Report Template For Children And Adolescents
advertisement

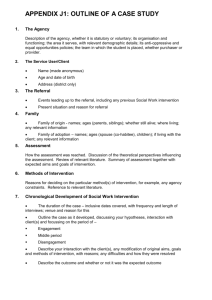
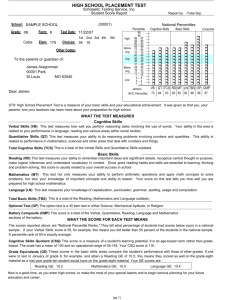
Report Template for Children and Adolescents – copyright Carol Oster, Psy.D. clo_60035@yahoo.com or 847-962-4089 for questions and permissions Leave room at the top for letterhead. Delete instructional comments in blue and red from your final report. They are there to help you think about what to write. Blue text is specific to cognitive assessment courses or basic to all reports. Red text is specific to objective and projective personality assessment courses. Throughout the report, strive to describe the child, not the tests. Pay attention to developmental stage: the child is on their way to peak performance. Where are they on that journey? Maintain a developmental, hopeful tone and future focus, as appropriate to the situation. PSYCHOLOGICAL EVALUATION (Confidential) Name: Date of Birth: Age: Referred by: Place of Examination: Date of Examination: Date of Report: Examiner: Give age in years and months. Spell name of month. Spell name of month Spell name of month Reason for Referral: Before beginning any assessment, clarify the questions to be answered by the assessment. Include the child's and parents’ questions, as well as those of third parties. The clearer the reason for the assessment is, the more helpful you can be to the child. Common referral questions are to clarify diagnosis, to assist in differential diagnosis, to identify a learning disability, to understand the child’s academic performance and help them learn better, to determine whether the child is qualified for a particular academic program, to assist in treatment planning, and to answer a particular question or set of questions. The better-delineated the referral question is, the more targeted – and on-target – the assessment, report, and recommendations will be. Procedures: List any procedures completed, in order of administration. In the standard approach to assessment, procedures are administered in a “peel the onion” order. For assessment courses in graduate school, include “Clinical Interview” in your list, even though you may not conduct a formal interview, to reflect your collection of any background information. There is not really a “standard battery” for assessing children. An assessment for learning disabilities purposes should include intelligence, achievement, and emotional components, tailored to assess the components of the possible problem – and to rule out competing hypotheses. That is, it might be a reading disability – or it might be depression, anxiety, OCD, and so on… so be sure to adequately gather Child Name 2 information for and against alternative hypotheses. The traditional “standard battery” consists of those tests marked with a *. Delete the * in the list below. Answering the referral question will usually require that the list be altered to include more, fewer, or different assessment methods. Clinical Interview (specify interview of parents, child)* Wechsler Intelligence Scale for Children - IV (WISC-IV)* Woodcock Johnson Test of Achievement – III Bender-Gestalt Test* House-Tree-Child* Incomplete Sentences Blank* Minnesota Multiphasic Personality Inventory – Adolescent Version (MMPI-A)* Thematic Apperception Test (TAT)* Rorschach Inkblot Method* Others as needed to answer the referral question, such as review of educational records, review of prior testing, the Gray Oral Reading Test, Conners’ ADHD scales, Achenbach Child Behavior Checklist, and so forth. List contacts with teachers, social workers, pediatricians, etc. Background Information: Throughout this template, I am referring to both children and adolescents when I say “child”. Include here information regarding the following topics, as relevant to the purposes of the assessment. This list is given to provoke your thinking and to encourage you to be thorough, wherever such thoroughness is warranted: Identifying information including age, gender, ethno-cultural identity, year in school. Describe the family context. Be careful about reporting that the child is adopted, or that one parent or another is a stepparent, or that “Mom and Dad” are actually “Grandma and Grandpa”. If the child has not been told, you might not want to put it in writing. What is the child’s birth order? Do not name relatives other than parents. Instead, refer to them by relationship; e.g. “older brother”. Presenting complaint and symptoms; o History of the presenting complaint including onset, duration, course (times when it’s better or worse); o Whether the problem seems to be improving or worsening as the child gets older; o Prior treatment efforts and success of these; o The parents’ and child’s (teacher’s, pediatrician’s?) conceptualization of the problem; Relevant personal history o Critical events in development and timeliness of meeting developmental milestones Child Name 3 o Life stressors in the time period preceding the presenting problem and preceding the referral for evaluation o Changes in the family situation prior to the onset of the symptoms (birth of a sibling, older sibling left for college or marriage, family moved, best friend moved away, finances changed, parent got ill, etc.) Academic history o Grade in school o School performance a/e/b report cards, teacher’s written comments over time, GPA, recent work handed in and graded, and similar hard data o How the child performs in reading and math (basic skills) as well as other subjects – parent, teacher and child perspectives. o Best/worst classes. Are those constant? Time of day those classes are scheduled; teacher characteristics; other factors affecting performance in those classes (ask the child!). o What the child recalls about learning to read and do math; what is hard/easy for them from their perspective; teacher and parent perspective; evidence in submitted work. o Whether any special assistance or accommodation has been needed or granted before this assessment, and effect of that intervention. o Parental expectations and standards o Setting effects: study area at home, environmental disruptions, etc. o Permission to contact school, if relevant and necessary to the evaluation o Review of previous psycho-educational assessments, including results of both standardized group achievement tests (E.g., Terra Nova tests) and any previous individual ability or achievement testing. Look at this chronologically for clues as to the evolution of the presenting problem or question. Occupational history for adolescents where applicable o What jobs the adolescent has had Functional job analysis – what