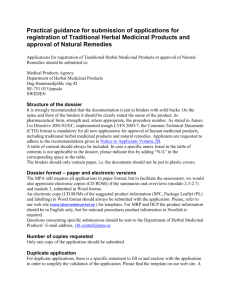
Monographs of Medicinal Plants in formulations supposedly used to
advertisement

MONOGRAPHS ON SELECTED MEDICINAL PLANTS OF GHANA LAUNCHED BY THE MINISTRY OF HEALTH Introduction One of the key challenges to the development of African traditional Medicine is that it has not been written down let alone codifying and standardizing it into a body of knowledge or into a single compendium for its official protection, development or study. The knowledge has been passed on by oral tradition from generation to generation but a considerable amount of the knowledge has now reached the public domain by way of individuals who are willing to share the knowledge, and through research and scientific publications. This was made possible partly due to community education, the activities of researchers and Ethno-medical anthropologists. Through training of traditional medicine practitioner, there has been increased understanding and goodwill between indigenous health practitioners and modern bio-medical scientist although part of traditional medicine knowledge is still held as secret between very few close family members. There is however, enough knowledge in the public domain for research and development of potentially useful medicines. This development together with other factors such as the search for better and safer medicines, availability of scientific and technological capacity to harness indigenous knowledge, has brought about the resurgence of interest in herbal medicines in even the most highly industrialized countries. Paradoxically, in this area where Africa ought to have a comparative advantage, we have highly stigmatized herbal and natural medicine due to its association to some bad practices and magicoreligious activities. There is also low application of technology, lack of data-bases and networks for scientific information and standard documents that would have driven medicines development and regulation. However, contrary to opinion in many circles that traditional medicine lack good science, there are now abundant research works in herbal and natural medicine available locally and on the international scene. 350 reviewed documents have been identified by internet search engines as credible references. Since herbal medicine constitutes the largest aspect of traditional medicine, some compilations have been made on herbal medicines in the form of handbooks and 1 publications, whilst others are in the form of data-bases that have been networked to registered experts. The challenge to us in Africa and for that matter Ghana is to begin to compile this knowledge and scientific research works into books, compendia, and pharmacopoeia and on electronic data-bases. Attempts that have been made in Ghana include the following publications: Publication Woody Plants of Ghana Useful Plants of Ghana Ghana Herbal Pharmacopoeia, Edn. 1 Floristic Studies in Ghana and Pharmacopoeia Ghana Herbal Pharmacopoeia (Revised) African Herbal Pharmacopoeia WHO Monographs on 26 Selected Medicinal plants Vol.1 WHO monographs on 30 Selected Medicinal Plants Vol. 2 Author Irvine Abbiw Consortium Content Botanical/ethno medical Botanical/ethno-medical Botanical/ethno-medical Year 1961 1990 1995 CSIR Botanical/ethno-medical 2001 CSIR Phytochemical/pharmacological 2007 AU WHO-HQ Ethno-Medical/Botanical Scientific Information 1996 1996 WHO-HQ Scientific Information 2002 What Are Monographs? Monographs can be said to be a summary of scientific information on a single topic in medical science targeted towards informing medical professionals. These are usually compiled into encyclopedias, Medical Dictionaries, compendia of global repute and data-bases that are reviewed by experts. In the case of pharmaco-therapeutic chemicals and medicines, the monographs are compiled into pharmacopoeias and their presentation must necessarily include a description of the substance, in terms of physical and chemical properties, its identity and purity tests and methods for its derivation, standardization and use. The contents of monographs are usually presented in standardized or stereotyped formats. The profile of information included in monographs depends on their targeted usage. 2 Pharmacopoeia monographs usually focuses on standards specifications for evaluating the raw material and assay of the material from products derived from it. In Pharmacopoeia Monographs, experimental pharmacology, clinical data and information on medicinal products and formulations, spectral information are considered as additional information to standards or described as Extrapharmacopoeia, Schedules and Annexes. The Scope and Value of Pharmacopoeia Monographs The standards in pharmacopoeias are targeted to inform manufacturers, bulk purchasers, drug regulators, standards specifications authorities, freight inspectors, and health professionals. Pharmacological and clinical information are however targeted to inform healthcare providers, medicine researchers and drug regulators. In other words, they are relevant for ensuring quality of raw material substances used in manufacture of medicines as well as the quality of manufactured products emanating from them. However pharmacopoeial monographs in themselves cannot produce quality assurance since they do not usually provide extra information on how the standards specified can be achieved. This would remain the experience of individual manufactures, technical experts and researchers. This is why manufacturer’s information and specifications are also as important. Monographs also are limited to cover the most essential or commonly used substances. For this reason, Limit tests for presence of micro-organisms, Pharmcokinetics and Bio-equivalence studies, have become part of WHO pre-qualification requirements and requirements of some standards authorities for approval of imports and manufacture of special medicines for programmed diseases of public health importance. These do not usually form part of pharmacopoeial standards and would remain the experience of specific reference laboratories and standards authorities. Typical Format of Monographs Including Monographs on Medicinal Plants Monographs on medicinal plants present peculiar challenges. There is the need to provide both the botanical description as well as the chemical characterization of the medicinal plants. Methods for standardization and bio-assays must necessarily be included. Below is a format for presenting Pharmacopoeial monographs of pure chemical compounds as compared to the format for presenting WHO and other Monographs on Medicinal Plants. 3 A Typical Monograph of Pure chemicals From Beckett and Stenlake Practical Pharmaceutical Chemistry Title (Approved name and Adopted Name) Structural Formula Molecular Formula and Weight Definition Standard of Purity Physical characteristics Test For Verification and Identity (Including Absorbance) Limit Tests for Contaminants Physical Constants (e.g. Solubility, optical rotation and PH of a standard solution) Quantitative Evaluation of Purity Storage Conditions Labeling Conditions Regulatory Requirements Cautionary Notices A Typical Herbal Pharmacopoeial Monograph A Common Format for Monographs of Official Drug Preparations and Substances (e.g.Tabs, Caps): from Ajibola A. Olaniyi Principles of Drug Quality Assurance and Pharmaceutical Analysis Main Name Other Names Chemical Name, graphic and Molecular Formula Method of derivation and Purity Tests Physical and Chemical Description Solubility Profile in common solvents Identification ( By Scientific tests) Dissolution Rate (especially for tablets and capsules) Uniformity of Content Methods of Assay of Strength Storage and Labeling Requirements Actions and Uses Usual Dose Ranges Dose-forms and Strengths Available WHO Monographs on Medicinal Plants Structure Based on Nigerian Herbal Pharmacopoeia 1. Title based on Approved International name or taxonomy 2. Common Name 3. Local Names 4. Geographical Distribution 5. General Description of Plant 6. Ethno-medical Uses 7. Morphological parts Used as Drug and Definition 8. Description of Drug by Macroscopy 9. Description of drug by Microscopy 10. Chemical and bio-activity Profile 11. Test for Identity and Purity 12. Chromatographic Finger Printing as a And Ghana’s Herbal Pharmacopoeia, 2007 1. Title by Approved Botanical Name 2. 3. 4. 5. 6. 7. Definition Synonym Selected Vemacular Names Geographical Distribution Description Part of Plant Material of Interest 8. Organoleptic Properties 9. Microscopic characteristics 10. Powdered Plant Material 11. General Identity Tests 12. Purity tests 4 quick standard assessment but other separation techniques may be uses e.g. TLC, HPLC 13. Chemical Tests and Assays 14. Indications and Dosage 15. Contraindications/Adverse Effects/Precautions 16. Storage conditions 17 Posology 18 References 13. Chemical Assay including absorbance 14. 11. Major chemical Constituents 15. 12. Medicinal Uses (Clinical, Ethno medical, experimental) 16. 13. Pharmacology(Experimental, Microbiology, Toxicological and Clinical) 17. Contraindications/adverse reactions 18. Dosage Forms 19. Posology 20. references Whilst the Nigerian Herbal Pharmacopoeia, like a typical pharmacopoeia monographs, focus on description, standards specifications and associated formularies, the Ghana Herbal Pharmacopoeia was formatted along the style of the WHO monographs which essentially composes of summaries of general scientific information, pharmacological and clinical information emanating from research and development and use of the product. The Objectives of the Monographs on Medicinal Plants The current monographs on medicinal plants are therefore not pharmacopoeia monographs and do not therefore emphasize on botanical descriptions, chemical assays and standards of raw materials. However, elaborate references have been given to other documents. Standards would be the emphases of the new West African Herbal Pharmacopeia which is being developed by WAHO- the West African Health Organization as common standard specifications for West African medicinal plants. The emphasis of this current herbal monograph is to inform users of the Recommended List of Herbal Medicines for Primary Healthcare, which was launched along side the monographs, about pharmacological information, clinical data and expected adverse effects, proposed dose ranges and the related selected herbal products. Although the scientific information is on individual medicinal plants composing the list of products, it generally predicts the performance and expected side effects of the combination products which have 5 been judged by the Food and Drugs Board to be stable and safe to use. The information is to guide the proposed pilot official use of approved herbal medicines in public hospital facilities and selected private herbal clinic facilities which may be accredited to operate under the National Health Insurance Scheme. The proposal is currently receiving the highest consideration by the Health Sector and would be soon outdoored. The Role of Pharmacists The Medical Herbalists is a health professional or cadre, who has undertaken a four-year clinical programme in herbal medicine. They are expected to work under supervision as equivalent to Physician Assistants, to provide herbal medicine treatment services. Medical Doctors who have been oriented in herbal medicine would supervise this new carrier pathway. The Director General of Ghana Health Service (GHS) has directed that herbal medicine services may be established as separate units within GHS facilities. However, in order to separate the diagnosis and management functions from dispensing, the hospital pharmacy and community pharmacies, should be sufficiently prepared to produce, procure, store and dispense herbal medicines. The pharmacy should also serve as information resource for herbal medicines. The Monographs on herbal medicines and the Recommended Formulary of herbal medicines, together with the Ghana Herbal Pharmacopoeia, The Food and Drugs Board Drug Register and other databases, would be an invaluable resource to the success of this programme for the official inclusion of herbal medicines in healthcare delivery and the National Health Insurance Scheme. Pharmacists in the selected centres, which would be dedicated as pilots, may contact the National Drug Information Centre, The Chief Pharmacist, the Pharmacy Council Offices or the Pharmaceutical Society Office, for further information and to procure copies of the Monographs and Herbal Formulary. The Traditional and Alternative Medicine Directorate of the Ministry of Health would stand-by to support this process. Conclusion It would be useful to re-state that herbal medicine practice that would be mainstreamed into healthcare would and should be backed by good science. The 6 WHO since the year 2002 has been pursuing a strategy towards institutionalizing procedures for the safety, efficacy, access and rational use of herbal medicines under structured regulatory, legislative and administrative frameworks. The Ministry of Health is at the verge of piloting the establishment of herbal medicine units in both selected accredited herbal and public health clinics and hospitals. To this end all efforts are being made to obtain a network of information on herbal medicine research in country and from data-bases in other countries in order to continually update the system. Let us discuss what would make such a health system continually functional and how it can help curb other excesses in herbal medicine practice, at the next publication of this journal. Attached is a monograph on Cassia alata from the Monographs on Medicinal Plants that was launched, for the perusal of the reader. Cassia alata Botanical name Cassia alata Local name(s) Osempe; Duawusu (Twi); asenti (Ga-Adangbe); agbobladzoe (Ewe) Chemical constituents Anthraquinones, flavonoid, glycosides; essential fatty acids, protein; minerals (e.g. calcium, magnesium, sodium, manganese and zinc) ((Yadav and Kalidhar 1994; Mora et al 1991; Ukhun and Ifebigh 1988; Gupta and Singh 1991)). Suggested method of standardisation As indicated earlier by Nyarko et al in the Harmonized Procedures for Assessing the Safety, Efficacy and Quality of Plant Medicines in Ghana and from other pharmacopoeal monographs. Pharmacology Experimental pharmacology Hexane fractions of C. alata caused a marked cytotoxic effect on breast cancer, urinary bladder cancer and colon cancer cell lines in a dose dependent manner (Olarte et al 2006). An extract of the leaves of C. alata and kaempferol 3-0-sophoroside, a polyphenolic constituent of the plant, exhibited significant analgesic effect in vivo (Palanichamy 1988; Palanichamy and Nagarajan 1990). Palanichamy et al (1988) also studied the anti-diabetic effect of the leaf extract in streptozotocininduced hyperglycemic rats and obtained results comparable to that of glibenclamide. The extract had no effect on glucose levels in normoglycemic animals. The leaf extract also showed antifungal activity in 7 vitro (Palanichamy and Nagarajan, 1990), probably due to the presence of chrysophanol (Chopra et al 1956). Antibacterial activity of the crude extracts of C. alata has been demonstrated in-vitro (Limsong et al 2004). Crude ethanol and water extract of leaves and barks from C. alata possessed anti-candida activity. Results were comparable to standard antifungal drug (Somchit et al 2003). A 10-year human study indicates that the leaf extract can be used to treat Pityriasis versicolor with no side-effects (Damodaran and Venkataraman 1994). The methanol extracts of leaves, flowers, stem and root barks of Cassia alata showed a broad spectrum of antibacterial activity (Khan et al 2001). Ethanolic leaf extract exhibited high activity against various species of derrnatophytic fungi but low activity against nondermatophytic fungi. Bacterial and yeast species, however, showed resistance against in vitro treatment with the extract (Ibrahim and Osman 1995). Topical administration of ointments made with ethanolic extracts of leaves of Senna alata, Lantana camara and Mitracarpus scaber on chronic crusty or acute lesions of dermatophilosis, induces healing of the disease infected animals treated without recurrence (Ali-Emmanuel et al 2003). Leaves of C. podocarpa Guill. and Perr. and of senna had identical laxative potency (Elujoba et al 1989). Medicinal uses Traditional system/folk medicine Treatment of skin diseases (e.g. ringworm, eczema, chronic pruritis, itching); constipation; bronchitis and asthma; liver diseases and gastrointestinal problems snake-bite; scorpion-sting; leprosy; wounds (Chopra et al 1956; Kirtikar and Basu 1975; Dey and Bahadur 1973; Dey and Bahadur 1973; Perry 1980) and in (Bokemo 1984; Ibrahim and Osman 1995; Palanichamy and Nagarajan 1990; Khan et al 2001). Uses as described in pharmacopoeia Abortifacient; antibacterial; antifungal; choleretic; digestive; diuretic; febrifuge; hypoglycaemic; insect repellent; insecticidal; laxative; purgative; vermifuge (Assane, 1993; (GHP, 1992); for the treatment of ascites; constipation; craw-craw, dermatitis; dhobey-itch; dystocia; eczema; gonorrhoea; leprosy; mycosis; parturition; ringworm; shingles; stomach ache; tattoo; tinea (Mshana et al 2000; GHP 1992). Uses supported by experimental or clinical data Antidiabetic; antifungal; antibacterial; analgesic; laxative Precautions and toxicology Seeds of C. pordocarpa are claimed to produce toxic symptoms by ingestion unless it is steam fried. (GHAFTRAM sources-Ghana ). Toxicity is suspected to result from a toxoalbumin cell content which is denatured by heat. (WAHO Presentation)). Short-term (upto 6-8 weeks) external application is preferred. Other uses are to be supported by expert advice, in small doses and for short periods. Toxicity in animals is exhibited by loss of appetite and ematiation (Sodipo et al. Nigeria). Contraindications Pregnancy and lactation; intestinal obstruction; inflammatory bowel disorders; idiopathic abdominal pains; haemorrhoids; colitis; ulcer. 8 Adverse effects Long-term use may cause electrolyte loss and pigmentation of the intestinal mucosa. Extracts may cause nausea and vomiting in large doses. Dosage form Tincture; infusion (tea); decoction Posology or recommended dose Infusion (hot or cold): the dried pods or leaves should be steeped in warm water for 6-12 hours; 1 tsp in ca. 150 ml of water; filter after 10 minutes; drink one cup in the morning and/or before going to the bed (BHC, 1992) Powder: 1-2 g in 150 ml of water (as purgative) Tincture: 1:5 in 50% alcohol; take 2-4 ml before bedtime (http://holistic-online.com/HerbalMed/_Herbs/ h205.htm). References 1. Ali-Emmanuel N, Moudachirou M, Akakpoc JA, Quetin-Leclercq J (2003). Treatment of bovine dermatophilosis with Senna alata, Lantana camara and Mitracarpus scaber leaf extracts. Journal of Ethnopharmacology 86 (2003) 167–171 2. Assane M, (1993) Choleretic effects of Cassia alata Linn in the rat. Dakar Med.; 38(1): 73-77 3. Bokemo W (1984). Les plantes antilepreuses de Kisangani, Haut Zaire. Bulletin Royal Society Belgium 117, 305-311. 4. Bradley PR, ed. (1992). British Herbal Compendium. Bournemouth (UK): British Herbal Medicine Association; 1, 199. 5. Chopra RN, Nayar SL and Chopra IC (1956). Glossary of Indian Medicinal Plants. Council of Scientific and Industrial Research, New Delhi, p. 54. 6. Damodaran S, Venkataraman S (1994). A study on the therapeutic efficacy of Cassia alata, Linn. leaf extract against Pityriasis versicolor. Journal of Ethnopharmacology 42, 19-23. 7. Dey KL, Bahadur R (1973) The Indigenous Drugs of India, 2nd Edn. Pama Primlane Publishers, New Delhi, 70. 8. Elujoba AA, Ajulo OO, Iweibo GO (1989). Chemical and biological analyses of Nigerian Cassia species for laxative activity. Journal of Pharmaceutical and Biomedical Analysis, 7(12): 14531457. 9. Ghana Herbal Pharmacopoeia (1992). The Advent Press: Accra, Ghana; 4-6 10. Gupta D, Singh J (1991). Flavonoid glycosides from Cassia alata. Phytochemistry 30:2761-2763. 11. http://holistic-online.com/Herbal-Med/_Herbs/ h205.htm. 12. Ibrahim D, Osman H (1995). Antirnicrobial activity of Cassia alata from Malaysia. Journal of Ethnopharmacology 45, 151-156 13. Khan MR, Kihara M, Omoloso AD (2001). Antimicrobial activity of Cassia alata. Fitoterapia 72, 561-564. 14. Kirtikar KR, Basu BD (1975) Indian Medicinal Plants Vol. II, 2nd Edn. Jayyed Press, Delhi, pp. 870 872. 15. Limsong J, Benjavongkulchai E, Kuvatanasuchati J (2004). Inhibitory effect of some herbal extracts on adherence of Streptococcus mutans. Journal of Ethnopharmacology 92, 281–289 16. Morah FNI, Otumu HE (1991). Cassia alata seeds constituents. Jamaican Journal of Sciences and Technology 2, 14-16. 9 17. Mshana, N.R., Abbiw, D.K., Addae-Mensah, I., Ahiyi, M.R.A. et al., (2000). Traditional medicine and pharmacopoeia. Contribution to the revision of Ethnobotanical and Floristics Studies of Ghana. Organisation of African Unity/Scientific, technical and research committee. 18. Ogunti EO, Elujoba AA (1993). Laxative activity of Cassia alata. Fitoterapia 64, 437-439. 19. Olarte EI, Herrera AA, Villasenor IM, Jacinto SD (2006). Selective cytotoxicity of an isolate from Cassia alata L. leaves. Poster Abstracts - Experimental Therapy. Cancer Prevention 59. 20. Palanichamy S, Nagarajan S (1990). Analgesic activity of Cassia alata leaf extract and kaemperol 3-O-sophoroside. Journal of Ethnopharmacology 29, 73-78 21. Palanichamy S and Nagarajan S (1990). Antifungal activity of Cassia alata leaf extract. Journal of Ethnopharmacology 29, 337-340. 22. Palanichamy S, Bhaskar EA, Bakthavathsalam R, Nagarajan S (1991). Wound healing activity of Cassia alata. Fitoterapia 62, 153-156. 23. Palanichamy S, Nagarajan S, Devasagayam M (1988). Effect of Cassia alata leaf extract on hyperglycemic rats. Journal of Ethnopharmacology 22, 81-90. 24. Palanichamy S (1988). Cassia alata: A Study of its Pharrnacognosy. Phytochemistry, Pharmacology and Formulation. Ph.D. Thesis, Bharathidasan University Tiruchirapalli, India. 25. Perry LM (1980). Medicinal plants of East and Southeast Asia: attributed properties and uses. Cambridge, Massachusetts and London: The MIT Press, 209. 26. Yadav SK, Kalidhar SB (1994). Alquinone: An Anthraquinone from Cassia alata. Planta Medica 60(6): 601. 27. Somchit MN, Reezal I, Nur IE, Mutalib AR (2003). In vitro antimicrobial activity of ethanol and water extracts of Cassia alata. Journal of Ethnopharmacology 84, 1-4. 28. Ukhun ME, Ifebigh EO (1988). Compositional Chemistry of Cassia alata Seeds. Food Chemistry 30, 205-210. Foot notes: Some Combination Products 1. 2. 3. 4. Ako Herbal Tonic Hayaat Tonic Odo Pee Ointment Chocho Cream 5. 6. 7. 8. Joy Ointment Nobi Cream Megyefo Cream Mayah Herbal Soap 10 Table of Contents FOREWORD…………………………………………………………………………………………………………1 2 PREFACE………………………………………………………………………………………………………….ER ROR! BOOKMARK NOT DEFINED. ACKNOWLEDGEMENTS…………………………………………………………………………….…………..E RROR! BOOKMARK NOT DEFINED. A HANDBOOK FOR THE MEDICAL HERBALIST AND NEW HEALTH WORKERS…………………..ERROR! BOOKMARK NOT DEFINED. APPENDIX TO THE HANDBOOK………………………………………………………………………………Error! Bookmark not defined. Classification of Medicinal Plants in a Herbal Fomulation…………………………………………….………….Error! Bookmark not defined. MONOGRAPHS ON SELECTED COMMONLY USED MEDICINAL PLANTS……………..……………...ERROR! BOOKMARK NOT DEFINED. Monograph of Plants used as Circulatory Tonics, Anaemia…………………………………….