Return to fertility after cessation of a continuous oral contraceptive
advertisement

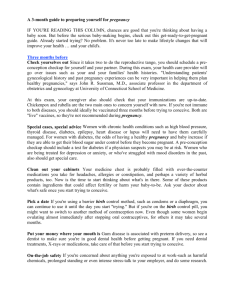
Return to fertility after cessation of a continuous oral contraceptive Kurt Barnhart, M.D., M.S.C.E.,a Sebastian Mirkin, M.D.,b Gary Grubb, M.D., M.P.H.,b and Ginger Constantine, M.D.b a b Department of Obstetrics and Gynecology, PENN Fertility Care, University of Pennsylvania, Philadelphia, Pennsylvania; and Women’s Health, Clinical Research and Development, Wyeth Research, Collegeville, Pennsylvania Objective: To evaluate the return to fertility among women planning to become pregnant after the use of a continuous regimen of levonorgestrel 90 mg and ethinyl E2 20 mg. Design: Descriptive analysis of pregnancy outcomes after participation in a contraceptive trial. Setting: Multicenter trial. Subject(s): Participants in a phase 3 contraceptive trial who discontinued to become pregnant. Intervention(s): Eligible subjects were contacted at 3 and 12 months after treatment discontinuation to determine if and when they had conceived. Main Outcome Measure(s): Kaplan-Meier analysis displaying the time until conception after oral contraceptive discontinuation. Result(s): In the phase 3 trial, 34 of 2,134 subjects cited a desire for pregnancy as a reason for discontinuation. Of these, 4 were already pregnant before stopping treatment, 4 initiated other contraception, and 5 were lost to followup. Of the remaining 21 subjects at risk of pregnancy, the pregnancy rate was 57% at 3 months, 81% at 12 months, and 86% (18 of 21) (95% confidence interval 64% to 97%) at 13 months after discontinuation of treatment. Conclusion(s): These findings suggest that a continuous oral contraceptive with levonorgestrel 90 mg and ethinyl E2 20 mg does not delay the return to fertility. (Fertil Steril 2009;91:1654–6. 2009 by American Society for Reproductive Medicine.) Key Words: Return to fertility, oral contraceptive, low-dose, continuous, noncyclic The traditional oral contraceptive (OC) 28-day cycle regimen of 21 active pills and 7 placebo pills was created to promote monthly withdrawal bleeding and mimic the natural menstrual cycle (1). However, many common adverse effects associated with OCs, including pelvic pain, breast tenderness, bloating or swelling, and use of pain medications, become significantly worse during the 7-day hormone-free interval than during the 21 days that women are taking estrogen and progestin, especially in long-term OC users (2). Continuous OC use (a pill is taken every day without a pill-free or placebo interval) eliminates the hormone-free interval and subsequent withdrawal bleeding associated with cyclic OCs, although breakthrough bleeding is common (3). Some hormonal contraceptive options such as depot medroxyprogesterone lead to amenorrhea, which may in turn lead to a delay in return to fertility because of hypothalamic Received October 15, 2007; revised February 8, 2008; accepted February 13, 2008; published online May 7, 2008. Supported by a grant from Wyeth Research, Collegeville, Pa. K.B. was an investigator for this poststudy follow-up and received research funding from Wyeth Research, Collegeville, Pa. Other sources of research funding and/or financial relationships include Novo Nordisk (consultant), Organon (speaker and investigator), Johnson & Johnson, Duramed, Xanodyne, Boehringer Ingelheim, Third Wave, Pfizer, and MGI Pharma (investigator). S.M., G.G., and G.C. are employees of Wyeth Research. Other financial affiliation for G.G. is Johnson & Johnson. S.M. and G.C. have no other financial affiliation to disclose. Reprint requests: Kurt Barnhart, M.D., M.S.C.E., 3701 Market St., Ste. 801, Philadelphia, PA 19104 (FAX: 215-615-4200; E-mail: kbarnhart@ obgyn.upenn.edu). 1654 suppression and anovulation (4, 5). Theoretically continuous OC use could also result in hypothalamic suppression. Even with cyclic OCs, the question of return to fertility or time to pregnancy has been controversial for some time (6, 7). Some data suggest that although there may be a slight delay in time to pregnancy compared with after discontinuation of cyclic combination OCs, no permanent impairment results (8). This report describes the return to fertility of women after using a continuous combined low-dose formulation containing levonorgestrel 90 mg and ethinyl E2 20 mg (LNG/EE). MATERIALS AND METHODS This was a prospective follow-up of subjects that took place after their participation in a large phase 3, multisite, openlabel contraceptive trial of a low-dose continuous LNG/EE (3). Criteria for inclusion in the phase 3 study included healthy women aged 18 to 49 years who were sexually active and at risk for becoming pregnant and had regular (21- to 35-day) menstrual cycles for 3 months preceding their first clinic visit. Exclusion criteria included standard contraindications for OCs and use of drugs or conditions that could interfere with contraceptive efficacy. The phase 3 