do they actually DO on a daily, weekly basis. What knowledge, skills, and attitudes are required for success and happiness on the job? Make sure you actually understand what the adolescent is supposed to do when he or she is at work. Don’t assume. Ask. What jobs they have previously had Level of accomplishment a/e/b promotions, added responsibilities, awards, etc. The child’s report of how easy or difficult it was to learn the job What they feel they do well and not so well What they like and dislike about the job o Quality of interactions with peers, supervisors, and supervisees o Parental expectations and standards o Whether any special assistance or accommodation has been needed or granted before this time o Permission to speak with employer if relevant and necessary to the evaluation Child Name 4 Social history o Report in writing only what is 1) relevant to the referral question, and 2) appropriate to share with a general audience. Some of this is none of a school’s business. Bear in mind that adolescents between 12 and 18 may be able to suppress some information they share with you – even from their parents. Know the law; follow it; consider the good of the child and need to know before you put something in writing or share it verbally. o Number and length of friendships; breadth of the group; whether friends are considered positive influences by parents and teachers; whether the older child/adolescent has changed friends lately or at the onset of the problems; any traumas within the friendship group, whether to this child or others; whether the child is popular, accepted, ostracized, bullied, etc. o Typical social activities and type and level of involvement in extracurricular activities (too few, too many, variety, level of commitment, task and time demands of the activity, etc.) o Whether the older child or adolescent is “dating” (check idiosyncratic meaning); who they date; history of break-ups (who, why, coping method, impact?). Ask a dating adolescent if he/she is sexually active, and if so, ask about birth control, STD protection, pregnancies/abortions, and so forth. Consider such information in your assessment, but do not put it in a written report without a clear, legal, ethical rationale for doing so. o Success of social activities a/e/b length and persistence of relationships, cooperation and reliability in group activities (e.g., gets to practice on time, practices the instrument, etc.) o Parental expectations and standards (too loose, too lax, high standards, standards adjusted for child’s ability, temperament, and personality?) o Satisfaction/dissatisfaction with friendships, community, dating o Quality and appropriateness of interaction with members of peer group, family, and community o Any difficulties – onset, course, duration, patterns, situational analysis o Capacity to tolerate being alone; demonstration of appropriate judgment and impulse control in history Medical and developmental history o Age at which major developmental milestones were attained (crawling, walking, first word, sentences, etc.) o Physical skills: walking, bike riding, coloring and writing, athletic or musical skills; comparison with peers, parental expectations o Congenital or neonatal history, congenital or inherited neuro-muscular problems such as cerebral palsy, dystonia, and the like o Childhood illnesses, particularly ear infections, asthma, injuries, hospitalizations, chronic illnesses, anything that could interfere with school attendance, either episodically or cumulatively o Later illnesses, especially… Chronic illnesses Diabetes Thyroid problems Child Name 5 Metabolic problems Fibromyalgia, juvenile or osteoarthritis, carpal tunnel, or other pain or functional disorder/disease MS or other degenerative disease/disorder Cerebral palsy, dystonia, “tics” or other neuromuscular disorder o Any hospitalizations What for and when Length of hospitalizations Any problems, complications, or sequelae? Success of treatment o Hearing, vision, orthotic, or vestibular problems, Impact on presenting problem Corrective measures or treatment Efficacy of corrective measures Whether the child is using those corrective measures at the time of testing o Medications taken previously or currently; Type and dosage What for Efficacy Side effects the child experiences How long they’ve been taking it Whether they take it regularly as prescribed Last time they took it (date and time) If today, “Is it working? How long does it take to “kick in”? o Substance use: Alcohol and street drugs the child “has tried” When started, largest amount consumed and when; current types and levels of use in dosage and exact frequency Last use Effects and impact Side effects Legal issues (Consider a formal substance abuse history where indicated.) Prior efforts to quit Social system’s reactions to use o Last physical checkup Results Whether parents have discussed the presenting problem with the pediatrician Parents’ and child’s relationship with medical professionals o Permission to contact physician if relevant and necessary to the evaluation Psychiatric/Psychological history o Previous psychiatric or psychological treatment With whom, what for, when and for how long Efficacy Child Name 6 What worked, what didn’t What the child and parents liked/disliked Long-term outcome Relationship with treating clinicians o Prior psychological or psycho-educational assessment or testing When? Why? Results – get copies if at all possible Interventions and efficacy Family history Adopted or related by blood (careful!)? Academic accomplishments and problems in siblings, parents, grandparents, aunts & uncles (think genetics, familial demands, social modeling) Occupational functioning in parents, grandparents, siblings (predicts target functioning level or self/other expectancies) Relevant medical history, Ps, Gs, Sibs Psychiatric history, Ps, Gs, Sibs, As & Us Level of acculturation of family Length of time in US; child and parent “generation” in US English-language fluency Conflict or acceptance of US cultural norms relevant to the referral question or diagnoses under consideration. Permission to speak with family members if relevant and necessary for the assessment Note: Do not name family members. Refer to them by relationship only. E.g., “Mr. X’s uncle” versus, “John Smith, Mr. X’s uncle”; “older brother” versus “Tom Smith”, Mr. X’s older brother”. Behavioral Observations: This section should describe what the child brings to the testing. It reports your general observations of the child. Observations are what a video recorder would pick up. Thus, they are a form of objective