…….Error! Bookmark not defined. - 67 Monograph of Medicinal Plants Used in the Treatment of Unspecific Diarrhoea (unless stated)….68 - 78 Monographs of Medicinal Plants in formulations supposedly used to expel intestinal worms (Helminthiasis) 14 Monographs on Medicinal Plants Used for Elevated Blood Pressure and Associated Symptoms ................................................... 63 Monographs on Medicinal Plants for Malaria and Febrile Illnesses ................................................................................................ 82 Monographs on Medicinal Plants Used for Pain and Arthritis ............................................................. Error! Bookmark not defined. Monographs on Medicinal Plants Used As Laxatives and for Relieve of Piles/Haemmorrhoids ................................................... 106 Monographs on Medicinal Plants Used for Skin Diseases .............................................................................................................. 114 Monographs on Medicinal Plants Selected for Gastritis, Peptic Ulcers ................................................ Error! Bookmark not defined. Monographs on Medicinal Plants Selected for Enteric/Typhoid Fever.......................................................................................... 127 Monographs on Medicinal Plants for Miscellaneous Conditions of Public Health Importance .................................................... 136 INDEX OF BOTANICAL AND LOCAL NAMES OF MEDICINAL PLANTS ........................................................................ 146 11 Foreword The herbal medicine industry is both old and new. Herbal Medicinal products and other naturally occurring substances have been in use as medicines since the dawn of creation. Documented evidence dates back 5000 BC. Until the rapid discovery of synthetic and semi-synthetic means of developing medicines at the turn of the 18th Century (1850 to 1950) and especially in the last eighty or so years (1935-2005), herbal and natural substances were the only forms of medication. During this period of recess in the use of herbal medicines, a lot of research and development work has taken place on natural and herbal medicines, both locally and abroad since they provided leads to the synthesis of chemical analogues. New findings in research and treatment of diseases have led to a resurgence of interest in the herbal medicine industry. This growth in the herbal medicine industry which is worldwide has generated heightened awareness about safety, efficacy issues and the need for regulations to ensure quality. The growth has been sustained by several other factors, particular, awareness by some consumers and health care professionals about the high levels of chemicals in the environment and thereby promoting natural and organic foods and medicines. Education and control measures by the media and regulatory authorities respectively, in many countries have also contributed to the popular use of herbal and natural medicines. It is imperative therefore, that, in the light of this interest, that the production of herbal medicines is guided by quality assurance procedures which ensure that production is based on proper manufacturing practices (GMP), and that services are provided under controlled environment(s). It is against this background and in line with the National Drug Policy and the Legislative Instruments (LI-1809) of the National Health Insurance Scheme and other health legislations which recognizes the use of herbal medicines, that the Ministry of Health tasked a team of experts to compile a list of recommended herbal formulations with proven safety and efficacy, to constitute Ghana’s Essential Herbal Medicines List. Although the list of herbal medicines given market authorization by the Food and Drugs Board was available, the Recommended Herbal Medicines List focuses on herbal medicines intended for treatment of diseases of priority public health importance. It is also intended to initiate rational prescribing of herbal medicines as a way of regulating unbridled access to herbal medicines for self-medication, and enhance the protocol of options in medical care, whilst ensuring cost-effectiveness in the use of this available health resource. An herbal formulary can be an effective tool for setting and measuring standards of best practices and ensuring rational physiotherapy. For effective use of the formulary of Recommended Herbal Medicines, monographs, which define the physiochemical composition, pre-clinical tests results, standardization procedures, pharmacologic and therapeutic information, must be made available. Monographs have been the form in which concise scientific information on medicines is presented to health professionals. The monographs presented here which are intended to serve this purpose were fashioned after the WHO Monographs on herbal medicines. However, they do not represent the full pharmacopoeia monographs on herbal medicines. Detailed ethno-botanical and organoleptic descriptions which were deliberately omitted can be obtained from other references such as the Floristic Studies in Ghana and The Ghana Herbal pharmacopoeia. There are altogether profiles on 250 Ghanaian medicinal plants which have been used in the formulation of the recommended herbal medicines. These medicinal plants have long-term folklore use, and have been subjected to laboratory investigations in the country as well as in other research institutions outside the country. Each monograph provides information about key chemical compounds, pharmacological actions, folkloric uses, toxicology, adverse effects, contraindications, dosage forms and recommended dosages. Detailed references are also given to support the scientific information and for further search. Interestingly, whereas there is the existence of a plethora of publications on laboratory studies on African medicinal plants, information on properly designed clinical trials and documented evidence on the use of combination herbal products, remain scanty. The challenge therefore is for Traditional Medicine Practitioners, Doctors and Research Scientists to pull their resources 12 together to fill this need gap, in our bid to promote quality of Traditional Medicine products and services and to make them safer to use as our contribution to human health. It is hoped that these monographs will not only serve as a compendium or reference source of information to the Recommended Herbal Medicines List for Herbal Medicine Practitioners, Doctors, Pharmacists, Research Scientists, Nurses and Students. It will also be expected to stimulate further research, larger-scale local production and investment into the further development of herbal and natural medicines. Acknowledgements The invaluable contributions of the following personalities, who served as chairpersons for the technical committee, committee of experts, task team on selection of herbal medicines, and the editorial task team respectively, are hereby acknowledged. Without their leadership and motivation, this task which started from February 2005, could not have been completed due to the many complex turns that the process had to take. The personalities are; Professor David Ofori-Adjei, Consultant, NOGUCHI/GNDP Professor A. C. Sackeyfio – Dean, UGMS-Pharmacy/NDIRC Dr. E. N. Mensah – Health Consultant/Former DG/GHS Professor L.N.K. Okine – Director, CSRPM/UG-Legon Professor A. K. Nyarko – Director. NOGUCHI MIMR-UG Dr. I. J. Asiedu-Gyekye – Dept. of Pharmacology, UGMS. The contributions of the following institutions are also acknowledged. The Ghana Federation of Traditional Medicine Associations The Department of Herbal Medicine – KNUST, Kumasi The Food and Drugs Board, Accra The Ghana National Drug Programme – MOH, Accra The WHO-Headquarters, TRM Department The WHO-AFRO The WHO-Ghana Office The Ghana Health Service WAHO and ECOWAS Headquarters The availability of successive Director Generals for Ghana Health Service and their team of Directors at the headquarters, Accra and in the Regions, in making their views, suggestions and questions available, are highly commended, as they provided direction in choosing suitable options for the presentation of these documents. Above all, the Minister of Health, Major Courage Quashigah deserves special honoour for providing the initiative, impetus, and for approving financial support and sustaining leadership for the process of underking this work. The support of the management of the Ministry of Health was equally visible and full of understanding considerations. This document consists of a short handbook as an introduction to the health sector and how herbal medicines work, the Scientific Monographs on the selected medicinel plants, The List of Recommended Herbal Medicinal Products and the Appendices. The monographs were written by the singular effort of Dr. Kofi Busia, the professional officer for traditional medicine at the West African Health Organization Headquarters, Bobo-Dioulasso, Burkina Faso. The editorial team consisited of Professor Alexander Nyarko (NOGUCHI), Prof. LNK Okine (CSRPM), Mr. Patrick Anum (NDIRC), Mrs Martha Ghansah Lutterodt (GNDP), Mrs Edith Annan (WHO), Mr. Abu Sumaila (FDB) and Mr. Peter Arhin (TAMD-MOH) The work could however, not have been completed without the continual financial support of WHO-AFRO and the interest that the WHO-Ghana Office took in all the various stages of the preparation of this document. A comprehensive list of individual contributors and those who represented institutions and people contacted have been provided in the Appendices. This document is therefore dedicated to all those individuals whose distinguished contributions led to the completion of this work. 13 Peter Arhin Director, Traditional and Alternative Medicine Directorate Ministry of Health, Accra ________________________________________________ Monographs of Medicinal Plants in formulations supposedly used to expel intestinal worms (Helminthiasis) 1. Allium sativum 2. Alstonia boonei 3. Carica papaya 4. Cassia occidentalis 5. Khaya senegalensis 6. Mitragyna inermis 7. Ricinus communis _______________________ Allium sativum Botanical name Allium sativum Local name(s) Gyene kankan (Twi); samanatsopa (Ga-Adangbe); tafamuwa (Hausa) Chemical constituents Organo-sulphur compounds (s-allyl cysteine, allicin, diallyl sulphide, diallyl disulphide and others); lectins, prostaglandins, fructan, pectin, adenosine, vitamins B1, B2, B6, C and E, biotin, nicotinic acid, fatty acids, glycolipids, phospholipids and essential amino acids; steroid saponins (β-chlorogenin); allixin and organo-selenium compounds (Corzo-Martínez et al 2007; Lanzotti 2006; Fenwick and Hanley 1985; Lancaster and Shaw 1989; Augusti and Mathew 1974). Pharmacology Several garlic compounds including allicin and its corresponding sulfide inhibit the proliferation and induce apoptosis of several human non-leukaemia malignant cells including breast, bladder, colorectal, hepatic, prostate cancer, and lymphoma and skin tumour cell lines. Several clinical trials and in vitro studies of ajoene have demonstrated its best-known anti-thrombosis, anti-microbial and cholesterol lowering activities. Topical application of ajoene produced significant clinical response in patients with skin basal cell carcinoma (Hassan 2004). Garlic oil, powder and constituents were shown to exert potent antibacterial effect on Helicobacter pylori (O’Gara et al 2000) that may explain epidemiological evidence for protection against gastric cancer (You et al 1998; 14 Takezaki et al 1999). Also, garlic was shown to stimulate immune effector cells including T- and natural killer cells that may explain its therapeutic effect in bladder cancer (Lamm and Riggs 2000). Moreover, numerous epidemiological, clinical and laboratory studies have demonstrated the role of garlic in cancer prevention (Milner 2001; Fleischauer and Arab 2001; Bianchini and Vainio 2001; Dorant et al 1996). These studies have demonstrated the chemopreventive activity of garlic by using different garlic preparations including fresh garlic extract, aged garlic, garlic oil and a number of organosulphur compounds derived from garlic Milner 2001; Fleischauer and Arab 2001; Bianchini and Vainio 2001). The chemopreventive activity has been attributed to the presence of organosulphur compounds in garlic that modulate the activity of several metabolising enzymes that activate (cytochrome P450s) or detoxify (glutathione S-transferases) carcinogens and inhibit the formation of DNA adducts in several target tissues (Milner 2001; Fleischauer and Arab 2001; Bianchini and Vainio 2001). Diallyl disulfide has been known to exert potent chemopreventative activity against colon, lung, and skin cancers (Kwon et al (2002). Garlic’s anti-arteriosclerotic properties have been demonstrated in in a randomized, double-blind, placebocontrolled clinical trial (Koscielny et al (1999). Garlic causes reduction in blood pressure (Al-Qattan et al 2003). Ajoene exerts potent inhibitory effects on platelet activation (Apitz-Castro et al 1986), platelet binding to damaged blood vessel wall (Apitz-Castro et al 1994) and thrombus formation (Apitz-Castro et al 1992). Also, ajoene prevented platelet loss from the blood (Apitz-Castro et al 1991), inhibited the lipooxygenase pathway and tyrosine phosphatase activity in human platelets (Srivastava and Tyagi 1993) and lowered cholesterol biosynthesis (Gebhardt et al 1994). Garlic oil produced a marked reversal of the metabolic changes associated with isoproterenol-induced myocardial infarction (Saravanan and Prakash 2004). Several animal studies using garlic essential oil and raw garlic have shown that garlic consumption decreases significantly the content of total serum cholesterol (Chang and Johnson 1980), low density lipoproteins and very low density lipoproteins. It also increases significantly the level of high density lipoproteins. In another study with cholesterol-fed rabbits, it was shown that garlic extract reduces vessel wall cholesterol accumulation and arteriosclerotic plaques development in arterial wall (Effendy et al 1997). Several clinical reports and meta-analyses have revealed the cholesterol-lowering effects of raw garlic and some garlic supplements (Lau et al 1987; Neil et al 1996). Aqueous and organic garlic extracts were also able to inhibit platelet aggregation in vivo (Mohammad and Woodward1986). Ajoene exhibited anti-mycotic effect in the treatment of tinea corporis and tinea cruris (Ledezma et al 1999) and exerted anti-microbial and anti-viral activities (Naganawa et al 1996; Walder et al 1997). Garlic extract showed high inhibitory activity against a range of pathogenic bacteria and fungus (Benkeblia 2004). In vitro and in vivo studies have shown garlic’s effectiveness against a broad spectrum of fungi and yeasts, including (Davis and Perrie 2003), as well as a synergistic activity with amphotericin B in vitro (Shen et al 1996). The antiviral activities of various commercial garlic products, against herpes simplex virus Types 1 and 2, influenza A and B viruses (Fenwick and Hanley 1985), human cytomegalovirus (Meng et al 1993), vesicular stomatitis virus, rhinovirus, human immunodeficiency virus (HIV), viral pneumonia and rotavirus, have been extensively investigated. Pharmacodynamics Several investigations have allowed the determination of the mechanism by which garlic exerts its antihypertensive action. Some studies of garlic effect on muscular contraction in vitro have concluded that its hypotensive action may be, at least partly, due to a direct relaxant effect on smooth muscles (Aqel et al 1991). On the other hand, other studies have suggested that garlic may also exert an indirect vasodilator effect, inducing the nitric oxide and hydrogen sulphide synthesis, both potent vasodilators. Medicinal uses Traditional system/folk medicine None available 15 Uses as described in pharmacopoeia Atherosclerosis; diabetes; diarrhoea; dysentery; earaches; gout; headache; hypertension; leprosy; rheumatism; snakebites; symptoms of upper respiratory tract infections; tuberculosis and gangrene of the lung; (Barnes et al 2002; WHO 1999; Rahman 2001; Watt and Breyer-Brandwijk 1962). Uses supported by experimental or clinical data Hypocholesterolemic, hypolipidemic, anti-hypertensive, anti-diabetic, antithrombotic and anti-hyperhomocysteinemia effects, antimicrobial, antioxidant, anticarcinogenic, antimutagenic, antiasthmatic, immunomodulatory; antifungal, antibacterial, antitumor, anti-inflammatory (Corzo-Martínez et al 2007; Lanzotti 2006; Agarwal 1996). Precautions and toxicology Consumption of excessive amounts of garlic, especially on an empty stomach, can cause gastrointestinal upsets (burning sensation and diarrhoea), flatulence and changes in the intestinal flora (Ackermann et al., 2001). Contraindications Patients on certain anti-clotting medications, e.g. warfarin (Ackermann et al 2001); Several recent studies have reported that concurrent intake of onion, with high quercetin content, markedly decreases the oral bioavailability of cyclosporin, with subsequent organ transplant rejection (Yang et al 2006). Adverse effects Unpleasant breath and body odour Dermatological problems in susceptible individuals (allergic dermatitis, burns and blisters) (Davis 2005; Friedman et al 2006) Asthmatic effects, in workers exposed to garlic powder in garlic growing or industrial processing (Lybarger et al 1982) Dosage form Intact bulb; Decoction, tincture, tablets, capsules Posology or recommended dose Fresh: 2-5g/day Oil from bulb: 2-5mg/day Powder: 400-1200mg/day; other preparations: corresponding to 2-5 mg allicin (Bradley 1992). Tincture: 1:5 in 60% alcohol, 5 ml three times a day References Ackermann RT, Mulrow CD, Ramirez G, Gardner CD et al (2001). Garlic shows promise for improving some cardiovascular risk factors. Archives of Internal Medicine 161, 813-824. Agarwal KC (1996). Therapeutic actions of garlic constituents. Med Res Rev; 16:111. Al-Qattan KK, Khan I, Alnaqeeb MA, Ali M et al (2003). Mechanism of garlic (Allium sativum) induced reduction of 3. hypertension in 2K-1C rats: a possible mediation of Na/H exchanger isoform-1. Prostaglandins, Leukotrienes and Essential Fatty Acids 69, 217–222. Apitz-Castro R, Escalante J, Vagase R, Jain MK (1986). Ajoene, the antiplatelet principle of garlic, synergistically potentiates the antiaggregatory action of prostacyclin. Thromb Res 42, 303.Apitz-Castro R, Badimon JJ, Badimon L (1994). A garlic derivative, ajoene, inhibits platelet deposition on severely damaged vessel wall in an in vitro porcine experimental model. Thromb Res 75, 243. Apitz-Castro R, Badimon JJ, Badimon L. Effect of ajoene, the major antiplatelet compound from garlic, on platelet thrombus formation. Thromb Res 1992;68:145. 16 Apitz-Castro R, Jain MK, Bartolli F, Ledezma E et al (1991). Evidence for direct coupling of primary agonist–receptor interaction to the exposure of functional IIb–IIIa complexes in human blood platelets. Results from studies with the anti-platelet compound ajoene. Biochim Biophys Acta 1094, 269. Aqel MB, Gharaibah MN, Salva AS (1991). Direct relaxant effects of garlic juice on smooth and cardiac muscles. Journal Ethnopharmacology 33, 13-19. Barnes J, Anderson LA, Phillipson JD (2002) Herbal Medicines: A guide for healthcare professionals. 2nd ed. London (UK): Pharmaceutical Press. Benkeblia N (2004). Antimicrobial activity of essential oil extracts of various onions (Allium cepa) and garlic (Allium sativum). Lebensm.-Wiss.u.-Technol. 37, 263-268 Bianchini F, Vainio H (2001). Allium vegetables and organosulfur compounds: do they help prevent cancer? Environ Health Perspect, 109(9): 893 Chang MLW, Johnson MA (1980). Effect of garlic on lipid metabolism and lipid synthesis in rats. The Journal of Nutrition, 110, 931-936. Corzo-Martínez M, Corzo N, Villamiel M (2007). Biological properties of onions and garlic. Trends in Food Science & Technology 18, 609-625. Davis SR, Perrie R (2003). The in-vitro susceptibility of Cryptococcus neoformans to allitridium. In Program and Abstracts of the 15th Congress of ISHAM (abstract 113). San Antonio, TX, USA, May 25-29, 2003. Davis SR (2005). An overview on the antifungal properties of allicin and its breakdown products exhibited the possibility of safe and effective antifungal properties. Mycoses 48(2), 95-100. Dorant E, van den Brandt PA, Goldbohm RA, Sturmans F (1996). Consumption of onions and a reduced risk of stomach carcinoma. Gastroenterology 110, 12. Effendy JL, Simmons DL, Campbell GR, Campbell JH (1997). The effect of aged garlic extract ‘‘Kyolic’’, on the development of experimental atherosclerosis. Atherosclerosis 132, 37-42. Fenwick GR, Hanley AB (1985). The genus Allium. CRC Critical Reviews in Food Science and Nutrition 22, 199-377. Fleischauer AT, Arab L (2001). Garlic and cancer: a critical review of the epidemiologic literature. Journal of Nutrition 131(3):1032S. Friedman T, Shalom A, Westreich M (2006). Self-inflicted garlic burns: our experience and literature review. International Journal of Dermatology 45(10), 1161-1163. Gebhardt R, Beck H, Wagner KG (1994). Inhibition of cholesterol biosynthesis by allicin and ajoene in rat hepatocytes and HepG2 cells. Biochim Biophys Acta 1213, 57. Hassan HT (2004). Ajoene (natural garlic compound): a new anti-leukaemia agent for AML therapy. Leukemia Research 28, 667-671. Koscielny J, Klüßendorf D, Latza R, Schmitt R et al (1999). The antiatherosclerotic effect of Allium sativum. Atherosclerosis 144, 237-249. Kwon K-B, Yoo S-J, Ryu D-G, Yang J-Y et al (2002). Induction of apoptosis by diallyl disulfide through activation of caspase-3 in human leukemia HL-60 cells. Biochemical Pharmacology 63, 41-47. Lamm DL, Riggs DR (2000). The potential application of Allium sativum (garlic) for treatment of bladder cancer. Urol Clin North Am 27, 157. Lancaster JE, Shaw ML (1989). G-Glutayl peptides in the biosynthesis of S-alk(en)yl-L-cysteine sulfoxides (flavor precursors) in Allium. Phytochemistry 28, 455-460. Lanzotti V (2006). The analysis of onion and garlic. Journal of Chromatography A, 1112, 3-22. Lau BHS, Lam F, Wang-Cheng R (1987). Effects of an odormodified garlic preparation on blood lipids. Nutrition Research 7, 139-149. Ledezma E, Lopez JC, Marin P, Romero H et al (1999). Ajoene in the topical short-term treatment of tinea cruris and tinea corporis in humans. Randomized comparative study with terbinafine. Arzneimittelforschung 49, 544. Lybarger JA, Gallagher JS, Pulver DW, Litwin A et al (1982). Occupational asthma induced by inhalation and ingestion of garlic. The Journal of Allergy and Clinical Immunology 69, 448-454. Meng Y, Lu D, Guo N, Zhang L et al (1993). Anti-HCMV effect of garlic components. Virologica Sinica 8, 147-150. Milner JA (2001). Mechanisms by which garlic and allyl sulfur compounds suppress carcinogen bio-activation: garlic and carcinogenesis. Adv Exp Med Biol 492, 69. Mohammad SF, Woodward SC (1986). Characterisation of a potent inhibitor of platelet aggregation and release reaction isolated from Allium sativum (garlic). Thrombosis Research 44, 793-806. Naganawa R, Iwata N, Ishikawa K, Fukuda H et al (1996). Inhibition of microbial growth by ajoene, a sulphur-containing compound derived from garlic. Appl Environ Microbiology 62, 4238. O’Gara EA, Hill DJ, Maslin DM (2000). Activities of garlic oil, garlic powder and their diallyl constituents against Helicobacter pylori. Appl Environ Microbiol, 66: 2269. Rahman K (2001) Historical Perspective on Garlic and Cardiovascular Disease. Journal of Nutrition 131, 977S-979S. 17 Saravanan G, Prakash J (2004). Effect of garlic (Allium sativum) on lipid peroxidation in experimental myocardial infarction in rats. Journal of Ethnopharmacology 94, 155-158 Shen JK, Davis LE, Wallace JM, Cai Y et al (1996). Enhanced diallyl trisulfide has in vitro synergy with amphotericin B against Cryptococcus neoformans. Planta Medica 62, 415-418. Srivastava KC, Tyagi OC (1993). Effects of a garlic-derived principle (ajoene) on aggregation and arachidonic acid metabolism in human blood platelets. Prostaglandins Leukotrienes Essential Fatty Acids 49, 587. Takezaki T, Gao CM, Ding JH, Liu TK et al (1999). Comparative study of lifestyles of residents in high and low risk areas for gastric cancer in Jiangsu province, China; with special reference to allium vegetables. Journal of Epidemiology 9, 297. Walder R, Kalvatchev Z, Garzaro D, Barrios M et al (1997). In vitro suppression of HIV-1 replication by ajoene [(e)-(z)-4,5,9-trithiadodeca-1,6,11-triene-9 oxide]. Biomed Pharmacother 51, 397. Watt JM, Breyer-Brandwijl MG (1962). The Medicinal and Poisonous Plants of Southern and Eastern Africa. E. & S. Livingstone Ltd: Edinburgh and London. WHO Monographs on Selected Medicinal Plants (1999). Geneva (Switzerland): World Health Organization. Yang CY, Chao PDL, Hou YC, Tsai SY et al (2006). Marked decrease of cyclosporin bioavailability caused by co-administration of ginkgo and onion in rats. Food and Chemical Toxicology 44, 1572-1578. You WC, Zhang L, Gail MH, Ma JL et al (1998). Helicobacter pylori infection, garlic intake and pre-cancerous lesions in a Chinese population at low risk of gastric cancer. International Journal of Epidemiology 27, 941. Footnotes: Some Combination Products for Helminthiasis 1. 