DRUG CALCULATIONS
advertisement

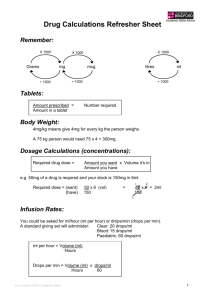
DRUG CALCULATIONS Mathematical accuracy is a matter of life and death”. [Keighley 1984] At the end of this practice sheet, you will be able to: Perform simple arithmetical tasks. Accurately calculate drug dosages using an accepted formula. Accurately calculate intravenous fluid rates using an accepted formula. The NMC Guidelines for the administration of medicines (20001 states: “Some drug administrations can require complex calculations to ensure that the correct volume or quantity of medication is administered. In these situations, it may be necessary for a second practitioner to check the calculation in order to minimise the risk of error. The use of a calculator to determine volume or quantity of medication should not act as a substitute for arithmetical knowledge and skill “. Calculations for Drug Administration – Part 1 A. Converting Units Most drugs are prescribed in milligram or microgram quantities. Occasionally, gram or nanogram quantities are also used. It is frequently necessary to convert units (e.g. from micrograms to milligrams), in order to calculate the correct dose to administer. Remember: 1 gram (g) = 1000 milligrams (mg) 1 milligram (mg) = 1000 micrograms (mcg or g) 1 microgram (mcg or g) = 1000 nanograms (ng) Similarly, 1 litre (L) = 1000 millilitres (ml) Micrograms and nanograms should be written out in full to avoid confusion. 1 1 To change from grams to milligrams, multiply by 1000 I.e. move the decimal point 3 places to the right E.g. 1g = 1000mg 4.2g = 4200mg 0.07g = 70mg To change milligrams to micrograms, multiply by 1000 I.e. move the decimal place 3 places to the right E.g. 1mg = 1000 micrograms 0.56mg = 560 micrograms 0.008mg = 8 micrograms To change from milligrams to grams, divide by 1000 I.e. move the decimal point 3 places to the left e.g. 100 mg 62,000mg 35mg = 0.1g = 62g = 0.035g To change from micrograms to milligrams, divide by 1000 i.e. move the decimal point 3 places to the left e.g. 2000micrograms 375 micrograms 62.5 micrograms = 2mg = 0.375mg = 0.0625mg Converting fractions to decimals To convert a fraction to a decimal, the number on the top of the fraction is divided by the number on the bottom. e.g. 7 = 4 So, 7 = 1.75 4 2 4I 7 = 1. 7 5 4 I 7. 3020 2 Where possible, large fractions should be simplified by cancelling, i.e. dividing both top and bottom by the same number. e.g. 250 can be simplified by dividing both top and bottom by 10 400 250 to give 25 . 400 40 This can be simplified further by dividing top and bottom by 5 5 25 to give 40 5 8 8 This fraction can then be converted to a decimal. 0. 6 2 5 8 I 5.502040 = 0.625 Rounding decimal numbers up and down Sometimes it is necessary to round numbers up or down to the nearest practical number, e.g. if a syringe has 0.1ml increments, we would round a volume of 4.69ml up to 4.7ml, or a volume of 4.62ml down to 4.6ml. When we convert fractions to decimals we may have a complex decimal answer, e.g. 5 12 = 0. 4 1 6 6 6 etc…. 12 I 5.5020808080 In this case the number would become 0.4 if rounded to 1 decimal place, or 0.42 to two decimal places, or 0.417 to three decimal places. 3 3 Tablet/capsule calculations The following formula can be used as an aid to work out the number of tablets required: Number of tablets required = e.g. what you want What you’ve got a prescription requires you to administer 150mg. You have a pot of 50mg tablets. How many tablets do you need? Number of tablets required = 150mg 50mg = 3 tablets. When using this formula you must make sure the units are the same. e.g. a prescription requires you to administer 25 micrograms. You have a pot of 0.05mg tablets. How many tablets do you need? Your first step is to make sure the units are the same. When converting units for this type of calculation it is usually easier to convert the number containing the decimal point into a larger figure, rather than the other way round. So, first multiply 0.05mg by 1000 to convert it to micrograms. 