data. Keep this section descriptive, not evaluative or conclusive. This not the place for diagnostic statements. This section also does not include the child's response to specific test stimuli. That belongs under "results". To clarify, “John became increasingly anxious as testing progressed and refused to complete the some tasks” does belong here, as it describes the child’s ongoing anxious state. “Mary laughed upon being presented with set 4 of the Picture Arrangement subtest, saying it reminded her of her mother” does not belong here (if, indeed, it is useful at all!) because it is a response to a specific test item. In addition, “John appeared to be using a kinesthetic approach to Matrix Reasoning,” belongs under test results because it indicates not a state, but an approach to the particular task. Finally, “Mary appeared to be suffering from a generalized anxiety,” is a diagnostic conclusion, and belongs at the end of the report, after test results (the data that informs the conclusion) have been presented. Child Name 7 DO include here the following: Setting constraints on testing (e.g., two or more sessions, background noise, interruptions in the testing, interference, etc.). Generally, you want to relate any environmental conditions that might have made it difficult for the child to put forth his/her best effort, or that might have affected the validity of testing. The parts of the Mental Status Exam that are readily observable belong here. For example, discuss the child’s appearance if it is noteworthy or related to referral question. Note his or her orientation to person, place and time, especially in settings where that might be in question, such as psychiatric, forensic, or rehabilitation/neurological settings. Observe speech quality, e.g., intonation, modulation, pressure, fluidity, speech problems, as well as reticence or garrulousness. Describe the child’s affect (visible display of emotion) in regard to feelings displayed, range of expressiveness (flat, labile, animated/normal), and appropriateness to content during the interview and formal testing. List any reported or observed handicaps to sensory-motor functioning: glasses or contacts (to correct what?), hearing aid, gait or motor problems, hand tremors, etc. Report on the child’s ideation evident in behavior, such as overtly anxious statements, suicidal/ homicidal comments, evidence of delusional or hallucinatory thinking evident in behavior (as opposed to evident in test results). Report on the child’s ability to separate from parents, and his/her apparent attention and concentration, cooperation, persistence, and effort – the conative factors involved in performance. Then make a statement about your sense of the validity of results, based on the full collection of behavioral observations and the child’s history. For example, you could say, "Based on John’s behavior, and his apparent effort and cooperation, test results are likely to be an (accurate, underestimate) assessment of his (typical functioning, functioning at this time, or potential)". Note the parentheses. Throughout this teaching template, parentheses suggest alternatives. Note especially the last set in the above paragraph. “Typical functioning” means you think this is the way the child functions generally, and that the test results are not unduly influenced by situational factors. “Current functioning” means this is the way the child is functioning NOW, but the results may not indicate prior functioning or predict future functioning. This is appropriate when, for example, you are testing a child who is recovering from brain injury, or who is severely depressed. “Potential” indicates you are trying to predict how the child will function in the future, such as on the job, or in school. For example, you might be evaluating a child for accommodation on the job, and the test results may reflect about how well the child can be expected to perform at his/her best, provided you were able to motivate him/her to perform well, and there were no situational or other constraints. Some examples: “Based upon John’s obvious cooperation, persistence, and effort, these tests results are likely to accurately reflect his true potential.” Child Name 8 “Based on the clear and persistent discrepancy between John’s test responses and his behavior during breaks from the testing, the test scores are likely to reflect his attempt to manipulate the outcome of the assessment rather than the “truth” about his capabilities.” (Such as happened in one personal injury assessment I observed.) “Based upon John’s lack of cooperation and his difficulty with concentration and persistence, these results likely underestimate his true potential. However, they may accurately reflect his functioning under the current stress of family disruption.” “Based upon Mary’s effort, concentration, and cooperation, these results likely accurately reflect her functioning under the influence of her depression.” “Based upon the number of interruptions and the less than optimal testing conditions, these results likely underestimate Mary’s true ability, despite her cooperation, effort, and obvious desire to succeed.” “These test results may slightly overestimate Mary’s true abilities, particularly on Performance tasks, due to her familiarity with the test materials.” “John’s history and his cooperation with the testing procedure suggest that the results reflect his typical functioning.” Cognitive Functioning: Select appropriate phrases. Note: here and throughout, underlines are space holders. Do not use underlining in the report itself. Consider using subheadings: General Ability, Academic Skills and Achievement, Reading Problems, and so forth, as appropriate to the referral question, rather than the general heading above. (Child’s name)'s performance on the WISC-IV places (him/her) within the (average/ above average/ superior/ borderline/ extremely low) range of intellectual functioning. (His/Her) general intelligence of ___ is higher than that of ____% of (children/adolescents) (his/her) age. This last statistic is called a percentile rank. Don’t confuse it with being “95% sure of your results.” An IQ of 90 to 109 is average. Were (s/he) tested again under similar circumstances, there is a 95% chance that (his/her) score would fall between ___ and ___. The last phrase is the “confidence interval.” You are 95% confident that the child’s “true score” falls within the given interval of scores. Contextualize the child’s general ability by referring to those things in the child’s life that fit with their overall ability. Discuss the implications of the