2. Dua ma aduro herbal worms expeller Okurufi Wormerplex _________________________________ Cassia occidentalis Botanical name Cassia occidentalis Linn. (Leguminosae) Local name(s) Mmofra borodee (Twi); anansedua (Fante); anyenle (Nzema); dzongbale (Ewe); faskori (Hausa). Chemical constituents Anthraquinone (e.g. sennoside, chrysophanol, physcion, helminthosporin, emodin); fatty oils, flavonoid ((jaceine 7rhamnoside, mattencinol 7-rhamnoside, cassiaoccidentalins A, B and C); xanthones (cassiollin); gallactomannan, polysaccharides and tannins (Chukwujekwu et al 2006; Chauhan et al 2001; Purwar et al 2003; Hatano et al 1999; Ikram et al 1978; Glasby 1991). Pharmacology Evaluation of C. occidentalis leaves showed antibiotic, anti-inflammatory and antihelmintic activity (Morton 1981; Robineau 1989; Chukwujekwu et al 2006). The leaf extracts exhibited significant broad spectrum activity against B. subtilis and S. aureus (Samy and Ignacimuthu 2000). The benzene and ether extracts of the leaves, root and seeds are active against Gram-positive and Gram-negative bacteria (Ikram et al 1978) and the leaf decoction was active against E. flocossum, M. gypseum, T. mentagrophytes and T. rubrum (Caceres et al 199lc). Ethanol and dichloromethane leaf extracts of the plant produced a high inhibition of parasite growth in vitro (Tona et al 1999). Aqueous extract of C. occidentalis possessed anti-mutagenic activity against benzo[a]pyrene and cyclophosphamide-induced mutagenicity in vitro and in vivo (Sharma et al 1999; Sharma et al 2000a). The administration of plant extract to cyclophosphamide-exposed animals resulted in improved humoral responses 18 (Bin-Hafeez et al 2001). C. occidentalis leaf powder and an ethanol extract of C. halicacabum exhibited antiinflammatory activity in male albino rats. C. occidentalis powder and C. halicacabum extract were able to stabilize the human erythrocyte membrane against hypotonicity-induced lysis (Sadique et al 1987). Medicinal uses Traditional system/folk medicine As an anti-inflammatory; antihepatotoxic; expectorant; antibacterial; antiplasmodial; tonic; febrifuge; diuretic, and are used against fevers, tuberculosis, anaemia, liver complaints; general weakness; fevers; asthma; bronchitis skin; venereal diseases, gastrointestinal disorders ; inflammation; rheumatism ((Chukwujekwu et al 2005; Tona et al 2004; Samy and Ignacimuthu 2000; Kuo et al 1996; Saraf et al 1994; Soukup 1970; Rutter 1990; Coimbra 1994; Ayensu 1981; Altschul 1983; Ronquillo 1988; Robineau 1989; Standley and Steyermark 1946 ; Kabiruddin 1951; Kirthikar et al 1969). Uses as described in pharmacopoeia Abdominal pains; anaemia; bacterial and fungal infections; cirrhosis; detoxification; hypertension; intestinal worms; liver disorders (jaundice, hepatitis, injury/failure, etc.); malaria; skin parasites; (Mshana et al 2000; GHP 1992). Uses supported by experimental or clinical data Antibiotic, anti-inflammatory; antimutagenic; antihelmintic Precautions and toxicology The fresh pod is toxic to cattle and pigs (Ikram et al 1978; Robineau 1989). Seeds of Cassia pordocarpa are also found to be toxic unless they are roasted. Contraindications Pregnancy; antihypertensives; hypotension Adverse effects Excessive consumption of seeds has been known to cause toxicity in poultry, cattle and rabbits Long term ingestion of small amounts and a single high dose of seeds caused myodegeneration, respiratory failure, disruption of mitochondrial structure and death in rabbits (O’Hara and Pierce, 1974) May interfere with the metabolism of some drugs in the liver because of its antihepatoxic and hepatic detoxification properties Dosage form Decoction; tincture Posology or recommended dose Decoction: 30 g of roasted ground seeds in 900 ml water; simmer until reduced to 600 ml; 1 teacup three times daily Tincture: 1:5 in 50% alcohol 5 ml three times daily References Altschul S (1983) Drugs and Foods from Lirrle-Known Planis. Harvard University Press, Cambridge MA 116-120. Ayensu ES (1981) Medicinal Plan& of the West Indies. Reference Publications, Algonac 282. 19 Bin-Hafeez B, Ahmad I, Haque R, Raisuddin S (2001). Protective effect of Cassia occidentalis L. on cyclophosphamide-induced suppression of humoral immunity in mice. Journal of Ethnopharmacology 75, 13-18. Cáceres A, Lopez BR, Giron MA, Logemann H (1991c) Plants used in Guatemala for the treatment of dermatophytic infections, And Screening for antifungal activity of 44 plant extracts. Journal of Ethnopharmacology 31, 263-276. Chauhan D, Chauhan JS, Siddiqui IR, Singh J (2001). Two new anthroquinone glycosides from leaves of Cassia occidentalis. Indian Journal of Chemistry Section BOrganic Chemistry including Medicinal Chemistry 40, 860-863. Chukwujekwu JC, Coombes PH, Mulholland DA, van Staden J (2006). Emodin, an antibacterial anthraquinone from the roots of Cassia occidentalis. South African Journal of Botany 72, 295-297. Chukwujekwu JC, van Staden J, Smith P (2005). Antibacterial, anti-inflammatory and antimalarial activities of some Nigerian medicinal plants. South African Journal of Botany 71, 316-325. Coimbra R (1994). Manual de Fitoterapia, 2nd edn. Editora Cejup, Belem, Brazil. Glasby JS (1991). Dictionary of Plants Containing Secondary Metabolites. Taylor & Francis, London 488. Hatano T, Mizuta S, Ito H, Yoshida T (1999). C-Glycosidic flavonoids from Cassia occidentalisPhytochemistry 52, 1379-1383 Ikram M, Hussain SF (1978) Compendium of Medicinal Plants. Pakistan Council of Scientific and Industrial Research, Peshawar 77-78. Jafri MA, Subhani MJ, Javed K, Singh S (1999). Hepatoprotective activity of leaves of Cassia occidentalis against paracetamol and ethyl alcohol intoxication in rats. Journal of Ethnopharmacology 66, 355-361. Kabiruddin M (1951). Makhzanul Advia Shaikh Mohd. Bashir, Lucknow, 454-455. Kirthikar KR, Basu BD, An ICS (1969). Indian Medicinal Plants, 2nd ed. Periodical Experts, New Delhi 1, 623. Kuo SC, Chen SC, La CF, Teng CM et al (1996). Studies on the anti-inflammatory and antiplatelet activities of constituents isolated from the roots and stem of Cassia occidentalis L. Chinese Pharmaceutical Journal 48, 291– 302. Morton JF (1987) Fruits of Warm Climates. Published by the author, Coral Gables FL 204-209. Mshana NR, Abbiw DK, Addae-Mensah I, Ahiyi MRA et al (2000). Traditional medicine and pharmacopoeia. Contribution to the revision of Ethnobotanical and Floristics Studies of Ghana. Organisation of African Unity/Scientific, technical and research committee. O’Hara PJ, Pierce KR (1974). Toxic cardiomyopathy caused by Cassia occidentalis II. Biochemical studies in poisoned rabbits. Vet Pathol. 11, 110-124. Purwar C, Rai R, Srivastava N, Singh J (2003). New flavonoid glycosides from Cassia occidentalis. Indian Journal of Chemistry Section B-Organic Chemistry Including Medicinal Chemistry 42, 434-436. Robineau L (1989) Hacia una Farmacopea Caribeia. Enda-Caribe y Universidad National Autonoma de Honduras, Santo Domingo 474. Ronquillo FA, Melgar MF, Carrillo JE, Martinez AB (1989) Especies Vegetales de Use Actual y Potential en Alimentacion y Medicina de Ias Zonas Semiaridas del Nororiente de Guatemala. Cuadernos de Investigacidn No. 7-88. USAC-DIGI, Guatemala, 249. Rutter RA (1990). Catalogo de Plantas Utiles de la Amazonia Peruana. Instituto Linguistico de Verano, Yarinacocha, Peru. Sadique J, Chandra V, Thenmozhi V, Elango V (1987). Biochemical modes of action of Cassia occidentalis and Cardiospermum halicacabum in inflammation. Journal of Ethnopharmacology 19, 201-212. Samy RP, Ignacimuthu S (2000). Antibacterial activity of some folklore medicinal plants used by tribals in Western Ghats of India. Journal of Ethnopharmacology 69, 63-71. Saraf S, Dixit VK, Tripathi SC, Patnaik GK (1994). Antihepatotoxic activity of Cassia occidentalis. International Journal of Pharmacognosy 32, 178-183. Sharma N, Trikha P, Athar M, Raisuddin S (1999). Protective effect of Cassia occidentalis extract on chemical-induced chromosomal aberrations in mice. Drug and Chemical Toxicology 22, 643-653. Sharma N, Trikha P, Athar M, Raisuddin S (2000a). In vitro inhibition of carcinogen-induced mutagenicity by Cassia occidentalis and Emblica officinalis. Drug and Chemical Toxicology 23, 477-484. Soukup J (1970). Vocabulary of the Common Names of the Peruvian Flora and Catalog of the Genera. Editorial Salesiano, Lima 436. Standley PC, Steyermark JA (1946). Flora of Guatemala. Fieldiana; Botany 24(5): 116-122, 246-266, 478-489. Tona L, Cimanga RK, Mesia K, Musuamba CT et al (2004). In vitro antiplasmodial activity of extracts and fractions from seven medicinal plants used in the Democratic Republic of Congo. Journal of Ethnopharmacology 93, 27-32. 20 Tona L, Ngimbi NP, Tsakala M, Mesia K et al (1999). Antimalarial activity of 20 crude extracts from nine African medicinal plants used in Kinshasa, Congo. Journal of Ethnopharmacology 68, 193-203. Footnotes: 1. Dua ma aduro herbal worms expeller _______________________________ Mitragyna inermis Botanical name Mitragyna inermis (Willd.) O. Kuntze Local name(s) Chemical constituents Indole alkaloids (rhynchophylline, rotundifoline, speciophylline and uncarine); triterpenoid saponins (inermiside I and inermiside II) (Cheng et al 2002; Shellard and Sarpong 1969, 1970; Shellard et al 1971). Pharmacology A synergistic antimalarial effect was shown between total alkaloids extracted from the leaves of Guiera senegalensis and those of M. inermis (Fiot et al 2006). The plant’s antimalarial activity and the lack of genotoxicity in vitro and in vivo have been demonstrated (Monjanel-Mouterde et al 2006). Antimalarial properties of the plant’s extracts have been demonstrated by its ability to inhibit Plasmodium falciparum growth (Mustafa et al 2000). Aqueous extracts of Mitragyna inermis produced a concentration-dependent ex vivo increase in cardiac contractile response and coronary flow but did not modify heart rate in the rat. This seemed to indicate that the extract possesses cardiac inotropic effect and induces an increase in coronary flow without inducing tachycardia in isolated heart (Ouédraogo et al 2004). Sy et al (2004) have reported the myorelaxant and antispasmodic actions of M. inermis’s extracts. Alkaloids from aqueous extracts of M. inermis have been reported to increase biliary flow, to decrease hepatic enzymes and total cholesterol in the rat (Touré et al 1996). Medicinal uses Traditional system/folk medicine Hepatic illness, stomach and intestinal disorders; malaria; hypertension (Adjanohoun et al 1985; Phillipson and Wright 1991). Uses as described in pharmacopoeia None available Uses supported by experimental or clinical data Antihypertensive; antispasmodic; antimalarial; choleretic Precautions and toxicology Acute and chronic evaluation of the toxicity of the hydroethanolic leaf extract of M inermis indicated the safety of repeated oral administration (up to 3 g/kg/d) of the herb (Monjanel-Mouterde et al 2006). 21 Contraindications None known Adverse effects None known Dosage form Decoction; tincture Posology or recommended dose Decoction: 30 g of leaves per litre of water. Boil for 10-15 minutes and drink a cup three times daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily References Adjanohoun FJ, Ake A, Floret JJ, Guinko S et al (1985). Contribution aux études ethnobotaniques et floristiques du Mali. Médecine Traditionnelle et Pharmacopée. ACCT, Paris, 64. Cheng Z-H, Yu B-Y, Yang X-W (2002). 27-Nor-triterpenoid glycosides from Mitragyna inermis. Phytochemistry 61, 379-382. Fiot J, Sanon S, Azas N, Mahioua V et al (2006). Phytochemical and pharmacological study of roots and leaves of Guiera senegalensis J.F. Gmel (Combretaceae). Journal of Ethnopharmacology 106, 173-178 Monjanel-Mouterde S, Traoré F, Gasquet M, Dodero F et al (2006). Lack of toxicity of hydroethanolic extract from Mitragyna inermis (Willd.) O. Kuntze by gavage in the rat. Journal of Ethnopharmacology 103, 319-326. Mustafa VA, Benoit-Vical F, Pelissier Y, Kone-Bamba D et al (2000). Antiplasmodial activity of plant extracts used in West African traditional medicine. Journal of Ethnopharmacology 73, 145-151. Ouédraogo S, Ranaivo HR, Ndiaye M, Kaboré ZI et al (2004). Cardiovascular properties of aqueous extract from Mitragyna inermis (wild). Journal of Ethnopharmacology 93, 345-350. Phillipson JD, Wright CW (1991). Can ethnopharmacology contribute to the development of antimalarial agents? Journal of Ethnopharmacology 32, 155-165. Shellard EJ, Sarpong K (1969). The alkaloids of the leaves of Mitragyna inermis (Willd.) O.Kuntze. J. Pharm. Pharmac. 21 (Suppl.), 113–117. Shellard EJ, Sarpong K (1970). The alkaloidal pattern in the leaves, stem-bark and root-bark of Mitragyna species from Ghana. J. Pharm. Pharmac. 22 (Suppl.), 34–39. Shellard EJ, Phillipson JD, Sarpong K (1971). Rhynchophylline and isorhynchophylline N-oxides from species of Mitragyna. Phytochemistry 10, 2505-2511. Sy GY, Sarr A, Dièye AM, Faye B (2004). Myorelaxant and antispasmodic effects of the aqueous extract of Mitragyna inermis barks on Wistar rat ileum. Fitoterapia 75, 447-450. Touré H, Balansard G, Pauli AM, Scotto AM (1996). Pharmacological investigation of alkaloids from leaves of Mitragyna inermis (Rubiaceae). Journal of Ethnopharmacology 54, 59-62. Wang XL, ZhangLM, Hua Z, ZhongY et al (1994), 15:115. Foot notes : 1. Okurufi Wormerplex ____________________________________ 22 Ricinus communis Botanical name Ricinus communis var. minor Local name(s) Castor bean; zurma (Hausa) Chemical constituents Glycerides of oleic, linoleic, stearic and ricinoleic acid; globulin, cholesterol, lipase, vitamin E; β-sitosterol; ricin, ricinine ((Scarpa and Guerci 1982). Pharmacology An ether-soluble fraction of a methanol extract of R. communis var. minor seeds administered subcutaneously to adult female rats and rabbits at doses up to 1.2 g/kg and 600 mg/kg, respectively, in divided doses showed antiimplantation and contraceptive activities (Okwuasaba et al 1991). Crude dichloromethane and methanolic extracts of plants (including R. communis) used traditionally in the treatment of wounds and retained placenta were screened for their antibacterial and anti-inflammatory activities. The results suggest that most plants used traditionally for treating wounds and retained placenta in animals are effective in combating infection and reduction of pain (Luseba et al 2007). Methanolic root extracts of R. communis showed anti-inflammatory and free radical scavenging activities in vivo (Ilavarasan et al 2006). Extracts of the leaves possess specific activity against Mycobacterium tuberculosis and Aspergillus niger (Kerharo 1967). The extract of the pericarp of castor bean showed some typical central nervous system stimulant effects when administered to mice. At lower doses the extract improved memory consolidation and showed some neurolepticlike properties, such as a decrease in exploratory behavior and catalepsy (Ferraz et al 1999). Extracts of the trunk have shown to be spasmolytic, caused increased blood flow in the hind leg of the rat and a decrease in blood pressure in the dog. Castor oil has purgative properties (Scarpa and Guerci 1982; Kerharo and Adams 1974). Ricin inhibits the formation of tumours in rats in the precocious stage, and also suppresses them after several days of development (Kerharo and Adams 1974). Pharmacodynamics The purgative properties of castor oil are due to ricinoleic acid liberated from glycerides, which acts on the small intestine, lyses the lipidic components of the intestinal mucosa, and cause a reflex exaggeration of peristalsis (Scarpa and Guerci 1982; Kerharo and Adams 1974). Medicinal uses Traditional system/folk medicine As purgative; in preparation for radiological examination of the gastrointestinal tract and as a vehicle for ophthalmic preparations oral contraceptive; treatment of various forms of dermatitis inflammation and liver disorders hepatoprotective laxative diuretic), antibacterial hypoglycaemic; rhinitis; angina; chest inflammation; bronchitis; pneumonia; asthma cerebral congestion; dental caries, odontalgia, swelling of the tongue, gastralgia, intestinal colic, belly-ache, vomiting, jaundice, peritonitis, dropsy, anthelmintic, diarrhoea and dysentery, astringent, purgative, strangulated hernia, prolapse of the rectum, hemorrhoids (Okwuasaba et al 1991; Fingl and 23 Freston 1979; Kirtikar and Basu 1991; Visen et al 1992; Dhar et al 1968; Capasso et al 1994; Abraham et al 1986; Verpoorte and Dihal 1987; Scarpa and Guerci 1982; Kerharo and Adams 1974; Watt and Breyer-Brandwijk 1962). Uses as described in pharmacopoeia None Uses supported by experimental or clinical data Contraceptive; antinociceptive; anti-inflammatory; antibacterial; spasmolytic; CNS stimulant; antioxidant. Precautions and toxicology Ricin produces an oxidative stress in the liver of mice which is maximal approximately 36 hr after parenteral administration of the toxin (Muldoon et al 1992). The alkaloid ricinine isolated from the plant Ricinus communis, when administered to mice at high doses, induces clonic seizures accompanied by electroencephalographic alterations in the cerebral cortex and hippocampus (Ferraz et al 2002).The fresh seeds are very poisonous (Scarpa and Guerci 1982). Contraindications None available Adverse effects The pulp of the seeds contains allergens (glycoproteins) which in particularly sensitive persons can promote strong allergic reactions such as coryza, conjunctivitis, dermatitis, eczema, and bronchial asthma (Kerharo and Adams 1974; Watt and Breyer-Brandwijk 1962). Dosage form Decoction; tincture Posology or recommended dose Decoction: 30 g in 900 ml water; simmer until reduced to 600 ml; 1 teacup three times daily Tincture: 1:5 in 50% alcohol 5 ml three times daily References Abraham Z, Bhakuni SD, Garg HS, Goel AK et al 1986. Screening of Indian plants for biological activity. Part XII. Indian Journal of Experimental Biology 24, 48-68. Dhar ML, Dhar MM, Dhawan BN, Mehrotra BN et al (1968). Screening of Indian plants for biological activity. Part I. Indian Journal of Experimental Biology 6, 232247. Capasso F, Mascolo N, Izzo AA, Gaginella TS (1994). Dissociation of castor oil induced diarrhoea and intestinal mucosal injury in rat: effect of NG-nitro-L-arginine methyl ester. British Journal of Pharmacology 113, 1127–1130. Ferraz AC, Angelucci MEM, Da Costa ML, Batista IR (1999). Pharmacological Evaluation of Ricinine, a Central Nervous System Stimulant Isolated from Ricinus communis. Pharmacology Biochemistry and Behavior 63(3): 367-375. Ferraz AC, Anselmo-Franci JA, Perosa SR, de Castro-Neto EF et al (2002). Amino acid and monoamine alterations in the cerebral cortex andhippocampus of mice submitted to ricinine-induced seizures. Pharmacology, Biochemistry and Behavior 72, 779-786. Fingl E, Freston JW (1979). Antidiarrhoeal agents and laxatives: Changing concepts. Clinical Gastroenterology 8,161-185. 24 Ilavarasan R, Mallika M, Venkataraman S (2006). Anti-inflammatory and free radical scavenging activity of Ricinus communis root extract. Journal of Ethnopharmacology 103, 478-480 Kerharo J, Adam JG (1974). La Pharmacopée Sénégalaise Traditionnelle, Vigot Frères, Paris, 429. Kerharo J (1967). La Pharmacopée Sénégalaise: Catalogue des Plantes Médicinales et Toxiques des Wolof et des Sérer, Masson Ed., Paris, 417. Kirtikar KR, Basu BA (1991). Indian Medicinal Plants 3, 2274-2277. Luseba D, Elgorashi EE, Ntloedibe DT, van Staden J (2007). Antibacterial, anti-inflammatory and mutagenic effects of some medicinal plants used in South Africa for the treatment of wounds and retained placenta in livestock. South African Journal of Botany 73, 378-383 Muldoon DF, Hassoun EA, Stohs SJ (1992). Ricin-induced hepatic lipid peroxidation, glutathione depletion, and DNA single-strand breaks in mice. Toxicon 30(9): 977984. Okwuasaba FK, Osunkwo UA, Ekwenchi MM, Ekpenyong KI et al (1991). Anticonceptive and estrogenic effects of a seed extract of Ricinus communis var. minor. Journal of Ethnopharmacology 34, 141-145. Scarpa A, Guerci A (1982). Various uses of the castor oil plant (Ricinus communis L.)