Journal of Pediatric Surgery 49 (2014) 1237–1241
Contents lists available at ScienceDirect
Journal of Pediatric Surgery
journal homepage: www.elsevier.com/locate/jpedsurg
Outcome of patients after single-stage repair of perineal fistula without
colostomy according to the Krickenbeck classification
Kin Wai Edwin Chan ⁎, Kim Hung Lee, Hei Yi Vicky Wong, Siu Yan Bess Tsui, Yuen Shan Wong,
Kit Yi Kristine Pang, Jennifer Wai Cheung Mou, Yuk Him Tam
Division of Paediatric Surgery and Paediatric Urology, Department of Surgery, The Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong
a r t i c l e
i n f o
Article history:
Received 21 August 2013
Received in revised form 6 November 2013
Accepted 12 November 2013
Key words:
Anorectal malformation
Perineal fistula
Krickenbeck
Single stage repair
a b s t r a c t
Purpose: The aim of the study is to assess the characteristics and outcome of anorectal malformation (ARM)
patients who underwent single-stage repair of perineal fistula without colostomy according to the
Krickenbeck classification.
Methods: From 2002 to 2013, twenty-eight males and four females with perineal fistula who underwent
single-stage repair without colostomy in our institute were included in this study. Patients with perineal
fistula who underwent staged repair were excluded. Demographics, associated anomalies, and operative
complications were recorded. The type of surgical procedures and functional outcome were assessed using
the Krickenbeck classification.
Results: Six patients had associated anomalies, including two patients with renal, two with cardiac, one with
vertebral, and one with limb abnormalities. Thirteen patients underwent perineal operation, and fourteen
patients underwent anterior sagittal approach in the neonatal period. One patient underwent anterior sagittal
approach, and four patients underwent PSARP beyond the neonatal period. One patient had an intra-operative
urethral injury and one a vaginal injury. Complications were not associated with the type of surgical
procedure (p = 0.345). All perineal wounds healed without infection. By using the Krickenbeck assessment
score, all sixteen children older than five years of age had voluntary control. One patient had grade 1 soiling,
and no patient had constipation.
Conclusions: Single-stage operation without colostomy was safe with good outcomes in patients with perineal
fistula. The use of Krickenbeck classification allows standardization in assessment on the surgical approach
and on functional outcome in ARM patients.
© 2014 Elsevier Inc. All rights reserved.
Traditionally, anorectal malformations (ARM) were classified as
high, intermediate or low anomalies according to the Windspread
classification [1]. According to Peña, a colostomy was performed in all
children with ARM [2]. In children with perineal fistula, the approach
of definite repair was posterior sagittal anorectoplasty (PSARP) [2].
Recently, there were reports evaluating a single-stage repair in patients with perineal fistula without a colostomy [3,4]. Anoplasty, cutback operation or anterior sagittal anorectoplasty (ASARP) was the
technique reported [3,4].
Regarding the tools used in outcome assessment, varied assessment
scoring systems were adopted worldwide [5]. With the presence of
different classification systems, it was difficult to compare the outcomes in patients with ARM between different centers.
Since the introduction of the Krickenbeck classification in 2005 [6],
there have been an increasing number of publications using this
system to classify the anatomy and assess postoperative results [7–9].
⁎ Corresponding author at: Division of Paediatric Surgery & Paediatric Urology, Department of Surgery, The Chinese University of Hong Kong, Prince of Wales Hospital,
Hong Kong SAR, China. Tel.: +86 852 26322953.
E-mail address: edwinchan@surgery.cuhk.edu.hk (K.W.E. Chan).
http://dx.doi.org/10.1016/j.jpedsurg.2013.11.054
0022-3468/© 2014 Elsevier Inc. All rights reserved.
However, a report which only focused on patients with perineal fistula
using the Krickenbeck classification was lacking. The assessments of
children with perineal fistula (Fig. 1) were often grouped together
with patients with vestibular fistula or with patients without a fistula
as ‘low-type’ ARM [10,11]. The aim of this study is to assess the
surgical procedures (Table 1) and outcome (Table 2) of patients with
perineal fistula using the Krickenbeck classification.
1. Materials and methods
From January 2002 to June 2013, 28 males and 4 females with
perineal fistula in our institute were included in this study. Our hospital is a tertiary referral pediatric surgical center. All patients presenting with a perineal fistula underwent single-stage repair without
protective colostomy. Patients with perineal fistula who underwent
colostomy in other hospitals or patients who underwent initial colostomy because the perineal fistula was not apparent at birth were
excluded from this study. VACTERL screening was performed in all
patients born with perineal fistula.