child’s general ability for the referral question. The WISC-IV also yields the following Index Scores and subtest scales scores. Index scores of 90 to 109 and scaled scores of 8 to 12 are average. (Child) obtained the following scores. The following table should appear on one page in your final report, with no break. If necessary, include a page break before the table. In your report, cell boundaries of the table will not print. If you TAB over to each cell, you will be able to Child Name 9 replace the data below with your child’s data. More data might appear in your table if you are using the WISC-IV Integrated. Index Verbal Comprehension Similarities Vocabulary Comprehension Information Word Reasoning Working Memory Score 108 %-ile 70 Index Perceptual Reasoning (101-114) 12 13 10 11 14 75 84 50 63 91 Block Design Picture Concepts Matrix Reasoning Picture Completion Block Design w/o time bonus 107 68 Processing Speed (99-114) Digit Span Letter-Number Sequencing Arithmetic 12 11 75 63 Symbol Search Cancellation 13 84 Coding CA Random/Structured Cued/Free Recall Score 127 (117-132) 14 12 17 10 15 %-ile 96 97 (88-106) 11 11 42 8 10/11 25 50/63 >25% 91 75 99 50 95 63 63 In interpreting results of intelligence tests – or any other test that has subscores – you can take a top-down or bottom-up approach to interpretation. The best approach is to do both simultaneously. Think about the aggregate scores as most reliable, but also attend to the component scores that contribute to that aggregate in interpreting it. So… the FSIQ is the best predictor of a child’s general ability, but the score accurately reflects his or her overall ability only insofar as it reflects a unified construct. Be careful here. Any difference between index scores or subtests that is not statistically significant is not clinically significant, under most circumstances. If the difference is too small to reach statistical significance, it is unlikely to be detectable to the observer or to the child themselves, or to make a difference in the child’s functioning, and thus will not have any meaning in describing the child’s behavior. Let me make this clear: if there is no statistical difference, you treat the scores as identical, and do not discuss the (illusory) difference in the report. Also, there is no such thing as “almost” statistically significant. It either is or is not. Do not interpret as useful, distinguishing, or relevant a difference that approaches but does not equal or surpass the cut off for significance! These cautions are necessary both because our tests are not perfectly precise tools, and because people are not perfectly consistent over time. When discussing each “index area”, first identify where the child’s ability is relative to the general population (normative range). A score that is significantly different from average (<90 or >109 for IQ and index scores) are strengths or weaknesses relative to the general population, regardless of how they compare to the child’s overall ability. When discussing significant discrepancies between index scores, consider the child’s overall Child Name 10 ability the “baseline”. Index scores significantly different from that baseline represent relative strengths if higher, or relative weaknesses if lower. “Relative” means relative to the child’s own average – the “local norm”. For example, if the child’s FSIQ is 140, and Processing Speed is 120, PSI may be a relative weakness compared to the child’s other scores, but it is still significantly stronger than the score for the average individual the child’s age. If you only say it is a weakness, the reader assumes the child can’t do things as well as the average child his/her age. You must include the term “relative,” or some other verbal indication that this is a within-child comparison, when describing differences from the child’s overall ability, rather than differences from the normal population (between-persons comparison). In the next sections, “drill down” from larger pools of data – index scores - to individual data points (individual items) to reveal patterns in the child’s performance. VCI and PRI are relatively “pure” measures of verbal and non-verbal reasoning, compared to the VIQ and PIQ found in the WAIS and previous editions of the WISC. Compare VCI and PRI as you would VIQ and PIQ. It is likely that most of the research on VIQ-PIQ differences applies fairly well to VCI-PRI differences, and that much of the research on the WISC-III and its predecessors applies to the WISC-IV, but be careful, and do not assume. In some ways, the WISC-IV is a very different animal from the WISC-III. Working down the hierarchy, each index score meaningfully assesses a unified construct or aspect of intellectual functioning only if the subtests that make up that measure “hang together” statistically. Discuss the meaning of the child's index scores individually, and their comparisons from the discrepancy analysis page of the WISC-IV record form using that hierarchy. Discuss both which scores are statistically high, low or average compared to the general population (nomothetic comparison), and which scores are strengths or weaknesses when compared to the child’s overall functioning (ipsitive comparison). Discuss whether the constructs assessed by each index area operate as unified wholes. That is, do the subtests that make up the index area co-vary, or are they discrepant? If discrepant, what accounts for that? Consider the sensory-motor stimulus-response demands of the task, whether the child displayed different levels of anxiety, whether scores fell as time went on (a fatigue effect), whether scores rose or fell depending on whether there were time limits, how the cognitive demands of stronger and weaker tests varied, and so on, in looking to understand differences in the child’s performance on different subtests within the same index. Address any other important patterns or discrepancies. For example, you might consider whether the child’s scores vary according to Bannatyne’s factors, according to the CHC theory of intelligence, according to whether the task requires more simultaneous or more sequential processing, and so on. At the bottom of the hierarchy, each subtest accurately assesses performance on its construct to the extent that intra-subtest scatter is minimal. Discuss any scatter. Look for patterns in “hits and misses.” E.g., does the child miss all geography questions on the Information subtest? All division problems on Arithmetic? Discuss the implications of any such patterns. Child Name 11 Verbal tasks on the WISC-IV are of two types: those measuring