C4 The Family Law Initiative

Infant Mental Health and Family Law
Brenda Packard
Chair, Family Law Initiatives
Committee
Infant Mental Health Promotion
Increased Awareness of Mental Health
Recent campaigns have raised awareness and understanding of mental health – much needed
These efforts have focused on youth and adults
We have been unable to find any evidence of any effort to raise awareness about infant mental health
We looked….and looked
We reviewed government documents – federal, provincial, municipal – no mention of infants and their mental health
We even asked our national commission on mental health and they admitted babies and toddlers had been left out (to their credit they are trying to correct this now)
We scanned the papers for months and the only evidence of a baby who may have been suffering from poor mental health was when that baby had died
A recently announced conference on mental health and the law again failed to have a speaker about infants and toddler mental health when the baby or toddler is involved with family courts and/or child welfare.
The images we do see are:
1. Perfect babies in perfect families
2. Babies of color in other countries far away who are suffering
3. References to children that exclude babies
Infants and toddlers are missing from the picture
While there has been an important and impactful effort to raise awareness about mental health these efforts have focused on youth and adults suffering
Most people do not realize that for too many, poor mental health begins during the first three years and sets a child on path that is riddled with mental health challenges
Children in Care
Many of these children are those who end up in our child welfare agencies.
They are babies and toddlers who have experienced trauma and have not had the supports necessary to recover
They are unable to speak, unable to tell you what they have experienced and what they are feeling
But to think that the trauma they have experienced has not impacted their mental health is naive
1
Your Context….
You deal with the most vulnerable people within Canada – those most vulnerable to poor mental health
They have no voice
They are dependent on those around them to protect them from harm and meet their basic needs
They are at HIGH risk for a life time of poor outcomes physically, emotionally and cognitively
For many of the children you see
This is a cycle that is repeating itself
This is a cycle that will continue to repeat itself
You are in a position to change the cycle
You are in a position, to help a child begin a journey of good mental health, and change that child’s developmental trajectory
Because the Needs of Babies and Toddlers ARE Unique
• The needs that babies and toddlers have when involved with child welfare are unique
• Yet, the system does not address these unique needs consistently
• This needs to be changed given what we now know about brain development during the first three years and the impact it will have on both short and long term development and health outcomes for a child
Recognizing the Unique Needs of
Professionals
We have started to create training and resources that will be customized for the following professionals:
– Child Welfare Workers/Social Worker
– Lawyers representing young children
– Judges presiding over family court
– Other professionals who may be involved with the child such as Early Childhood Educators
Competencies for Child Protection Work with Maltreated Infants
1.
Competencies
Basic understanding of how infants develop in the first years of life
Knowledge Base
Basic brain development
Defining infant mental health
The role of relationships, genetics & experience in development
Basic knowledge of attachment theory & implications/limitations for child welfare practice
Skills
Ability to observe a parent/infant interaction & recognize signs of distress or dysfunction
Appreciation of the importance of early intervention & timely decisions in cases of infant maltreatment
Who?
Case workers
Physicians
Home visitors
Visit supervisors
Phn’s
Lawyers
Judges
Police
Foster parents
Foster care support workers
2. Basic understanding of physical/emoti onal neglect, trauma & the impact on infants
Definitions for neglect, emotional neglect & trauma in infancy
Knowledge of the traumatic nature of exposure to family violence & chronic neglect
Understanding the development of the stress response system in infancy and the impact of chronic stress in infancy
Competency 1
Ability to observe & describe parent/infant interactions
Ability to differentiate between mild/moderate & severe dysfunction in parent infant interactions
Ability to recognize signs & symptoms of serious emotional/physical harm in infants
Ability to recognize imminent risk vs. long term risk
Case workers investigators (child welfare police)
Gp’s
Home visitors
Visit supervisors
Phn’s
Lawyers
Judges
Foster parents
Foster care support workers
3. Assessment skills
Familiarity with how parent ability to read & respond to cues impacts baby
Familiarity with how to apply attachment theory to custody & access questions
Competency 1,2
4. Basic case management skills for high risk infants
5.