Demographics and associated anomalies were recorded. The surgical procedure was classified according to the Krickenbeck system.
1238
K.W.E. Chan et al. / Journal of Pediatric Surgery 49 (2014) 1237–1241
Table 2
International classification (Krickenbeck) for postoperative results.
1. Voluntary bowel movements
Yes/no
Feeling of urge,
capacity to verbalize,
hold the bowel movement
Fig. 1. A female with a perineal fistula.
The principle of the operation was to mobilize and place the anorectum within the sphincter complex.
2. Soiling
Yes/no
Grade 1
Grade 2
Grade 3
Occasionally (once or twice per week)
Every day, no social problem
Constant, social problem
3. Constipation
Yes/no
Grade 1
Grade 2
Grade 3
Manageable by changes in diet
Requires laxative
Resistant to laxatives and diet
fistula opening. The mobilization of anorectum and reconstitution
of the perineal body are similar to the technique described in the
anterior sagittal approach.
2. Operative technique
6. Post-operative management
Parenteral antibiotics (cefuroxime and metronidazole) were given
on induction of general anesthesia. A urethral catheter was placed
preoperatively. In neonates, the patient was positioned supine with
both legs wrapped, elevated and fixed to the handle bar of the operative table. For patients who underwent operation beyond the
neonatal period, dilatation of the fistula opening was performed
regularly before the operation. Rectal washout was performed the day
before operation. The use of the anterior sagittal approach or posterior
sagittal anorectoplasty (PSARP) depended on the surgeon’s preference. The center of the sphincter complex was defined by an electrical muscle stimulator. In all the cases, rectal washout was performed
after the anoplasty but before reversal of general anesthesia. The
definition of different surgical approaches was described as follows:
Parenteral antibiotics were continued for 5–7 days post-operatively. Feedings were started 2–3 days after the operation. The
perineal wound was irrigated with saline solution three times per
day in the early post-operative period. Anal dilatation was started
2 weeks after the operation. The dilatation was carried out regularly
3. Perineal operation
The patient was placed in a supine position. Only a limited perineal
dissection was required to mobilize and place the anorectum within
the sphincter complex because the fistula opening was close to the
sphincter complex (Fig. 2).
4. Anterior sagittal approach
The patient was placed in a supine position. A more extensive
mobilization of anorectum and reconstitution of the perineal body
were required in order to place the anorectum within the sphincter
complex (Fig. 3).
5. PSARP
The patient was placed in a prone position. The incision was
extended from the posterior border of the sphincter complex to the
Table 1
International grouping (Krickenbeck) of surgical procedures for follow-up.
Perineal operation
Anterior sagittal approach
Sacroperineal procedure
PSARP
Abdominosacroperineal pull-through
Abdominoperineal pull-through
Laparoscopic-assisted pull-through
Fig. 2. (A) A patient with the anorectum located slightly anterior to the sphincter
complex. (B) Perineal dissection was performed.
K.W.E. Chan et al. / Journal of Pediatric Surgery 49 (2014) 1237–1241
1239
had delayed diagnosis. The diagnosis of ARM was missed in the neonatal check-up. They presented with constipation and the actual
diagnosis was made at 8 and 12-months-old respectively. One patient
underwent anterior sagittal approach and the other a PSARP.
Intra-operative complications encountered in this study included
urethral injury in a boy during anterior sagittal approach and a girl
who suffered a vaginal injury during PSARP. The injuries were noted
and repaired intraoperatively with no adverse outcome. Regarding
the risk of intra-operative complication, no significant differences
were observed between the perineal operation group and the anterior
sagittal approach/PSARP group (p = 0.345) (Table 3). Post-operatively, all perineal wounds healed without infection. There were no
instances of wound dehiscence or rectal prolapse. None of the patients
required a salvage colostomy.
All 16 children older than 5 years of age had voluntary control. One
patient had grade 1 soiling and none of the patients had constipation
(Table 4). There was no instances of urinary incontinence. The two
patients with delayed diagnosis were too young for the functional
outcome assessment.
8. Discussion
Fig. 3. (A) Another patient with perineal fistula. (B) Anterior sagittal approach
was performed.
up to a 14 Hegar dilator size. A bowel management program involving
the pediatric surgeons and nurse specialists was offered to all patients.
