Universal protocol for preventing wrong site, wrong procedure, and
advertisement

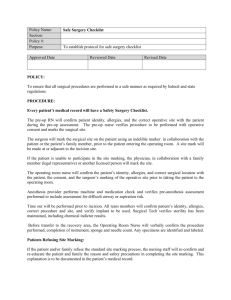
VIDANT MEDICAL CENTER CARE SERVICES POLICY/PROCEDURE SUBJECT: Universal Protocol for Preventing NUMBER: D11-1 Page 1 of 5 Wrong Site, Wrong Procedure, Wrong Person Surgery, or other Invasive Procedure: MINIMUM STANDARDS ________________________________________________________________________ ORIG: 11/1/05 REVIEWED: REVISED: 1/06, 5/06, 8/06, 2/07, 11/08, 9/10, 10/11, 7/12, 12/12 RESPONSIBLE FOR REVIEW: AVP, OPERATIVE SERVICES ________________________________________________________________________ APPROVED BY SR VP OF NURSING APPROVED BY AVP, OPERATIVE SERVICES POLICY This policy establishes minimum standards to be implemented by all Vidant Health departments to ensure verification of correct patient, correct procedure, correct site and timeout process for invasive and surgical procedures, including outpatient and bedside procedures. Patient identity and surgical procedure/site must be verified at following times: During scheduling. During pre-admission or entry into the system as an inpatient or outpatient. Pre-operatively or pre-procedure - by any department preparing a patient for a procedure. Prior to transport to the procedure or operative area. During change of caregivers. Prior to administration of pre-op medication or treatment. Prior to site marking. During a Time Out. DISCREPANCIES A discrepancy at any point in time must stop the case from proceeding until resolved. All Team members and, if possible, patient must agree on the resolution(s) to the identified discrepancy. The Registered Nurse must document the discrepancy, action(s) taken, and resolution.\ EQUIPMENT/SUPPLY VERIFICATION The surgical/procedure team will ensure all items needed during the procedure are available and matched to the patient prior to the start of the procedure. GUIDELINES FOR IMPLEMENTATION I. Pre-Procedure/Pre-Operative Verification A. Scheduling The following information is required when scheduling an invasive or surgical procedure: o Correct spelling of the patient’s full name. o Medical Record Number. o Date of Birth. o Procedure to be performed with right, left, or bilateral spelled out fully on the schedule. o Implants, if required. B. Pre-Admission Testing VIDANT MEDICAL CENTER CARE SERVICES POLICY/PROCEDURE SUBJECT: Universal Protocol for Preventing NUMBER: D11-1 Page 1 of 5 Wrong Site, Wrong Procedure, Wrong Person Surgery, or other Invasive Procedure: MINIMUM STANDARDS ________________________________________________________________________ ORIG: 11/1/05 REVIEWED: REVISED: 1/06, 5/06, 8/06, 2/07, 11/08, 9/10, 10/11, 7/12, 12/12 RESPONSIBLE FOR REVIEW: AVP, OPERATIVE SERVICES ________________________________________________________________________ APPROVED BY SR VP OF NURSING APPROVED BY AVP, OPERATIVE SERVICES The following information is required during the Pre-Admission Testing visit: o Correct spelling of the patient’s full name. o Medical Record number. o Date of Birth. C. Inpatient and Outpatient Units The following information is to be reviewed prior to the patient’s transport to Surgery: o Correct spelling of the patient’s full name. o Date of Birth o Procedure to be performed with right, left, or bilateral spelled out fully on the schedule. o Consent forms complete with right, left, or bilateral spelled out fully. o All relevant documentation and studies are available prior to transport. Non-Surgical procedure consents may be completed in the procedure area if the risk, benefits, and alternatives are explained and obtained by the provider performing the procedure. D. Pre-Procedure/Pre-Operative Verification Checklist Process The verification checklist process is to be completed in the Pre-Op Area for surgical cases, Prep Area when available, or at the Bedside for bedside procedures. The Checklist is to include: o All relevant documents and studies are available prior to transport to OR/Procedure Area: History and Physical (H&P), required updates to the H&P, nursing assessment, and preAnesthesia Assessment. o Completed Consent form with right, left, or bilateral spelled out fully. o Verify both Consent and Surgical Schedule agree on side and site. o Labeled diagnostic and radiology tests. o Any required blood products, implants, devices and/or special equipment for the procedure. If the patient is a minor, incompetent, or unable to verify the information for him/herself, the patient’s health care power of attorney, family, interpreter, or legal guardian will be included in the verification checklist process. II. Site