verbal comprehension and those measuring working memory. Verbal Comprehension tasks include defining words, answering questions requiring common sense or common knowledge, identifying similarities between two concepts or words, and using verbal clues to “construct” a concept. Verbal comprehension is strongly related to overall ability and academic performance. On these tasks, (Child) scored in the (name the range using Wechsler’s terminology) range, (higher/lower) than about NN% of children (his/her) age. In the paragraph on Verbal Comprehension, discuss how the child’s abilities or difficulties, as assessed by VCI alone, function in his/her life. Contextualize and individualize this description. Talk about the child, not the test. Point out any discrepancies between specific abilities the subtests identify and what the differences imply, by analyzing how the tasks in subtests with higher and lower scores differ in terms of needed skills, stimulus and response modalities, and theoretical constructs being measured. How do these relative strengths and weaknesses function in the child’s life? How do they relate to the referral question? Discuss any noteworthy response patterns or behaviors the child demonstrated when presented with these tasks. Speech patterns, response latencies, word-finding difficulties, Spartan or verbose responses, need for repetition or encouragement could all be discussed, especially if persistent. Idiosyncratic responses to items or idiosyncratic problem solving methods that may be relevant to diagnosis or referral question should be addressed. Emotional response, concentration, and so forth could be discussed here, if different from what was displayed on other tasks. The subtests that make up the construct Working Memory measure the ability to hold information active in mind while solving a problem with it, selectively attend to some information while ignoring other information, and perform mental tasks using a step-bystep logical approach. Child’s Working Memory score is (name the range), (higher/lower) than NN% of children (his/her) age. Working memory is engaged when, for example, Child (here include some examples of working memory as it might show up in the child’s life, such as using math knowledge to solve longer problems, adding long rows of numbers, keeping track of what he/she reads sufficient for comprehension, remembering complex or multi-step instructions, taking organized notes during a lecture, performing mental math, and so on. Use examples that fit the child’s context.) Discuss the implications of the score given the referral question. Discuss any significant differences between subtests. Both immediate auditory recall of meaningless information (Digit Span and Letter-Number Sequencing) and recall and processing of meaningful information (Arithmetic) are assessed in this area. Discuss the meaning of a difference between Digits Forward and Digits Backward, if significant or relevant. Address the assessment of incidental memory from Digit Symbol - and later relate this to the recall portion of Bender. Add observations as appropriate, as described in the section above. Compare and contrast the child’s abilities as assessed by VCI and WMI areas. Discuss the implications of any significant difference or lack thereof, in light of the referral question, the child’s history, the context to which you are predicting, and so forth. Discuss how the abilities assessed by VCI and WMI affect each other. Note, for example, whether retrieval difficulties or problems with incidental learning appeared to Child Name 12 impact Information, or whether language processing affected the Arithmetic subtest. Identify any relevant commonalities in the child’s approach to these tasks, in light of stimulus factors (auditory) and response factors (verbal), or other relevant patterns. Non-verbal problem solving tasks on the WISC-IV are of two types. The first of these, Perceptual Reasoning, required Child to construct visual models using a visual guide, perform hands-on problem solving, understand complex ideas presented visually, solve abstract visual problems, and identify important missing visual details. Child’s ability in this area is (name the range), higher than NN% of (children/adolescents his/her) age. Continue discussing as above. Discuss the implications of the child’s perceptual reasoning for academic functioning – given this specific child. For example, it might affect the child’s handwriting, discrimination between similar letters, ability to track across and down a page when reading, copy from the board, set up math problems in columns, read maps, understand graphs, make sense of geometry, follow demonstrations in science, read social cues, or find his/her way around the school. Since POI and VCI are the most “pure” measures of reasoning, subtracting out WMI and PSI, compare and contrast the child’s verbal and non-verbal reasoning abilities next. That is, compare and contrast their abilities as reflected in PRI and VCI. What are the implications? Talk about the child and their relative abilities, not the scores. Processing Speed tasks assessed the speed with which (Child) learns material presented visually, (his/her) visual alertness, and the speed with which (he/she) makes decisions, given visual information. (Child)’s abilities in this area were (name the range), (higher/lower) than NN% of children (his/her) age. Continue discussing as above. Differentiate poor performance on Coding due to motor vs. incidental learning problems, and relate this to the “recall” portion of the Bender, if you administered it, as well as any other incidental learning issues. Discuss the meaning of any difference between Cancellation Structured and Random. Comment on any problems with retrieval speed or response latencies observed on subtests other than those directly assessing processing speed. For example, did the child lose points on Block Design due to slow speed? Were his/her responses to verbal subtests delayed? Compare and contrast the child’s abilities as reflected in PRI and PSI. Overall, Child’s intelligence test results indicate that (he/she) thinks at a (name the range) level. Briefly reiterate areas of absolute and relative strength and weakness, and any critical patterns and observations. Continue your report by discussing the results of any other achievement or cognitive testing. I’ve provided one way to set up Woodcock Johnson test results at the end of this report, which is where I include them. I’ve given set-ups for both cognitive and achievement results, using all – or nearly all -subtests available for