Post-operative complications including wound infection, wound
dehiscence, rectal prolapse and the need of colostomy were recorded.
The functional outcome was assessed in patients older than 5 years of
age using the Krickenbeck classification.
Statistical analysis was accomplished using the SPSS program for
Windows 15.0 (SPSS, Chicago, Illinois, USA). Fisher exact test was
used to compare the categorical data with a p b 0.05 considered
statistically significant. The study was approved by the local clinical
research ethical committee.
7. Results
On VACTERL screening, 6 patients had associated anomalies. Two
patients had cardiac anomalies including one with an atrial septal
defect and one with pulmonary artery branche turbulence. Two
patients had renal anomalies including 1 with a horseshoe kidney and
1 with vesicoureteral reflux. One patient had spina bifida occulta and
one had an extra-thumb. Regarding the patient with spina bifida
occulta, the MRI did not detect any spinal cord anomaly.
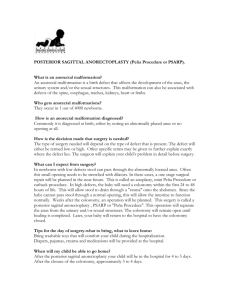
The surgical procedures performed are listed in Fig. 4. Regarding
the three patients who were diagnosed with ARM at birth but the
operation was performed beyond the neonatal period; were labeled as
anterior displaced anus at birth. Regular anal dilatation was carried
out until PSARP was performed at 1–3 months of age. Two patients
Two infants had delayed diagnosis. If the diagnosis was made at
birth, traditionally they were described as having an anterior
displaced anus. These patients were now grouped under the category
of ‘perineal fistula’ according to the Krickenbeck classification [3].
When the diagnosis was made at birth, regular dilatation of the
perineal openings was performed and effective passage of feces was
observed in the neonatal period [7]. However, children with delayed
diagnosis presented with constipation after the introduction of more
solid food as noticed in this study. In those children with this diagnosis at birth, we would delay the repair after the neonatal period
after considering the non-urgent status of this condition and to
balance the risk of general anesthesia in the neonatal period.
In performing a neonatal repair, placing the patient in the supine
position can provide excellent exposure of the perineum and
eliminate the possible adverse effects in ventilation when the neonate is placed in prone position. Harjai et al. preferred the use of
anterior sagittal approach in the management of vestibular fistula as
it may provide better exposure for the anterior dissection where
separation of the vagina and rectum takes place under direct vision
[12]. We observed the operative view when the patients were positioned in supine position was as good as the prone position.
The most obvious advantage of single-stage repair of perineal
fistula is to avoid 2 additional operations. Besides, colostomy related
complications were not uncommon [13]. Peña et al. reported 616
colostomy related complications in 464 ARM patients [13]. However,
a single-stage operation was not entirely without risk [10]. In our
study, one patient has urethral injury and one a vaginal injury. They
all underwent a more extensive sagittal approach (Table 3). The
urethra in the male and the vagina in the female were in fact in close
proximity with the fistula opening. Despite placing a urethral catheter
in all the cases, meticulous dissection is still required during dissection of the anterior rectal wall. Of course with less dissection, the
chance of injury to surrounding tissue is reduced. Pakarinen et al.
compared anoplasty to PSARP and concluded that anoplasty was safer
and less prone to complications [7]. However, since the principle of
the operative approach was different, their conclusion cannot directly
be applied in this study.
All patients were free of perineal wound infection post-operatively.
Since the majority of the cases were operated in the early neonatal
period, neonatal repair may be one of the reasons for the zero infection
rate. Albanese et al. performed a one stage repair for ‘high’ type
anorectal malformation and no perineal wound infection was observed
[14]. They suggested the neonatal bowel was theoretically sterile when
the surgery was performed. A proper peri-operative care program
1240
K.W.E. Chan et al. / Journal of Pediatric Surgery 49 (2014) 1237–1241
ARM with perineal
fistula
n = 32 (28M, 4F)
Diagnosis at birth
Delay in diagnosis
n = 30 (27M, 3F)
n = 2 (1M, 1F)
Operation within
Operation beyond
Anterior sagittal
PSARP
neonatal period
neonatal period
Approach
n = 1 (F)
n = 27 (26M, 1F)
n = 3 (1M,2F)
n = 1 (M)
Perineal operation
PSARP
n = 13 (12M,1F)
n = 3 (1M,2F)
Anterior sagittal
approach
n = 14 (14M)
n=number of patients, M=male, F=Female
Fig. 4. A flow chart showing the surgical procedures performed in ARM patients with perineal fistula according to the Krickenbeck classification. n = number of patients, M = male,
F = Female.
consisted of antibiotics, rectal washout and wound irrigation was
essential for successful single stage repair without the need of salvage
colostomy [15].