Marking A. Procedures Requiring Site Marking o Site verification must be done on all cases that involve laterality, multiple structures (e.g., fingers and toes), or multiple levels (e.g. spinal surgery). VIDANT MEDICAL CENTER CARE SERVICES POLICY/PROCEDURE SUBJECT: Universal Protocol for Preventing NUMBER: D11-1 Page 1 of 5 Wrong Site, Wrong Procedure, Wrong Person Surgery, or other Invasive Procedure: MINIMUM STANDARDS ________________________________________________________________________ ORIG: 11/1/05 REVIEWED: REVISED: 1/06, 5/06, 8/06, 2/07, 11/08, 9/10, 10/11, 7/12, 12/12 RESPONSIBLE FOR REVIEW: AVP, OPERATIVE SERVICES ________________________________________________________________________ APPROVED BY SR VP OF NURSING APPROVED BY AVP, OPERATIVE SERVICES o For spinal procedures, in addition to pre-operative skin marking of the general spinal region, special intraoperative radiographic techniques may be used for marking the exact vertebral level. Intraoperative x-rays with immovable marker(s) may be used to determine exact location and level of surgery. X-ray(s) will be reviewed by the operating physician for confirmation. Once confirmed, the surgeon should mark the site with cautery, stitch, or bone bite before removing the x-ray marker. o For certain interventional procedures the exact site is not predetermined. Specialized equipment such as Fluoroscopy may be required. The physician will mark the site when the patient is on the procedure table. B. Time of Site Marking o Site marking should take place with the patient involved, awake, and aware if possible. o Site marking should be done prior to sedation/anesthesia and entrance into the Operative/Procedure area. o Procedure areas with no prep area may allow the provider to perform site marking in the procedure area prior to sedating the patient. NOTE: Final confirmation/verification of the site mark takes place during the Time Out. If the patient is a minor, incompetent, or unable to verify the information for him/herself, the verification of site marking will take place with the patient’s health care power of attorney, family, interpreter, or legal guardian. C. Type & Location of Site Mark by the Provider o The person performing the procedure will mark the site. The appropriate site mark is the provider’s initials. o The site marking will be made at or near the procedure site or the incision site. Other nonprocedural site(s) are not marked unless necessary for some other aspect of care. o The site mark is made using a marker that is sufficiently permanent to remain visible after the completion of the skin prep and sterile draping. Adhesive markers are not to be used as the sole means of site marking (non-OR areas). D. Alternative Process for Site Marking o For cases in which it is technically or anatomically impossible or impractical to mark the site (mucosal surfaces, perineum) and/or when a patient refuses to be marked, an armband will be marked with the correct side and site as well as the physician’s initials. VIDANT MEDICAL CENTER CARE SERVICES POLICY/PROCEDURE SUBJECT: Universal Protocol for Preventing NUMBER: D11-1 Page 1 of 5 Wrong Site, Wrong Procedure, Wrong Person Surgery, or other Invasive Procedure: MINIMUM STANDARDS ________________________________________________________________________ ORIG: 11/1/05 REVIEWED: REVISED: 1/06, 5/06, 8/06, 2/07, 11/08, 9/10, 10/11, 7/12, 12/12 RESPONSIBLE FOR REVIEW: AVP, OPERATIVE SERVICES ________________________________________________________________________ APPROVED BY SR VP OF NURSING APPROVED BY AVP, OPERATIVE SERVICES o For certain interventional procedures the exact site is not predetermined. Specialized, for example, equipment such as Fluoroscopy may be required to locate the site for spinal procedures which is then marked by the physician. o For minimal access procedures that intend to treat a lateralized internal organ, whether percutaneously or through a natural orifice, the intended side is indicated by a mark at or near the insertion site and should remain visible after completion of the skin prep and sterile draping. o For teeth, the operative tooth name(s) and number are indicated on documentation or the operative tooth (teeth) is marked on the dental radiographs or dental diagram. The documentation, images, and/or diagrams are available in the procedure room before the start of the procedure. o Neonatal Population: Site marking may cause a permanent tattoo. The Nursing staff will write the specific side and procedure to be performed on the patient addressograph label. The label will be attached to the side of the patient