HIP Item 4 Obesity Paper 16 Dec 2013
advertisement

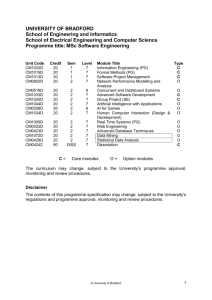
Health Improvement Partnership Title of Paper Healthy Weight Strategic Lead Julia Burrows Report Contact Alison Moore Action Required by the Partnership 1.0 Purpose of the Report To increase levels of knowledge and awareness of current healthy weight agenda, identify gaps and areas for action. 2.0 Background / Context The number of obese people in England has been rising sharply for the best part of 20 years. Today one in four adults are obese, according to the Health Survey for England, compared to less than 15 per cent in 1993. By 2050 these figures are predicted to have more than doubled (LGA 2012). The 2011/12 NCMP prevalence figures show the substantial changes that have occurred in children’s BMI over the past two decades – with the proportion of children classified as obese nearly doubling for children in Reception and increasing more than threefold for Year 6 since baseline in 1990 (NHS Information Centre 2011). 2.1 Causes: Unhealthy diets and low levels of physical activity, as well as more subtle causes, including societal influences, individual psychology and the environment around us, which could often make it hard to make healthy choices (Foresight 2007). Studies have shown that obesity reduces life expectancy by an average of three years, while morbid obesity reduces it by eight years – the same effect as a lifetime of smoking. This is because being obese can increase the risk of developing a range of diseases and health problems; cancer, heart disease, stroke, type 2 diabetes, and musculoskeletal problems. The resulting NHS costs attributable to overweight and obesity are projected to reach £9.7 billion by 2050, with wider costs to society estimated to reach £49.9 billion per year (Foresight 2007). On 1st April 2013 public health became the responsibility of local government creating opportunities to tackle the wider determinants of obesity and reduce health inequalities in local communities, especially the poorest. The public health outcomes framework identifies two specific indicators in relation to healthy weight; excess weight in adults and excess weight in 4-5 and 10-11 year olds. Plus a number of key contributable indicators; proportion of inactive adults, diet, breastfeeding, take up of NHS Health Check, falls in over 65’s, utilisation of green space for exercise. The work of the healthy weight team will also contribute to the over arching objective of reducing the numbers of people living with preventable ill health and dying prematurely, while reducing the gap between communities, namely mortality from cardiovascular disease and cancer. 2.2 Prevalence: Adult obesity in Bradford is currently 25.6% (Health Survey for England, 2008), which is significantly higher than the National Average of 24.2%. Childhood obesity is 10.4% in Reception and 21.7% in Year 6 (NHS IC 2012), both above the national average. Plus it must be pointed out that the national average is extremely high, this means almost a third of 10-11 year olds and over a fifth of 4-5 year olds were overweight or obese. 2.3 Addressing overweight and obesity in the population: To achieve a reduction in obesity and overweight in Bradford’s population the work needs to be done at a number of different levels; environment, organisational, and influencing personal choice. The Local Authority commissions and delivers prevention initiatives and commissions and provides community lifestyle weight management programmes and an exercise referral scheme thought its public health function. These programmes are generally defined as Tier 1 and Tier 2. Specialist, multidisciplinary obesity services are generally defined as Tier 3 services, and we do not have these currently in Bradford. Bariatric surgery is a Tier 4 service that is commissioned by NHS England. The diagram below sets out proposed definitions of these tiers: CLINICAL CARE COMPONENTS COMMISSIONED SERVICES 2.4 Current work programme: Responsible for delivering the National Child Measurement Programme (NCMP) locally. Measuring the height and weight of children in Reception and Year 6 and the central return of that data is mandatory. Currently commission the School Nursing Service to deliver the NCMP and followup families Develop a locally tailored strategy for healthy weight – ensuring it is a priority at strategic and delivery levels and external partners such as local employers, schools, VCS organisations and the NHS are working together to integrate support and provide preventative services. Access to support by developing pathways from primary care to secondary care and into sustainable community support Currently have a partnership agreement for the delivery of adult healthy weight courses that run in the community, provide training, resources and support. Commission a voucher scheme for primary care for Weight Watchers Making Every Contact Count – deliver a two-hour briefing session to groups of front-line staff enabling them to raise lifestyle issues, assess readiness to change and signpost to local lifestyle support services Children’s Healthy Weight courses (2-4, 5-11 and 12+) are in development and being piloted. Every Baby Matters Strategy – actions around breastfeeding and child food poverty Commission an Infant Feeding Co-ordinator School Nursing Service commissioned the Healthy Child Programme Commission evidence based Food Dudes Programme in Special schools Partnership agreement for the delivery of Walkshire – school based walking programme The Exercise Referral Scheme for Bradford – Bradford Encouraging Exercise Programme (BEEP) increases access to specialist physical activity advice and signposting to appropriate opportunities across the district. Responsible for delivering the NHS Health Check locally. A cardiovascular screening programme for 40-74 years measuring height, weight, blood pressure, cholesterol, risk factor questions and blood glucose (if necessary) and the central return of that data is mandatory. The national model indicates referral and signposting to stop smoking services, exercise referral and community weight management. Good Food Bradford – Food Strategy and Food Network, Good Food Award, Ministry of Food work Highway to Health/Tour de France Cross department working (eg environmental health, transport and planning) both within the council and across West Yorkshire to assess health impacts of their policies and strategies and to use opportunities to shape them to promote physical activity and healthier lifestyles 3.0 Report Issues Public Health currently commissions VCS organisations to deliver a range of health improvement activities – a review of this work is currently underway The lack of a specialist obesity service (tier 3) in Bradford. NHS England (the commissioner of bariatric surgery) has specified that patients need to have been through a Tier 3 service in order to be eligible for surgery. This means that unless they have a very high Body Mass Index (>50kg/m2), patients in Bradford can not currently access bariatric surgery. Work is ongoing between Public Health, the Clinical Commissioning Groups and NHS England to address this problem, which is an issues at local and national level. 4.0 Proposed Outcome / impact measurement Establish effective partnership working to maximise impact and ensure a co-ordinated approach. Commission for health outcomes by developing meaningful performance measures for providers and appropriate reporting mechanisms. 5.0 Contribution of Health Improvement Partnership Public Health Healthy Weight supports and contributes to addressing a number of health inequalities and co-ordinates effort towards tackling the issue of obesity 6.0 Recommendations Address gaps in services: Healthy Weight Pathway for adults and children, including addressing the issues regarding a lack of Tier 3 service and access to bariatric surgery by all commissioning organisations Work with partners Physical Activity opportunities with appropriate support for pregnant women Comprehensive delivery of a children’s lifestyle weight management service Physical activity pathways for secondary care Workplace health improvement initiatives Stronger links needed with Adult Services For more information please contact Alison Moore Senior Public Health Manager Bradford MDC alison.moore@bradford.gov.uk