study and poststudy follow-up process were reviewed by the Institutional Review Board at each site and an independent ethics committee and conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and are consistent with good clinical practice and the applicable regulatory requirements. All participants provided written informed consent. Fertility and Sterility Vol. 91, No. 5, May 2009 Copyright ª2009 American Society for Reproductive Medicine, Published by Elsevier Inc. 0015-0282/09/$36.00 doi:10.1016/j.fertnstert.2008.02.122 The primary endpoint of this follow-up study was return to fertility within 12 months after the last dose of continuous LNG/EE. Subjects were included in this follow-up study regardless of the length of time that they took continuous LNG/EE (see Table 1). Women who stopped treatment because they said they planned to become pregnant were contacted twice by phone at 3 and 12 months after discontinuation of continuous LNG/EE to determine whether they were pregnant. At each contact, subjects reported if and when they had conceived. If subjects were not pregnant, they were asked if they still were trying to conceive or if they had resumed contraception. A Kaplan-Meier analysis of the time from treatment discontinuation to estimated day of conception was performed. RESULTS Of the 2,134 women included in the phase 3 trial, 34 stopped taking continuous LNG/EE because they planned to become pregnant. Of these 34 subjects, 4 were found to be pregnant before the start of the follow-up process and were contraceptive failures in the phase 3 trial, 4 initiated other contraception in the first month after discontinuation of the continuous OC (despite previously stated interest in planning a pregnancy), and 5 were lost to follow-up. For the remaining 21 subjects, the mean SD duration of treatment with continuous LNG/ EE was 197 120.2 days (range, 27 to 364 days). The demo- graphic characteristics of the 21 subjects are listed in Table 1. Compared with the phase 3 population (3), these subjects were younger (mean age, 26.9 and 29.5 years, respectively) and of lower mean body weight (mean weight, 67.0 and 72.4 kg, respectively). Six (28.6%) subjects were nulligravid compared with 38.5% in the phase 3 study. The pregnancy rate was 57% (12 of 21; 95% confidence interval [CI] 34% to 78%) at 3 months and 81% (17 of 21; 95% CI 58% to 95%) at 12 months after discontinuation of continuous LNG/EE (Fig. 1). The median time from treatment discontinuation to estimated date of conception was 4 months. After the 12-month poststudy follow-up, information was sought on the remaining 4 of 21 subjects who had not become pregnant. One subject had an estimated date of conception of 376 days after the last treatment, for a total 13-month pregnancy rate of 86% (18 of 21; 95% CI 64% to 97%). For the 3 remaining subjects who did not conceive (including 1 nulligravid subject), 1 had stopped trying to become pregnant by 12 months, and 2 were lost to follow-up after 12 months. The 18 pregnancies resulted in 17 live births and 1 spontaneous abortion. Twelve reported delivery outcomes of healthy babies. The reported Apgar scores (n ¼ 9) were R9 at 5 minutes, and the reported weights (n ¼ 10) averaged 3.54 kg (range, 3.26 kg to 4.08 kg). TABLE 1 Demographic characteristics and time to pregnancy in women who discontinued a continuous combined OC containing LNG 90 mg and EE 20 mg to become pregnant. Subject 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Age (y) Race Weight (kg) Gravidity/parity Days in study Time (d) to pregnancy after last continuous LNG/EE OC 22 25 31 25 23 28 30 30 21 25 30 32 26 27 24 25 24 31 26 35 27 Hispanic White White White White White White White White White White White White Black White White White White White White White 52.7 66.4 62.3 69.2 66.5 59.2 69.1 48.4 55.0 82.7 71.4 56.4 55.4 110.0 59.6 53.6 70.7 82.7 74.6 71.9 68.2 1/1 3/3 2/1 3/3 1/1 1/0 2/1 1/1 0/0 0/0 2/2 2/1 0/0 2/0 1/0 0/0 0/0 2/2 1/0 1/1 0/0 334 126 168 241 274 80 364 33 133 130 48 364 120 110 160 364 152 189 364 364 27 14 17 19 20 32 41 47 49 68 75 77 107 111 127 131 212 261 376 Lost to follow-up Not pregnant Not pregnant Barnhart. Continuous OC and return to fertility. Fertil Steril 2009. Fertility and Sterility 1655 FIGURE 1 tility (6) and differences in study methodology, notably data collection after the delivery. Time to return to fertility. Kaplan-Meier survival function estimates. The primary limitation of this poststudy follow-up was the small number of patients with no comparison group. However, these data are consistent with other findings regarding the impact of fertility of current cyclic hormonal contraception, and they are supported by a separate study after the phase 3 trial of the continuous LNG/EE OC. Among 187 women who stopped OC use after 6 to 12 months and completed 3 months of follow-up, the median time to return to menses was 32 days, and the incidence of spontaneous menses or pregnancy within 