-A review. Journal of Ethnopharmacology 5, 117-137. Verpoorte R, Dihal PP (1987). Medicinal plants of the Surinam. IV. Antimicrobial activity of some medicinal plants. Journal of Ethanopharmacology 21, 315-318. Visen P, Shukla B, Patnaik G, Tripathi S et al (1992). Hepatoprotective activity of Ricinus communis leaves. International Journal of Pharmacognosy 30, 241–250. Watt JM, Breyer-Brandwijk MG (1962). Medicinal and Poisonous Plants of Southern and Eastern Africa, E. S. Livingstone, Edinburgh, London, 430. Footnotes: 1. Dua ma aduro herbal worms expeller ___________________________ Monographs on Medicinal Plants for Malaria and Febrile Illnesses 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. Acanthospermum hispidum Alchornea cordifolia Alstonia boonei Anthocleista nobilis Azadirachta indica Canthium glabriflorum Carapa procera Carica papaya Cassia siamea Cassia occidentalis Cryptolepis sanguinolenta Hoslundia opposita Hydrastis Canadensis Khaya ivorensis Khaya senegalensis Lantana camara Mangifera indica Ocimum basilicum Paullinia pinnata Parinari robusta Persea Americana Phyllanthus niruri Psidium guajava Pycnanthus angolensis Momordica charantia 25 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. Monodora myristica Morinda lucida Nauclea latifolia Newbouldia laevis Rauwolfia vomitoria Solanum torvum Spathodea campanulata Tabernaemontana crassa Trema orientalis Xylopia aethiopica Vernonia amygdalina ______________________________ Acanthospermum hispidum Botanical name Acanthospermum hispidum DC Local name(s) Not available Chemical constituents Essential oils (sesquiterpenes, aliphatic aldehydes and aromatic compounds); alkaloids; diterpenes; sugars (Fleischer et al 2003; Cartagena et al 2000; Nair et al 1976) Pharmacology The crude ethanolic extracts of the leaves and flowering tops of A. hispidum showed various degrees of antibacterial activity particularly against Gram-positive organisms (Fleischer et al 2003). A significant antimalarial activity has been observed with alkaloid extract of A. hispidum (Sanon et al 2003). Aqueous extract of the leaves of A. hispidum exhibited antiviral activity by interaction with α-herpes virus particles resulting in inhibition of attachment to and penetration into target cells (Summerfield et al 1997). The immunostimulatory capacity of A. hispidum was studied in vitro. The plant was shown to enhance the proliferation of T lymphocytes. The virusspecific MHC class II restricted in vitro immune response against pseudorabies virus (PRV) was also enhanced in a co-stimulating manner (Summerfield and Saalmüller 1998). In an attempt to evaluate the abortifacient/or teratogenic effect of extracts of A. hispidum and Cajanus cajan, used in Brazil to cause, female Wistar rats were treated with the aqueous extract (infusion, proportion C. cajan and A. hispidum 1:1.3). There was no significant change in the mean weight of the fetuses, and no change in the percentage of post implantation loss in the treated groups. There was, however, an increase in the number of external malformations in a dose-related manner. No internal malformations were observed in fetuses at term, but there was a significant incidence of fetuses with visceral anomalies (Lemonica and Alvarenga 1994). Medicinal uses Traditional system/folk medicine As an anthelmintic; abortifacient; diuretic, febrifuge, sudorific; for the treatment of boils; hypertension; gonorrhea ((Fleischer et al 2003; Menut et al 1995; Lemonica and Alvarenga 1994; Uphof 1968; Morton 1981). Uses as described in pharmacopoeia Not available 26 Uses supported by experimental or clinical data Immunostimulant; antimalarial; antiviral; teratogenic Precautions and toxicology Seeds of A. hispidum have toxic effects characterized by haemorrhage, weakness and diarrhoea (Ali and Adam 1978). Poisoning in goats manifested as jaundice, diarrhoea, weakness of the hind limbs and debility (Ali and Adam 1978). Contraindications Not available Adverse effects None reported in humans Dosage form Decoction; tincture; fluid extract Posology or recommended dose Decoction: 30 g dried leaves in 900 ml water; simmer until reduced to 600 ml; 1 teacup three times daily Tincture- 1:5 45% alcohol, 5 ml three times daily Liquid extract (1:2), 45% alcohol, 2.5 ml three times daily References CMD (1994). Abortive and teratogenic Ali B and Adam SEI (1978a). Effects of Acanthospermum hispidum on goats. Journal of Comparative Pathology 88, 533-544. Ali B and Adam SEI (1978b). Toxicity of Acanthospermum hispidum to mice. Journal of Comparative Pathology 88, 443-448. Cartagena E, Bardon A, Catalan CAN, de Hernandez ZNJ et al (2000). Journal of Natural Products 63(10):1323. Fleischer TC, Ameade EPK, Sawer IK (2003). Antimicrobial activity of the leaves and flowering tops of Acanthospermum hispidum. Fitoterapia 74, 130–132. Lemonica IP, Alvarenga effect of Acanthospermum hispidum DC. and Cajanus Cajan (L.) Millps. in pregnant rats. Journal of Ethnopharmacology 43, 39-44. Menut C, Molangui T, Lamaty G, Ouamba JM et al (1995). Journal of Essential Oil Research 7, 589. Morton JF (1981). Atlas of Medicinal Plants of Middle America, Bahamas to Yucatan. Charles C. Thomas, Springfield, IL, 900. Nair AGR, Subramanan SS, Bohlmann F, Schöneweiss S et al (1976). A new diterpene galactoside from Acanthospermum hispidum. Phytochemistry 15, 1776-1778. Sanon S, Ollivier E, Azas N, Mahiou V et al (2003). Ethnobotanical survey and in vitro antiplasmodial activity of plants used in traditional medicine in Burkina Faso. Journal of Ethnopharmacology 86, 143-147. Summerfield A, Keil GM, Mettenleiter TC, Rziha H-J et al (1997). Antiviral activity of an extract from leaves of the tropical plant Acanthospermum hispidum. Antiviral Research 36, 55–62 Summerfield A, Saalmüller A (1998). Interleukin-2 dependent selective activation of porcine γδ T lymphocytes by an extract from the leaves of Acanthospermum hispidum. International Journal of Immunopharmacology 20, 85-98. Uphof JCTh (1968) Dictionary of Economic Plants, 2nd edn. Verlag von J. Cramer, F.R.G.; 7, 273, 281 and 507. Footnotes: 27 Some Combination Products for Malaria 1. 2. 3. 4. 5. 6. 7. 8. 9. Class Malacure Herbaquin Millennium Fever Remedy Top Fever Syrup Freedom Herbal Mixture Alafia Malaria Fever Herb Golden Malacure Cryptoquine Malaherb\ 10. Mist Nibima ___________________________ Alchornea cordifolia Botanical name Alchornea cordifolia (Schumach. & Thonn.) Müll. Arg. Local name(s) Agyamma (Twi); gboo (Ga-Adangbe); avovlo (Ewe) Chemical constituents Yohimbine, gentisic acid and anthranilic acid; alchornoic acid; β-sitosterol; flavonoids, tannins (ellagic acid), carbohydrates, saponins, alkaloids (Osadebe and Okoye 2003; Banzouzi et al 2002; Ajali 2000). Pharmacology Results from the in vitro antiamoebic activity of some Congolese plant extracts used as antidiarrhoeic in traditional medicine indicated that root bark extract of A. cordifolia had antiamoebic (Tona et al 1998). The aqueous extracts of A. cordifolia, Persea americana and Psidium guajava inhibited the growth of all bacterial species tested. The extract of Alchornea cordifolia inhibited the growth of all 15 MRSA isolates (Pesewu et al 2008). Extracts of A. cordifolia stem bark extracts exhibited antimicrobial activities (Ajali 2000). Extracts of A. cordifolia containing phenolics and terpenoids, exhibited significant activity against Pseudomonas aeruginosa, Bacillus subtilis and Escherichia coli (Ebi 2001). The extracts from Alcornea cordifolia leaves extract showed a pronounced antiprotozoal activity against Trypanosoma cruzi as well as a pronounced antiplasmodial activity against P. falciparum (Mesia et al 2008). The seeds of A. cordifolia displayed high antiviral activity against HIV-1 strain HTLVIIIB cytopathicity and HIV-1 reverse transcriptase (RT) activity (Ayisi and Nyadedzor 2003). The ethanol fraction from hexane extract of A. cordifolia leaves exhibited potent anti-inflammatory activity (Osadebe and Okoye 2003). Topical application of methanolic leaf extract showed anti-inflammatory activity (Mavar-Manga et al 2004). An in vitro study conducted on four commonly used tropical medicinal plants (Kigelia africana, Calotropis procera, Hibiscus sabdariffa and Alchornea cordifolia) antioxidant effects showed that the use of these plants in the treatment of various diseases, especially liver disease, is probably due to their ability to act as antioxidants (Olalye and Rocha 2007). Administration of (100 mg/kg) of A. cordifolia acted as a hepatoprotective against paracetamol toxicity (Olaleye and Rocha 2007). Ethanolic extracts of A. cordifolia has antidrepanocytary actvity (anti-sickle cell anemia) (Mpiana et al 2007). Medicinal uses Traditional system/folk medicine Anti-inflammatory; as a purgative; for fever; reuhmatic pains, and for the treatment of leprosy dermatitis, asthma, hepatitis, splenomegaly, vaginitis, colitis; yaws, wounds; ulcers, gum inflammation and conjunctivitis ((MavarManga et al 2004; Neuwinger 2000; (Agoha 1960). 28 Uses as described in pharmacopoeia Antidiarrhoeal; antifungal; antiinflammatory; antiprotozoal; antirheumatic; antispasmodic; antiviral; (GHP 1992; Ogungbamila and Samuelsson 1990); for the treatment of abdominal pain; diarrhoea; dysentery; dysmenorrhoea; fever; fracture; gonorrhoea; hernia; herpes zoster; rheumatic pains; ringworm; septicaemia; stomatitis; ulcer; whooping cough; wounds; yaws (Mshana et al 2000; GHP 1992; Ogungbamila and Samuelsson 1990). Uses supported by experimental or clinical data Antioxidant; antiamoebic; antibacterial; antiviral; antidrepanocytary actvity (anti-sickle cell anemia); antiprotozoal; antiplasmodial Precautions and toxicology See contraindications and adverse effects Contraindications Liver dysfunctions; hepatitis, cirrhosis, Adverse effects None known Dosage form Decoction; tincture; infusion Posology or recommended dose Infusion: 20-30 g of dried leaves per litre of water; 3-4 cups daily Decoction: 30-50 g per litre of water; 3-4 teacups daily Tincture: 1:5, 45% alcohol, take 5 ml three times daily References Ajali U (2000). Antibacterial activity of Alchornea cordifolia stems bark. Fitoterapia 71, 436-438. Agohas BC (1960). Malaria. In: Oliver OB, editor. Medicinal plants in Nigeria. Ibadan: University Press, 22. Ayisi NK, Nyadedzor C (2003). Comparative in vitro effects of AZT and extracts of Ocimum gratissimum, Ficus polita, Clausena anisata, Alchornea cordifolia, and Elaeophorbia drupifera against HIV-1 and HIV-2 infections. Antiviral Research 58, 25-33. Banzouzi J, Prado R, Menan H, Valentin A et al (2002). In vitro antiplasmodial activity of extracts of Alchornea cordifolia and identification of an active constituent: ellagic acid. Journal of Ethnopharmacology 81, 399–401. Ebi GC (2001). Antimicrobial activities of Alchornea cordifolia. Fitoterapia 72, 69-72 Ghana Herbal Pharmacopoeia (1992). The Advent Press: Accra, Ghana; 7-9. Mavar Manga H, Brkic D, Marie DEP, Quetin-Leclercq J (2004). In vivo Anti-inflammatory activity of Alchornea cordifolia (Schumach. & Thonn.) Müll. Arg. (Euphorbiaceae). Journal of Ethnopharmacology 92, 209-214. Mesia GK, Tona GL, Nanga TH, Cimanga RK et al (2008). Antiprotozoal and cytotoxic screening of 45 plant extracts from Democratic Republic of Congo. Journal of Ethnopharmacology 115, 409-415. Mpiana PT, Tshibangu DST, Shetonde OM, Ngbolua KN (2007). In vitro antidrepanocytary actvity (anti-sickle cell anemia) of some Congolese plants. Phytomedicine 14, 192-195 Mshana NR, Abbiw DK, Addae-Mensah I, Ahiyi MRA et al (2000). Traditional medicine and pharmacopoeia. Contribution to the revision of Ethnobotanical and Floristics Studies of Ghana. Organisation of African Unity/Scientific, technical and research committee. Neuwinger HD (2000). African traditional medicine-a dictionary of plant use and applications. Medical Pharmacology. Stuttgart, Germany, 29-30. 29 Ogungbamila FO, Samuelsson G (1990). Smooth muscle relaxing flavonoids from Alchornea cordifolia. Acta Pharm Nord.; 2(6): 421-2. Olalye MT, Rocha JBT (2007). Commonly used tropical medicinal plants exhibit distinct in vitro antioxidant activities against hepatotoxins in rat liver. Experimental and Toxicologic Pathology 58, 433–438. Olaleye MT, Rocha BTJ (2007). Acetaminophen-induced liver damage in mice: Effects of some medicinal plants on the oxidative defense system. Experimental and Toxicologic Pathology, doi:10.1016/j.etp.2007.10.003 Osadebe PO, Okoye EC (2003). Anti-inflammatory effects of crude methanolic extract and fractions of Alchornea cordifolia leaves. Journal of Ethnopharmacology 89, 19–24. Pesewu GA, Cutler RR, Humber DP (2008). Antibacterial activity of plants used in traditional medicines of Ghana with particular reference to MRSA. Journal of Ethnopharmacology 116, 102–111. Tona L, Kambu K, Ngimbi N, Cimanga K et al (1998). Antiamoebic and phytochemical screening of some Congolese medicinal plants. Journal of Ethnopharmacology 61, 57-65. Footnotes: 1. Nyame Ndae Bitters _____________________________ Canthium substratum Botanical name Canthium subcordatum Local name(s) Not available Chemical constituents Iridoid (shanzhiside methyl ester); calmatambin; orcinol monomethyl ether and scopoletin (Achenbach et al 1981). Pharmacology It has been reported that alcoholic extracts of the stem bark have potential antidiabetic Properties (Ampofo 1977). Medicinal uses Traditional system/folk medicine Hypertension; diabetes Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Antidiabetic Precautions and toxicology Not available 30 Contraindications None known Adverse effects None known Dosage form Decoction ; tincture Posology or recommended dose Decoction: 30 g of dried plant part in 900 ml water; simmer until reduced to 600 ml; 1 teacup three times daily Tincture: 1:5 in 50% alcohol, 5 ml three times daily References Achenbach H, Waibel R, Raffelsberger B, Addae-Mensah I (1981). Iridoid and other constituents of Canthium subcordatum. Phytochemistry 20(7): 1591-1595 Ampofo O (1977). Paper read at the Third Symposium on Medicinal Plants, Ife, Nigeria. Footnotes: 1. Kaasa Feverquine __________________________ Carapa procera Botanical name Carapa procera Local name(s) Not available Chemical constituents Tannins, phytic acid, tetranortriterpenoid; amino acid (Amubode and Fetuga 1984; Balogun and Fetuga 1988; Sondengam et al 1981) Pharmacology Not available Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available 31 Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References Amubode FO, Fetuga BL (1984). Amino Acid Composition of Seeds of Some Lesser Known Tree Crops. Food Chemistry 13, 299-307 Balogun AM, Fetuga BL (1988). Tannin, Phytin and Oxalate Contents of Some Wild Under-utilized Crop-seeds in Nigeria. Food Chemistry 30, 37-43 Sondengam BL, Kamga CS, Kimbu SF, Connolly JD (1981). Proceranone, a new tetranortriterpenoid from Carapa procera. Phytochemistry, 20, 173-174 Footnotes: 1. Malakare 2. Nyame Ndae Bitters _______________________________ Cassia siamea Botanical name Cassia siamea Local name(s) Not available Chemical constituents Anthraquinones (Singh et al 1992); barakol, emodin, α- and β-sitosterol, lupeol, luteolin, d-pinitol, chromone alkaloids, flavonoid (Ahn et al 1978; Shafiullah et al 1995). Pharmacology Crude hot aqueous extracts of the plant exhibited antimalarial properties against Plasmodium falciparum in vitro (Gbeassor et al 1989). The alcoholic extract of C. siamea flowers has potent antioxidant activity (Kaur et al 2006). C. siamea bark extracts have antimalarial properties (Mbatchi et al 2006). Alcoholic extracts of C. siamea have been shown to possess central nervous system depressant activity, decrease spontaneous locomotor activity, increase smooth muscle tone (Arunlakshana 1949) and decrease blood pressure (Mokasmit 1981). Barakol, a purified 32 extract of C. siamea is hypotensive (Suwan et al 1992), anti-serotonergic (Tongroach et al 1992) and anxiolytic in vivo (Thongsaard et al 1996). It reduced spontaneous locomotor activity and prolonged the thiopental-induced sleeping time, indicating a sedative effect (Sukma et al 2002). In addition, barakol suppressed K+-stimulated endogenous dopamine release from striatal slices of the rat brain (Thongsaard et al 1997) and exhibited purgative action in small intestine (Deachapunya et al 2005). Anthraquinone monomers obtained from C. siamea showed higher anti-tumor promoting activity than that of bianthraquinones (Koyama et al 2001). Also the compounds emodin and cassiamin B, isolated from Cassia siamea have remarkable anti-tumor promoting effect in mouse (Koyama et al 2002). Medicinal uses Traditional system/folk medicine As a purgative; antipyretic; for treating fever; diabetes, as a dressing for ringworm and chilblains; constipation; hypertension and insomnia (Ahn et al 1978; Satyavati et al 1979; Kinghorn and Balandrin 1992). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Antimalarial; antioxidant; depressant; anti-serotonergic; hypotensive; anxiolytic; antitumour; purgative Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Decocoction; infusion; tincture Posology or recommended dose Infusion: 20-30 g per litre of water; 3-4 cups daily Decoction: 30-50 g per litre of water; 3-4 teacups daily Tincture: 1:5, 45% alcohol, take 5 ml three times daily References Ahn BZ, Degen U, Lienjayetz C, Pachaly P et al (1978). Constituents of Cassia siamea. Archives of Pharmacology 311, 569-578. Arunlakshana O (1949). Pharmacological study of the leaves of Cassia siamea. Siriraj Hospital Gazette 1, 434-444. Deachapunya C, Thongsaard W, Poonyachoti S (2005). Barakol suppresses norepinephrine-induced inhibition of spontaneous longitudinal smooth muscle contractions in isolated rat small intestine. Journal of Ethnopharmacology 101, 227-232 Gbeassor M, Kossou Y, Amegbo K, De Souzas C et al (1989). Antimalarial effects of eight African medicinal plants. Journal of Ethnopharmacology 25, 115-118 . Kaur G, Alam MS, Jabbar Z, Javed K et al (2006). Evaluation of antioxidant activity of Cassia siamea flowers. Journal of Ethnopharmacology 108, 340–348. 33 Koyama J, Morita I, Tagahara K, Nobukuni Y et al (2002). Chemopreventive effects of emodin and cassiamin B in mouse skin carcinogenesis. Cancer Letters 182, 135139 Koyama J, Morita I, Tagahara K, Ogata M et al (2001). Inhibitory effects of anthraquinones and bianthraquinones on Epstein-Barr virus activation. Cancer Letters 170, 15-18 Mbatchi SF, Mbatchi B, Banzouzi JT, Bansimba T et al (2006). In vitro antiplasmodial activity of 18 plants used in Congo Brazzaville traditional medicine. Journal of Ethnopharmacology 104, 168–174 Mokasmit M (1981). Hypertensive effects of Thai medicinal plants. Newsletter of National Research Council of Thailand 22, 3–4. Shafiullah M, Parveen M, Kamil M, Illyas M (1995). A new isflavone C-glycoside from Cassia siamea. Fitoterapia 65, 339-341. Singh V, Singh J, Sharma JP (1992). Anthraquinones from heartwood of Cassia siamea. Phytochemistry 31(6): 2176-2177 Sukma M, Chaichantipyuth C, Murakami Y, Tohda M et al (2002). CNS inhibitory effects of barakol, a constituent of Cassia siamea Lamk. Journal of Ethnopharmacology 83, 87-94 Suwan G, Sudsuang R, Ghumma-Upakorn D, Werawong C (1992). Hypertensive effects of barakol extracted from leaves of Cassia siamea Lam. in rats and cats. Thai Journal of Physiological Science 5, 53–65. Thongsaard W, Deachapunya C, Pongsakorn S, Boyd EA et al (1996). Barakol: A potential anxiolytic extracted from Cassia siamea. Pharmacology Biochemistry and Behavior 53, 753–758. Thongsaard W, Pongsakorn S, Sudsuang R, Bennett GW et al (1997). Barakol, a natural anxiolytic, inhibits striatal dopamine release but not uptake in vitro. European Journal of Pharmacology 319, 157-164. Tongroach P, Jantarayota P, Tantisira B, Kunluan P et al (1992). Barakol, a neuroactive compound from Cassia siamea. In: Proceedings of the First JSPS-NRCT Joint Seminar in Pharmaceutical Sciences: Advances in Research on Pharmacologically Active Substances from Natural Sources, Chiangmai, Thailand, and P21. Footnotes: 1. Nyame Ndae Bitters ________________________________ Hoslundia opposita Botanical name Hoslundia opposita Vahl, Local name(s) Aberewa-aninsu (Twi); ablewa nunsu (Ga-Adangbe); akotadzeveti (Ewe) Chemical constituents Flavonoids (hoslundin, hoslundal, hoslunddiol, oppositin); jacarandic acid, oleanolic and ursolic acids, sitosterol, campesterol, stigmasterol and stigmastanol; abietane-type esters (3-O-benzoylhosloppone; 3-Ocinnamoylhosloppone; 3-O-benzoylhinokiol; 3-O-benzoylhosloquinone); tannins; sesquiterpenes (germacrene, ßcaryophylline) (Ngadjui et al 1993; 1991; Achenbach et al 1992; GHP 1992). Pharmacology A chloroform extract of H. opposita roots exhibited anticonvulsant activity and potentiated the phenobarbitone sleeping time (Olajide et al 1999). Aqueous and ethanol extracts of 43 plants including H. opposita, that are traditionally used to treat epilepsy and convulsions (Moshi et al 2005), showed anticonvulsant effects in the GABAA-benzodiazepine receptor binding assay (Risa et al 2004). The crude n-hexane extract of the root bark was 34 found to have significant in vitro activity against Plasmodium falciparum. It showed potent activity against the multidrug resistant K, strain of Plasmodium falciparum and the chloroquine sensitive strain (Achenbach et al 1992). The essential oil has significant antibacterial activity against Aspergillus niger, Acinetobacter calcoacetica, Brochothrix thermosphacta and Flavobacterium suaveolens (Gundidza et al 1992). Medicinal uses Traditional system/folk medicine Purgative, diuretic, febrifuge, antibiotic, and antiseptic; for the treatment of gonorrhoea, cystitis, coughs, fever, wounds, convulsions, sores, mental disturbances, abdominal pains, malaria; snake bites and for the relief of swellings; snake bite, herpes, conjuctivitis, chest pain, yellow fever (Watt and Breyer-Brandwijk 1962; Achenbach et al 1992; Olajide et al 1999; Ngadjui et al 1991). Uses as described in pharmacopoeia Colds; cough; convulsion; diabetes mellitus; fever; jaundice; Herpes zoster (liniment); purgative; sore throat; wounds (GHP 1982). Uses supported by experimental or clinical data Anticonvulsant, antimalarial; antibacterial Precautions and toxicology Not available Contraindications None known Adverse effects None known Dosage form Tinctures; decoctions/infusions; liniment Posology or recommended dose Decoction: 40 g in1 litre of water; drink 4 cups daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily References Achenbach H, Waibel R, Nkunya MHH, Weenen H (1992). Antimalarial compounds from Hoslundia opposita. Phytochemistry 31(11): 3781-3784. Ghana Herbal Pharmacopoeia (1992). The Advent Press: Accra, Ghana 71-73, Gundidza GM, Deans SG, Svoboda KP, Mavi S (1992) Antimicrobial activity of essential oil from Hoslundia opposita. Central African Journal of Medicine 38(7): 290293 Moshi MJ, Kagashe GAB, Mbwambo ZH (2005). Plants used to treat epilepsy by Tanzanian traditional healers. Journal of Ethnopharmacology 97, 327-336. Ngadjui BT, Ayafor JF, Sondengam BL, Connolly JD (1993). Oppositin and 5-O-methylhoslundin, pyrone-substituted flavonoids of Hoslundia opposita. Phytochemistry 32(5): 1313-1315. 35 Ngadjui BT, Ayafor JF, Sondengam BL (1991). Hoslundin, hoslundial and hoslundiol: three new flavonoids from the twigs of Hoslundia opposita (Lamiaceae). Tetrahedron 47(22): 3555-3564. Olajide OA, Awe SO, Makinde JM (1999). Central nervous system depressant effect of Hoslundia opposita Vahl. Phytotherapy Research 13, 425-426. Risa J, Risa A, Adsersen A, Gauguin B et al (2004). Screening of plants used in southern Africa for epilepsy and convulsions in GABAA-benzodiazepine receptor assay. Journal of Ethnopharmacology 93, 177-182. Watt JM, Breyer-Brandwijk MG (1962). The Medicinal and Poisonous Plants of Southern and Eastern Africa. Livingstone, Edinburgh. Footnotes: 1. Golden Malacure ___________________________________ Hydrastis canadensis Botanical name Hydrastis Canadensis Local name(s) Goldenseal Chemical constituents Alkaloids (Berberine, hydrastine, canadine); volatile oil; chlorogenic acid Pharmacology Ethanolic extracts from fresh Echinacea purpurea, Spilanthes acmella and dried H. canadensis were studied for their ability to inhibit cytochrome P4502E1 mediated oxidation of p-nitrophenol in vitro. H. canadensis was a strong inhibitor of the P4502E1, probably due to the presence of the alkaloids berberine, hydrastine and canadine in the extract (Ranner et al 2007) and therefore holds potential as an antioxidant. Hydrastine and berberine can reduce gastric inflammation, relieve congestion, and destroy many types of bacterial and viral infections (Palmery et al 1997; Seazzocchio et al 2001). From an investigation of the antigen-specific in vivo immunomodulatory potential of continuous treatment with Echinacea and Goldenseal root extract over a period of 6 weeks in rats injected with the antigen keyhole limpet hemocyanin (KLH) and re-exposed to KLH after the initial exposure, it was observed that the Echinacea-treated group showed a significant augmentation of their primary and secondary IgG response to the antigen, whereas the Goldenseal-treated group showed an increase in the primary IgM response (Rehman et al 1999). Alcoholic extract of H. canadensis showed inhibitory action on adrenaline, serotonin or histamineinduced contraction of rabbit aorta (Palmery et al 1993). 