0.05mg = 50 micrograms. Now you can use this figure to calculate the number of tablets needed. Number of tablets needed = what you want What you’ve got Number of tablets needed = 25micrograms = 50 micrograms 1 tablet 2 Liquid Medication Calculations The following formula can be used for calculating the volume needed of oral liquid medication or injectable drugs. It is essential when using this formula that you use the same units for “what you want” and “what you’ve got”. 4 4 Volume needed E.g. = What you want What you’ve got x Volume it’s in you need to give 300mg Paracetamol to a child. The suspension contains 120mg in 5ml. What volume of suspension do you give? Volume needed = = 300mg 120mg 30 x 5ml 12 x 5ml = 75 6 = 12.5ml Other units Some drugs are expressed in other units, e.g. millimoles of potassium, or units of heparin, etc. You can use the formula in exactly the same way provided “what you want” and “what you’ve got” are in the same units. E.g. 7500 units’ heparin required from ampoules containing 5000units per ml. Volume needed = 7500 units 5000 units = 75 50 = 15 10 = x 1ml 1.5ml Mg/kg calculations Many medication doses, particularly for children, are calculated on a mg/kg basis. The prescribing doctor should work this out and prescribe the dose required. Nurses should be able to check the prescribed dose. E.g. the dose required is 4mg/kg. The child weighs 5kg. I.e. the child needs 4mg of medicine for every kg body weight. So the dose needed is 5 4mg x 5 = 20mg. 5 Care should be taken when using paediatric dose references as some books state the total daily dose in mg/kg, which then has to be divided into the number of doses per day. E.g. the dose required is 4mg/kg total daily dose, divided into 4 doses. In this case, for a 5kg child, the total daily dose is 20mg. Each individual dose is 5mg given 4 times daily. Calculations for Drug Administration Part 2 – Intravenous Drugs Drip Rate Infusion Calculations It is important that calculation of the rate of i.v. administration is accurate. For some drugs there are specific monograms and calculation aids available. However, it is useful to be able to perform these calculations from first principles and to do them step-by-step. E.g. At what rate (drops per minute) do you need to set the giving set to administer 1000ml of glucose 5% over 8 hours? Step 1 - How many ml per hour? This is the total volume (1000ml) divided by the time (8 hours). 125 81000 = 125mls Step 2 - How many ml per minute? This is the number of mls per hour (125) divided by the number of minutes per hour (60) = 125 60 It is a good idea to keep this as a fraction and move on to step 3 Step 3 - How many drops per minute This is the number of drops per ml multiplied by the number of ml per minute The number of drops per ml depends on the fluid you are giving (the thicker the fluid the bigger the drops, so there are less drops in 1ml) and the type of administration set you are using. 6 6 A standard giving set gives 15 drops per ml of blood Or 20 drops per ml of solutions A micro drop or paediatric giving set gives 60 drops per ml of solutions Using a standard giving set: Number of drops per minute = number of drops per ml x number of ml per minute = 20 x 125 60 So = 120 x 125 = 125 3 3 60 41.6 3125 As it is not possible to give a fraction of a drop the answer is 'rounded up' to 42. If we are giving solutions via a giving set the number of drops per ml and the 60 minutes per hour always stay the same. This means that steps 2 and 3 can be combined So whenever aqueous solutions are given via a standard giving set: Drops per minute = ml per hour divided by 3 For aqueous solutions given by a paediatric (micro drop) giving set: Drops per minute = ml per hour H. Dilutions Sometimes the dilution instructions for a drug are expressed in different ways, for example: Dilute 50:50 means dilute the drug solution with an equal volume of diluent, I.e. dilute 1ml drug solution with 1ml diluent to give 2ml. 7 7 Dilute 1 part with 4 parts means dilute 1 part drug solution with 4 parts diluent, I.e. dilute 1ml drug solution with 4ml diluent to give 5ml. Dilute 1 in 20 means dilute 1 part drug solution to a total volume of 20 parts I.e. dilute 1ml drug solution with 19ml diluent to give 20ml. I. Percentage Calculations Drug concentration may also be measured as % (w/v). % Means the number of grams