Basic intervention skills for maltreating parents with infants
Legislation & policy regarding infants
Community resources for high risk infants
Common errors in reasoning affecting child welfare decision making
Competency 1,2,3
Knowledge of parent infant intervention strategies
Competency 1,2,3
Ability to use guidelines to assess parent, infant, & parent/infant
relationship
Ability to evaluate evidence of
accumulating risk factors such as congenital impairments (FASD & others), family adversity, parent infant relationship difficulties, parental competence
Ability to use assessment to develop a strategy for intervention
Ability to create developmentally appropriate & therapeutic access
& visitation plans
Ability to develop concurrent plans for infants in care
Ability to plan placement transitions
Ability to create a team to provide intervention
A repertoire of basic strategies to enhance parent sensitivity, cue reading & responsiveness, parental skills to regulate affect & manage behavior
Ability to recognize basic characteristics of evidence based therapeutic intervention programs
& appropriately utilize them
Parenting assessors
Case workers
Case managers
Intervention programs/services
Case managers
Home visitors
2
6. Skills for supporting infants in foster care
Knowledge of developmental/transactional framework for understanding traumatized infant/toddler behavior
Knowledge of common problems of traumatized infants/toddlers in foster care incl developmental delays, regulatory problems
(sleep, digestion & activity), behavior difficulties
Competency 1,2
Specific skills to reframe problem behaviour as developmental adaptations to stressful environments
Repertoire of strategies for helping caregivers recognize and cope with emotional trauma in young children
Specific strategies for handling sleep disturbance, food issues, attention & behaviour problems
Specific strategies to support language development
Foster care support workers
Foster parents
Case workers
7. Attachment for
Attorneys
Knowledge of attachment theory
& its application in family court
Knowledge of the ‘state of the evidence’ regarding forensic application of attachment theory
Knowledge of the implications of attachment theory for custody, access, termination of parental rights
Knowledge of evidence-based interventions for infant/parent relationship problems
Knowledge of common errors in reasoning & decisions affecting maltreated infants
Competency 1,2
Ability to use attachment theory appropriately in case presentations
Ability to recognize errors in judgment and reasoning in testimony
Ability to effectively advocate for the best interests of a maltreated infant
Judges, lawyers
FAMILY LAW INITIATIVES
COMMITTEE
Making Decisions About
Maltreated Babies
Training is being developed for
Judges
Lawyers
Child protection workers
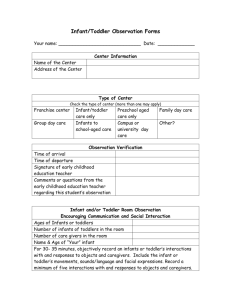
DEVELOPMENTAL SCREENING
-long waitlists meant infants and toddlers were sitting in care
-workers couldn’t accurately describe child’s needs to the court
How Can We Improve Practice?
A pilot project
All children between 0-5 were screened using the
ASQ and ASQ-SE
THEN
A program plan is developed by an ECE .
3
The Program Plan
Informs both the child’s plan of care and the access visits with the parents
Babies are born relationship ready
– their growth is dependent on the relationships they have in their daily life
LIAM
-admitted to care at 14 months
-developmental screen showed global delay, so a program plan was developed to address the issues in the foster home AND during access
-developmental assessment was booked, and now will be done – one year later
Training for Judges and
Lawyers
-Partnering with the National Judicial Institute to provide online training for judges
This can only help babies and toddlers before the court
Also- training for lawyers who represent babies and toddlers, parents, and Child protection
What kind of relationships do babies and toddlers need to support their mental health?
Responsive
–
I am here to meet your needs , comfort you and protect you
Engaged
–
I want to be with you, play with you, watch you grow and be a big part of your world as you are a big part of my world
Present
–
I am here in body, mind and soul , you have my full attention and my love
What experiences are VERY likely to be traumatic for infants and toddlers?
– Abuse
– Neglect / maltreatment
– Constant and consistent interactions that leave a child feeling disrespected, abandoned, rejected, unworthy, betrayed, ashamed, frightened
– Poverty
– Parental mental illness
– Maternal substance abuse
– Intimate Partner Violence (IPV)
– Exposure to violence
4
When a child is vulnerable to continued exposure to any of these experiences they are more likely to be traumatized
At the time of the trauma the protective factors surrounding a child may help a child overcome and recover from the event
But for too many infants and toddlers those factors are not consistently present in their lives
Emotional abuse and or neglect has no obvious visible scars
But… we can SEE poor mental health in infants and toddlers – if we know what to look for
There are behaviours that are indicative of poor infant mental health
There are developmental signs that should raise a flag
There is the absence of milestones that should cause concern
But can infants experience trauma symptoms?
Yes they most certainly can.
For example, it was concluded that “infants as young as 1-year-old can experience trauma symptoms as a result of hearing or witnessing
IPV.” in a study by G. Anne Bogat , Erika
DeJonghe, Alytia A. Levendosky, William S.
