GAP Analysis
advertisement

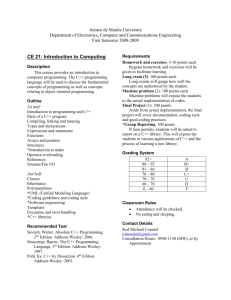
GAP Analysis Program Name/School: Office Technologies Medical Coding Certificate/Allegany College of Maryland Length of Program: Please identify in weeks/months the time typically needed to complete the coding certificate. This is a one year/2 semester program comprised of 30-31 college credit hours. Contact Name, &Title: Mrs. Peggy Hughes, Program Director Phone: 301-784-5319 Email: phughes@allegany.edu Program does not indicate if they seek Comprehensive or Physician Coding Approval – please indicate such on the CEPA response. Model Curriculum: The column below represents the knowledge cluster components (KCs) of the model coding curriculum. Contact Hours Required Your program’s Contact Hours = Comprehensive Coding Program = Physician Coding Program Anatomy and Physiology Study of the structure and function of the human body systems Course needs to cover all body systems; ( lab not required) 45-60 45-90 Program Equivalent: NOTES: Please complete this column. Identify in which course this content is covered, and how many contact hours are devoted TO THIS CONTENT. Where you have combined multiple KCs into a single class you must identify how many hours of instruction are dedicated for each KC. Make your entries in blue font. Please use this column if there are comments you wish to provide about the program equivalents. Add your comments in blue font. Students are required to take a Biology Elective from the following list: Human Biology (3 credit) Principles of Biology (4 credit with lab) Human Anatomy and Physiology (4 credit with lab) Anatomy and Physiology of the Human (4 credit with lab) Note: A&P is a foundation course for the coding process and should be taken prior to the coding classes. Due to the 2-semester nature of our program, this course is taken concurrently with the Introduction to Medical Coding course. Oneyear certificate programs at our school are discouraged from having prerequisite courses as this would make them selective admission programs. Additionally, a large number of our students come to us on federal or state retraining funds (i.e. TAA, WIA, and voc. rehab). These funds are limited to 12 months of instruction. Adding prereqs to the coding certificate program would eliminate the ability of these students to enroll in the program. The majority of the students who are enrolled in the Medical Coding Certificate curriculum take the 3-credit Human Biology course. However, some of the students who graduate with a coding certificate are also enrolled in other 2-year allied health curricula that require the 4-credit biology electives. These students come from a variety of backgrounds including Medical Assistant, Medical Office Systems, and Pre-Nursing. I would prefer if the Med Term and Anatomy were not being taken concurrently with the intro to Coding class – does not state if these four options include a full body review (12 major body systems are required to meet domain) Medical Terminology Spell, define, and pronounce (through supplemental CD tools), medical terms as well as understanding the concepts of root/suffix/prefix word builds. Common medical terms of major disease processes, diagnostic procedures, laboratory tests, abbreviations, drugs, and treatment modalities. 30-45 34 of 45 (11 hours remain) Medical Terminology I—This is a 45 contact hour course that concentrates on building student understanding of basic medical terms including prefixes, suffixes and root words. Approximately 11 hours of this course are dedicated to the study of pharmacology as it relates to disease of the body systems that are studied in Medical Terminology I. Note: Medical Terminology is a foundation course for the coding process and should be taken prior to the coding classes. Due to the 2 semester nature of our program, this course is taken concurrently with the Introduction to Medical Coding course. Oneyear certificate programs at our school are prohibited from having prerequisite courses as this would make them selective admission programs. Additionally, a large number of our students come to us on federal or state retraining funds (i.e. TAA, WIA, and voc. rehab). These funds are limited to 12 months of instruction. Adding prereqs to the coding certificate program would eliminate the ability of these students to enroll in the program. 34 hours meets minimum – again concerned about student retention given course sequencing. Pathophysiology Specific disease processes By human body system Causes, diagnosis, and treatment of disease. 