36 Medicinal uses Traditional system/folk medicine To treat sore eyes and mouth, cold; flu; whooping cough, pneumonia, digestive disorders and postpartum haemorrhage (He et al 2007; Duke 2001). Hydrastis is thought to be a potent remedy for disorders affecting mucus membranes throughout the body, especially in the eye, ear, nose and throat, stomach and intestines and the vagina. Internally, it increases digestive secretions, astringes the mucous membranes lining the gut, and checks inflammation Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Anti-inflammatory; antibacterial; antiviral; immunomodulatory; astringent; vasoconstrictive; antioxidant; choleretic; stimulant to the autonomic nervous system and sedative to the central nervous system; canadine is stimulant to the muscles of the womb Precautions and toxicology Do not prescribe for extended periods of time as it is thought to inhibit absorption of nutrients, notably vitamin B. Contraindications Pregnancy and lactation; high blood pressure Adverse effects Toxic if taken to excess; max 3 months continual use Dosage form Decoctions, tinctures; fluid extracts; capsules; lotion Posology or recommended dose Decoction/capsules: max 2.5 g a day; tablet as recommended Tincture: 1:5, 60% alcohol, 40 ml per week Fluid extract: about 20 ml per week Lotion: use decoction; or tincture diluted (50/50%) with water or glycerine References Duke J (2001). Handbook of Medicinal Herbs. CRC Press LLC, Boca Raton, FL, 238-247. He S-s, Liu C-z, Saxena PK (2007). Plant regeneration of an endangered medicinal plant Hydrastis canadensis L. Scientia Horticulturae 113, 82-86. Palmery M, Comela ME, Abdel-Haq H (1997). Antiscrotoninergic activity of the major alkaloid from Hydrastis canadensis L. on isolated rabbit aorta. Pharm. Res. 35, 28. Palmery M, Leone MG, Pimpinella G, Romanelli L (1993). Pharmacological Research 27(1): 73-74. 37 Raner GM, Cornelious S, Moulick K, Wang Y et al (2007). Effects of herbal products and their constituents on human cytochrome P450 2E1 activity. Food and Chemical Toxicology 45, 2359–2365 Rehman J, Dillow JM, Carter SM, Chou J et al (1999). Increased production of antigen-specific immunoglobulins G and M following in vivo treatment with the medicinal plants Echinacea angustifolia and Hydrastis canadensis. Immunology Letters 68, 391-395 Seazzocchio F, Cometa MF, Tomassini L, Palmery M (2001). Antibacterial activity of Hydrastis canadensis extract and its major isolated alkaloids. Planta Medica 67, 561-564. Footnotes: 1. Millennium Fever Remedy _______________________ Lantana camara Botanical name Lantana camara Linn Local name(s) Not available Chemical constituents Triterpenes (lantadene A and lantadene B); monoterpenoids; sesquiterpenoids; iridoid glycoside (theveside) umuhengerin, verbascoside, flavonoids (camaraside), phenylpropanoids (lantanaside) (Mahato et al 1994). Pharmacology Crude extracts of L. camara exhibited significant antimicrobial activity (Kumar et al 2006). The plant has antibacterial activity against Bacillus subtilis and Staphylococcus aureus (Ioset et al 2000; Misra and Laastsch 2000; Magassouba et al 2007). The essential oil has a wide spectrum of antibacterial and antifungal activities (Deena and Thoppil 2000; Magassouba et al 2007). Verbascoside contained in L. camara has been reported to possess antimicrobial, immunosuppressive and antitumor activities (Mahato et al 1994). Petroleum ether and methanol extracts of the aerial parts of L. camara exhibited insecticidal, antiovipositional and antifeedant activity (Saxena et al 1992). The steroid, lancamarone, from the leaves exhibited cardiotonic properties. An alkaloid fraction isolated from the leaves has promising antipyretic, antiasthmatic and hypotensive properties. The alkaloid, lantamine obtained from the stem bark and roots showed antipyretic and antisplasmodial properties comparable to those of quinine (Ghisalberti 2000). Topical application of ointments made with ethanolic extracts of leaves of Senna alata, L. camara and Mitracarpus scaber, on chronic crusty or acute lesions of dermatophilosis, induces healing of the disease and provoked the falling off of the crusts after 3–4 days of treatment. The treated areas healed without scarring and became free of dermatophilosis without recurrence for more than 3 years (Ali-Emmanuel et al 2003). Medicinal uses Traditional system/folk medicine Antiseptic; vermifuge; for treating wounds, tetanus, rheumatism, malaria; diarrhoea; diaphoretic, carminative, antispasmodic, tonic, fistula, pustules, tumours, toothache, cold, headache, uterine haemorrhage, chicken pox, eye injuries, whooping cough, asthma (Tabuti 2008) (Kumar et al 2006; (Hernandez et al 2003; CSIR 1962 a,b; Chopra et al 1956; Agarwal 1997); bronchitis, ulcers and as a vermifuge; leprosy and scabies. 38 Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Antibacterial; antifungal, immunosuppressive; antitumor; insecticidal, antipyretic and antispasmodic; antiasthmatic; antispasmodic; antiovipositional and antifeedant activity (Mahato et al 1994). Precautions and toxicology The plant causes hepatotoxicity and photosensitization in grazing animals (Mahato et al 1994). Symptoms of poisoning in cattle, sheep, buffalo and guinea pigs include cholestasis, obstructive jaundice, photosensitization and a rise in serum bilirubin (Sharma et al 1980, 1981a; Seawright and Alien 1972). Hydroalcoholic extract from L. camara induced embryotoxicity in rats (Mello et al 2005). Contraindications None known Adverse effects None reported in humans Dosage form Decoction; tincture Posology or recommended dose Decoction: 40 g in1 litre of water; drink 4 cups daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily References Agarwal VS (1997). Drug plants of India, vol. II. Ludhiana: Kalyani Publishers, 1997:426. Ali-Emmanuel N, Moudachirou M, Akakpo JA, Quetin-Leclercq J (2003). Treatment of bovine dermatophilosis with Senna alata, Lantana camara and Mitracarpus scaber leaf extracts. Journal of Ethnopharmacology 86, 167-171. Chopra RN, Nayar SL, Chopra IC (1956). Glossary of Indian medicinal plants. New Deli: CSIR, 149. CSIR (1962a). Weath of India, vol. VI. Council of Scientific and Industrial Directorate, New Delhi, 31. CSIR (1992b). The useful plants of India. Publication and Information Directorate, CSIR, New Delhi, 316. Deena MJ, Thoppil JE (2000). Antimicrobial activity of the essential oil of Lantana camara. Fitoterapia 71, 453-455. Ghisalberti EL (2000). Lantana camara L (Verbenaceae). Fitoterapia 71, 467-486 Hernandez T, Canales M, Avila JG, Duran A et al (2003). Ethnobotany and antibacterial activity of some plants used in traditional medicine of Zapotitlan de las Salinas, Puebla (Mexico). Journal of Ethnopharmacology 88, 181-188. Ioset JR, Marston A, Gupta MP, Hostettmann K (2000). Antifungal and larvicidal cordiaquinones from the roots of Cordia curassavica. Phytochemistry 53, 613-617. Kumar VP, Chauhan NS, Padh H, Rajani M (2006). Search for antibacterial and antifungal agents from selected Indian medicinal plants. Journal of Ethnopharmacology 107, 182-188. 39 Mabato SB, Sabu NP, Roy SK, Sharrna OP (1994). Potential Antitumor Agents from Lantana camara: Structures of Flavonoid- , and Phenylpropanoid Glycosides. Tetrahedron 50(31): 9439-9446 Magassouba FB, Diallo A, Kouyaté M, Mara F et al (2007). Ethnobotanical survey and antibacterial activity of some plants used in Guinean traditional medicine. Journal of Ethnopharmacology 114, 44-53. Mello FB, Jacobus D, Carvalho K, Mello JRB (2005). Effects of Lantana camara (Verbenaceae) on general reproductive performance and teratology in rats. Toxicon 45, 459-466 Misra L, Laastsch H (2000). Triterpenoids, essential oil and photooxidative 28-13-lactonization of oleanolic acid from Lantana camara. Phytochemistry 54, 969–974. Saxena RC, Dixit OP, Harshan V (1992). Insecticidal action of Lantana camara against Callosobruchus chinensis (Coleoptera: Bruchidae). Journal of Stored Prod. Research 28(4): 279-281. Seawright AA, Alien JG (1972) Pathology of the liver and kidney in lantana poisoning of cattle. Aust. Veterinary Journal 48, 325. Sharma OP, Makkar HPS, Pal RN, Negi SS (1980) Lantadene A content and toxicity of the lantana plant (Lantana camara Linn) to guinea pigs. Toxicon 18, 485. Sharma OP, Makkar HPS, Dawra RK, Negi SS (1981a). A review of the toxicity of Lantana camara (Linn) in animals. Clinical Toxicology 18, 1077 Tabuti JRS (2008). Herbal medicines used in the treatment of malaria in Budiope County, Uganda. Journal of Ethnopharmacology 116, 33-42 Footnotes: 1. Tropical Herbal Mixture _____________________________________________ Mangifera indica Botanical name Mangifera indica L. cv. Tommy Atkins Local name(s) Mango Chemical constituents Polyphenols, carotenoids, vitamin E and vitamin C (Ajila et al 2007a); flavonoids, tannins, steroids, triterpenes Pharmacology Many of the pharmacological properties of mango fruit and stem bark of mango may be attributed to the presence of phytochemicals such as polyphenols, carotenoids, vitamins, etc. (Nunez-Selles et al 2000; Singh et al 2004). M. indica has been reported to possess antiviral, antibacterial and anti-inflammatory activities. In the present study, the alcoholic extract of stem bark of M. indica, containing mangiferin 2.6%, exhibited immunostimulant properties (Makare et al 2001). Mango peel extracts protected erythrocytes against oxidative stress (Ajila and Rao 2008). Mango polyphenols and carotenoids possess antioxidant (Berardini et al 2004; Talcott et al 2005; Mahattanatawee et al 2006), immunomodulatory (Naved et al 2005) antimutagenic (Botting et al 1999) and anticancer activities (Percival et al 2006). Aqueous stem bark extract from selected species of mango, which was used in pharmaceutical formulations under the brand name of Vimang, has been reported to display a potent in vitro and in vivo antioxidant and anti-inflammatory activity (Sanchez et al 2000; Garrido et al 2004; Rodriguez et al 2006; Pardo-Andreu et al 2006). Mangiferin has been reported to possess anti-inflammatory activity and also displays a high antibacterial activity against Gram-positive bacteria (Leiro et al 2003). The bioactivities of mangiferin are 40 mediated by systemic antioxidant/antiradical functions and immunomodulation (Cholbi et al 1991) property. M. indica extract has shown a dose-dependent antispasmodic effect (Agbonon et al 2002). Aqueous decoction of the flowers showed potential gastroprotective and ulcer-healing properties in vivo (Lima et al 2006). Aqueous extract of M. indica leaves has been reported to possess hypoglycemic activity in glucose-induced hyperglycaemic rats as well as in mice (Aderibigbe et al 1999; 2001). Mangiferin possesses significant antidiabetic, antihyperlipidemic and antiatherogenic properties thus suggesting its beneficial effect in the treatment of diabetes mellitus associated with hyperlipidemia and related cardiovascular complications (Muruganandan et al 2005). It also protected mice against the radiation-induced sickness and mortality (Jagetia and Baliga 2005). Medicinal uses Traditional system/folk medicine Vermifuge; antidiarrhoeal; antimicrobial; anticancer; antidiabetic, antioxidant, antiproliferative, immunomodulatory; antioxidant; cardiotonic; diuretic; for the treatment of fever, gastritis, ulcers; immunodeficiency diseases such as arthritis, diabetes, hepatitis, cardiac and mental disorders and as a gargle to treat swollen gums (Agbonon et al 2002; Robineau 1995; Sanchez et al 2000; Andreu et al 2005; Ghosal et al 1996; Leiro et al 2003). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Antiviral, antibacterial; anti-inflammatory; antioxidant; immunostimulant; gastroprotective; ulcer-healing; antidiabetic, antihyperlipidemic and antiatherogenic Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Decoction; tincture Posology or recommended dose Decoction: 40 g in1 litre of water; drink 4 cups daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily References Aderibigbe AO, Emudianughe TS, Lowal BA (1999). Antihyperglycemic effect of Mangifera indica in rat. Phytotherapy Research 13, 504–507. Aderibigbe AO, Emudianughe TS, Lowal BA (2001). Evaluation of antidiabetic action of Mangifera indica in mice. Phytotherapy Research 15, 456-458. 41 Agbonon A, Eklu-Gadegbeku K, Aklikokou K, Essien K et al (2002). The effects of Mangifera indica stem bark and Pluchea ovalis roots on tracheal smooth muscle in vitro. Fitoterapia 73, 619–622 Ajila CM, Rao UJSP (2008). Protection against hydrogen peroxide induced oxidative damage in rat erythrocytes by Mangifera indica L. peel extract. Food and Chemical Toxicology 46, 303–309 Ajila CM, Bhat SG, Prasada Rao UJS (2007a). Valuable components of raw and ripe peels from two Indian mango varieties. Food Chemistry 102, 1006-1011. Andreu GP, Delgado R, Velho JA, Curti C et al (2005). Iron complexing activity of mangiferin, a naturally occurring glucosylxanthone, inhibits mitochondrial lipid peroxidation induced by Fe(2+)-citrate. European Journal of Pharmacology 513, 47-55. Berardini N, Carle R, Schieber A (2004). Characterization of gallotannins and benzophenone derivatives from mango (Mangifera indica L. cv. Tommy Atkins) peels, pulp and kernels by high-performance liquid chromatography/electrospray ionization mass spectrometry. Rapid Communications in Mass Spectrometry 18, 2208– 2216. Botting KJ, Young MM, Pearson AE, Harris PJ et al (1999). Antimutagens in food plants eaten by Polynesians: Micronutrients, physiochemical and protection against bacterial mutagenicity of the heterocyclic amine 2-amino-3-methylimidazo (4,5-f)quinoline. Food and Chemical Toxicology 37, 95–103. Cholbi MR, Paya M, Alcaraz MJ (1991). Inhibitory effect of phenolic compounds on CCl4-induced microsomal lipid peroxidation. Experientia 472, 195-199 . Garrido G, Gonźalez D, Lemus Y, Garcia D et al (2004). In vivo and in vitro anti-inflammatory activity of Mangifera indica L. extracts (VIMANG). Pharmacology Research 50, 143-149. Ghosal S, Rao G, Saravanan V, Misra N et al (1996). A plausible chemical mechanism of the bioactivities of mangiferin. Indian Journal of Chemistry 35, 561-566. Jagetia GC, Baliga MS (2005). Radioprotection by mangiferin in DBAxC 57BL mice: a preliminary study. Phytomedicine 12, 209-215. Leiro JM, Alvarez E, Arranz JA, Siso IG et al (2003). In vitro effects of mangiferin on superoxide concentrations and expression of the inducible nitric oxide synthase, tumour necrosis factor-alpha and transforming growth factor-beta genes. Biochemical Pharmacology 65, 1361-1371. Lima ZP, Severi JA, Pellizzon CH, Brito ARMS et al (2006). Can the aqueous decoction of mango flowers be used as an antinuclear agent? Journal of Ethnopharmacology 106, 29-37 Makare N, Bodhankar S, Rangari V (2001). Immunomodulatory activity of alcoholic extract of Mangifera indica L. in mice. Journal of Ethnopharmacology 78, 133-137 Muruganandan S, Srinivasan K, Gupta S, Gupta PK et al (2005). Effect of mangiferin on hyperglycemia and atherogenicity in streptozotocin diabetic rats. Journal of Ethnopharmacology 97, 497-501. Naved T, Siddiqui JI, Ansari SH, Ansari AA et al (2005). Immunomodulatory activity of Mangifera indica L.. Journal of Natural Remedies 5, 137–140. Nunez-Selles AJ, Velez-Castro H, Aguero-Aguero J, Gonzalez-Gonzalez J et al (2000). Isolation and quantitative analysis of phenolic constituents, free sugars, fatty acids and polyols from mango (Mangifera indica L.), stem bark aqueous decoction used in Cuba as nutritional supplement. Journal of Agricultural and Food Chemistry 50, 762-766. Percival SS, Talcott ST, Chin ST, Mallak AC et al (2006). NeoplasticTransformation of BALB/3T3 cells and cell cycle of HL-60 cells are inhibited by mango (Mangifera Indica L.) Juice and mango juice extracts. The Journal of Nutrition 136, 1300-1304. Robineau LG (1995). Hacia una Farmacopea Caribeña. Enda-Caribe, Santo Domingo, 351-353. Rodriguez J, Pierro DD, Gioia M, Monaco S et al et al (2006). Effects of natural extract from Mangifera indica L., and its active compound, mangiferin, on energy state and lipid peroxidation of red blood cells. Biochemica et Biophysica Acta 1760, 1333-1342. Sanchez GM, Re L, Giuliani A, Nunez-Selles A et al (2000). Protective effects of Mangifera indica L. extract mangiferin and selected antioxidants against TPA-induced Bio-molecules oxidation and peritoneal macrophage activation in mice. Pharmacology Research 42, 565-573. Singh UP, Singh DP, Singh M, Maurya S et al (2004). Characterization of phenolic compounds in some Indian mango varieties. International Journal of Food Science and Nutrition 55, 163-169. Footnotes: 1. Yaakson Mixture ____________________________________________ Ocimum basilicum 42 Botanical name Ocimum basilicum Local name(s) Basil Chemical constituents Essential oil (linalool, epi-α-cadinol, α-bergamotene, γ-cadinene) (Hussain et al 2008); sesquiterpenes; flavonoids (Bruneton 1999) Suggested method of standardisation Not available Pharmacology Numerous laboratory studies have the diverse pharmacological effects of Ocimum sp. These include bactericidal, Antiinflammatory, antioxidant, antinuclear, Antidiarrheal, Chemopreventive, hypoglycaemic, nervous system stimulatory and radioprotective (Klem et al 2000; Maity et al 2000; Prakash and Gupta 2000; Uma Devi et al 2000; Chattopadhyay 1999; Offiah and Chikwendu 1999). The Chemomodulatory effect of O. Basilicum leaf extract on drug metabolizing and antioxidant enzymes has been reported (Dasgupta et al 2004). Basil essential oil possesses antimutagenic properties comparable to that obtained with the antioxidant vitamin E (Berić et al 2008). The essential oils exhibited good antioxidant and antimicrobial activity in vitro (Hussain et al 2008). O. basilicum essential oils showed insect repellent activity (Erler et al 2006). The powdered aerial parts of O. basilicum and its aqueous and methanolic extracts had antiulcerogenic properties. The methanolic extract decreased the acid output and enhanced hexosamine secretion (Akhtar and Munir 1989). The methanol extracts appeared to be highly toxic to the larvae of Egyptian cotton worm (Pavela 2004). A leaf-extract of O. basilicum was used in formulating an aerosol and mosquito coil, and their efficacy tested against adult mosquitoes. The efficacy of the formulations depended on the duration of fumigation (Umerie et al 1998). Medicinal uses Traditional system/folk medicine Antiseptic; preservative, mild sedative, digestive, diuretic; carminative, galactogogue, stomachic; antispasmodic; for the treatment of headaches, coughs, infections of upper respiratory tract and kidney malfunction (Sajjadi 2006; Tucakov 1996). Uses as described in pharmacopoeia None Uses supported by experimental or clinical data Antioxidant; bactericidal; anti-inflammatory; antioxidant; antinuclear; Antidiarrheal; Chemopreventive, hypoglycaemic, nervous system stimulatory; radioprotective; insecticidal; insect repellent; antimutagenic Precautions and toxicology Not available Contraindications Not available Adverse effects Not available 43 Dosage form Decoction; infusion; tincture; essential oil Posology or recommended dose Decoction: 30 g dried leaves in 900 ml water; simmer until reduced to 600 ml; 1 teacup three times daily Infusion: 30g dried herb in 600 ml of water; 1 teacupful three times a day Tincture: 1:5 in 50% alcohol, 5 ml three times daily Essential oil: 2-3 drops three times daily References Akhtar MS, Munir M (1989). Evaluation of the gastric antiulcerogenic effects of Solanum nigrum, Brassica oleracea and Ocimum basilicum in rats. Journal of Ethnopharmacology 27, 163-176. Berić T, Nikolić B, Stanojević J, Vuković-Gačić B et al (2008). Protective effect of basil (Ocimum basilicum L.) against oxidative DNA damage and mutagenesis. Food and Chemical Toxicology 46, 724-732 Bruneton J (1999). Pharmacognosy phytochemistry medicinal plants. Paris; Lavoiser Chattopadhyay RR (1999). A comparative evaluation of some blood sugar lowering agents of plant origin. Journal of Ethnopharmacology 67, 367-372. Dasgupta T, Rao AR, Yadava PK (2004). Chemomodulatory efficacy of Basil leaf (Ocimum basilicum) on drug metabolizing and antioxidant enzymes, and on carcinogen-induced skin and forestomach papillomagenesis. Phytomedicine 11, 13-151. Erler F, Ulug I, Yalcinkaya B (2006). Repellent activity of five essential oils against Culex pipiens. Fitoterapia 77, 491-494 Hussain AI, Anwar F, Sherazi STH, Przybylski R (2008). Chemical composition, antioxidant and antimicrobial activities of basil (Ocimum basilicum) essential oils depend on seasonal variations. Food Chemistry 108, 986-995 Klem MA, Nair MG, Sraassburg GM, Dewitt DL (2000). Antioxidant and cyclooxygenase inhibitory phenolic compounds from Ocimum sanctum Linn. Phytomedicine 7, 7-13. Maity TK, Mandal SC, Saha BP, Pal M (2000). Effect of Ocimum sanctum roots extract on swimming performance in mice. Phytotherapy Research 14, 120-121. Offiah VN, Chikwendu UA (1999). Antidiarrheal effects of Ocimum gratissimum leaf extract in experimental animals. Journal of Ethnopharmacology 68, 327-330. Pavela R (2004). Insecticidal activity of certain medicinal plants. Fitoterapia 75, 745- 749. Prakash J, Gupta SK (2000). Chemopreventive activity of Ocimum sanctum seed oil. Journal of Ethnopharmacology 72, 29-34. Sajjadi SE (2006). Analysis of the essential oils of two cultivated basil (Ocimum basilicum L.) from Iran. Daru, 14(3): 128-130. Tucakov J (996). Lečenje Biljem, 6th ed. In: Fitoterapija Rad, Beograd,. 247–248. Uma Devi P, Ganasoundri A, Vindra B, Srinivasan KK (2000). Radiation protection by the Ocimum flavonoids orientin and vicenin: mechanism of action. Radiat. Res. 154, 455-460. Umerie SC, Anaso HU, Anyasoro LJC (1998). Insecticidal Potentials of Ocimum Basilicum Leaf-extract. Bioresource Technology 64, 237-239 Footnotes: 1. Power My Power _______________________________ 44 Parinari polyandra Botanical name Parinari polyandra Local name(s) Not available Chemical constituents Flavonoids, tannins, and saponin glycoside. Pharmacology The methanolic extract of the stem bark of P. polyandra had significant anti-nociceptive effect in mice and rats. The extract also exhibited anti-inflammatory (Vongtau et al 2004) and hypoglycaemic effects (Vongtau et al 1997). Medicinal uses Traditional system/folk medicine Antiinflammatory; antimalarial; blood tonic, cardiac stimulant; wounds or fractures; fever; tooth ache; diabetes mellitus; eye lotion for inflamed, painful (Vongtau et al 1997; Lewis and Elvin-Lewis 1977; Dalziel 1937). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Antinociceptive; anti-inflammatory; hypoglycaemic Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Decoction; infusion; tincture Posology or recommended dose Decoction: 30 g in 900 ml water; simmer until reduced to 600 ml; 1 teacup three times daily Tincture: 1:5 in 50% alcohol, 5 ml three times daily References Dalziel JM (1937). The Useful Plants of West Tropical Africa. Crown Overseas Agents for the Colonies and Administration, London, 168-170. Lewis WH, Elvin-Lewis PF (1977). Medical Botany: Plants Affecting Man’s Health. Wiley, New York, 226–235. 