Davidson, Alexander von Eye (September
2005) www.msu.edu/~mis/publish/Infant_Trauma.pdf
Traumatic events/experiences
One parent is an abuser
Second parent removes child and her/himself from the situation
Parent accesses support
Protective Factors that may mitigate minimize impact
Baby or Toddler who has recovered from traumatic experience/event
Parental death
Other family members step in and provide the response the baby needs
Traumatic events/experiences
Limited/weak
Protective
Factors
Baby or Toddler unable to recover from trauma
Infant or Toddler suffering from poor mental health
Mother dies
Father emotionally vulnerable/ no one else to respond
(examples)
Trauma
Brain development
Overall development
Stress
Relationship/ attachment
Overall health
5
What happens when babies are exposed to threats
1. Insecure Attachment - They are vulnerable to insecure attachment
2. Developmental Delays - Their development is impeded and they experience developmental delays in other areas
3. Poor Health Outcomes - They become vulnerable to poor mental health and may be vulnerable to a lifetime of poor mental and physical health outcomes
4. Poor Brain Development – The profound development in the brain during this time is compromised and cannot always be recovered
What is Stressful to a Baby?
Stress response system (brain, nervous system, immune system) is highly sensitive but immature
Infants are entirely dependent on their caregiver to help them manage stress, arousal, & emotions – affect regulation
Toxic Stress & Brain Development
Toxic stress is the frequent, prolonged activation of the stress response system
Triggers the release of chemicals that impair brain development and functioning
World wide data on the lifelong implications of stress in early childhood
Normative, Developmentally Appropriate
Stress
A Continuum from Stress to Trauma
Emotionally
Costly Stress
Traumatic Stress
What causes stress?
What can be stressful to a Baby
- inadequate nutrition
- poor or absent stimulation
- inconsistent care
- lack of parental protection
- lack of emotional presence and connection between baby and caregiver
- absence of empathy/sympathy
- lack of response
What is Stress to a Baby?
Takes place in the caregiver relationship
Not specific event but chronic stress that impairs development
The repetitive & sustained failure to help infant manage distress
When caregivers are extraordinarily inconsistent, frightening, intrusive or neglectful
6
Poor Mental Health Can Impact the Attachment Relationship
“It is here, in the primacy of intimacy and trust, that trauma works it toxic and corrosive mischief. We have to understand that the child’s first self-image is mirrored in the eyes of his or her parents.”
(Pruett, 2007 in Young Children and Trauma)
A Secure Attachment is Important
For EVERY Baby & Toddler
The children in child welfare are no exception –
They need a secure attachment relationship
– Attachment can be difficult to assess when children cannot verbally tell you what they are feeling or experiencing
– Your observation of the attachment relationship may be the only clue to neglect or abuse with an infant and/or toddler
Your role in understanding a child’s attachment relationship
You cannot diagnose an attachment disorder
You can be familiar with the behaviors that may be indicative of a possible problem with attachment
You can be one of the first to recognize that an assessment is needed of the attachment relationship
You can be the one to make the appropriate referral for an assessment
While the family waits, you can be working with them to create opportunities for interactions that will support the attachment relationship
What can poor infant mental health look like when there is a disruption to the attachment relationship?
Poor attachment relationships
– Disruption of the attachment relationship is in itself trauma for a baby or toddler
– When disrupted, attachment can lead to behaviours such as
• The child searching for the absent parent figure
• Emotional withdrawal
• Disruptions in regulatory functions – disrupted sleep patterns
• Indifference to reminders of the caregiver
• Extreme sensitivity to reminders or to themes connected to separation or loss
• Extreme clinginess to the replacement caregiver
• Lack of interest in age appropriate activities
• Diminished appetite or food stuffing or hoarding
• Flat or sad affect
• Emotional withdrawal
• Lethargy
Adapted from Zeanah, Boris, Bakshi, and Lieberman (2000). Copyright by John Wiley & sons
Secure Attachment
Infants show a balance of attention to the mother and toys
They explore freely when the mother is present
When separated, the reactions may vary but upon reunion, their reactions are consistently very positive toward their mother
These mothers are very quick to respond to their baby with comfort when distressed
Secure Attachment
(Kendra Van Wagner)
7
Avoidant Attachment
With this pattern of attachment babies will:
– Appear to be quite independent and very busy with the toys their mother presents
– They will show little distress at her departure
– They may snub or ignore her upon her return
Moms are typically unresponsive to distress and seemed uncomfortable with close body contact
Avoidant Attachment
(Kendra Van Wagner)
Ambivalent/ Resistant
Attachment
These infants will:
– appear preoccupied with their mothers
– They explore very little even when mom is present
– They become very distressed when mom leaves
– They will seek comfort when reunited with mom, but will not settle and may even resist mom’s comfort
These moms are typically inconsistent in their response to their baby’s distress
Ambivalent/Resistant Attachment
(Kendra Van Wagner)
Disorganized Attachment
The fourth classification was later added by Main and colleagues
Babies have mixed strategies that use any combination of secure, avoidant and resistant attachment behaviors
This pattern is most predictive of later psychopathology
(Zeanah, 2009)
Disorganized Attachment
Kendra Van Wagner)
8
This Relationship is Essential
This attachment relationship is essential
Early development is dependent on relationships and the quality of experiences those relationships offer an infant
A baby who looks well cared for, may not be experiencing good care.