30-45 30 of 45 (15 hours remain) Medical Terminology II—This is a 45 contact hour course which further develops the student’s understanding of medical terminology, pathophysiology and pharmacology. Students concentrate more on the disease process and treatment during this course as they have already studied basic terminology in Med Term I. 2 hours per week are devoted to the disease process and 1 hour per week is devoted to pharmacology for these diseases. Note: Pathophysiology (Disease Processes) is a foundation course for the coding process and should be completed prior to the coding classes, or during the first coding class. Due to the 2 semester nature of our program, this course is taken in the second semester of the program as Med Term I (taken in the first semester) is a prerequisite for Med Term II. One-year certificate programs at our school are discouraged from having prerequisite courses as this would make them selective admission programs. Additionally, a large number of our students come to us on federal or state retraining funds. These funds are limited to 12 months of instruction. Adding prereqs to the coding certificate program would eliminate the ability of these students to enroll in the program. Patho in a medical term course; concern about depth of coverage. States 2 hours per week on patho; for how many weeks, again concern of depth of coverage for this important topic for coding – what textbook is used for disease process? Pharmacotherapy Emphasis is placed on the understanding of the action of drugs such as: absorption, distribution, metabolism and excretion of drugs by the body. Drug classifications Most commonly prescribed drugs What is a formulary 20-30 26 (11 hours Pharmo from MT-I) (15 hours Pharmo from MT-II) Medical Terminology I—(11 hours) This course introduces students to the study of pharmacology in relation to the organ systems diseases that are covered in this class. Students have one 3-hour class devoted to the study of general pharmacology along with an additional 8 hours that focus on the study of pharmacology for each organ system studied in Med Term I Medical Terminology II— (15 hours) This course combines instruction of pathophysiology and pharmacology with one hour each week devoted to the study of pharmacology as related to the disease process being taught during that week. Pharmocotherapy as inbedded in a MT course – what textbook is used, do the exams reflect this domain? CEPA results examination will answer these questions. Information Technology Introduction to Computers -Concepts related to hardware and software, the impact of computers on society and computer systems/data communications networks. Computer Software Applications in Healthcare Overview of commonly available software tools used in health care, including introduction to encoding tools and computer assisted coding software used in health care data processing today. Introduction to the electronic health record. (Recommend 45 contact hours) Intro to Computers may be waived through a pretesting placement process – for example testing level of competence of prior knowledge of Microsoft Office Suite, or else, a beginning computer course is required. Note: 75 (0 hours) 45 hours on Intro – being cancelled Fall 2007 30 - 45 30 hours on Front Office Application Students are required to take Computer Literacy (45 hours) which introduces them to basic e-mail, Internet, word processing, spreadsheet, data base and presentation software. Please see notes**. Medical Office Financial Management (30 hours) Students learn to use Medisoft Advanced Patient Accounting to perform a variety of front office skills including scheduling, patient registration, transaction entry, and billing procedure. Please see notes *. Students are required to use encoding software in Intermediate and Advanced Coding. This instruction is provided on an as needed basis in these classes at the beginning of the semester and students then use both Encoder Pro and 3M to assign codes to coding problems and cases throughout the semester. NOTE: The intent of the Computer software applications in healthcare knowledge cluster is to introduce the concepts of computer technology related to healthcare and the tools and techniques for collecting, storing and retrieving healthcare data. Taking a keyboard course, or a standard intro to computers course will not satisfy this KC. *Medical Office Financial Management is currently undergoing a curriculum change that will result in changing the objectives to cover not only Medisoft but also variety of software packages available for both inpatient and outpatient administrative functions, including encoders and electronic health records and basic Microsoft Office functions. The course will be renamed Administrative Medical Software and will be available in the Fall 2007 semester. **Computer Literacy--We will be deleting Computer Literacy and adding the computer concepts to the Administrative Medical Software class. This will reduce the number of contact hours from 75 to 30. This change will be effective Fall 2007 Where does student gain knowledge about eHIM, imaging (which affects coding processes) and grouper software? This domain appears underrepresented as planned. Introduction