each. If you administer only the basic subtests, some of the general indices will not be computed, and you may need to alter the table. Child Name 13 If additional or other academic tests were administered, such as Key Math, the GORT, the WRAT-III, and so on, report results and what they mean about the child’s abilities here. Discuss the implications of such results. Compare with WISC-IV results, and discuss the implications of the differences. Learning disability assessment is shifting from solely an ability-achievement discrepancy to include an assessment of strengths and weaknesses in cognitive processes thought to underlie learning. Pay attention, therefore, to the underlying processes assessed in all instruments, as, for example, the index scores on the Wechsler. Is the child performing as would be expected from his/her intelligence test results? If not, what seems to be the problem? How does that explain actual academic performance in the classroom? Include relevant findings from the MSE, Bender, House-Tree-Person, and Sentence Completion, TAT, Rorschach, etc. (Koppitz’s and/or Lacks’ criteria, construction complexity on HTP and/or results of DAP scoring of person drawing; presence of cognitive, motor, or perceptual problems on the Bender, HTP; vocabulary usage, fluency of language, evidence of learning disabilities or higher intelligence in content, grammar, spelling, punctuation, on Sentence Completion; complexity, coherence, orderliness, and language skills evident in TAT, number and intactness of responses on the Rorschach, and so forth.) Resolve any discrepancies in the data by identifying the differences or similarities in the constructs being measured, setting or child characteristics, or task demands. For example, memory tested using sentences, numbers, words, mixed stimuli, or spatial location; visual vs. auditory stimuli; familiar/contextual vs. nonsense/out-of-context stimuli; and free versus cued recall may differ. What are the implications of these differences for the child’s ability to perform as expected in his/her context? Note the child’s behavioral responses to test stimuli, or to the testing situation itself, particularly unusual responses. Alternately, note normal responses when the unusual would be expected. For example, an allegedly hyperactive child attends, persists, concentrates, and so forth (might be effect of medication, misdiagnosis, or…) An adolescent claims not to be able to do a task on the test, yet performs a similar task during breaks without difficulty. Describe any information gained or performance differences observed from “testing the limits” (and describe the method of testing of the limits – which did not violate test security, did it?). Translate all of this into terms relevant to the child’s life. What do strengths and weaknesses in the above areas look like in this child’s everyday life and the contexts in which he or she lives? How are they connected to the presenting problem or other reason for referral? Sum up this section by discussing the implications of the results. What do they say about the child’s overall cognitive functioning and cognitive style? Social-Emotional Functioning Child Name 14 Consider a different heading than the above. For example, in reporting results for a child with ADHD, it might say, “Behavior” or “Behavioral Problems and Strengths”. For an anxious child, it might say, “John’s Ability to Cope with Anxiety” Caveat: I conceptualize clients from a multi-theoretical perspective, but my core approach is CBT. Alter all of the below to fit your theoretical orientation. But talk about the child, not their “mirroring transference”, “oral fixation”, “incongruence”, or whatever. Describe the child so that their grandmother and best friend would recognize them from your description. In describing children through college aged individuals, it is critical to take a developmental perspective. Personality is in the process of being created, not hard-set, in children, and is more plastic in young adulthood than in older years. Describe the child, adolescent, and young adult as in development, rather than set in stone. Talk about the social and self-skills they have or have not developed YET, about how far they have come and where they are going next. While this is important for all clients, it’s especially important when describing children, adolescents, and young adults. In addition, on the whole, children do not select their environments, and it is therefore much more critical to consider social environment effects on their performance and behavior (family, neighborhood, SES, global level of education in the neighborhood, this year’s teacher, the school as a whole, the unique combination of personalities in the child’s peer group, and so forth) than for adults. While staying true to the data that emerged from the assessment, carefully consider the reciprocal influence of child/adolescent and environment in describing the child/adolescent. Start by discussing the implications of the child's cognitive strengths, weaknesses, and style (as reported in the prior section) for daily functioning. Address the child's capacity for self-control. Address his/her ability to appreciate reality and control irrationality, his/her judgment and empathic ability, his/her ability to initiate and maintain friendships, and likely areas of difficulty in solving social-emotional problems based simply on cognitive strengths and weaknesses. Identify the child's primary psychological symptoms, if any. If you could identify a basic direction of movement (a developing personality style, if you will) or diagnostic characteristic, what would it be? If this is the core of the child, or the core of his or her problem, how do the rest of the characteristics or symptoms relate to, contribute to, maintain, or emanate from this core? What environmental factors might be contributing to, modifying, or maintaining the problem cognition, emotion, or behavior, or keeping the child stuck in development? Identify the child's predominant affect and mood. Discuss the child’s degree of responsiveness to affective stimuli, his/her range of affect, and its appropriateness to the situation. What is his/her capacity to delay gratification, to delay action, to cope with frustration? Again, contextualize this in terms of social learning theory and other environmental factors. Child Name 15 What is the nature of the child's anxiety? I.e., under what circumstances does the child manifest anxiety? How is the anxiety manifested? How does the child attempt to cope with anxiety, stress, and the current situation? How