45 Vongtau HO, Abbah J, Ngazal IE, Kunle OF et al (2004). Anti-nociceptive and anti-inflammatory activities of the methanolic extract of Parinari polyandra stem bark in rats and mice. Journal of Ethnopharmacology 90, 115–121 Vongtau HO, Osunkwo UA, Okwuasaba F, Gamaniel KS et al (1997). Potential antidiabetic activity of extracts of Parinari polyandra. Journal of Pharmaceutical Research and Development 2, 33–37. Footnotes: 1. Power My Pow ___________________________ Momordica charantia Botanical name Momordica charantia Linn. Local name(s) Nyinya (Twi); nyanya (Fante); kakle (Ewe); daddagu (Hausa) Chemical constituents Alkaloid (momordicine); vitamin C; fatty acid; γ-aminobutyric acid; charantin; volatile oil; carotenoids (cryptoxanthin, ß-carotene); cucurbitacins, saponins; carbohydrates; rosmarinic acid Pharmacology Experimental pharmacology M. charantia has been reported to possess antilipolytic (Ng et al 1987), analgesic (Biswas et al 1991), abortifacient (Ng et al 1988), antiviral (Lee-Huang et al 1995), cytotoxic (Porro et al 1995), hypoglycaemic (Shabib et al 1993) and antimutagenic (Guevara et al 1990) properties. The glycoproteins, α- and β-momorcharins are thought to play a crucial role in the plant’s diverse pharmacological properties, (Ng et al, 1992). The alcoholic extract of the pulp of M. charantia demonstrated antidiabetic activity (Sarkar et al 1996). In vitro studies have found the leaf extract to possess immunostimulant as well as broad-spectrum antimicrobial effects (Derrida, htpp://www.mdidea.com/products/herbextract/bittermelon/data.html). Leaves of M. charantia have been found to possess antibacterial effects against E. coli and Staphylococcus aureus (Georges and Pandelai, 1949), while the fruit extract exhibited antibacterial properties against Helicobacter pylori. The proteins α- and β-Momorcharins have been reported to inhibit HIV virus in vitro. Male Antifertility properties have been observed in the fruit; an ethanol extract caused a decrease in testicular weights and sperm production in gerbils and dogs (Hanna et al 1981). Roots have anti-abortifacient effects in females (Jamwall and Anand, 1964). Certain isolated compounds of the herb showed anticancer and antitumor properties. In vitro antitumor activity of ribosome inactivating protein MAP30 of Momordica has also been observed to be effective against certain tumor cell lines (Rybak et al 1994). The compound momordicin demonstrated cytotoxic activity against Hodgkin’s lymphoma in vivo. In one study, an aqueous extract blocked the growth of rat prostate carcinoma and a hot aqueous extract of the entire plant inhibited the development of mammary tumours in mice (Derrida, htpp://www.mdidea.com/products/herbextract/bittermelon/data.html). Clinical pharmacology The fruit juice of M. charantia was found to significantly improve the glucose tolerance of patients with maturity onset diabetes (Welihinda et al 1986). p-Insulin showed hypoglycaemic activity (Khanna et al 1974; 1976; 1981; Best et al. 1924; Ng et al 1986; Welihinda et al 1986). Several small-scale studies have reported decreases in blood 46 glucose levels and/or improvements in the glucose-tolerance tests of diabetic patients, who received various doses of bitter melon fruit, juice, or powder (Welihinda et al 1986). Medicinal uses Traditional system/folk medicine Infectious diseases; malaria; diabetes; abdominal pains; wounds; hypertension; fever Uses as described in pharmacopoeia Arterial hypertension; abdominal pains; wounds and burns; cancer; contraception; dermatitis; diabetes; dracontiasis; fever; HIV/AIDS; infectious diseases; malaria; measles; otitis; skin rashes; whitlow (Mshana et al 2000; GHP 1992; Dennis 2002). Uses supported by experimental or clinical data Antilipolytic; analgesic; abortifacient; antiviral; cytotoxic; hypoglycaemic; antimutagenic; antitumor Precautions and toxicology Not available Contraindications Genetic erythrocytic deficiency of glucose 6-phosphate dehydrogenase; pregnancy and lactation Adverse effects Abortifacient Antifertility effects Hypoglycaemic coma and convulsions Dosage form Decoction; infusion; tincture; tablets; capsules Posology or recommended dose Decoction: 30 g dried aerial parts in 900 ml water; simmer until reduced to 600 ml; 1 teacup three times daily Infusion: 30 g dried aerial parts in 600 ml of water; 1 teacup three times daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily Capsules: 1-2 g of powdered leaf, 1 capsule two times daily References Best CH, Smith RG, Scott DA (1924). An insulin-like material in various tissues of the normal and diabetic animal. Amer. J. Physiol. 68:161-182. Biswas AR, Ramaswamy S, Bapna JS (1991). Analgesic effect of Momordica charantia seed extract in mice and rats. Journal of Ethnopharmacology 31, 115–118. Dennis, F. (Ed). Manual for the propagation of medicinal plants in Ghana. Darwin Initiative for the Survival of Species. Derrida, M. What is Bitter Melon (Momordica charantia): What is Bitter Melon used for today? htpp://www.mdidea.com/products/herbextract/bittermelon/data.html 47 Ghana Herbal Pharmacopoeia (1992), 95-98, The Advent Press: Accra, Ghana Georges, M. and Pandelai, K.M. (1949). Investigation on plant antibiotics IV. Further search for antibiotic substances in Indian Medicinal plants. Indian J Med Res., 37, 169-181; cited by Oliver-Bever, 1986. Guevara AP, Lim-Sylianco C, Dayrit F, Finch P (1990). Antimutagens from Momordica charantia. Mutat. Res. 230, 121–126. Jamwall, K.S. and Anand, N.K. (1964). Preliminary screening of some reputed abortifacient indigenous plants. Indian J Med Res., 24, cited by Oliver-Bever, 1986. Khanna, P., Nag, T.N., Jain, S.C. and Mohan, S. (1974). Extraction of insulin from a plant source. 3rd International Congress on Plant Tissue & Cell Cultures, 21-26th July, Leicester, UK. Mshana, N.R., Abbiw, D.K., Addae-Mensah, I., Ahiyi, M.R.A., Ekper, J.A., et al., (2000). Traditional medicine and pharmacopoeia. Contribution to the revision of Ethnobotanical and Floristics Studies of Ghana. Organisation of African Unity/Scientific, technical and research committee. Ng TB, Wong CM, Li WW, Yeung HW (1986) Insulin-like molecules in Momordica charantia seeds. J. Ethnopharmacol. 15:107-117. Lee-Huang S, Huang PL, Huang PL, Bourinbaiar AS et al (1995). Inhibition of the integrase of human immunodeficiency virus (HIV) type 1 by anti-HIV plant proteins MAP30 and GAP31. Proc. Natl. Acad. Sci. USA 92, 8818–8822. Ng TB, Wong CM, Li WW, Yeung HW (1987). Peptides with antilipolytic and lipogenic activities from seeds of the Bitter Gourd Momordica charantia (family cucurbitaceae). General Pharmacology 18, 275-281. Ng TB, Tam PP, Hon WK, Choi HL et al (1988). Effects of Momorcharins on ovarian response to gonadotropin-induced super ovulation in mice. Int. J. Fertil. 33, 123– 128. Ng TB, Chan WY, Yeung HW (1992). Proteins with abortifacient, ribosome inactivating, immunomodulatory, antitumor and anti-AIDS activities from cucurbitaceae plants. General Pharmacology 23, 579–590. Porro G, Lento P, Marcucci F, Gromo G et al (1995). Different cytotoxic activity and intracellular fate of an anti-CD5-momordin immunotoxin in normal compared to tumor cells. Cancer Immunol. Immunother 40, 213–218. Rybak SM, Lin JJ, Newton DL, et al (1994). In vitro anti-tumor activity of the plant ribosome inactivating proteins MAP30 and GAP31. International. Journal of Oncology 5, 88–94. Sarkar, S., Pranava, M. and Marita, R. (1996). Demonstration of the hypoglycaemic action of Momordica charantia in a validated animal model of diabetes. Pharmacol Res., 33: 1-4. Shabib BA, Khan LA, Rahman R (1993). Hypoglycaemic activity of Coccinia indica and Momordica charantia in diabetic rats: depression of the hepatic gluconeogenic enzymes glucose-6-phosphatase and fructose-1,6-biphosphatase and elevation of both liver and red-cell shunt enzyme glucose-6-phosphate dehydrogenase. Biochem. J. 292, 267–270. Welihinda J, Karunanayake EH, Sheriff MH, Jayasinghe KS (1986) Effect of Momordica charantia on the glucose tolerance in maturity onset diabetes. J Ethnopharmacol, 17(3): 277-82. Footnotes: 1. Krobo Fever Eduro _______________________________________________ Tabernaemontana crassa Botanical name Tabernaemontana crassa Local name(s) Not available Chemical constituents Tannins, saponins, alkaloids (ibogaine, conopharyngine), glycosides, fixed oil and proteins (Agwu and Akah 1990). 48 Pharmacology Hot water extract of T. crassa leaves appears to contain pharmacologically active compounds with local doserelated, reversible anaesthetic properties. The ability of the extract to cause both infiltration and nerve block anaesthesia is very desirable (Agwu and Akah 1990). The ethanolic stem bark extract of the plant showed significant activity against gram-positive bacteria and weak activity against gram negative bacteria (Van Beek et al 1985). Medicinal uses Traditional system/folk medicine Wound disinfectant; ringworm infestation; fever; wound disinfectant; local anaesthetic (especially bone resetting) ((Iwu 1982; Irvine 1961; Oliver 1960; Cooper and Record 1931). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Local anaesthetic; antibacterial Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Decoction: 30 g of dried plant part in 900 ml water; simmer until reduced to 600 ml; 1 teacup three times daily Infusion: 30 g dried, powdered plant part in 600 ml of water; 1 teacup three times daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily References Agwu IE, Akah PA (1990). Tabernaemontana crassa as a traditional anesthetic agent. Journal of Ethnopharmacology 30, 115-119 Cooper GB, Record SJ (1931). The Evergreen Forest of Liberia. Yale University School of Forestry, New Haven 31. Irvine FR (1961). Woody Plants of Ghana with Special Reference to Their Uses. Oxford University Press, London, 463. Iwu MM (1982). Perspective of Igbo tribal ethnomedicine. Ethnomedicine 7, 31-45. Oliver B (1960). Medicinal Plants in Nigeria. Nigerian College of Arts, Science and Technology, Ibadan, 23. 49 Van Beek TA, De Smidt C, Verpoorte R (1985). Photochemical investigation of Tabernaemontana crassa. Journal of Ethnopharmacology 14, 315-318 Footnotes: 1. Malamixture ___________________________ Trema orientalis Botanical name Trema orientalis Local name(s) Not available Chemical constituents Triterpenoid alcohols (trematol, simiarenol, sitosterol), simiarenone (Obafemi et al 1979; Ogunkoya et al 1977). Pharmacology No pharmacological data exists Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References Obafemi CA, Ogunkoya L, Quartey JAK, Waight ES (1979). Structure of the triterpenoid alcohol trematol. Phytochemistry 18, 496-497 50 Ogunkoya L, Olubajo OO, Sondha (1977). A new triterpenoid alcohol from Trema orientalis. Photochemistry 16, 1606-1608. Foot notes: 1. Golden Malacure Monographs on Medicinal Plants for Miscellaneous Conditions of Public Health Importance 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. Ipomea species Witheria indica Sorghum bicolor Ageratum conyzoides Desmodium adscendens Zanthoxyllum xanthoxyloides Phyllanthus niruri Solanum torvum Rauwolfia vomitoria Spiropetalum heterophyllum Kigelia africana Alstonia boonei Morinda lucida Oxytenanthera abyssinica Tipananthus bangwensis Spathodea campanulata Azadirachta indica Carica papaya Baphia nitida Clausena anisata Alchornea cordifolia Cryptolepis sanguinolenta Khaya senegalensis Nauclea latifolia Piliostigma thonningii Trichilia monadelpha Strophanthus hispidus Piper guineense Eugenia caryophyllata Xylopia aethiopica Monodora myristica Capsicum frutescens Anthocleista nobilis Lecaniodiscus cupanioides Dalium guineense Treculia africana Zingiber officinale Eugenia caryophyllata Balanites aegyptiaca Cassia occidentalis Momordica charantia Cassia alata Rauwolfia vomitoria Theobroma cacao Persea itrates 51 46. Olea europea 47. Pascartina ngonnyukpa 48. Kontu glabriflorum 49. Leonurus cardiaca 50. Mangifera indica 51. Corynanthe pachyceras 52. Parinari robusta 53. Muur ___________________________ Ipomea batatas Botanical name Ipomea batatas (L) Lam) Local name(s) Not available Chemical constituents Proteins; fibre; phytates, oxalates and tannins (Oboh et al 1989), phytosterol, complex carbohydrates and sugars. Suggested method of standardisation Not available Pharmacology There appears to be no pharmacological data on the medicinal properties of sweet potato although its forage has been shown to be an effective protein supplement for animals (Aregheore 2004). Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Adverse effects Not available Dosage form Not available Posology or Not available 52 Contraindications Not available Recommended dose Not available References Aregheore EM (2004). Nutritive value of sweet potato (Ipomea batatas (L) lam) forage as goat feed: voluntary intake, growth and digestibility of mixed rations of sweet potato and batiki grass (Ischaemum aristatum var. indicum). Small Ruminant Research 51, 235-241. Oboh S, Ologhobo A, Tewe O (1989). Some Aspects of the Biochemistry and Nutritional Value of the Sweet Potato (Ipomea batatas). Food Chemistry 31, 9-18. ______________________________________ Waltheria indica Botanical name Waltheria indica Local name(s) Not available Chemical constituents Minerals (Zn, Cu, Mn, Rb, Sr, Na and K) (Gandhi and Aswathanarayana 1975). Suggested method of standardisation Not available Pharmacology No studies on its medicinal applications have been reported in published literature. Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available 53 Dosage form Not available Posology or recommended dose Not available References 1. Gandhi SM, Aswathanarayana U (1975). A possible base-metal indicator plant from Mamandur, South India. Journal of Geochemical Exploration 4, 247250. ____________________________ Sorghum bicolor Botanical name Sorghum bicolor (L.) moench Local name(s) Great millet and guinea corn Chemical constituents Alkaloids, saponins ; phytates, phenols, tannins, trypsin inhibitory factors, fibre; proteins; carbohydrates; saturated and unsaturated fatty acids (Mehmood et al 2008; Oladiji et al 2007; Hegde and Chandra 2005). Suggested method of standardisation Methods of standardisation of plant extracts have been extensively covered in Nyarko et al (2005). Pharmacology Aqueous stem bark extracts of S. bicolor at the doses of 200, 400 and 800 mg/kg body weight showed anti-anaemic properties in iron deficient weaning rats (Oladiji et al 2007). Antioxidant activity of the methanolic extracts has been demonstrated in vitro (Hegde and Chandra 2005). The peptide designated 2 kD peptide obtained from S. bicolor, strongly inhibited the replication of herpes simplex virus type 1 (HSV-1) in a dose-dependent manner. The peptide also had an in vitro prophylactic effect against HSV-1 infection (Filho et al 2008). The decoction S. bicolor exhibited membrane stabilizing activity in vitro and could therefore help to stabilize red blood cells from stress injury (Falade et al 2005). Klopfenstein et al (1981) reported a cholesterol-lowering effect of low-tannin sorghum grain when fed to guinea pigs at 58% of diet and Cho et al (2000) observed that feeding rats with whole sorghum, proso millet or buckwheat caused increased fecal bile acid excretion and HDL cholesterol levels without a change in total cholesterol. However, Rooney et al (1992) found that both high-tannin and non-tannin sorghums as well as wheat bran increased blood serum total cholesterol in rats. Lee and Pan (2003) have also shown that dietary tannin-sorghum distillery residues had antioxidant activity by their ability to inhibit hemoglobin-catalyzed oxidation of linoleic acid and significantly improve blood-thinning and erythrocyte membrane integrity of the fish blood cells during winter. There have been several reports on reduced weight gain of animals fed high tannin sorghum (Cousins et al 1981; Lizardo et al 1995; Al-Mamary et al 2001; Muriu et al 2002). In vitro studies have also revealed anti-carcinogenic properties of sorghum. Grimmer et al. (1992) demonstrated anti-mutagenicity of sorghum polyphenol extracts. Medicinal uses Traditional system/folk medicine Anaemia (Oladiji et al 2007). 54 Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Anti-oxidant; anti-anaemic; anti-cholesterolemic; aniviral; anti-carcinogenic; anti-obesity; anticoagulant. Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References Al-Mamary M, Al-habori M, Al-Aghbari A, Al-Obeidi A (2001). In vivo effects of dietary sorghum tannins on rabbit digestive enzymes and mineral absorption. Nutrition Research 21, 1393-1401. Cho S-H, Choi Y, Ha T-Y (2000). In vitro and in vivo effects of proso millet, buckwheat and sorghum on cholesterol metabolism. FASEB Journal 14 (4), A249. Cousins BW, Tanksley TD, Knabe DA, Zebrowska T (1981). Nutrient digestibility and performance of pigs fed sorghums varying in tannin concentration. Journal of Animal Science 53, 1524-1529. Falade OS, Otemuyiwa IO, Oladipo A, Oyedapo OO et al (2005). The chemical composition and membrane stability activity of some herbs used in local therapy for anemia. Journal of Ethnopharmacology 102, 15-22. Filho IC, Cortez DAG, Ueda-Nakamura T, Nakamura CV et al (2008). Antiviral activity and mode of action of a peptide isolated from Sorghum bicolor. Phytomedicine 15, 202-208. Grimmer HR, Parbhoo V, McGarth RM (1992). Antimutagenicity of polyphenol-rich fractions from Sorghum bicolor grain. Journal of Agricultural and Food Chemistry 59, 251-256. Hegde PS, Chandra TS (2005). ESR spectroscopic study reveals higher free radical quenching potential in kodo millet (Paspalum scrobiculatum) compared to other millets. Food Chemistry 92, 177-182 Lee SM, Pan BS (2003). Effects of dietary sorghum distillery residue on hematological characteristics of cultured grey mullet (Mugil cephalus) – an animal model for prescreening antioxidant and blood thinning activities. Journal of Food Biochemistry 27, 1-18. Lizardo R, Peiniau J, Aumaitre A (1995). Effect of sorghum on performance, digestibility of dietary-components and activities of pancreatic and intestinal enzymes in the weaned piglet. Animal Feed Science and Technology 56, 67-82. Mehmood S, Orhan I, Ahsan Z, Aslan S et al (2008). Fatty acid composition of seed oil of different sorghum bicolor varieties, Food Chemistry (2008), doi: 10.1016/j.foodchem.2008.01.014 Muriu JI, Njoka-Njiru EN, Tuitoek JK, Nanua JN (2002). Evaluation of sorghum (Sorghum bicolor) as replacement for maize in the diet of growing rabbits (Oryctolagus cuniculus). Asian-Australian Journal of Animal Science 15, 565-569. Nyarko AK, Asiedu-Gyekye IJ, Sittie AA (2005). A manual of harmonised procedures for assessing the safety, efficacy and quality of plant medicines in Ghana. Yamens Press Ltd., Accra. Oladiji AT, Jacob TO, Yakubu MT (2007). Anti-anaemic potentials of aqueous extract of Sorghum bicolour (L.) moench stem bark in rats. Journal of Ethnopharmacology 111, 651-656. 55 Rooney TK, Rooney LW, Lupton JR (1992). Physiological characteristics of sorghum and millet brans in the rat model. Cereal Foods World 37, 782-786. _______________________________ Oxytenanthera abyssinica Botanical name Oxytenanthera abyssinica Local name(s) Bamboo Chemical constituents Not available Suggested method of standardisation Not available Pharmacology Pharmacological studies on this plant are very scarce Pharmacodynamics Not available Efficacy Not available Pharmacokinetics Not available Microbiology Not available Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available 56 Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References None ___________________________ Tapinanthus banguensis Botanical name Not available Local name(s) Not available Chemical constituents Not available Suggested method of standardisation Not available Pharmacology Not available Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available 57 Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References None _________________________ Eugenia caryophyllata Botanical name Eugenia caryophyllata L Local name(s) Clove Chemical constituents Eugenol, α-humulene; carvacrol; methyl salicylate, α- and β-caryophyllene, tannins (eugenin, casuarictin, tellimagrandin I) and flavonoids (quercetin and kaempferol) (Heinrich et al 2004; Yu and Hungju 1981). Suggested method of standardisation Methods of standardisation of plant extracts have been extensively covered in Nyarko et al (2005). Pharmacology E. caryophyllata has been shown to have anti-parasitic properties. The essential oil of the plant exhibited acaricidal activity in vitro and in vivo (Fichi et al 2007). Other workers have also shown the antibacterial activity of different extracts of E. caryophyllata against pathogenic bacteria (Burt and Reinders 2003; Feres et al 2005). Kurokawa et al (1995; 1998) have reported the plant’s antiviral efficacy on Herpes simplex and on Hepatitis C virus (Hussein et al 2000). The fungicidal activity of the essential oil of E. caryophyllata was demonstrated on several food-borne fungal species (Ranasinghe et al 2002; Velluti et al 2004; Lopez et al 2005), on fungi isolated from onychomicosis (Gayoso et al 2005) and on the yeast model Saccharomyces cerevisiae (Chami et al 2005). E. caryophyllata essential oil showed insect repellent properties against the mosquitoes Ades aegypti, Culex quinquefasciatus and Anopheles dirus (Trongtokit et al 2005), insecticidal activity on Pediculus capitis (Yang et al 2003), and acaricidal activity on Dermatophagoides farinae and D. pteronyssinus (Kim et al 2003). Pharmacological studies have shown the anticonvulsant activity of E. caryophyllata essential oil (Pourgholami et al 1999; Dallmeier and Carlini 1981) and anti-stress (Sen et al 1992) properties of eugenol. The effectiveness of an inhalable drug containing carvacrol in control of human seizures has also been reported (Xi et al 1994). Eugenol has been shown to possess antiinflammatory or cancer chemopreventive effects (Kim et al 2003). Pharmacodynamics No specific data exists 58 Efficacy See pharmacological studies above Pharmacokinetics An in vivo evaluation of the effect of repeated oral intake of eugenol on neuropathic pain and hyperalgesia showed that concentrations of eugenol in blood and plasma peaked rapidly with mean half lives of 14.0 and 18.3 hours, respectively ((Guénette et al 2007). Microbiology See pharmacological studies above Medicinal uses Traditional system/folk medicine Actions Antimicrobial (bacteria and fungi); antioxidant; anti-inflammatory; anticarcinogenic and antimutagenic; insect repellent; for the treatment of pain; toothache; worms; arthritis; asthma; bronchitis; rheumatism (Lawless 1995). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Antimicrobial (bacteria and fungi); antioxidant; anti-inflammatory; anticarcinogenic and antimutagenic; insect repellent Precautions and toxicology Clove oil and eugenol may be mucous membrane and dermal irritant. (Tisserand 1995). Contraindications Alcoholism, prostate cancer; haemophilia, kidney and liver disorders; anticoagulant therapy Adverse effects See precautions and toxicology above Dosage form Decoctions; tinctures; essential oil Posology or recommended dose Decoction: 30 g of plant material per litre of water. Boil for 10-15 minutes and drink a cup three times daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily Steam inhalation References Burt SA, Reinders RD (2003). Antibacterial activity of selected plant essential oils against Escherichia coli O157:H7. Letters in Applied Microbiology 36, 162-167. 