to Health Information Management & Healthcare Data Content and Structure Emphasis is placed on content and components of the health record including: Content of the health record Documentation requirements Primary vs. secondary records Legal/ethics issues Privacy, confidentiality and computer security HIPAA requirements Release of information Code of Ethics of the AHIMA Standards of Ethical Coding of the AHIMA Healthcare Delivery Systems & Computer Applications in Healthcare (eHIM) A thorough understanding of the types and levels of Healthcare Delivery Systems in the U.S., and of the governing bodies that regulate the HIM processes, and understanding the eHIM environment: Organization of healthcare delivery Accreditation standards Licensure/regulatory agencies Identify the issues involving the migration 45-60 45 Introduction to Health Records—(30 hours) This course introduces students to health records in a variety of settings including inpatient, ambulatory surgery and physician office. The students do a unit on HIPAA as well as legal issues surrounding health records both in paper and electronic format. Will need to see how much of the content reflects acute care needs – this appears to be designed as an outgrowth of a medical office environment – will program grow to include necessary knowledge of acute care processes? Is the RHIT on staff being consulted in the development of this domain? Principles of Medical Insurance—(15 hours) This course includes information about HIPAA in relationship to reimbursement issues. We also look at ethical issues surrounding coding and billing in addition to requirements for release of patient information and computer security. 30-60 30 Introduction to Health Records—(15 hours) In this course we spend approximately 15 hours looking at healthcare delivery systems models and organization in the United States, accreditation standards and accrediting and licensing organizations for each healthcare setting. We also look at electronic health records. These subjects are covered in addition to those required by the Introduction to Health Information Management & Healthcare Data Content and Structure knowledge cluster. Medical Office Financial Management—(15 hours) Students in this class look at various types of medical office software, encoders and electronic health records systems. The name of this course is being changed to more accurately reflect the nature of the course (Administrative Medical Software). Please see the note about this curriculum change in the Information Technology knowledge cluster. NOTE: As a separate course, this is optional for Physician Coding Programs, but required for the Comprehensive Coding Programs. The fundamental KCs in this domain should be introduced to the Physician Coding Program student in their Medical Office Procedures course with special emphasis on the agencies and practices that affect physician coding and billing issues. Program already used the hours in previous domain – this reflects strong background on physician practice environment – this domain deals with acute care regulatory processes – see bullets in column one. These are the areas that must be covered to satisfy this domain – at this time this is a non-represented domain. from a paper-based HIM to an electronic HIM The student should be aware of the major acute care environment vendors and their system strengths. Knowledge of different types of encoder systems, and the effect of natural language processing on the coding process. Basic Diagnosis Coding Systems Detailed Instruction in: Student will learn about the International Classification of Diseases ICD-9-CM, how to code, and guidelines for usage. Volumes I, II, and III The topic of encoders and electronic health records and other healthcare computer applications is interspersed in many of our courses including Intro to Health Records, Medical Office Financial Management, Principles of Medical Insurance, Intermediate and Advanced Medical Coding. 45-60 15 Introduction to Medical Coding--Basic diagnostic coding is covered in a combination course where students spend the first half of the semester working on basic procedural coding and the second half of the semester working on basic diagnostic coding. We currently offer this general introduction course to students in a variety of allied health courses including Medical Assistant and our 2-year Medical Office Systems course. **Please see the notes column. Note: Coding courses must include hands-on experience to computerized encoding systems – local and distance students must have equal access to the encoding application. The encoder may be introduced in the basic or advanced coding coursework, or both. Explain how your program uses encoders: Encoders are introduced to students in the Intermediate Medical Coding course. We use both Encoder Pro and the 3M Reimbursement System. Once students have