effective are these methods for him/her? Discuss the child's capacity for appropriate (not too lax, not too harsh) impulse control. Identify the cognitive, social-emotional, situational (and biological, if applicable) factors that underlie the presenting problem, if any, or that relate to the referral question. Relate the above to the child's presenting problems, and social, academic/occupational, peer-group, and family functioning. Identify the child's emerging view of self, world, others, future – and describing these as in the process of development, rather than fixed. Relate these to the life tasks of work, love, community/friendship, self and spirituality. What are the emerging core beliefs that are affecting the child’s functioning, especially those relevant to the referral question? Identify the areas in which the child demonstrates psychological strength and positive qualities. How does the child use these strengths in his/her life? How do they mitigate the presenting problem or add to an understanding of the referral question? How might the child’s strengths be used in therapy or in the situation to which you are “predicting” to improve the child’s functioning? How will those strengths continue to affect the child’s development. Summary: Briefly summarize the report as a whole. Some audiences (judges, busy psychiatrists) read only the summary, so you must be succinct, clear, and direct. What was the referral question? What is the child’s general level of intelligence, and any noteworthy strengths, weaknesses, or stylistic patterns observed. Then summarize overall social/emotional assessment results, highlighting the more central and salient aspects of the child’s developing self, and his/her current functioning. Clearly and simply relate the results to the referral question, and ANSWER THE QUESTION/S in as straightforward and clear a manner as possible. Make sure your answer is clearly supported by the test data. Give MUCH more weight to the data and to actuarial interpretation of results than to your “clinical judgments,” as research says the former is likely to be more accurate. Where there is conflict between clinical impression and data, say so, identify which is which, describe your conclusions and rationale for them, and help the reader know how to handle the discrepancies. NOTE: Information and hypotheses listed in the summary should reflect PREVIOUSLY DISCUSSED information and hypotheses. No new information or hypotheses should be presented here. Check to make sure you have CLEARLY ANSWERED the referral question. Child Name 16 Diagnosis: Note that for some referral questions, diagnosis is not the issue, and no diagnosis should be given. For example, pre-employment screening does not require a diagnosis. For doctoral students in assessment courses and preparing competency examinations, full 5-axis diagnoses must be given. Axis I: XXX.XX (Write out diagnosis and modifiers for Axes I and II Axis II: XXX.XX in addition to their codes. If there is no diagnosis on either of these axes, the code is “V71.09 No Diagnosis”. Axis III: (Medical conditions that impact on the referral question, if any. Note the source of the information, such as medical file, patient report, or pediatrician, or “per DSM-IV criteria”. Failure to cite the source can leave you open to charges of practicing medicine without a license, because you are not qualified to make medical diagnoses. ) Axis IV: (Psychosocial stressors: list category of stressors and the specific stressors, and identify them as mild, moderate, severe or extreme. Note that the rating is by objective criteria. Adjusting to a new school is usually a mild stressor, but may become moderate is preceded by a move at a vulnerable age or by a complication such as coping with peer reaction to a physical disability, or may be more severe if it comes as a result of some trauma.) Axis V: GAF Current: __ GAF Highest in past year: __ (Note that a child’s current level of adaptive functioning cannot exceed his/her highest level of functioning in the past year, since the day you assessed him/her is a part of the past year!) Recommendations: Use whichever apply of those below, and/or additional or alternative ones pertinent to the referral questions. Group recommendations according to the major findings of the report. Place major recommendations first, and less critical recommendations later in each numbered point. Present recommendations in numbered outline format, for easy digestion and referral. 1. Your first point, when needed, should be anything urgent or emergent: the need to hospitalize, to take action to protect the child or others from the child’s dangerousness, to protect the child due to extremely poor reality testing, to urgently have the child assessed for medical or neurological problems. If it’s serious, say so clearly. Further, if something needs to be done emergently, don’t wait for the report to be written to get in touch with the child, their family, the referrer, etc., so that emergency needs can be met immediately. 2. Identify any educational interventions needed, arranging them by problem area. Consider interventions that need to be done at school, that can be implemented at home, that a therapist should help with, or that the child/adolescent can work on themselves, with support. My recommendations start with a numbered statement of the problem (E.g., 2. John does indeed have a reading disability, characterized primarily by problems in comprehension due to severe difficulties with working Child Name 17 memory. Suggestions to improve, his comprehension are:) and then several ways to help improve or accommodate the difficulty. 3. Identify whether psychological treatment is warranted. If so, related to what specific issues? What mode? What kind? What frequency, intensity, setting, and urgency? To achieve what goals? Of what expected duration? If this is an inpatient assessment, is continued hospitalization warranted? Based on what? Example: “Continued inpatient hospitalization is warranted due to John’s suicidal ideation and plan, concurrent severe anxiety, lack of social support, and refusal to participate in outpatient therapy.” “John’s therapist should help him cope with the learned and habitual behavior patterns that accompany his ADHD, and specifically should focus on helping him develop impulse control, the capacity to delay gratification, and frustration tolerance.” “Individual, outpatient, cognitive-behavioral therapy, once weekly, to address Mary’s adjustment to high school and separation anxiety is recommended. Mary should begin working with the high school counselor this week if possible, as she is considering dropping out of school.” “Mary should be referred to Kinheart for participation in “coming out” groups to help her identify and cope with the issues related to her decision to reveal her sexual orientation to her family, and to receive support from others after having been “outed” at school.” (If making a specific referral, give contact information.) 