dissolved in 100ml of solution I.e. grams per 100ml. This is the same whatever the size of the container E.g. Glucose 5% means that 5 grams of glucose is dissolved in 100ml of fluid. This is the same if in a 500ml bag as it is in a 1 litre bag, but obviously the 1 litre bag actually contains twice as much glucose as the 500ml one. This way of measuring the concentration is also sometimes used in ointments and creams. In calculations we can use the same formula as before: E.g. a patient is prescribed 20g of glucose to be given as Glucose 50% injection. What volume (ml) do you give? Volume needed = what you want x what it is in What you've got 50% glucose contains 50g in 100ml Volume needed 8 = 20 50 x 100ml = 20 x 2 = 40ml 8 J. Ratio Calculations This is only used for measuring the concentration of drugs such as adrenaline (epinephrine) or tuberculin. It is stated as 1 in 100, 1 in 10,000 etc. One in something concentrations means grams in mls I.e. 1 in 100 1 in 1000 1 in 10,000 E.g. give 1mg of adrenaline (epinephrine) using 1 in 10,000 injection 1 in 10,000 means means means 1g in 100ml 1g in 1000ml 1g in 10,000ml = 1g in 10,000ml = 1000mg in 10,000ml Volume needed = = what you want x what it is in What you've got 1 1000 x 10,000ml = 10ml K. Displacement Values Displacement values need to be considered when using part-vials of freeze-dried injections that require reconstitution. The displacement value is the volume of fluid displaced by the powder. For some drugs this volume is negligible, but for others it will make a significant difference if only a small fraction of the vial is needed, e.g. for neonates. 9 9 E.g. the displacement value for cefotaxime is 0.2ml per 500mg vial. If 2ml water for injection is added, the final concentration is 500mg in 2.2ml, not 2ml. This is important if a small dose is needed. It is better to adjust the volume of diluent according to the displacement value - in this case 1.8ml water for injection is used to reconstitute the vial to give a final concentration of 500mg in 2ml. The displacement value can usually be found in the package insert. L. Drug Infusion Calculations Intermittent infusions Intermittent infusions usually involve administering a certain dose over a short time period, e.g. clarithromycin 500mg in 250ml glucose 5% over 60 minutes. This can be given in drops per minute via a standard giving set, or via a volumatic device. Using a volumatic device Number of ml per hour = 250ml/hr. Number of ml per hour = 250ml/hr Number of ml per minute = 250 ml / min 60 Using drip rate Number of drops per minute = 250 x 20 60 = 83 drops/min. 10 10 Continuous Infusions Some drugs, particularly in ITU, CCU, HDU etc. are prescribed by continuous infusion, for example in mg per minute or micrograms per kg per minute. Often the drugs are very potent and it is crucial that they are given at the correct rate. This may often mean making up a stock solution and setting a suitable rate of administration. E.g. Administer Lignocaine 1mg per minute using a solution of 1 gram Lignocaine in 500ml glucose 5%. What is the required rate of administration in ml per hour? Step 1 - How many ml per minute Firstly ensure all the units are the same by converting the solution strength from g to mg. Lignocaine 1g in 500ml = 1000mg in 500ml Now you can use the formula: Volume needed = what you want x what it is in What you've got = 1 x 500 1 = 0.5ml per minute 2 1000 Step 2 - How many ml per hour To change ml per minute into ml per hour, multiply by 60 So: 0.5 x 60 = 30 ml per hour. M. Microgram/kg/min calculations E.g. a woman weighing 40kg needs Dobutamine at 5mcg/kg/minute. The stock solution, which has been prepared, contains 500mg in 500ml of glucose 5%. 11 11 What is the required rate of administration in ml per hour? Step 1 - How many micrograms per minute The patient needs 5 micrograms per minute for every kg body weight. Dose required = 5 x 40 = 200 micrograms/minute Step 2 - How many micrograms per hour Multiply by 60 to convert minutes to hours Dose required = 200 x 60 = 12,000 micrograms per hour Step 3 – How many mg per hour Divide by 1000 to convert micrograms to mg Dose required = 12,000 = 12 mg/hr 1000 Step 4 – How many ml per hour Volume required (ml/hr) = what you want (mg/hr) What you’ve got (mg) ml /hour = 12 mg/hr 500mg x 500ml= x Volume it’s in (ml) 12 ml/hr Remember! 