In this study, using the Krickenbeck classification, all patients were
free from constipation and only 1 patient had grade 1 soiling.
Constipation was reported as a major problem in patient with ‘lowtype’ ARM including patients with perineal fistula. The incidence of
constipation is around 50% in various reports [4,7,16]. Of course it was
very difficult to compare the results since the inclusion criteria of the
various studies were different. Some studies included patients with
anal stenosis or vestibular anus. Hassett et al. studied the 10 year
outcome in all ARM patients using the Krickenbeck classification after
PSARP [4]. 21% of patients with perineal fistula had grade 2 constipation
and 1 patient required a Malone antegrade continence enema (MACE),
but since this study involved all ARM patients, clinical details including
the associate anomalies and the incidence of protective colostomy in
patients with perineal fistula were not documented.
Associated anomalies, in particular spinal anomalies may have
adverse effect in the functional outcome [4]. Overall the incidence of
associated anomalies was 19% but none of the patients had spinal
cord anomalies. The incidence is lower when compared with other
reports. Hassett et al. reported 31% of patients with perineal fistula
Table 3
Relationship between the type of surgical procedures and the incidence of
complications.
Table 4
Functional outcome of the 16 children older than 5 years of age according to the
Krickenbeck assessment system.
Surgical procedures
Number of patients
Complications⁎
p value
Surgical procedures
Voluntary control
Constipation
Soiling
Perineal dissection
Anterior sagittal approach/PSARP
Total number
13
19
32
0
2
2
0.345
Perineal operation (n = 8)
Anterior sagittal approach
(n = 7)
PSARP (n = 1)
8
7
0
0
1 (Grade 1)
0
1
0
0
⁎ Complications – 1 patient had urethral injury and 1 patient had vaginal injury.
K.W.E. Chan et al. / Journal of Pediatric Surgery 49 (2014) 1237–1241
had associate anomalies using the Krickenbeck classification [4].
Screening for associated anomalies is required in patients with
perineal fistula [17].
We believe one of the reasons for the good functional outcome
achieved was to place the anorectum within the sphincter complex. In
contrast to previous reports, the aim of ‘anoplasty’ was not to place the
anorectum within the sphincter complex [16]. They suggested the
fistula opening although anteriorly displaced, was still partially
encased by the sphincter [7,16]. Pakarinen et al. reported there was
no difference in outcome between anoplasty and PSARP in the
management of perineal fistula [16]. In their study, 43% of children
after anoplasty and 60% children after colostomy had constipation.
However a recent study using 3D reconstruction showed the vertical
sphincter fibers did not wrapped around the distal end of the perineal
fistula [18]. The author suggested using the cutback technique it was
difficult to place the anorectum into the sphincter complex. In
addition, Lombardi et al. noticed abnormalities of the muscle coat
and the nervous system of the anorectal canal in patients with perineal
fistula. They suggested resection of the distal fistula may permit a
better functional result [19]. The majority (90%, 27/30) of patients with
the diagnosis at birth underwent primary operation within 72 hours
after birth. Even in patients who underwent anal dilatation, operation
was carried out within 3 months of age. The brain-defecation reflex
can be maintained in patients that underwent early operation and may
lead to a better functional outcome [14,20]. In addition, the implementation of a post-operative bowel management program was an
important factor that contributed to the good outcome [21].
Our experience show that single-stage repair of perineal fistula
with the aim in placing the anorectum within the sphincter complex
is safe, feasible and is associated with a good functional outcome. The
use of the Krickenbeck classification allows more standardized
documentation of the diagnosis, procedure and the outcome. A
more direct comparison of our results with future studies in other
institutions is possible.
Disclosures
Drs. Kin Wai Edwin Chan, Kim Hung Lee, Hei Yi Vicky Wong, Siu
Yan Bess Tsui, Yuen Shan Wong, Kit Yi Kristine Pang, Jennifer Wai
Cheung Mou, Yuk Him Tam have no conflicts of interest or financial
ties to disclose.
Acknowledgments
Nil.