basic knowledge of these encoders, they are used in both Intermediate and Advanced Coding courses to assign codes to coding worksheets as well as coding cases. ** We currently offer this general introduction course to students in a variety of allied health courses including Medical Assistant and our 2-year Medical Office Systems course. In completing the gap analysis, we realize that we are missing 45 hours of basic coding that is vital to the coding students’ success. Therefore, we are adding a new course to our curriculum which will be available in the Fall 2007 semester that will increase the number of hours for both basic diagnostic and basic procedure coding. The new course, Acute Care Coding, will be specifically for students in the coding curriculum and will include instruction specifically geared toward inpatient and ambulatory care coding. Since the primary focus of this course is the acute care setting, we will spend 30 hours in ICD-9-CM, concentrating instruction around the official coding guidelines. Only 15 hours; new course being added. Need syllabi, textbook, and sample testing instruments with CEPA manual to evaluate this course and requirement. Agree, it is critical that enough time be spent of coding skills development. Basic Procedure Coding Systems 45-60 Student will focus on Basic HCPCS coding, with a focus on CPT-4 coding (Anesthesia, E&M, Surgical, Pathology/Laboratory, Radiology and Medicine) and HCPS II codes. 30 Introduction to Medical Coding--Basic procedural coding is covered in a combination course where students spend the first half of the semester working on basic procedural coding and the second half of the semester working on basic diagnostic coding. We currently offer this general introduction course to students in a variety of allied health courses including Medical Assistant and our 2-year Medical Office Systems course. **Please see the notes column. Note: Students must attain a minimum of 45 hours of diagnosis training, and an additional 45 hours of procedure training. Programs that combine the diagnosis and procedure KCs into a single basic coding course should have a minimum of 90 hours of instruction. ** We currently offer this general introduction course to students in a variety of allied health courses including Medical Assistant and our 2-year Medical Office Systems course. In completing the gap analysis, we realize that we are missing 45 hours of basic coding that is vital to the students’ success. We are adding a new course to our curriculum which will be available in the Fall 2007 semester that will increase the number of hours for both basic diagnostic and basic procedure coding. The new course, Acute Care Coding, will be specifically for students in the coding curriculum and will include instruction in coding ambulatory surgery and emergency room visits. The course will add 15 contact hours to procedural coding which will then bring this total up to 45 hours Only 30 hours; new course being added. Need syllabi, textbook, and sample testing instruments with CEPA manual to evaluate this course and requirement. Has not met minimal number of hours in procedural coding – will need to see the final categories from the CEPA to see if program will be compliant. Intermediate (or Advanced) Diagnosis Coding Having attained basic coding skills, this course focuses on case studies using more complex code assignments to determine the correct diagnoses. Students should be exposed to medical records and learn how to interpret actual charts. Student should be introduced to diagnostic based prospective payment groupers: DRG, APR-DRG, & RUGS. An introduction to International Classification of Diseases ICD-10-CM, and other diagnosis coding systems (DSM-IV, ICD-0) Introduction to Systematized Nomenclature of Medicine (SNOMED) – Includes a brief overview of its role in the health care delivery 45-60 40 (30 hours from IMC) (10 hours from MCPP) Intermediate Medical Coding—30 hours Intermediate Medical Coding is a 60 contact hour course in which students learn to assign codes from both CPT and ICD-9-CM to basic, intermediate and advanced case studies. It is in this class that students also are introduced to Encoder Pro and the 3M encoder systems. Students gain a working knowledge of both types of encoders while also sharpening their coding skills using coding books. We also cover HCPCS Level II coding and payment groups. Medical Coding Professional Practice—10 hours This course is a 60 contact hour course in which the majority of time is spent in a simulated coding environment. However, 10 hours of this class at the beginning of the semester is spent introducing students to the various coding references that are available to them (Coding Clinic, CPT Assistant, etc) as well as going over the basic changes that will accompany ICD-10 and ICD-10-PCS. We also touch on SNOMED and its importance in the future of electronic