3. Consider medical evaluation? To alleviate what symptoms? Example: “If Mary’s anxiety does not abate within two weeks of starting treatment, her parents should consult with her pediatrician or an adolescent psychiatrist to determine whether anti-anxiety mediation would help her calm down enough to attend classes while she is beginning therapy. Specific attention should be paid to evaluating her sleep pattern, since she reports she stays up “all night” worrying.” 4. Non-psychological, non-psychiatric interventions needed? What kind? By whom? Other agencies need to be involved? Example: “Given the nature of Mary’s cultural and religious beliefs and their impact on her parents’ willingness to seek therapy, consultation with their rabbi is recommended. This consultation should identify whether the rabbi is capable of helping Mary with her Child Name 18 depression, or whether the rabbi can assist her and her parents in accepting the professional help she clearly needs.” 6. Environmental interventions (e.g., stimulus control) needed? Example: “Johnny needs to be seated at the front of each classroom, so that he is able to see the board.” “At work, Johnny should be switched to a position that minimizes interaction with customers. He should have the opportunity to socialize with a small group of fellow workers, to reduce his anxiety and provide him with opportunities to check out his interpretation of his experiences.” 7. Issues that might interfere with treatment and how to address them? Example: “Mary’s parents see her as a victim of “the high school’s impersonal, uncaring environment.” They repeatedly sympathize with and encourage her distress. Unless her parents can be helped to adopt a supportive yet adaptive approach, this otherwise capable student may continue to struggle with the transition to high school. It is recommended that her counselor arrange to meet with her parents and that they be encouraged to participate in the Parents-in-Transition outreach program.” 8. Further assessment? What kind? By whom (what specialty)? To resolve what questions? Example: “Neuropsychological assessment is recommended to assess the extent and nature of brain damage John has suffered as a result of his substance abuse. Rehabilitation evaluation is recommended to identify interventions that may help him cope with his impairments.” “Given the nature of John’s learning disability and his slow progress despite the special education services he is receiving, reassessment is recommended in one year to assess the efficacy of the new Individual Education Plan and to determine whether an alternative educational placement should be considered.” Finally, include a formal signature block, which looks like this: Child Name 19 Respectfully submitted, ________________________________ Your name, highest EARNED and RELEVANT degree Examiner (or Psychology Intern, if you are one) ________________________ First Last, Degree Supervisor Ethical guidelines specify that you should list only your highest, relevant degree (or two if both are relevant, such as J.D., Psy.D. if you practice mental health law). That is, you cannot load your signature to make your credentials look more impressive. Do not list your Ph.D. in economics, English, or even education (unless it’s school psychology). Your M.D. or R.N. are irrelevant and not to be listed, because that education did not train you to perform psychological testing/assessment. Do not list a bachelor’s degree. You can list masters’ level training in a related mental health field if you have not completed your doctorate in psychology. If you are a diplomat (i.e., have passed advanced competency board exams), you may add these initials to your degree initials, e.g., “John Smith, Psy.D., ABPP”. In addition, if you are a doctoral student in a program where I teach, it is expressly prohibited to list yourself as “Psy.D. Candidate”. Psy.D. programs generally do not recognize or use the term. Traditionally, the term is reserved for persons who have completed everything for the doctoral degree except for the dissertation, and whose dissertation proposals have been accepted. Because the path to the Psy.D. varies from the path to the Ph.D., most programs do not use or endorse the term. Do not use it! Similarly, do not list A.B.D.. The public thinks this is a credential. It is not. It is the absence of a credential. See the next pages for WJ-III results tables I use in my reports. Child Name 20 Woodcock Johnson – III Cognitive Test Results Cluster/Test Thinking Ability Verbal Ability Comprehension-Knowledge General Information Verbal Comprehension Cognitive Efficiency Processing Speed Visual Matching Decision Speed Pair Cancellation Retrieval Fluency Working Memory Numbers Reversed Memory for Words Auditory Working Memory Long-Term Retrieval Visual-Auditory Learning Visual-Auditory Learning Delayed Retrieval Fluency Rapid Picture Naming Fluid Reasoning Concept Formation Analysis-Synthesis Cognitive Fluency Broad Attention Numbers Reversed Auditory Working Memory Pair Cancellation Executive Processes Concept Formation Pair Cancellation Visual-Spatial Processing Spatial Relations Picture Recognition Phonemic Awareness Sound Blending Incomplete Words %ile Standard Score Functioning Level Name the range Z = .nn Child Name 21 Woodcock-Johnson III Achievement Test Results Cluster/Test A. Broad Reading 1. Basic Reading Skills a. Letter/Word Identification b. Word Attack 2. Reading Fluency 3. Reading Comprehension a. Passage Comprehension b. Reading Vocabulary B. Oral Language 4. Oral Expression a. Story Recall b. Story Recall – delayed c. Picture Vocabulary 5. Listening Comprehension a. Understanding Directions b. Oral Comprehension C. Broad Written Language 6. Basic Writing Skills a. Spelling b. Spelling of Sounds c. Editing d. Punctuation & Capitals 7. Written Expression a. Writing Fluency b. Writing Samples D. Broad Math 8. Calculation 9. Math Fluency 10. Math Reasoning a. Applied Problems b. Quantitative Concepts Academic Skills (A1a, C6a, D8) Academic Fluency (A2, C7a, D9) Academic Applications (A3a,C7b, D9) Academic Knowledge Phonemic/Graphemic Knowledge Total Achievement %ile Standard Score Functioning Level Name the range Z = .nn