90 days was 98.9% (13). Based on a pregnancy rate of 86% at 13 months, the return to fertility after up to 13 months of use of a continuous LNG/ EE is comparable to that of cyclic OCs. These findings suggest that a continuous OC of 90 mg LNG and 20 mg EE does not delay return to fertility. Barnhart. Continuous OC and return to fertility. Fertil Steril 2009. DISCUSSION This is the first report to address the concern that the prolonged amenorrhea that occurs with continuous OC use may affect return to fertility and suggests that there is no delay in return to fertility after use of continuous LNG/EE. Among the 21 women who planned to become pregnant and remained at risk of pregnancy after stopping continuous LNG/EE OC, 86% became pregnant within 13 months after the discontinuation of the OC. These findings are supported by a recent case study that showed the rapid resumption of ovulation and menstruation after stopping use of a continuous combined OC containing LNG/EE (9). The pregnancy rate shown in this poststudy follow-up of continuous OCs is comparable with that shown in several studies of cyclic OCs. The larger studies have shown a 1year return-to-fertility rate of 84% to 88% following cyclic OC use (6, 7, 10, 11). Two of these studies (6, 7) had a nonhormonal contraceptive comparison group and the time to pregnancy was longer for cyclic OC users than for nonhormonal contraceptive users. In one study (6), the time to pregnancy was 5.88 cycles for OC users versus 3.18 cycles (P<.001) for users of various nonhormonal methods (i.e., intrauterine device, barrier, rhythm, and withdrawal). This study also found that 88% of former OC users were pregnant after 12 months. In another study (7), the time to pregnancy was 7.7 months for former OC users versus 3.9 months (adjusted P<.001) for condom users, with a total of 83.8% of OC users having conceived by 12 months. One exception to the larger study findings of a 12-month return-to-fertility rate in the 84% to 88% range is a 1982 study (12) of married women, which found a 1-year return-tofertility rate of 72% following OC discontinuation. Possible explanations for this outlying result could be the higher doses of OCs used in the early 1980s delaying return to fer1656 Barnhart et al. Continuous OC and return to fertility Acknowledgments: The authors acknowledge the contribution of the principal investigators and staff at the clinical sites that conducted the study protocol and thank Vincent Haudiquet, Ph.D., of Wyeth Research for the statistical analysis and Mr. John Patton of Wyeth Research for assistance in the preparation of this manuscript. REFERENCES 1. Sulak PJ, Kuehl TJ, Ortiz M, Shull BL. Acceptance of altering the standard 21-day/7-day oral contraceptive regimen to delay menses and reduce hormone withdrawal symptoms. Am J Obstet Gynecol 2002;186: 1142–9. 2. Sulak PJ, Scow RD, Preece C, Riggs MW, Kuehl TJ. Hormone withdrawal symptoms in oral contraceptive users. Obstet Gynecol 2000;95: 261–6. 3. Archer DF, Jensen JT, Johnson JV, Borisute H, Grubb GS, Constantine GD. Evaluation of a continuous regimen of levonorgestrel/ ethinyl estradiol: phase 3 study results. Contraception 2006;74:439–45. 4. Schwallie PC, Assenzo JR. The effect of depo-medroxyprogesterone acetate on pituitary and ovarian function, and the return of fertility following its discontinuation: a review. Contraception 1974;10: 181–202. 5. Pardthaisong T, Gray RH, McDaniel EB. Return of fertility after discontinuation of depot medroxyprogesterone acetate and intra-uterine devices in Northern Thailand. Lancet 1980;1:509–12. 6. Bracken MB, Hellenbrand KG, Holford TR. Conception delay after oral contraceptive use: the effect of estrogen dose. Fertil Steril 1990;53:21–7. 7. Hassan MAM, Killick SR. Is previous use of hormonal contraception associated with a detrimental effect on subsequent fecundity? Hum Reprod 2004;19:344–51. 8. Stenchever MA, Droegemuller W, Herbst AL, Mishell D. Comprehensive gynecology. 4th ed. St. Louis: Mosby, 2001. 9. Craig LB, Miller L, Criniti A. Rapid resumption of ovulation and menstruation following continuous use of the combination oral contraceptive [abstract]. Fertil Steril 2005;83:S16. 10. Farrow A, Hall MGR, Northstone K, Taylor H, Ford WCL, Golding J. Prolonged use of oral contraception before a planned pregnancy is associated with a decreased risk of delayed conception. Hum Reprod 2002;10:2754–61. 11. Wiegratz I, Mittman K, Dietrich H, Zimmermann T, Kuhl H. Fertility after discontinuation of treatment with an oral contraceptive containing 30 mg of ethinyl estradiol and 2 mg of dienogest. Fertil Steril 2006;85:1812–9. 12. Linn S, Schoenbaum SC, Monson RR, Rosner B, Ryan KJ. Delay in conception for former ’pill’ users. JAMA 1982;247:629–32. 13. Davis AR, Kroll R, Soltes B, Haudiquet V, Zhang N, Grubb GS. The occurrence of menses or pregnancy after cessation of a continuous oral contraceptive. Fertil Steril 2008;89:1059–63. Vol. 91, No. 5, May 2009