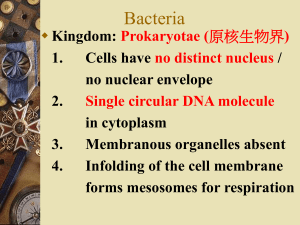
Microbiology: Gram Positive Bacteria pg. 1 Haleigh Stidham GRAM
advertisement

Microbiology 09/19/2008 Gram Positive Bacteria Transcriber: Haleigh Stidham 37 minutes GRAM POSTIVE COCCI …Continuation of first lecture (starting at 35:45 on recording) 22. There are several characteristics of Strep pyogenes that enables it to produce disease. Here is an arm that has cellulitis on it because the virulence factors that it produces can stimulate the host’s inflammatory system. You can get the erythrogenic toxin that causes “Scarlet Fever” which is a red rash that occurs with this strep infection. Streptokinases dissolve clots, and that’s why they are used in people that have had myocardial infarctions. Enzymes that depolymerize DNA and all the hemolysins are used there. The body can produce antibodies to “streptolysins” in the course of a strep infection. If you suspect Rheumatic Fever, you can measure the antibody levels of the antistreptolysin O, and if this is elevated if can help confirm the diagnosis of Rheumatic Fever. 23. Erysipelas is a skin infection and is more severe than impetigo. It has a number of different proteins that help bind it to fibronectin in the host’s cells. There is also a protein to inactivate compliment. So there are all these different things that help it produce disease in the host and also combat the host’s defense mechanisms. This is why it is such a successful pathogen. 24. S. agalactiae is part of the Group B streptococci. We sometimes see this as a cause of meningitis in children and UTIs and bacteremia in older adults. It used to be an important cause of sepsis and meningitis in newborn infants. So now all women are screened for Group B strep in their cervix, vagina, and rectum during pregnancy. If it is passed to their baby during birth, the baby can get severe pneumonia, blood stream infections, and meningitis. As a result, we don’t see this as an infection in babies anymore because the mother has been screened. To help identify Group B strep in lab, there is a unique reaction with Staph aureus. If you take a Staph areus strain and streak it across a blood agar plate and then streak a Group B strep close to it but not touching it, the CAMP factor is a sphingomyelinase produced by Group B strep that interacts with the hemolytic activity of S. aureus and it produces arrowheads (picture). This helps you identify the Group B strep from other Strep. 25. This table is to show you some of the other organisms that are beta-hemolytic Strep that produce disease. Strep pyogenes is one that we studied in pathology. You can get a strep infection and then you can get a type III immune complex disease—glomerulonephritis. It usually follows a respiratory infection or a skin infection with a Group A Strep. 26. S. pneumoniae is important because it is the most common cause of community acquired pneumonia, and in severe cases, you can get bacteremia (blood stream involvement). In children, it is the most common cause of middle ear infections (otitis media). This is the most common reason why antibiotic prescriptions are written in the United States. Also, this a common cause of meningitis. So this is a very important pathogen. It is not a beta-hemolytic organism, so it does not have a Lancefield antigen. It does have a species specific Microbiology: Gram Positive Bacteria Haleigh Stidham pg. 2 polysaccharide C. There are over 90 different serotypes based on its capsule. That is why you can get pneumococcal disease over and over. To identify S. pneumoniae in lab, we use the bile solubility and optochin susceptibility tests. Optochin is an antibiotic compound used to separate Strep pneumoniae from other alphahemolytic strep species found in the body. S. pneumoniae is susceptible to optochin. It also likes to grow in a carbon dioxide environment, so we can say it is captophillic. 27. S. pneumoniae has many virulence factors. One is the antiphagocytic capsule, which is an important immunogen. Here is the quelling reaction—where the capsule will swell if there is a serum-specific antibody that is mixed with the strep. Here is a sputum specimen with WBC, inflammation cells, and S. pneumoniae with it. Pneumococcus Surface Protein A (PspA) is a surface protein that inhibits the opsonization of the strep. It has autolysins and pneumolysins to protect it from the body. The main thing is if we inhale the S. pneumoniae, it begins to multiply in the alveoli of the lungs. It stimulates chemotatic factors that bring neutrophils there, increases vascular permeability, and you get the whole acute inflammatory reaction. So you get fluid in the alveoli, which allow the bacteria to grow better. You get coughing and consolidation, and that can spread to the blood stream. It is really a combination of the inflammatory reaction that the bacteria are eliciting and the host response that causes the disease. 28. Here is a picture of a brain with the person that had fatal pneumococcal meningitis. The brain is edematous. You see congestion from acute inflammatory reaction with pus at the base of the brain. 29. Pneumococcus is such an important disease. A vaccine was introduced in the 1970s that contained antigens against 23 of the different pneumococcal capsule types that cause disease in adults. Everyone over the age of 65, people without spleens, sickle cell anemia patients, or underlying lung diseases should get the vaccine. The problem in children is that they don’t respond well to a polysaccharide vaccine. So a new vaccine that has the seven most common serotypes was introduced in 2000. This is now part of the infant vaccination for all children. It is a combination vaccine that has the polysaccharide antigens along with a protein conjugate to improve the antibody response. 30. Viridans streptococci are found in oral cavity and upper respiratory tract. They are alphahemolytic, have no lancefield antigens, and usually do not cause problems. The main problems they do cause are by S. mutans, which polymerizes dextran for glucose in the development of dental caries. They can cause problems when they get into the blood stream and cause endocarditis. 