1241
References
[1] Murphy F, Puri P, Hutson JM, et al. Incidence and Frequency of Different Types, and
Classification of Anorectal Malformations, in Holshneider AM, Hutson JM (eds):
Anorectal Malformations in Children. Springer-Verlag Berlin, pp163-84.
[2] deVries P, Pena A. Posterior anorectoplasty. J Pediatr Surg 1982;17:638–43.
[3] Kuijper CF, Aronson DC. Anterior or posterior sagittal anorectoplasty without
colostomy for low-type anorectal malformation: how to get a better outcome?
J Pediatr Surg 2010;45(7):1505–8.
[4] Kumar B, Kandpal DK, Sharma SB, et al. Single-stage repair of vestibular and
perineal fistulae without colostomy. J Pediatr Surg 2008;43(10):1848–52.
[5] Ochi T, Okazaki T, Miyano G, et al. A comparison of clinical protocols for assessing
postoperative fecal continence in anorectal malformation. Pediatr Surg Int 2012;
28(1):1–4.
[6] Holschneider A, Hutson J, Pena A, et al. Preliminary report on the International
Conference for the Development of Standards for the Treatment of Anorectal
Malformations. J Pediatr Surg 2005;40:1521–6.
[7] Hassett S, Snell S, Hughes-Thomas A, et al. 10-year outcome of children born
with anorectal malformation, treated by posterior sagittal anorectoplasty, assessed according to the Krickenbeck classification. J Pediatr Surg 2009;44(2):
399–403.
[8] England RJ, Warren SL, Bezuidenhout L, et al. Laparoscopic repair of anorectal
malformations at the Red Cross War Memorial Children's Hospital: taking stock.
J Pediatr Surg 2012;47(3):565–70.
[9] De Vos C, Arnold M, Sidler D, et al. A comparison of laparoscopic-assisted (LAARP)
and posterior sagittal (PSARP) anorectoplasty in the outcome of intermediate and
high anorectal malformations. S Afr J Surg 2011;49(1):39–43.
[10] Pakarinen MP, Rintala RJ. Management and outcome of low anorectal malformations. Pediatr Surg Int 2010;26:1057–63.
[11] Javid PJ, Barnhart DC, Hirschl RB, et al. Immediate and long-term results of
surgical management of low imperforate anus in girls. J Pediatr Surg 1998;33(2):
198–203.
[12] Harjai MM, Sethi N, Chandra N. Anterior sagittal anorectoplasty: An alternative to
posterior approach in management of congenital vestibular fistula. Afr J Paediatr
Surg Apr-Jun 2013;10(2):78–82.
[13] Pena A, Migotto-Krieger M, Levitt MA. Colostomy in anorectal malformations: a
procedure with serious but preventable complications. J Pediatr Surg 2006;41(4):
748–56.
[14] Albanese C, Jennings R, Lopoo J, et al. One-stage correction of high imperforate
anus in the male neonate. J Pediatr Surg 1999;34:834–6.
[15] Sharma S, Gupta DK. Delayed presentation of anorectal malformation for definitive surgery. Pediatr Surg Int 2012;28(8):831–4.
[16] Pakarinen MP, Goyal A, Koivusalo A, et al. Functional outcome in correction of
perineal fistula in boys with anoplasty versus posterior sagittal anorectoplasty.
Pediatr Surg Int 2006;22(12):961–5.
[17] Nah SA, Ong CC, Lakshmi NK, et al. Anomalies associated with anorectal
malformations according to the Krickenbeck anatomic classification. J Pediatr
Surg 2012;47(12):2273–8.
[18] Watanabe Y, Takasu H, Mori K. Unexpectedly deformed anal sphincter in low-type
anorectal malformation. J Pediatr Surg 2009;44(12):2375–9.
[19] Lombardi L, Bruder E, Caravaggi F, et al. Abnormalities in "low" anorectal
malformations (ARMs) and functional results resecting the distal 3 cm. J Pediatr
Surg 2013;48(6):1294–300.
[20] Liu G, Yuan J, Geng J, et al. The treatment of high and intermediate anorectal
malformations: one stage or three procedures? J Pediatr Surg 2004;39:
1466–71.
[21] Schmiedeke E, Busch M, Stamatopoulos E, et al. Multidisciplinary behavioural
treatment of fecal incontinence and constipation after correction of anorectal
malformation. World J Pediatr 2008;4(3):206–10.