1 gram (g) = 1000 milligrams (mg) 1 milligram (mg) = 1000 micrograms (mcg or g) 1 microgram (mcg or g) = Volume needed 12 = 1000 nanograms (ng) What you want What you’ve got 12 x Volume it’s in Percentages % means the number of grams dissolved in 100ml of solution i.e. grams per 100ml. e.g. 5% = 5g in 100ml 0.25% = 0.25g in 100ml Ratios 1 in 100 1 in 1000 1 in 10,000 13 means means means 1g in 100ml 1g in 1000ml 1g in 10,000ml 13 Drip Rates A standard giving set gives 15 drops per ml of blood Or 20 drops per ml of solutions A micro drop or paediatric giving set gives 60 drops per ml of solutions Aqueous solutions are given via a standard giving set: Drops per minute = ml per hour divided by 3 Aqueous solutions given by a paediatric (micro drop) giving set: Drops per minute = ml per hour Dilutions Dilute 50:50 means dilute the drug solution with an equal volume of diluent, i.e. dilute 1ml drug solution with 1ml diluent to give 2ml. Dilute 1 part with 4 parts means dilute 1 part drug solution with 4 parts diluent, i.e. dilute 1ml drug solution with 4ml diluent to give 5ml. Dilute 1 in 20 means dilute 1 part drug solution to a total volume of 20 parts i.e. dilute 1ml drug solution with 19ml diluent to give 20ml. 14 14 Calculations for Drug Administration: Part 1 Converting Units Please complete the following: - 1. 0.3g = ……………….mg 2. 725 micrograms = …………..….. mg 3. 300ml = ………………litres 4. 0.025 mg = ………….micrograms 5. 27,500 micrograms = ……………….mg Convert the following fractions to decimals: - 1. 200 5 = ……….…………… 2. 3 2 = …………………… 3. 180 150 = …………………… 15 15 Round the following numbers to one decimal place: - 1. 5.769 = ……………………… 2. 0.853 = ……………………… 3. 8.3333 ……………………… = Tablet/capsule calculations Complete the following table: - Prescription 1. Sodium Valproate 1.5g 2. Co-amilozide 5/50mg 3. Captopril 6.25mg 16 Tablet strength 500mg tablets 2.5/25mg tablets 12.5mg tablets 16 Number of tablets needed. Liquid Medication Calculations Complete the following table: - Prescription Liquid Concentration 1. Metronidazole 120mg 200mg in 5ml 2. Diazepam 500micrograms 2mg in 5ml 3. Spironolactone 7mg 25mg in 5ml 17 17 Volume needed mg/kg calculations Complete the following table: - Prescription Patients Body Weight 1. Gentamicin 7mg/kg 55kg 3. Digoxin 3micrograms per kg 16kg 3. Cefotaxime 200mg/kg/day in 4 divided doses 7.5kg 18 18 Dose required per dose Calculations for Drug Administration Part 2 – Intravenous Drugs Please complete the following: Drip rate infusion calculations What rate of administration (drops per minute) is required to give 500ml sodium chloride 0.9% over 6 hours using a standard giving set? What rate (drops/minute) is needed to give 250ml glucose 5% over 8 hours using a micro drop (paediatric) giving set? Dilutions An intravenous dose of 300mg Phenobarbitone has been prescribed, which must be diluted 1 in 10 with water for injections prior to administration. The ampoules contain 60mg phenobarbitone in 1ml. What volume of concentrated phenobarbitone do you need? b) What volume of water for injections do you need? 19 19 Percentage calculations What volume of 20% potassium chloride injection contains 3g of potassium chloride? What is the concentration (in mg/ml) of a 4.2% sodium bicarbonate infusion? Ratio calculations How many mg of adrenaline does 7ml of 1: 10,000 adrenaline (epinephrine) contain? Displacement value calculations The displacement value for co-amoxiclav is 0.9ml per 1.2g vial. What volume of water for injection would you add to the vial to give a concentration of 60mg in 1ml? 20 20 Drug infusion calculations 1. Aminophylline 0.5mg/kg/hr is prescribed for an 80kg man. A 500mg in 500ml infusion is prepared. At what rate should the infusion run (in ml/hr)? 2. A bag of 0.2% Lignocaine is prescribed at a rate of 3mg per minute for a 65kg lady. At what rate should the infusion run (in ml/hr)? 3. Dobutamine is prescribed at 6micrograms/kg/min for a 75kg man. The infusion prepared contains 250mg in 50ml. At what rate should the infusion run (in ml/hr)? 21 21