records. Note: Students must attain a minimum of 45 hours of intermediate/advanced diagnosis training, and an additional 45 hours of intermediate/advanced procedure training. Programs that combine the diagnosis and procedure KCs into a single intermediate/advanced coding course should have a minimum of 90 hours of instruction. Physician programs will emphasize physician based coding issues while comprehensive programs will emphasize acute care and ambulatory setting coding. Note: Coding courses must include hands-on experience to computerized encoding systems – local and distance students must have equal access to the encoding application. The encoder may be introduced in the basic or advanced coding coursework, or both. Explain how your program uses encoders Encoders are introduced to students in the Intermediate Medical Coding course. We use both Encoder Pro and the 3M Reimbursement System. Once students have basic knowledge of these encoders, they are used in both Intermediate Medical Coding and Medical Coding Professional Practice courses to assign codes to coding worksheets as well as coding cases. system as the basis for an electronic health record , Even with the combining of hours from two different courses, the program fails to meet the absolute minimum of 45 contact hours for diagnosis coding – see if this is resolved in the CEPA. Intermediate (or Advanced) Procedure Coding 45-60 Using case studies, students should practice more complex procedure code assignments with ICD-9-CM and CPT-4.. Student should be introduced to procedure based payment systems: RBRVS, E&M codes, and APC assignments and the impact coding and sequencing has on reimbursement. 40 (30 hours from IMC) (10 hours from MCPP) Intermediate Medical Coding—30 hours Intermediate Medical Coding is a 60 contact hour course in which students learn to assign codes from both CPT and ICD-9-CM to basic, intermediate and advanced case studies. It is in this class that students also are introduced to Encoder Pro and the 3M encoder systems. Students gain a working knowledge of both types of encoders while also sharpening their coding skills using coding books. We also cover HCPCS Level II coding and payment groups. Medical Coding Professional Practice—10 hours This course is a 60 contact hour course in which the majority of time is spent in a simulated coding environment. However, 10 hours of this class at the beginning of the semester is spent introducing students to the various coding references (CPT Assistant, Coding Clinic, etc) that are available to them. We also spend time evaluating E&M worksheets, going over the difference between the 1995 and 1997 E&M Guidelines, and look at sequencing procedures to maximize reimbursement. Note: Students must attain a minimum of 45 hours of intermediate/advanced diagnosis training, and an additional 45 hours of intermediate/advanced procedure training. Programs that combine the diagnosis and procedure KCs into a single intermediate/advanced coding course should have a minimum of 90 hours of instruction. Physician programs will emphasize physician based coding issues while comprehensive programs will emphasize acute care and ambulatory setting coding. Even with the combining of two courses, the program fails to meet minimum number of contact hours for procedural coding – see if this is resolved in the CEPA. Reimbursement Methodologies (30 – 45 contact hours) 30-45 Prospective payment system Diagnosis Related Groups Ambulatory Payment Classifications ASC Groups Resource Based Relative Value Scale Third party payers Billing and insurance procedures Explanation of benefits Quality Improvement Organizations (QIO) and their role in the payment process Charge master description and maintenance Managed care/capitation Compliance issues Health plan claims processing and coding Billing for healthcare services using codes Auditing and monitoring the coding process for regulatory compliance Medical Office Procedures (45 – 60 contact hours) Provide a working knowledge of concepts, processes and procedures encountered in the physician office management setting, to include: physician payment systems, scheduling, End of Month Reporting, insurance processes, EOB explanation, series billing, filing appeals, and auditing and monitoring of coding for regulatory 30 Principles of Medical Insurance—In this course we concentrate on basic principles of billing in both the inpatient and the outpatient setting. The students are introduced to all major third party payers as well as billing processes and collection procedures. NOTE: As a separate course, this is optional for Physician Coding Programs, but required for the Comprehensive Coding Programs. The fundamental KCs in this domain should be introduced to the Physician Coding Program student in their Medical Office Procedures course with special emphasis on the reimbursement issues that directly affect physician coding and billing. Does this course reflect groupers such as those noted on bullets? It appears an outgrowth of Medical Office program – will need to see if the domain is met in the CEPA for this category of content. The intent of this domain is beyond processing a bill – it is understanding the critical nature of grouping assignments to inpatient and outpatient coding in the acute care environment – failure to appreciate the coder’s obligations can lead to criminal violations. 