where the procedure is planned. E. Pre-Op or Pre-Procedure Treatment o When pre-op or pre-procedure treatments such as an anesthesia block or medication administration (e.g., eye drops) are performed prior to the site being marked, the patient identification process will be followed as outlined above. o Prior to beginning any pre-operative procedure, there should be a visual confirmation of the correct site/side validated by the Operative Consent, and when possible, the patient’s attestation of the surgical site all match. The patient/s H&P may be used in the place of any one of these elements. o When confirmation of the procedure/surgical site(s) is completed, the team members may perform the treatment before the surgical site is marked. The patient cannot, however, be moved to the operative area until the procedure/surgical site(s) is marked by the provider who will perform the procedure and visually confirmed by the Pre-OP RN. o Bedside Procedures o The provider performing the procedure at the patient’s bedside will mark procedures requiring site marking. Site marking is not required as long as the person performing the procedure identifies the patient and confirms all data, including consent, history and physical, and radiographs; and is in continuous attendance once it has been determined a procedure is required. A Time Out must occur prior to the start of the procedure. o VIDANT MEDICAL CENTER CARE SERVICES POLICY/PROCEDURE SUBJECT: Universal Protocol for Preventing NUMBER: D11-1 Page 1 of 5 Wrong Site, Wrong Procedure, Wrong Person Surgery, or other Invasive Procedure: MINIMUM STANDARDS ________________________________________________________________________ ORIG: 11/1/05 REVIEWED: REVISED: 1/06, 5/06, 8/06, 2/07, 11/08, 9/10, 10/11, 7/12, 12/12 RESPONSIBLE FOR REVIEW: AVP, OPERATIVE SERVICES ________________________________________________________________________ APPROVED BY SR VP OF NURSING APPROVED BY AVP, OPERATIVE SERVICES F. Exempted Site Marking o Midline, single organ procedures as well as endoscopies without intended laterality do not require site marking. Site marking is not required before procedures in which there is no predetermined site of insertion such as cardiac catheterization, vascath and other interventional procedures. o The following procedures are exempt: IV therapy, Foley catheter insertion, and arterial line insertion. G. Emergency Situations o III. Site marking may be waived in critical emergencies at the discretion of the operating physician, but a Time Out or pause should be conducted unless there is more risk than benefit to the patient. Time Out Process Once the patient has been prepped and draped with the site mark still visible, a verbal “Time Out” Must be done in the location where the procedure is to be performed, immediately before the start of the procedure (i.e. before the first instrument is passed) in the presence of and with full participation of the entire surgical/procedure team. During the Time Out, all other activities are suspended to the extent possible without compromising patient safety, so that all relevant members of the team are focused on the active confirmation of the Time Out. The Time Out may be initiated by any member of the Team. All immediate members of the team must be present, participate in the Time Out, and communicate verbal agreement that all of the following are correct: o Correct patient. o Correct side/site. o Correct procedure. If there is any disagreement by any member of the team, the procedure will not start until all discrepancies are resolved. Documentation: a member of the surgical/procedure team will document the completion of the Time Out. Two or more procedures on the same patient: When two or more procedures are being performed on the same patient by one or more different members of the team, a Time Out is performed to confirm each subsequent procedure before it is initiated. VIDANT MEDICAL CENTER CARE SERVICES POLICY/PROCEDURE SUBJECT: Universal Protocol for Preventing NUMBER: D11-1 Page 1 of 5 Wrong Site, Wrong Procedure, Wrong Person Surgery, or other Invasive Procedure: MINIMUM STANDARDS ________________________________________________________________________ ORIG: 11/1/05 REVIEWED: REVISED: 1/06, 5/06, 8/06, 2/07, 11/08, 9/10, 10/11, 7/12, 12/12 RESPONSIBLE FOR REVIEW: AVP, OPERATIVE SERVICES ________________________________________________________________________ APPROVED BY SR VP OF NURSING APPROVED BY AVP, OPERATIVE SERVICES References: The Joint Commission: National Patient Safety Goals Effective January 1, 2012 AORN: Correct Site/Surgery Tool Kit