Poor Mental Health Can Impact
Development Leading to Delays
– Infants and toddlers who are experiencing neglect may also be experiencing developmental delays
– Delays can occur for organic reasons or they may be the result of abuse and/or neglect
– A delay that is undetected will not “resolve itself” when the child attends school at age 4
– Most children are not resilient enough to recover from a delay without serious intervention
Poor Mental Health Can Impact
Development Leading to Delays
– An untreated delay in the first three years will likely lead to more serious delays when child enter school
– the cost of intervention increases dramatically for every year interventions are not introduced
– cost refers to dollars and the impact on the child
– A developmental delay is not something that should left to the naked eye to determine
– there are tools that are easy to use to determine if a child is delayed
Your role in understanding a child’s development
You cannot diagnose
You can implement a developmental screen either in partnership with the biological family, the foster family, through your own observations or a combination of any two of the above
You can be trained on how to implement both a screen and curriculum based assessment tool
Your role in understanding a child’s development
You can reach out to community agencies such as Early Years Centres, children’s mental health agencies and ask for guidance with the creation of a developmental plan to support the needs of a child
You can refer parents to programs in the community that provide guidance around parenting and supporting development
Poor Mental Health Can Impact Health
Outcomes – Short and Long Term
We know that when young children experience poor mental health the impact is also on their physical health and well being
According to researchers at
Harvard, children who experience poor mental health experience higher rates of illnesses throughout life.
9
Health Outcomes:
Physiological /Medical Challenges
– You can be the FIRST RESPONDER
– You cannot diagnose
– You can make referrals to the appropriate professional who can diagnose
– You can be making observations that can be shared with other professionals (with parental consent) that could be very helpful – for instance, a child with poor muscle tone making observations of movements, any pain the child experiences etc… can be helpful to a clinician
– You can be reviewing medical records
– You can be consulting with/to the other disciplines involved with the case (with the appropriate consents)
Don’t be dismissive about what you may see with a child – if it doesn’t seem “normal” ask questions, observe more and keep observing
Brain Development
3/4 of brain development occurs between third trimester & age 2
90% of post-natal growth occurs before age 5
700 new neural connections are made every second in the first three years of life – but environment and experience can change that for a baby
This period of brain growth devours more calories than any other phase of development
According to Zero to Three (2010)
“A baby’s experiences and environment can change that course. For low-income babies, differences in world learning and development appear by 16 to 18 months of age, and patterns that suggest widening gaps are established by age 3” http://developingchild.harvard.edu/index.php/resources/multimedia/brain_hero/
10
The Window of Opportunity
The brain is producing 700 new synapses every
SECOND for the first 2-3 years of life
Excellent opportunity to change the life trajectory
Most vulnerable and sensitive period of development
Pruning depends on Experiences
Early experiences trigger genetic and biological adaptations that prepare the organism for what life will be like
Deprivation and abuse cause genetic, neurological, and biological changes
These include changes to the immune system, cardiovascular system, neurological system
Stress
The implications for child protection work are ominous
Brain Growth in the Early Months
newborn 1 month 3 months 6 months
Neglect: The Quiet Assault
Over pruning of synaptic connections
Same stress related impairments as trauma – including PTSD
Higher mortality rates (lifelong) from all causes – including random violence
Unresponsive parenting appears to be key
In these brain “heat maps red corresponds to high activity and blue connotes no activity
The different frequency bands (left-hand scale) reflect different types of brain activity
Across all frequencies, the level of activity was lower for children raised in
Romanian orphanages
(institutions with minimal interaction) than for those who grew up with their parents
11
Ask yourself this:
What
is
in
the
best
interest
of
the
baby?
- Put out of your mind
- The parents
- Society
- The Judge
- The lawyers
- Put in
- Research
- Brain development
- Attachment
- Self regulation
Development Counts but No
One is Watching
“Developmental structures are incorporated into later developmental structures, so that early competence tends to foster later competence, and early incompetence tends to promote later incompetence”
(Cicchetti & Cohen, 1995; Waters & Sroufe, 1983)
If this is the case how is that we don’t monitor development and respond to what a child needs?
12