45-60 This knowledge cluster is covered in Principles of Medical Insurance and Medical Office Financial Management courses that have been used in the Reimbursement Methodology and Healthcare Delivery System/Computer Applications in Health knowledge clusters. NOTE: Optional for Comprehensive Coding Programs but required for Physician Coding Programs. It is in this course the Physician Coding Program student covers the Reimbursement Methodology and the Healthcare Delivery System/Computer Applications in Healthcare knowledge clusters (KCs) from the perspective of physician practice. In this course, the student must have an opportunity to experience hands-on learning with a computerized physician office application. Local and distance students must have equal access to the practice management application. compliance. Professional Practice Experience/Practicum/Internship (40 - 60 dedicated hours) 40-60 40 Field Based PPE: To provide the student with coding practice experiences in a hospital, physician’s office, clinic or other healthcare setting with directed projects common to a clinical coding specialist on the job. Virtual PPE: Review presentations from coding specialist guest speakers (CCS, CCS-P) either prerecorded or live. Practicum hours to focus on building speed and accuracy using paper and scanned medical records. Comprehensive Coding Program = 495 program hours Note: Lab hours that focus on coding workbook assignments in the basic and intermediate coding courses do not satisfy the virtual PPE practicum hours. Technically this is a 60 contact hour class, however, for the first 20 hours of the semester, we spend time reviewing intermediate coding principles along with the use of E/M worksheets, coding references, and official coding guidelines as well as the future of coding. The virtual PPE plan fulfills this domain – the CEPA will be reviewed to see how students are exposed to actual records, and how the encoder systems are used in their assignments. Students should gain experience coding a variety of record types including: acute care, ambulatory surgery, emergency records, and physician office. Practicum hours should be based on analysis of actual medical records with a learning focus on coding accuracy and speed. Programs should calculate their total contact hours and indicate the total hours in the program equivalent column . Minimum Contact Hours: Physician Coding Program = 465 program hours Medical Coding Professional Practice—Due to the rural area that Allegany College of Maryland serves, we have been unsuccessful in contracting providers that will serve as internship sites in which the students would actually gain coding experience. Unfortunately, most of our sites would only allow student to file patient records. As an alternative, we have set up a coding simulation wherein the students come to the coding lab and work on coding a variety of sample records including inpatient, emergency room, ambulatory surgery, and physician office records. The students apply ICD-9-CM, CPT-4, and HCPCS Level II codes as needed to these sample records. 480-525 Program needs to either add considerable content to meet acute care needs, or should pursue a Physician Coding Certificate approval which would free them from being accountable for the depth of materials. SYNOPSIS OF CURRICULUM Include all courses required in their appropriate sequence Course Title: Primary Instructor Total Contact Hours: Lab Hours Component: Biological Science Elective Various instructors 45-90 *45 Medical Holly Terminology I McDonald, RN, BSN Introduction Cindy to Medical Zumbrun, Coding MEd, RHIT, CCS-P Introduction to Cindy Health Zumbrun, Records MEd, RHIT, CCS-P Computer Various Literacy instructors Medical Holly Terminology McDonald, II RN BSN Intermediate Cindy Medical Zumbrun, Coding MEd, RHIT, CCS-P Medical Cindy Coding Zumbrun, PPE Hours Component: Comments *If the student takes the 4-credit biology electives with labs, the lab component is 45 hours. However, students who choose to take Human Biology will not have the lab component 45 45 45 45 45 60 60 *60 *40 *40 hours of this lab class are devoted to a simulated PPE with students Professional Practice Principles of Medical Insurance MEd, RHIT, CCS-P Cindy Zumbrun, MEd, RHIT, CCS-P Medical Cindy Office Zumbrun, Financial MEd, RHIT, Management CCS-P independently coding simulated records from a variety of healthcare settings 45 45