapeutics Committee ©WAB/06/12 I. ANTIBIOTIC STEWARDSHIP • (1) Before initiating empiric antibiotic therapy; or, making a change in therapy due to lack of response to initial therapy, make certain that all relevant cultures have been obtained or repeated. • (2) Always change (“de-escalate”) to a narrower spectrum antibiotic(s) based on culture results. • (3) Whenever possible, consider stopping Vancomycin if: cultures are negative for MRSA, MRSE, or pencillin-resistant Enterococcus; and, no Hx of MRSA colonization; and, MRSA infection unlikely; and, no Type I allergy to penicillins. • (4) Combination therapy with Levaquin PLUS [Zosyn or Cefepime] is not beneficial beyond 48 hr (except for proven nonurinary Pseudomonas infections) - one or the other should be discontinued based on culture data. • (5) Switch Therapy: convert IV to PO, and change to narrower - spectrum agent(s) (“de-escalate”) based on microbiology results. II. “SEPSIS” OF UNKNOWN ETIOLOGY • Community-Acquired/Normal Host: [Levaquin 750mg or Gentamicin (5-7mg/kg)], PLUS Ceftriaxone 2gm q 24h, PLUS Vancomycin 18mg/kg (then per Pharmacy protocol). • Health Care-Associated/Compromised Host: [Levaquin 750mg or Tobramycin (5-7mg/kg)], PLUS [Zosyn 3.375gm q 8h (x 4hr) or Cefepime 2gm q 12h], PLUS Vancomycin 18mg/kg, (then per Pharmacy protocol). III. COMMUNITY-ACQUIRED PNEUMONIA (CAP) [CID 2007;44(Suppl 2):S27] • First doses within 6 hours of presentation. • Non-ICU: OPTION 1 - Ceftriaxone 2gm q 24h, PLUS [Azithromycin 500mg q 24h or Doxycycline 100mg q 12h]. OPTION 2 - Levaquin 750mg q 24h (x 5 days). • ICU: Ceftriaxone 2gm q 24h, PLUS Levaquin 750mg q 24h (x 5 days). IV.HEALTH CARE ASSOCIATED PNEUMONIA (HCAP) [Am J Respir Crit Care Med 2005;171:388] • [Cefepime 1gm q6h or Zosyn 3.375gm q 8h (x 4hr)], PLUS Levaquin 750mg q 24h, PLUS [Vancomycin 18mg/kg or Zyvox 600mg q 12h]. Zyvox ONLY if gram (+) cocci in clusters on sputum gram-stain, or Hx of MRSA colonization - Zyvox MUST be discontinued at 48hr if no MRSA in culture. • For proven MRSA HCAP, Zyvox is superior to Vancomycin (CID 2012;54;621). • For respiratory infections due to Pseudomonas with a Cefepime MIC ≥ 4, 1gm q 6h is superior to 2gm q 12h. • Duration of Rx for HCAP = 8 days (14 days if proven Pseudomonas). V.ASPIRATION PNEUMONIA [Ceftriaxone 2gm q 24h (CAP) or Cefepime 1gm q 6h (HCAP)], PLUS Flagyl 500mg q 8h. OR Zosyn 3.375gm q 8h (x 4hr). Both options PLUS Vancomycin 18mg/kg or Zyvox (as above). VI.COMPLICATED INTRA-ABDOMINAL, or BILIARY TRACT INFECTIONS, and PANCREATITIS [CID 2010;50:133-164] • A. Community-Acquired/Normal Host/Mild-Moderate Severity: Preferred: Ceftriaxone 2gm q 24h, PLUS Flagyl 500mg IV q 8h. First alternate: Ertapenem 1gm q 24h. 2nd Alternate: Tigecycline 100mg x 1, then 50mg q 12h. . • B. Community-Acquired/Compromised Host/High Severity: Zosyn 3.375gm q 8h (x 4h). OR Cefepime 2gm q 12h, PLUS Flagyl 500mg q 8h. • C. Health Care Associated: Same as “B” PLUS Vancomycin 18mg/kg, PLUS Fluconazole 400mg q 24h (if yeast on gram-stain). • D. “Bonafide” Type I Penicillin Allergy: Tigecycline 100 mg x 1, then 50mg q 12h, PLUS Levaquin 750mg q 24h (if “B” or “C”), PLUS Fluconazole 400mg q 24h (if “C” above) . • E. Duration of ATBs: 7 days after adequate “source control” is generally sufficient. • F. Pancreatitis: Routine “prophylactic” Meropenem on admission is not recommended (Ann Surg 2007;245:674. Am J Gastroenterol. 2006;101:2379. UpToDate. Crit Care Med. 2004:32;2524). Antibiotics indicated only if admission CT, or repeat CT (with contrast) at 48hr after admission shows ≥ 30% pancreatic necrosis. Ideally, CT-directed FNA for culture to guide Rx. VII. PYLEONEPHRITIS, or SEPSIS DUE to UTI [CID 2010;50:133-164] • A. Community-Acquired/Normal Host: Gentamicin 5mg/kg x 1, PLUS [Ceftriaxone 2gm q 24h or Levaquin 500mg q 24h], PLUS Ampicillin 2 gm q 6h. • B. Health Care Associated: Tobramycin 5mg/ kg x 1, PLUS [Cefepime 2gm q 12h or Levaquin 500mg q 24h], PLUS Ampicillin 2 gm q 6h. VIII.COMPLICATED SKIN AND SOFT TISSUE INFECTIONS [CID 2005;41:1373-1406] • A. Cellulitis: Strep: Penicillin G 4 million units q 6h, PLUS Clindamycin 600mg q 8h. Unknown or Staph: Nafcillin 2 gm 6h or Cefazolin 1gm q 8h. • B. Wound Infection or Abscess: [Nafcillin 2gm q 6h or Cefazolin 1gm q 8h], PLUS Levaquin 750mg q 24h. Add Vancomycin 18mg/kg x 1 dose pending culture results. Discontinue Levaquin if no gram-negative rod in culture. • C. Diabetic or Ischemic Foot Infection (AFTER deep tissue, ulcer curettage, or bone biopsy culture): Levaquin 750mg q 24h, PLUS Clindamycin 600mg q 8h. OR, Ceftriaxone 2gm q 24h, PLUS Flagyl 500mg q 8h. OR, Ertapenem 1gm q 24h. Each option: Vancomycin 18mg/kg x 1 dose pending culture results. IX. OPTIONS FOR MRSA INFECTIONS: [CID 2011;52:285-292] • Older, Inexpensive Agents: Bactrim DS 2 tabs PO q 12h, Minocycline 100mg PO q 12h; Clindamycin 450-600mg PO/IV q 8; or Vancomycin IV. • Newer/Expensive Agents: Linezolid 600mg IV/PO q 12h; Tigecycline 100mg, then 50mg IV q 12h; or Daptomycin 4-6mg/kg IV q 24h. (Note: ID consultation will occur when newer, expensive agents are continued ≥ 48h.) Remember: Antibiotic Stewardship!