59 Chami F, Chami N, Bennis S, Bouchikhi T et al (2005). Oregano and clove essential oils induce surface alteration of Saccharomyces cerevesieae. Phytotherapy Research 19, 405-408. Dallmeier K, Carlini EA (1981). Anesthetic, hypothermic, myorelaxant and anticonvulsant effects of synthetic eugenol derivatives and natural analogues. Pharmacology 22, 113-127. Fichi G, Flamini G, Giovanelli F, Otranto D et al (2007). Efficacy of an essential oil of Eugenia caryophyllata against Psoroptes cuniculi. Experimental Parasitology 115, 168-172. Feres M, Figueiredo LC, Barreto IM, Coelho MN et al (2005). In vitro antimicrobial activity of plant extracts and propolis in saliva samples of healthy and periodontally-involved subjects. Journal International Academy Periodontology 7, 90-96. Gayoso CW, Lima EO, Olivera VT, Pereira FO et al (2005). Sensitivity of fungi isolated from onichomicosis to Eugenia caryophyllata essential oil and eugenol. Fitoterapia 76, 247-249. Guénette SA, Uhland FC, Hélie P et al (2007). Pharmacokinetics of eugenol in rainbow trout (Oncorhynchus mykiss). Aquaculture 266, 262–265. Heinrich M, Barnes J, Gibbons S and Williamson EM (2004). Fundamentals of Pharmacognosy and Phytotherapy. Churchill Livingstone, London. Hussein G, Miyashiro H, Nakamura N, Hattori M et al (2000). Inhibitory effects of Sudanese medicinal plant extract on Hepatitis C virus (HCV) protease. Phytotherapy Research 14, 510-516. Kim SS, Oh O-J, Min H-Y, Park E-J et al (2003). Eugenol suppresses cyclooxygenase-2 expression in lipopolysaccharide-stimulated mouse macrophage RAW264.7 cells. Life Sciences 73, 337-348 Kim EH, Kim HK, Ahn YJ (2003). Acaricidal activity of clove bud oil compounds against Dermatophagoides farinae and Dermatophagoides pteronyssinus (Acari: Pyroglyphidae). Journal of Agricultural and Food Chemistry 51, 885-889. Kurokawa M, Nagasaka K, Hirabayashi T, Uyama S et al (1995). Efficacy of traditional herbal medicines in combination with acyclovir against Herpes simplex virus type 1 infection in vitro and in vivo. Antiviral Research 27, 19-37. Kurokawa M, Hozumi T, Basnet P, Nakano M et al (1998). Purification and characterization of eugeniin as an anti-herpes virus compound from Geum japonicum and Syzygium aromaticum. Journal Pharmacology Experimental Therapeutics 284, 728-735. Lawless J (1995). The Illustrated Encyclopedia of Essential Oils. Rockport, MA: Element Books, 59-62. Lopez P, Sanchez C, Batlle R, Nerin C (2005). Solid- and vapor-phase antimicrobial activities of six essential oils: susceptibility of selected food-borne bacterial and fungal strains. Journal of Agricultural and Food Chemistry 53, 6939-6946. Nyarko AK, Asiedu-Gyekye IJ, Sittie AA (2005). A manual of harmonised procedures for assessing the safety, efficacy and quality of plant medicines in Ghana. Yamens Press Ltd., Accra. Pourgholami MH, Kamalinejad M, Javadi M, Majzoob S et al (1999). Evaluation of the anticonvulsant activity of the essential oil of Eugenia caryophyllata in male mice. Journal of Ethnopharmacology 64, 167-171 Ranasinghe L, Jayawardena B, Abeywickrama K (2002). Fungicidal activity of essential oils of Cinnamomum zeylanicum (L.) and Syzygium aromaticum (L.) Merr et L.M. Perry against rot and anthracnose pathogens isolated from banana. Letters in Applied Microbiology 35, 208-211. Sen P, Maiti PC, Puri S (1992). Mechanism of anti-stress activity of Ocimum Sanctum Linn., eugenol and tinospora malabaria in experimental animals. Indian Journal of Experimental Biology 30, 592-596. Tisserand R 1(995). Essential Oil Safety. Churchill Livingstone: United Kingdom, 131. Trongtokit Y, Rongsriyam Y, Komalamisra N, Apiwathnasorn C (2005). Comparative repellency of 38 essential oils against mosquito bites. Phytotherapy Research 19, 303-309. Tyler VE, Brady LR, Robbers JE (1988). Pharmacognosy. Lea and Febiger, Philadelphia, 103-135. Velluti A, Sanchis V, Ramos AJ, Turon C et al (2004). Impact of essential oil on growth rate, zearalenone and deoxynivalenol production by Fusarium graminearum under different temperature and water activity condition in maize grain. Journal Applied Microbiology 96, 716-724. Xi LY, Zheng WM, Zhen SM, Xian NS (1994). Rapid arrest of seizure with an inhalation aerosol containing diazepam. Epilepsia 35, 356-358. Yang YC, Lee SH, Lee WJ et al (2003). Ovicidal and adulticidal effects of Eugenia caryophyllata bud and leaf oil compounds on Pediculus capitis. Journal of Agricultural and Food Chemistry 51, 4884-4888. Foot Notes: 60 Name of Medicine Main Indication Dua Ma Aduro Tonic Dysmenorrhoea Golden Uterovino Menstrual Disorders; Female infertility Appomens Ointment Management of Breast Pains Old Timer Tonic Gonorrhoea, Leucorrhoea, Retention of Urine __________________________ Lecaniodiscus cupanioides Botanical name Not available Local name(s) Not available Chemical constituents Not available Suggested method of standardisation Not available Pharmacology Pharmacodynamics Not available Efficacy Not available Pharmacokinetics Not available Microbiology Not available Medicinal uses Traditional system/folk medicine Not available 61 Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References None ________________________ Kontu glabriflorum (No information found. Consult Indian Pharmacopoeia) Botanical name Not available Local name(s) Not available Chemical constituents Not available Suggested method of standardisation Not available Pharmacology Pharmacodynamics Not available Efficacy Not available Pharmacokinetics Not available 62 Microbiology Not available Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References None ____________________ Pascartina ngonnyukpa (N o information found) Botanical name Not available Local name(s) Not available Chemical constituents Not available Suggested method of standardisation Not available 63 Pharmacology Not available Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References None _____________________ Leonurus cardiaca Botanical name Leonurus cardiaca Local name(s) Not available Chemical constituents Alkaloids-0.35%stachydrine (a pyrrolidine-type alkaloid), betonicine and turicin (sterioisomers of 4hydroxystachydrine), leonurine 0.0068% (a guanidine derivative) Flavonoids – glycosides of apigenin, kaempferol, and quercetin (eg hyperoside, kaempferol-3-D-glucoside, genkwanin, quinqueloside, quercitrin and rutin) Iridoids ajugol, ajugoside, garliridoside, leonurid and three or four more unidentified glycosides Tannins 64 Terpenoids – volatile oil, resin, wax, ursolic acid. Citric acid, malic acid, oleic acid, bitter principles, carbohydrates, choline and a phenolic glycoside (caffeic acid 4rutinoside Suggested method of standardisation Not available Pharmacology In Vitro and animal studies show oxytocic activity has been documented and attributed to another alkaloid constituent, stachydrine. Uterogenic activity has been reported for leonurine in various in vitro preparations includine human myometrial strips and isolated rat uterus. In vitro cardioactivity has been documented for motherwort. An alchoholic extract was found to have a direct inhibitory effect on myocardial cells; antagonistic action towards calcium chloride (provided that the extract was administered before calcium chloride), and towards both α- and β- adrenoceptor stimulation was observed. Antiplatelet activity has been stated for a related species, leonurus heterophyllus. Medicinal uses Traditional system/folk medicine Cardiac debility, simple tachycardia, effort syndrome, amenorrhea, and specifically for cardiac symptoms associated with neurosis. Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Sedative and antispasmodic property Precautions and toxicology Affects menstrual cycle. Leaves of motherwort may cause contact dermatitis and that the lemon-scented oil may result in photosensitization. Contraindications Excessive use may interfere with existing therapy for a cardiac disorder. Sensitive individuals may experience an allergic reaction Adverse effects See precautions and toxicology Dosage form Dried herb, liquid extract, tincture Posology or recommended dose Dried herb 2-4g or by infusion three times daily Liquid extract 2-4ml (1:1 in 25% alchohol) three times daily 65 Tincture 2-6ml (1:5 in 45% alchohol) three times daily. References Kong YC et al. Isolation of the uterotonic principle from leonurus Artemisia, the Chinese motherwort. Am J chin med 1976;4: 373-382. Tschesche RA et al. caffeic acid 4-rutinoside from leonurus cardiaca. Phytochemistry 1980;19:2783. Yanxing X. The inhibitory effect of motherwort extract on pulsating myocardial cells in vitro. J Trad Chin Med 1976;4: 373-382. Yeung HW et al. The structure and biological effect of leonurine-a uterotonic principle from the chineses drug, I-mu Ts’ao. Planta med 1977; 31:51-56. __________________________ Viburnum opulus Botanical name Viburnum opulus Local name(s) Not available Chemical constituents Resin, a bitter (viburnin), valerianic acid, salicosides, tannin, saponins Suggested method of standardisation Not available Pharmacology Pharmacodynamics Not available Efficacy Not available Pharmacokinetics Not available Microbiology Not available Medicinal uses Traditional system/folk medicine Cramp, ovarian and uterine pains, spasmodic muscular cramp, uterine dysfunction, menopausal metrorrhagia, threatened miscarriage, partus preparator, infantile enuresis. 66 Uses as described in pharmacopoeia Spasmolytic, sedative, astringent, smooth and skeletal muscle relaxant, cardiac tonic, uterine relaxant, antiinflammatory Uses supported by experimental or clinical data Viburnum opulus is a specific remedy for visceral tensions. It helps to relax muscular tension and spasm and is primarily used in the treatment of muscular cramps and ovarian and uterine muscle problems. It relaxes the uterus and relieves the painful cramps associated with menstruation. It may also be used in threatened miscarriage. Its astringent action gives it a role in the treatment of excessive blood loss in periods and especially bleeding associated with the menopause. It may also be used to help quieten convulsive states in children. It relaxes the cardiovascular system in hypertension and eases constipation associated with tension. Applied externally, it relieves skeletal muscle tension or cramps. It may also be helpful in some cases of migraine. Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Liquid extract, Tincture, Dried bark Posology or recommended dose Dried bark: 2-4g or by decoction Liquid extract: 1:1 in 25% alcohol, 2-4ml Tincture: 1:5 in 45% alcohol, 5-10ml References BHMA 1983 British Herbal Pharmacopoeia, BHMA, Bournemouth. Grieve, M. 1931 A Modern Herbal, (ed. C.F. Leyel 1985), London. Hoffmann, D. 1990 The New Holistic Herbal, Second Edition, Element, Shaftesbury. Mills, S.Y. 1993 The A-Z of Modern Herbalism, Diamond Books, London. Ody, P. 1993 The Herb Society's Complete Medicinal Herbal, Dorling Kindersley, London. __________________________ Mitchella repens Botanical name Mitchella repens Local name(s) Not available 67 Chemical constituents Largely unknown. Tannin, bitter principle, saponins, mucilage, unspecified alkaloids, glycosides, resin Suggested method of standardisation Not available Pharmacology Partus preparator, uterine relaxant, anti-dysmenorrhoeic, emmenagogue, astringent, nervous tonic and restorative Medicinal uses Traditional system/folk medicine Dysmenorrhoea, pregnancy, catarrhal colitis. Specifically indicated for the facilitation of parturition Uses as described in pharmacopoeia Mitchella is reputed to promote an easy labour by aiding contraction of the womb during childbirth. It is also recommended for dysmenorrhoea and other painful conditions of the female reproductive tract. It also has a calming effect on the nervous system and, in addition, improves the digestion. As an astringent, it has been used in the treatment of colitis, especially if there is much mucus. It may be used in nervous exhaustion, irritability or debility in either sex, especially when symptoms involve the reproductive system. Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Dried plant: 2-4g or by infusion Liquid Extract: 1:1 in 25% alcohol, 2-4ml References None _________________________ Parinari robusta Botanical name Parinari robusta 68 Local name(s) Not available Chemical constituents Not available Pharmacology Not available Medicinal uses Traditional system/folk medicine Not available Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References None 69 Monographs on Medicinal Plants Selected for Enteric/Typhoid Fever 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. Jatropha curcas Nauclea latifolia Phyllanthus fraternus Hoslundia opposita Ginkgo biloba Psidium guajava Spondia mombin Persea americana Trema orientalis Cnestia ferruginea Momordica charantia Vernonia amygdalina Lantana camara Paullinia pinnata Citrus aurantifolia Morinda lucida Bidens pilosa Hydrastis canadensis Lannea kerstingii Melia azedarch Piliostigma thonningii Carica papaya Vitis vinifera Azadirachta indica Khaya ivorensis Psidium guajava Citrus aurantifolia Vernonia amygdalina Cassia siamea Terminalia ivorensis __________________________ Ginkgo biloba(Ginkgoaceae). Botanical name Ginkgo biloba L. Local name(s) Ginkgo, maidenhair tree, temple balm, yin guo, yinhsing Chemical constituents Flavonoids; diterpene lactones (ginkgolides A, B, C, J and M); sesquiterpene lactone (bilobalide); catechins; proanthocyanidins; lipid; sterols; benzenoids; carotenoids; phenylpropanoids 70 Pharmacology Experimental pharmacology The effect of Ginkgo biloba extracts (GBE) on activated human peripheral T lymphocytes was evaluated and found that the extract might have beneficial effects in inflammation-based atherosclerotic diseases (Tsao et al 2008). GBE and constituents produced electropharmacological actions in cardiomyocytes and caused vasodilation, probably via inhibition of Ca2+ influx and the activation of nitric oxide release in the endothelium and aortic vascular muscles (Satoh and Nishida 2004). GBE has also been shown to have platelet activating factor (PAF) inhibitory activity. It antagonizes thromboxane induced vasoconstriction in rat cremaster muscle and improves both peripheral and cerebral blood flow. It also induces a dose-dependent contractile or relaxing effect on vascular smooth muscle (Ritch 2000). Given the diverse pharmacological properties of GBE, which includes ocular blood flow stimulation, antioxidant activity, PAF inhibitory activity, nitric oxide inhibition, and neuroprotective activity, it has been suggested that it could be an effective remedy for treating glaucoma (Ritch 2000). GBE has shown free radical scavenging and lipid peroxidation inhibitory activity in various tissues and experimental systems (Seif-El-Nasr and El-Fattah 1995). Clinical pharmacology Several clinical and experimental studies have reported G. biloba extract’s (GBE) diverse pharmacological actions. GBE has been reported to be beneficial in the management of ischaemic brain injury (Kleijnen et al 1992; Zhang et al 2000), symptoms of cerebrovascular insufficiency (e.g. difficulty in concentration and memory, absentmindedness, confusion, lethargy, depression, anxiety, dizziness, tinnitus and headache) (Vesper and Hänsegen 1994; Kennedy et al 2000; Kleijnen and Knipschild 1992a, 1992b); dementia and Alzheimer’s disease (Le Bars et al 1997), and peripheral vascular disease (Peters et al 1998; Diamond et al 2000). GBE has been shown to improve has circulatory stimulating effect in humans. There have been several reports alluding to the extract’s ability to enhance local cerebral blood flow, microcirculation and tissue metabolism. In addition, GBE has been shown to protect against hypoxia and reduce capillary permeability (Költringer et al 1989a, 1989b; Schaffler and Reeh 1985; Jung et al 1990; Hofferberth 1991; Ernst and Marshall 1992; Rudofsky 1987). Patients with coronary heart disease, hypertension, hypercholesterolemia and diabetes had improved fibrinogen levels and plasma viscosity after treatment with GBE (Ritch 2000). Placebo-controlled, double blind clinic trials conducted in humans have demonstrated the effectiveness of GBE in the treatment of intermittent claudication (Kleijnen and Knipschild 1992b; Bauer 1984; Saudreau et al 1984). GBE’s effectiveness has also been shown in some small-scale placebocontrolled, double-blind studies. In a study involving 68 patients GBE (120-160mg daily, for 4-12 weeks) was shown to be effective in treating inner ear disorders, such as hearing loss, vertigo and tinnitus (Kleijnen and Knipschild 1992a; 1992b). Pharmacodynamics Ginkgolide B is a competitive antagonist at the PAF receptor site. Pharmacokinetics It has been reported that bilobalide and ginkgolides A and B possess high bioavailability, when orally administrated (Biber and Koch 1999; Foutillan et al 1995; Mauri et al 200). The plasma concentrations of ginkgolides A and B after oral administration of 160 mg of GBE to healthy volunteers were 41.8, 5.6 and 37.6 μg/ml respectively (Mauri et al 2001), while the Tmax of terpenoids is about 120 min (Mauri et al 2001). 71 Medicinal uses Traditional system/folk medicine Vermifuge, oxytocic; for the treatment of bronchitis, chronic rhinitis, chilblains, arthritis, and oedema (Squires 1995; Farnsworth 1995; Huh and Staba 1992). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Antineoplastic; anticlastogenic; for treating tinnitus, vertigo, acute hearing loss (Ritch 2000). Precautions and toxicology Investigations with GBE showed no mutagenic, carcinogenic, or teratogenic effects (German Commission E Monographs 1994). Contraindications Hypersensitivity to G. biloba preparations (German Commission E Monographs 1994). Adverse effects Headaches, gastrointestinal disturbances, and allergic skin reactions (German Commission E Monographs 1994; Ritch 2000). Dosage form Standardized extracts (dry extracts from dried leaves, extracted with acetone and water, drug:extract ratio 35– 67:1); coated tablets and solution for oral administration are prepared from standardized purified extracts (Kleijnen and Knipschild 1992a; German Commission E Monographs 1994); fluid extracts Posology or recommended dose Dried extract: 120–240mg daily in 2 or 3 divided doses (2); 40 mg extract is equivalent to 1.4–2.7 g leaves (20) Fluid extract: (1:1), 0.5 ml 3 times a day (WHO Monographs). References Bauer U (1984). Six month double-blind randomized clinical trial of Ginkgo biloba extract versus placebo in two parallel groups in patients suffering from peripheral arterial insufficiency. Arzneimittel-Forschung 34, 716-720. Biber A, Koch E (1999). Bioavailability of ginkgolides and bilobalide from extracts of Ginkgo biloba using GC/MS. Planta Medica 65, 192-193. Diamond BJ, Shiflett SC, Schoenberger NE (2000). Ginkgo biloba extract: mechanisms and clinicals indications. Arch Phys Med Rehabil 81, 668-678. Farnsworth NR, ed. NAPRALERT database. University of Illinois at Chicago, IL, August 8, 1995 production (an on-line database available directly through the University of Illinois at Chicago or through the Scientific and Technical Network (STN) of Chemical Abstracts Services). Foutillan JB, Brisson AM, Girault J, Ingrand I et al (1995). Phamacokinetic properties of bilobalide and ginkgolides A and B in healthy subjects after intravenous and oral administration of Ginkgo biloba extract (EGb 761). Therapie 50, 137-144. German Commission E Monograph, Trockenextrakt (1994) aus Ginkgo-biloba-Blättern Extrakt mit Aceton-Wasser. Bundesanzeiger 46, 7361-7362. 72 Hofferberth B (1991). Simultanerfassung elektrophysiologischer, psychometrischer und rheologischer Parameter bei Patienten mit hirnorganischem Psychosyndrom und erhöhtem Gefässrisiko-Eine Placebo-kontrollierte Doppelblindstudie mit Ginkgo biloba-Extrakt EGB 761. In: Stodtmeister R, Pillunat LE, eds. Mikrozirkulation in Gehirn und Sinnesorganen. Stuttgart, Ferdinand Enke 64-74. Huh H, Staba EJ (1992). The botany and chemistry of Ginkgo biloba L. Journal of Herbs, Spices and Medicinal Plants 1, 91–124. Jung F et al (1990). Effect of Ginkgo biloba on fluidity of blood and peripheral microcirculation in volunteers. Arzneimittel-Forschung 40, 589-593. Kennedy DO, Scholey AB, Wesnes KA (2000). The dose-dependent cognitive effects of acute administration of Ginkgo biloba to healthy young volunteers. Psychopharmacology 151, 416-423. Kleijnen J, Knipschild P (1992). Ginkgo biloba for cerebral insufficiency. British Journal of Clinical Pharmacology 34, 352-358. Kleijnen J, Knipschild P (1992a). Ginkgo biloba. Lancet 340, 1136–1139. Kleijnen J, Knipschild P (1992b). Ginkgo biloba for cerebral insufficiency. British Journal of Clinical Pharmacology 34, 352-358. Költringer P et al (1989). Die Mikrozirkulation und Viskoelastizität des Vollblutes unter Folium Ginkgo167 Ginkgo biloba extrakt. Eine plazebokontrollierte, randomisierte Doppelblind-Studie. Perfusion 1, 28-30. Költringer P et al (1989). Mikrozirkulation unter parenteraler Ginkgo biloba Extrakt-Therapie. Wiener Medizinische Wochenschrift 101, 198-200. Le Bars PL, Katz MM, Berman N, Itil TM et al (1997). A placebo-controlled, double-blind, randomized trial of an extract of Ginkgo biloba for dementia. JAMA 278, 1327-1332. Mauri P, Simonetti P, Gardana C, Minoggio M et al (2001). Liquid chromatography/atmospheric pressure chemical ionization mass spectrometry of terpene lactones in plasma of volunteers dosed with Ginkgo biloba L. extracts. Rapid Commun Mass Spectrom 15, 929–934 Peters H, Kieser M, Hölscher U (1998). Demonstration of the efficacy of Ginkgo biloba special extract EGb 761R on intermittent claudication-a placebo-controlled, double-blind multicenter trial. VASA 27, 106-110. Rudofsky G (1987). Wirkung von Ginkgo-biloba-extrakt bei arterieller Verschlusskrankheit. Fortschritte der Medizin 105, 397-400. Ritch R (2000). Potential role for Ginkgo biloba extract in the treatment of glaucoma. Medical Hypotheses 54(2): 221-235 Satoh H, Nishida S (2004). Electropharmacological actions of Ginkgo biloba extract on vascular smooth and heart muscles. Clinica Chimica Acta 342, 13–22 Saudreau F, Serise JM, Pillet J (1989). Efficacité de l’extrait de Ginkgo biloba dans le traitement des artériopathies obliterantes chroniques des membres inferieurs au stade III de la classification de Fontaine. Journal malade vasculare 14, 177-182. Schaffler K, Reeh PW (1985). Doppelblindstudie zur hypoxieprotektiven Wirkung eines standardisierten Ginkgo-biloba-Präparates nach Mehrfachverabreichung an gesunden Probanden. Arzneimittel-Forschung 35, 1283-1286. Seif-El-Nasr M, El-Fattah AA (1995). Lipid peroxide, phospholipids, glutathione levels and superoxide dismutase activity in rat brain after ischaemia: effect of ginkgo biloba extract. Pharmacol Res 1995; 32: 273–278. Squires R. Ginkgo biloba. Australian traditional medicine society (ATOMS), 1995:9–14. Tsao T-P, Lai J-H, Yang S-P, Ho L-J et al (2008). Suppression of tissue necrosis factor-alpha or hydrogen peroxide-activated primary human T lymphocytes by Ginkgo biloba extract through down-regulation of activator protein-1 signal transduction. Phytomedicine 15, 170–176 Vesper J, Hänsegen KD (1994). Efficacy of Ginkgo biloba in 90 outpatients with cerebral insufficiency caused by old age; results of a placebo-controlled double-blind trial. Phytomedicine 1, 9-16. World Health Organization, Geneva (1999). WHO monographs on selected medicinal plants 1, 154-167. Zhang WR, Hayashi T, Kitagawa H, Sasaki C et al (2000). Protective effect of Ginkgo biloba extract on rat brain with transient middle cerebral artery occlusion. Neurol Res 22, 517-521. Foot notes: Some Combination Products of Typhoid 1. 2. 3. 4. 