31. Enterococcus used to belong to the Streptococcus. There are at least 12 different species. They are gamma-hemolytic most of the time. The one that we see the most in hospitals is E. faecalis. Enterococcus can be distinguished from Streptococcus in biochemical ways. They will hydrolyze esculin and PYR. They will grow in 6.5% sodium chloride like staph does. They are present in the intestine and enteric tract. They are nosocomial and opportunistic pathogens. They can Microbiology: Gram Positive Bacteria Haleigh Stidham pg. 3 cause peritonitis and UTIs. The big problem is the fact that they have become resistant to vancomycin and are easily spread and transmitted throughout the hospital. ….recording picks up on page 11, slide 33. GRAM POSITIVE BACILLI 33. LISTERIA MONOCYTOGENES: You take a semi-solid medium in a tube and take a needle with some bacterial colonies and stick it down into the medium. If the bacterium is motile, it will spread out through the tube. In the case of Listeria since it is an aerobic organism, it will make a fan-shaped umbrella shape at the top where there is more air. So, “umbrella motility” is a characteristic of Listeria. 34. CORYNEBACTERIUM: It is a large genius with a lot of different species. These are gram positive rods. A term associated is “Chinese Letters.” If you use your imagination, it looks like Chinese characters from the Chinese alphabet. They will grow on a lot of different media and are easy to grow in the lab. Most of the time we are not concerned about these organisms because they are contaminants. Corynebacterium is present of the skin and mouth. So you have to consider whether it is a contaminate or a pathogen. Catalase and oxidase positive and non-motile, and that’s how you can tell it apart from Listeria. There are two main pathogens in this group. C. jeikeium is an antibiotic resistant organism that is an opportunist in cancer patients and people with impaired immune systems. The other is Corynebacterium diphtheriae. 35. DIPHTHERIA: We don’t see diphtheria much in the United States because of vaccines. Vaccinations for children include the diphtheria vaccine. The diphtheria organism produces disease by an exotoxin. It grows in the throat like a Streptococcus and transmitted by respiratory droplets. It acts locally on mucous membranes. This is a pseudomembrane in the back of the throat. It has a potent exotoxin that kills the epithelial cells in the pharynx, and the dead cells break off. There is this big mass of necrotic cells, inflammatory cells, white blood cells, fibrin, bacteria, and everything else down there. This big, thick, tenacious membrane could literally enclose the trachea and cause asphyxiation. That is the pathogenesis of this disease, and it is all due to the exotoxin. The toxin can actually spread to other organs too and impair protein synthesis. By shutting down protein synthesis, you literally shut down all the cell metabolism and the cell will die this way. The way the vaccine works is by a toxoid, which is antigenetically similar to the diphtheria toxin. So when you give a toxoid, the host recognizes this and makes antibodies that will cross react with the diphtheria toxin if you encounter it. Fewer than five case each year in the United States. Even Microbiology: Gram Positive Bacteria Haleigh Stidham pg. 4 though this is not a common disease, it is important to recognize this as an exotoxin-mediated disease that was essentially wiped out with the introduction of a toxoid vaccine in the 1940s. 36. BACILLUS: It is another organism that is ubiquitous in the environment—dust, soil, skin. We see these as contaminant organisms from time to time. Bacillus and Clostridium are the only two organisms that produce spores. Spores are environmentally resistant structures that allow the bacterium to survive indefinitely. When the environment is favorable again, they will begin to grow again. Gram positive bacilli, motile (big grey colonies), beta-hemolysis, catalase positive. It is an agent of food poisoning. B. cereus spores can be found in rice, grains, macaroni and you ingest these spores and get food poisoning. B. cereus also causes ocular infections. Anthrax is the one that we are mostly worried about. Cows are vaccinated against this disease since it is common in animals. Our protection from anthrax changed seven years ago when anthrax spores were mailed around the US. Anthrax is an ideal, successful agent of bioterrorism. It is very easy to grow, turn it into spores, put some in an envelope, and then open the envelope and it flies up in the air, you inhale it, and then you get inhalational anthrax. 37. Here is an endospore (arrow) and that is the part that will survive. You can also see these spores on a gram stain. 38. You can get different kinds of anthrax. Cutaneous anthrax is from handling animal hides that were contaminated, and you get a lesion on the skin. The more severe form is inhaling the anthrax, and you get respiratory anthrax which has a high mortality. If you go into the military, you get the anthrax vaccine. It is not recommended to give the vaccine to everyone because it has side effects. Unless there is bioterrorism, you shouldn’t give everyone the vaccine. 39. The way anthrax produces disease is by a number of different exotoxins that it secretes. It has a protective antigen (PA) that binds to cells. It binds to the cell and allows the other two toxins to get into the cells. The edema factor (EF) is an adenyl cyclase and causes fluid to accumulate and inhibit immune function. The lethal factor (LF) actually kills the cell and stimulates cytokines. These three exotoxins damage cells, and that’s why you get the severe clinical manifestations. 40. The vaccine is made from an avirulent strain of anthrax. When you inject the vaccine with its surface antigens, the body recognizes this and makes antibodies to it. If you are exposed to the anthrax organism, it will rapidly send out antibodies to destroy the anthrax bacteria before it has a chance to make all of its exotoxins. Now when we see anthrax in the clinical laboratory, we have to do a beta-hemolytic test and a motility test so we can say it’s a bacillus species and not anthrax. If we have any doubt, we have to send it to the public health lab to have it identified. We will see all these organisms next week in the lab (with the exception of anthrax). Microbiology: Gram Positive Bacteria Haleigh Stidham pg. 5