5. Mist Alomal Fralena Tafoss Capsules Obiri Mixture Class Typlex Mist Enterica 73 6. Tafoss Mixture 7. Alafia Alaherbs Typhoid 8. Abibiman Herbal Mixture 9. Maame Frema Taif Medicine 10. Top Bintah Mixture 11. Taiphoid Strong 12. Anidaso Taifaplex _______________________________________ Bidens pilosa Botanical name Bidens pilosa Linn. var. Radiata Local name(s) Not available Chemical constituents β-caryophyllene; τ-cadinene; phenylpropanoid glucosides, polyacetylenes, diterpenes, flavonoids, and flavone glycosides; alkaloids, saponins, triterpenes; acyl chalcones and glucosides (Chiang et al 2004; Zollo et al 1995; Hoffmann and Hölzl, 1988),). Pharmacology The essential oils and aqueous extracts of B. pilosa possess antioxidant and antimicrobial activities (Deba et al 2008; Abajo et al 2004). The ethanol and ethyl acetate/ethanol extracts from the whole B. pilosa demonstrated protective antioxidant properties (Yang et al 2006). The total flavonoids had a protective and therapeutic effect on carbon tetrachloride (CCl4)-induced liver injury in mice and rats, (Yuan et al 2007). B. pilosa extract has been reported to modulate T cell differentiation and prevent the development of non-obese diabetes in mice (Chiang et al (2007). Antitumour activity has been shown by the chloroform extract; it increased the life span of EAC-tumor bearing mice, and decreased both, serum LDH activity and the GSH content of the tumor fluid (Kviecinski et al 2007). A study by Steenkamp and Gouws (2006) on aqueous extracts prepared from six South African medicinal plants, with cancer-related ethnobotanical uses showed extracts of B. pilosa to possess anticancer activity. Experimental evidences have shown that crude extracts from roots, prepared with 80%ethanol by percolation, show in vitro activity against Plasmodium falciparum (Oliveira et al 2004). From a study that investigated the effect of the leaf methanol extract of B. pilosa on systolic blood pressure and plasma glucose, insulin, cholesterol, triglycerides and creatinine levels in rats with fructose-induced hypertension, it was found B. pilosa extract was anti-hypertensive. The extract also reduced the fructose-induced elevated plasma insulin levels (Dimo et al 2002). The methylene chloride extract displayed a very high anti-ulcerogenic activity (100% inhibition) at a dose of 750 mg/kg in vivo (Tan et al 2000). B. pilosa extract showed antiulcer activity against indomethacin-induced gastric lesions. The extract effectively inhibited gastric haemorhagic lesions induced by ethanol, and with an effective dose of 2 g/kg being more potent than sucralfate (400 mg/kg) (Alvarez et al 1999). Components of B. pilosa exhibited an immunosuppressive and anti-inflammatory activity in vitro and in vivo (Pereira et al 1999). Leaf aqueous extract of B. pilosa relaxed norepinephrine-induced aortic strips contractions, an effect which was thought to be due to the blockade of the influx of extracellular Ca2+ into the cell (Dimo et al 1998). Medicinal uses Traditional system/folk medicine Anti-inflammatory, antiseptic, hepatoprotective, antihypertensive, hypoglycaemic effects; hepatitis, stomach disorders, diabetes, hypertension, malaria, pain, fever, angina, oedema; laryngitis, headache; ulcers; diuretic; choleretic; influenza, diarrhea, conjunctivitis; wounds and chronic gastro–duodenal ulcers (Dimo et al 2002; Alvarez et al 1999; Alarcon-Aquilar et al 2002; Andrade-Neto et al 2004; Vasquez 1990; Valdés and Rego 2001; Kokwaro 1976; Adjanohoun et al 1988; Girault 1984). 74 Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Anti-inflammatory, antiseptic, hepato-protective, antihypertensive, hypoglycaemic Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References Abajo C, Boffill MA, del Campo J, Méndez MA et al (2004). In vitro study of the antioxidant and immunomodulatory activity of aqueous infusion of Bidens pilosa. Journal of Ethnopharmacology 93, 319-323. Adjanohoun EJ, Ake Assi L, Ahmed A., Eyme J et al (1988). Médecine Traditionnelle et Pharmacopée. Contribution aux Etudes Botaniques et Floristiques aux Comores. Rapport Agence de Coope´ration Culturelle et Technique (ACCT) Paris, 243. Alarcon-Aquilar FJ, Roman-Ramos R, Flores-Saenz JL, Aquirre-Garcia F (2002). Investigation on the hypoglycaemic effects of extracts of four Mexican medicinal plants in normal and alloxan-diabetic mice. Phytotherapy Research 16, 383-386. Alvarez A, Pomar FS, Montero MJ (1999). Gastric antisecretory and antiulcer activities of an ethanolic extract of Bidens pilosa L. var. radiata Schult. Bip. Journal of Ethnopharmacology 67, 333-340. Andrade-Neto VF, Brandao MG, Oliveira FQ, Casali VW et al (2004). Antimalarial activity of Bidens pilosa L. (Asteraceae) ethanol extracts from wild plants collected in various localities or plants cultivated in humus soil. Phytotherapy Research 18, 634-639. Chiang YM, Chuang DY, Wang SY, Kuo YH et al (2004). Metabolite profiling and chemopreventive bioactivity of plant extracts from Bidens pilosa. Journal of Ethnopharmacology 95, 409-419. Chiang Y-M, Chang CL-T, Chang S-L, Yang W-C et al (2007). Cytopiloyne, a novel polyacetylenic glucoside from Bidens pilosa, functions as a T helper cell modulator. Journal of Ethnopharmacology 110, 532–538. Deba F, Xuan TD, Yasuda M, Tawata S (2008). Chemical composition and antioxidant, antibacterial and antifungal activities of the essential oils from Bidens pilosa Linn. var. Radiata. Food Control 19, 346-352. Dimo T, Rakotonirina SV, Tan PV, Azay J et al (2002). Leaf methanol extract of Bidens pilosa prevents and attenuates the hypertension induced by high-fructose diet in Wistar rats. Journal of Ethnopharmacology 83, 183-191. Dimo T, Rakotonirina S, Kamgang R, Tan PV et al (1998). Effects of leaf aqueous extract of Bidens pilosa (Asteraceae) on KCl- and norepinephrine-induced contractions of rat aorta. Journal of Ethnopharmacology 60, 179-182. Girault L (1984). Kallawaya, Guérisseurs Itinérants des Andes: Recherche sur les Pratiques Médicales et Magiques. Office de la Recherche Scientifique et Technique d’Outre-Mer (ORSTOM), Paris 1-99. Kokwaro JO (1976). Medicinal Plants of East Africa. East African Literature Bureau, Kampala, Nairobi, Dar es Salaam, 61. Kviecinski MR, Felipe KB, Schoenfelder T, Wiese LPL et al (2007). Study of the antitumor potential of Bidens pilosa (Asteraceae) used in Brazilian folk medicine, Journal of Ethnopharmacology doi:10.1016/j.jep.2008.01.017 75 Oliveira FQ, Andrade-Neto V, Krettli AU, Brandão MGL (2004). New evidences of antimalarial activity of Bidens pilosa roots extract correlated with polyacetylene and flavonoids. Journal of Ethnopharmacology 93, 39-42. Pereira RLC, Ibrahim T, Lucchetti L, da Silva AJR et al (1999). Immunosuppressive and anti-inflammatory effects of methanolic extract and the polyacetylene isolated from Bidens pilosa L. Immunopharmacology 43, 31-37 Steenkamp V, Gouws MC (2006). Cytotoxicity of six South African medicinal plant extracts used in the treatment of cancer. South African Journal of Botany 72, 630633 Tan PV, Dimo T, Dongo E (2000). Effects of methanol, cyclohexane and methylene chloride extracts of Bidens pilosa on various gastric ulcer models in rats. Journal of Ethnopharmacology 73, 415-421 Valdés HAL, Rego HPL (2001). Bidens pilosa Linné. Revista Cubana Planta Medica 1, 28-33. Vasquez MR (1990). Useful plants of Amazonian Peru. Second Draft. Filed with USDA's National Agricultural Library. USA. Yang H-L, Chen S-C, Chang N-W, Chang J-M et al (2006). Protection from oxidative damage using Bidens pilosa extracts in normal human erythrocytes. Food and Chemical Toxicology 44, 1513–1521 Yuan Li-p, Chen F-h, Ling L, Dou P-f et al (2007). Protective effects of total flavonoids of Bidens pilosa L (TFB) on animal liver injury and liver fibrosis. Journal of Ethnopharmacology doi:10.1016/j.jep.2008.01.010 Foot notes: 1. Mist Enterica ________________________ Cnestia ferruginea Botanical name Cnestia ferruginea Local name(s) Not available Chemical constituents Dicoumarol; 4-hydroxycoumarin; squalene, myricyl alcohol, β-sitosterol (Olugbade et al 1982; Vickery and Vickery 1980) Suggested method of standardisation Not available Pharmacology A phytochemical investigation of a neurotoxic syndrome that had caused about 50 human deaths in Casamance (Senegal) revealed the presence of a neurotoxic amino acid methionine sulfoximine and the leaf decoction was subsequently found to exhibit cytotoxic effects (Garon et al 2007). Extracts of C. ferruginea and Voacanga africana showed strong activity against Aspergillus niger. C. ferruginea was also active against dermatophytes (le Grand et al 1998). Aqueous extract of the roots (Malcolm and Sofowora 1969) and the methanolic extract of the root stem and leaves of the plant (Boakye-Yiadom and Konning 1975) were shown to have antimicrobial properties. 76 Pharmacodynamics No specific data exists other than the animal studies above Pharmacokinetics No pharmacokinetic data exists Microbiology See pharmacological studies above Medicinal uses Traditional system/folk medicine Various infantile illness; laxative; fever; chills; migraine; infected gums; snakebite; conjunctivitis; bronchitis; tuberculosis; dysmenorrhoea; epilepsy; dysentery; syphilis; gonorrhea; aphrodisiac; abortifacient; epilepsy (Olugbade et al 1982; Jongkind and Lemmens 1989; Olugbade et al 1982; Dalziel 1937; Kerharo 1974). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Cytotoxic; neurotoxic; antimicrobial; antifungal Precautions and toxicology Beagle dogs fed an unspecified dose of C. ferruginea seeds showed serious clinical symptoms such as emesis, lateral recumbency, decreased locomotor activity, clonic and tonic convulsions, salivation, irritability and death after 24–25 h (Murakoshi et al 1993). Toxicity thought to be due the presence of the compounds dicoumarol and 4-hydroxycoumarin has been reported in rabbits (Vickery and Vickery 1980). Contraindications No data exists, but given the presence of coumarins in this plant care must attend its concomitant use with anticoagulants Adverse effects Neurotoxic effects reported although the dose is not specified Dosage form Decoctions, infusions, tinctures Posology or recommended dose Decoction: 40 g of dried plant material in 1 litre of water; drink 4 cups daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily References 77 Boakye-Yiadom A, Konning R (1975). Planta Medica 28, 397. Dalziel JM (1937). The Useful Plants of West Tropical Africa. The Crown Agents for the Colonies, London, 612. Garon D, Chosson E, Rioult J-P, de Pecoulas PE et al (2007). Poisoning by Cnestis ferruginea in Casamance (Senegal): An etiological approach. Toxicon 50, 189-195. Jongkind CCH, Lemmens RHMJ (1989). The Connaraceae: a taxonomic study with special emphasis on Africa. Agric. University Wageningen Papers 89, 1-403. Kerharo J (1974). La pharmacopée Sénégalaise traditionnelle, plantes médicinales et toxiques. Vigot, Paris, 1012. le Grand A, Wondergem PA, Verpoorte R, Pousset JL (1998). Anti-infectious phytotherapies of the tree-Savannah of Senegal (West Africa) II. Antimicrobial activity of 33 species. Journal of Ethnopharmacology 22, 25-31. Malcom SA, Sofowora EA (1969). Lloydia 32, 512. Murakoshi I, Sekin T, Maeshima K, Ikegami F et al (1993). Absolute configuration of Lmethionine sulfoximine as a toxic principle in Cnestis palala (Lour.) Merr. Chem. Pharm. Bull. 41, 388-390. Olugbade TA, Oluwadiya JO, Yisak WA-B (1982). Chemical constituents of Cnestis ferruginea DC. I. Petroleum ether fraction. Journal of Ethnopharmacology 6, 365370. Vickery M, Vickery B (1980). Coumarins and related compounds in members of the Connaraceae. Toxicology Letters 5, 115-118. Foot notes: 1. Mist Enterica _______________________ Spondia mombin Botanical name Spondia mombin Local name(s) Not available Chemical constituents Not available Pharmacology The leaves of S. mombin have been shown to exhibit sedative and antidopaminergic effects. The aqueous, methanolic and ethanolic extracts dose-dependently prolonged hexobarbital-induced sleeping time and reduced novelty-induced rearing (NIR) in both mice and rats. Phenolic compounds present in the ethanolic and methanolic extracts, possessed exhibited anticonvulsant properties. In addition, the extracts decreased amphetamine/apomorphine-induced stereotyped behaviour (Ayoka et al 2006). The antibacterial and molluscicidal effects of the phenolic acid, 6-alkenyl-salicylic acid, obtained from S. mombin has also been reported (Corthout et al 1994). Extracts containing phenolic derivatives have demonstrated antiherpes and antioxidant properties (Corthout et al 1992; Castner et al 1998; Shultes and Raffauf 1990; Mats 1994). The anacardic acid derivative from the hexane extract of the plant demonstrated β-lactamase inhibitory properties (Coates et al 1994). 78 Pharmacodynamics The NIR inhibitory effects of the S. mombin extracts were not mediated via muscarinic, α2-adrenergic, and μ-opioid receptors. However, the extracts seemed to facilitate GABAergic transmission (Ayoka et al 2006). Efficacy No specific data exists other than the animal studies above Pharmacokinetics No specific data exists other than the animal studies above Medicinal uses Traditional system/folk medicine As a diuretic; febrifuge, emetic, anti-diarrhoeal, antibacterial, antifungal, antiviral; abortifacient; for the treatment of dysentery, haemorrhoids; gonorrhoea; leucorrhoea; stomach ache, various inflammatory conditions; wounds; psychiatric disorders (Ayoka et al 2006; Ajao and Shonukan 1985; Abo et al 1999; Corthout et al 1991; Rodrigues and Hesse 2000; Villegas et al 1997; Offiah and Anyanwu 1989) Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Sedative; antidopaminergic; antibacterial; molluscicidal; antiviral; antioxidant; antiepileptic; antipsychotic Precautions and toxicology None known Contraindications Not available Adverse effects Not available Dosage form Decoction; tincture Posology or recommended dose Decoction: 40 g of dried plant material in 1 litre of water; drink 4 cups daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily References Abo KA, Ogunleye VO Ashidi JS (1999). Antimicrobial potential of Spondias mombin Croton Zambesicus and Zygotritonia Crocea. Phytotherapy Research 13, 494497. 79 Ajao AO, Shonukan O (1985). Antibacterial effects of aqueous and alcohol extracts of Spondias mombin and Abchornea cordifolia: two local antimicrobial remedies. International Journal of Crude Drug Research 23, 67-72. Ayoka AO, Akomolafe RO, Iwalewa EO, Akanmu MA et al (2006). Sedative, antiepileptic and antipsychotic effects of Spondias mombin L. (Anacardiaceae) in mice and rats. Journal of Ethnopharmacology 103, 166-175 Castner JL, Timme SL, Duke JA (1998). A Field Guide to Medicinal and Useful Plants of the Upper Amazon. Feline Press, Gainsville, FL. Coates NJ, Gilpin ML, Gwynn MN, Lewis DE et al (1994). SB-202742 a novel beta-lactamase inhibitor isolated from Spondias mombin. Journal of Natural Products 57, 654-657. Corthout FJ, Pieters LA, Claeys M, Vanden Berghe DA et al (1991). Antiviral; Ellagitannins from Spondias mombin. Phytochemistry 30, 1190. Mats FJA (1994). Farmacias Vivas, Ed. UFC, and 2a, Ed., Forteleza. Offiah VN, Anyanwu II (1989). Abortifacient activity of an aqueous extract of Spondias mombin leaves. Journal of Ethnopharmacology 26, 317-320. Rodrigues KF, Hesse M (2000). Antimicrobial activities of secondary metabolites produced by endophytic fungi from Spondias mombin. Journal of Basic Microbiology 40, 261-267. Shultes RE, Raffauf RF (1990). The Healing Forest: Medicinal and Toxic Plants of the Northwest Amazonia. Dioscorides Press, Portland, Oregon. Villegas LF, Fernadez TD, Maldonado H, Torres R et al (1997). Evaluation of wound healing activity of selected plants from Peru. Journal of Ethnopharmacology 55, 193-200. Foot notes: 1. Class Typlex _________________________________ Lannea acida Botanical name Lannea acida A. Rich. Local name(s) Not available Chemical constituents Not available Suggested method of standardisation Not available Pharmacology Not available Medicinal uses Traditional system/folk medicine (Lannea acida) diarrhoea, stomach-ache, gonorrhoea, rheumatism (Koné et al 2004). Uses as described in pharmacopoeia Not available 80 Uses supported by experimental or clinical data Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References Koné WM, Atindehou KK, Terreaux C, Hostettmann K et al (2004). Traditional medicine in North Côte-d’Ivoire: Screening of 50 medicinal plants for antibacterial activity. Journal of Ethnopharmacology 93, 43-49. Foot notes: 1. Maame Frema Taif Medicine ____________________________ Melia azedarch Botanical name Melia azedarch Local name(s) Not available Chemical constituents Not available Suggested method of standardisation Not available Pharmacology No pharmacological studies exist Medicinal uses Traditional system/folk medicine Not available 81 Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical dat Not available Precautions and toxicology Not available Contraindications Not available Adverse effects Not available Dosage form Not available Posology or recommended dose Not available References None Foot notes: 1. Abibiman Herbal Mixture ______________________ Piliostigma thonningii Botanical name Piliostigma thonningii Local name(s) Not available Chemical constituents Tannins; alkaloids; tannins; flavonols; hydropectin; sugars; kaurane diterpene (Akinpelu and Obuotor 2000; Asuzu et al 1999; Baratta et al 1999). Suggested method of standardisation Not available Pharmacology The component D-3-O-methylchiroinositol showed anthelmintic properties (Asuzu et al 1999) and the methanolic stem bark extract exhibited activity against six out of eight bacterial isolates (Akinpelu and Obuotor 2000). 82 Medicinal uses Traditional system/folk medicine As an anthelmintic; antitussive; bronchodilator; cicatrizant; antiseptic; to treat dysentery; snake-bite; tooth ache; leprosy; smallpox; coughs; myalgias; enteritis; anuria; fever, leprosy, respiratory ailments, and as a dressing for wounds and ulcers (Akinpelu and Obuotor 2000; Asuzu et al 1999; Baratta et al 1999). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Anthelminthic; antibacterial; antitussive; bronchodilator; cicatrizant; antiseptic Precautions and toxicology None reported Contraindications None known Adverse effects None known Dosage form Decoctions; tinctures; powdered plant Posology or recommended dose Decoction: 40 g of dried plant material in 1 litre of water; drink 4 cups daily Tincture: 1:5 in 45% alcohol; 5 ml three times daily References Akinpelu DA, Obuotor EM (2000). Antibacterial activity of Piliostigma thonningii stems bark. Fitoterapia 71, 442-443 Asuzu IU, Gray AI, Waterman PG (1999). The anthelmintic activity of D-3-O-methylchiroinositol isolated from Piliostigma thonningii stem bark. Fitoterapia 70, 77-79. Baratta MT, Ruberto G, Tringali UC (1999). Constituents of the pods of Piliostigma thonningii. Fitoterapia 70, 205-208. Foot notes: 1. Alafia Alaherbs Typhoid _________________________ 83 Vitis vinifera Botanical name Vitis vinifera var. Ribier Local name(s) Grapes Chemical constituents Tannins ((+)-catechin, (-)-epicatechin, (+)-gallocatechin); flavonoids (anthocyanins, quercetin, myricetin, and kaempferol); organic acids, lipids, enzymes; vitamins; hydroxybenzoic acids, hydroxycinnamic acids, stilbenes (German and Walzem 2000; Bombardelli and Morazzonni 1995; Hebash et al 1991; Hmamouchi et al 1997; Felicio et al 2001). Pharmacology The polyphenolic-rich ethyl acetate fraction of V. vinifera exhibited a significant antihyperglycaemic and antioxidant activity equipotent with the reference hypoglycaemic agent (tolbutamide) in diabetic rats (Orhan et al 2006). The lyophilized extract of wine obtained from Jacquez grapes (V. aestivalis-cinerea x V. vinifera grapes) showed anti-inflammatory and antioxidant properties in and could be useful in the treatment of diseases associated with cartilage degradation (Panico et al 2006). A trial which evaluated the anti-proliferative potential of red muscadine (V. rotundifolia) and red cabernet sauvignon (V. vinifera) wines in cell culture found that extracts from both wines exerted anti-cancer effects in leukemia cells (Mertens-Talcott et al 2008). Grape juice and skin and seed extracts of V. vinifera black table grapes were found to be highly inhibitory against Listeria monocytogenes (Rhodes et al 2006). A study of the efficacy of procyanidins from V. vinifera seeds, a standardized mixture of polyphenol antioxidants, on cardiac mechanics following ischemia/reperfusion stunning in the rat, after 3 weeks supplementation showed that procyanidins supplementation in the rat had potent antioxidant and cardioprotective effects (Facino et al 1999). Alam et al (2002) have shown the chemopreventive propertes of V. vinifera. Alcoholic extracts of the plant demonstrated dose-dependent hepatoprotective and antioxidant effects in vivo (Orhan et al 2007). Medicinal uses Traditional system/folk medicine Antidiabetic; haemostatic; anti-inflammatory; analgesic; for the treatment of wounds, diarrhoea; jaundice; liver diseases, high blood pressure and anaemia (Orhan et al 2007; Orhan et al 2006; Bombardelli and Morazzonni 1995; Baytop 1999; Karaman and Kocabas 2001; Celik et al 1998). Uses as described in pharmacopoeia Not available Uses supported by experimental or clinical data Hypoglycaemic; antioxidant; anti-inflammatory; anti-proliferative; anti-cancer; antibacterial; cardioprotective; hepatoprotective Precautions and toxicology None known 84 Contraindications None reported Adverse effects V. vinifera has minimal toxicity and a wider therapeutic window (Panico et al 2006). Dosage form Decoctions; infusions; tincture Posology or recommended dose Not available References Alam A, Khan N, Sharma S, Saleem M et al (2002). Chemopreventive effect of Vitis vinifera extract on 12-O-tetradecanoyl-13-phorbol acetate-induced cutaneous oxidative stress and tumour promotion in murine skin. Pharmacological Research 46(6): 557-564. Baytop T (1999). Bitkiler Ile Tedavi (Geçmişte ve Bugün). Nobel Tıp Kitabevleri, Istanbul, 357-358. Bombardelli E, Morazzonni P (1995). Vitis vinifera L. Fitoterapia 66, 291-317. Celik H, Agaoglu YS, Fidan Y, Marasali B et al (1998). General Viniculture. Sun Fidan A.S. Professional Books Series, Ankara 1, 1-253. Facino RM, Carini M, Aldini G, Berti F et al (1999). Diet enriched with procyanidins enhances antioxidant activity and reduces myocardial post-ischaemic damage in rats. Life Sciences 64(8): 627-642 Felicio JD, Santos R, Gonçalez E (2001). Chemical Constituents from Vitis vinifera (Vitaceae), 68. Arquivos Do Instituto Biologico, São Paulo 47-50. Hebash KAH, Fadel HM, Solıman MMA (1991). Volatile components of grape leaves. Journal of Islamic Academy of Sciences 4, 26-28. Hmamouchi M, Es-Safi N, Essassi EM (1997). Oligomeric and polymeric proanthocyanidins from Moroccan grapewine (Vitis vinifera) leaves. Fitoterapia 68, 332-337. Karaman S, Kocabas YZ (2001). Traditional Medicinal Plants of K. Maras (Turkey). The Scientist 1, 125–128. Mertens-Talcott SU, Percival SS, Talcott ST (2008). Extracts from red muscadine and cabernet sauvignon wines induce cell death in MOLT-4 human leukemia cells. Food Chemistry 108, 824-832. Orhan DD, Orhan N, Ergun E, Ergun F (2007). Hepatoprotective effect of Vitis vinifera L. leaves on carbon tetrachloride-induced acute liver damage in rats. Journal of Ethnopharmacology 112, 145-151. Orhan N, Aslan M, Orhan DD, Ergun F et al (2006). In-vivo assessment of antidiabetic and antioxidant activities of grapevine leaves (Vitis vinifera) in diabetic rats. Journal of Ethnopharmacology 108, 280-286. Panico AM, Cardile V, Avondo S, Garufi F et al (2006). The in vitro effect of a lyophilized extract of wine obtained from Jacquez grapes on human chondrocytes. Phytomedicine 13, 522–526. Rhodes PL, Mitchell JW, Wilson MW, Melton LD (2006). Antilisterial activity of grape juice and grape extracts derived from Vitis vinifera variety Ribier. International Journal of Food Microbiology 107, 281-286. Foot notes: 1. Abibiman Herbal Mixture 85