Physical Environment Health Services
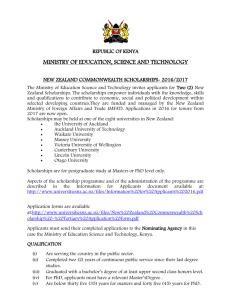
advertisement

on behalf of all DHBs PUBLIC HEALTH SERVICES REGULATORY SERVICES AND REPORTING – PHYSICAL ENVIRONMENTAL HEALTH SERVICES TIER LEVEL TWO SERVICE SPECIFICATION Status: Approved for recommended nationwide use for the non-mandatory description of services funded by DHBs. RECOMMENDED Status: MANDATORY Approved for mandatory nationwide use for the description of services to be funded by the Ministry of Health. Review History Date Endorsed by Nationwide Service Framework Coordinating Group (NCG) Published on NSFL Review: of Public Health Handbook (2003): Amendments: inserted into service specification format, added support services ,service linkages table, quality requirements, Purchase Unit Code table, reporting requirements, links to Public Health Services tier one service specification . Consideration for next Service Specification Review April 2010 Within three years Note: Contact the Service Specification Programme Manager, National Health Board Business Unit, Ministry of Health to discuss the process and guidance available in developing new or updating and revising existing service specifications. Web site address of the Nationwide Service Framework Library: http://www.nsfl.health.govt.nz/. PUBLIC HEALTH SERVICES -REGULATORY SERVICES AND REPORTING – PHYSICAL ENVIRONMENTAL HEALTH SERVICES TIER LEVEL TWO SERVICE SPECIFICATION This tier two service specification for Public Health Services Regulatory Services and Reporting – Physical Environmental Health Services (the Service) must be used in conjunction with the overarching tier one Public Health Specification and is linked to the tier two Social Environments and Health Promoting Schools service specification. Refer to the Public Health tier one service specification under the following headings for generic details on: Service Objectives Service Users Access Service Components Service Linkages Exclusions Quality Requirements The above heading sections are applicable to all the Service delivery. Background When considering the role of the physical and social environments on the health of populations, the concepts of sustainable development and supportive environments must be included. Ecological public health involves creating physical and social environments conducive to health, to make healthy choices easier choices. It requires a comprehensive approach to public health including developing linkages between existing areas of public health activity. Creating sustainable healthy environments contributes to key public health outcomes such as healthy eating healthy action, for example through urban design contributing to healthy action or health promoting schools providing a vehicle for nutrition policies in the education sector. 1. Service Definition Enforcement is the investigation and action in response to alleged non-compliance, and requires specialist experience and skilled practitioners. While there is a distinction between compliance and enforcement, it is not always easy to practicably separate the two. The enforcement of public health legislation is undertaken by District Health Board (DHBs) Public Health Units, which are responsible for planning and delivering compliance and enforcement functions as part of comprehensive public health programmes. In addition, the Director-General of Health directly employs or contracts enforcement officers to undertake the enforcement of more complex, or precedent setting, or specialised legislation. The Services must provided in accordance with the tier one Public Health Services service specification Appendix One Regulatory Services and Reporting Requirements and the Ministry of Health Environmental Health Protection Manual. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 2 The following legislation is required to be enforced by DHB’s Public Health Units under this service specification: Biosecurity Act 1993 Burial and Cremation Act 1964 Civil Defence and Emergency Management Act 2002 Epidemic Preparedness Act 2006 Hazardous Substances and New Organisms Act 1996 Health Act 1956 Misuse of Drugs Act 1975 New Zealand Public Health and Disability Act 2000 Prostitution Reform Act 2003 Radiation Protection Act 1965 Sale of Liquor Act 1989 Smoke-Free Environments Act 1990. Officers within Public Health Units are designated (or appointed) under the Health Act 1956, Smoke-free Environments Act 1990, Hazardous Substances Act 1996, and the Biosecurity Act 1993. Public health managers may also use the Ministry of Health’s (the Ministry’s) specialised enforcement officers for compliance and enforcement activities to support and enhance the public health unit’s staff. The Director of Public Health, and other appropriately experienced public health medicine specialists within the Ministry, have been appointed as national medical officers of health, although these national medical officers of health would largely exercise their powers during public health emergencies, rather than for more routine compliance and enforcement functions. 2. Service Objectives 2.1 General The overarching health goal is that public health and whanau health are improved through the protection and promotion of healthy communities and healthy environments including the global environment. The key outcomes, to be achieved in 10 to 20 years, are the reduction in the incidence and impact of: environmental hazards environmental inequalities across sectors settings-based environmental health issues See Appendix One Figure 1 for Outcomes Focused Framework for Environmental Health and Social Environments. Individual contract service specifications each have a goal, which is focused on that particular aspect of the environment. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 3 2.2 Māori Health Refer to the tier one Public Health service specification. 3. Service Users The New Zealand general public. 4. Access The services under this service specification are accessed though the DHB’s Public Health Units. 5. Service Components and Linkages 5.1 General Service Categories Environmental Health Subcategories Included Air quality (indoor and outdoor) Border health protection Burial and cremation Contaminated land Drinking water quality Environmental noise management Hazardous substances Ionising/non-ionising radiation Public Health emergency planning and response Recreational water Resource management Sewage treatment and disposal Waste management (liquid and solid waste) 5.2 Other regulatory activities. Environmental Health 5.2.1 Air Quality (Indoor and Outdoor) Health Goal Rationale and Key Issues To reduce the incidence and impact of environmental hazards by developing strategies to prevent or control the adverse impacts of air quality (indoor and outdoor) on public health. Air pollution from industrial, domestic and mobile sources can give rise to serious health problems, particularly in urban areas where the majority of the New Zealand population (over 80%) reside and work. Air pollution can also occur from natural sources, such as geothermal areas. Risks to public health exist both outdoors and indoors (including nonoccupational environments) where exposure to short-term high, or long-term low, concentrations of air pollutants can give rise to acute and chronic conditions and, in extreme cases, death. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 4 Objectives Key Linkages To have strategies to prevent or minimise the health risks and diseases associated with air pollution. To promote a physical environment both outdoors and indoors, which has clean air. Department of Building and Housing Emergency Services Ministry for the Environment Department of Labour Relevant Legislation Regional Councils and territorial authorities Agricultural Compounds and Veterinary Medicines Act 1997 Building Act 2004 Building Regulations 1992 (under review) Hazardous Substances and New Organisms Act 1996 Health Act 1956 Housing Improvement Regulations 1947 Health and Safety in Employment Act 1992 Land Transport Management Amendment Act 2008 Land Transport Act 1998 Land Transport Rules (a form of delegated legislation similar to regulations made under the Land Transport Act 1998) Local Government Act 2002 New Zealand Public Health and Disability Act 2000 Resource Management Act 1991 Resource Management (National Environmental Standards Relating to Certain Air Pollutants, Dioxins and Other Toxics) Regulations 2004 Traffic Regulations 1976 (only requirements relating to vehicle noise, brakes, steering and couplings remain in these regulations) Components of Service Service Descriptions/Activities Promote public health knowledge Provide information and advice to other agencies and the public on adverse effects of adverse air quality. Provide advice and input into the activities of linkage agencies Make timely and professional submissions on national (including national policy statements, national environmental standards and or guidelines) and regional plans and policy statements, district plans, and where appropriate, resource consent applications to ensure that the public health effects of adverse air quality are considered and managed. Seek to develop a Memorandum of Understanding (or equivalent) with regional councils that describe roles and responsibilities in this area. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 5 5.2.2 Border Health Protection Health Goal To reduce the incidence and impact of settings-based environmental health issues through the management of public health risks entering or leaving New Zealand and through the surveillance, exclusion, eradication, and effective management of pests of public health significance from the environment. Rationale and Key Issues New Zealand has remained free from many imported human, animal and plant diseases and their vectors. Effective border health protection procedures are needed to prevent the entry and establishment of new diseases or disease vectors, and other public health risks. Objectives To prevent potential health risks caused by the arrival of travellers, goods, aircraft and vessels from overseas, and the introduction of pests and unwanted diseases. To prevent the international spread of disease and other public health risks by facilitating New Zealand’s international reporting obligations and compliance with international obligations. Key Linkages Department of Labour Department of Conservation Ministry for the Environment Ministry of Agriculture and Forestry Ministry of Fisheries NZ Customs Service Port and airport companies Territorial authorities and regional Councils Travel industry Relevant Legislation Biosecurity Act 1993 Health Act 1956 Anthrax Prevention Regulations 1987 Health (Quarantine Regulations) 1983 New Zealand Public Health and Disability Act 2000 International Health Regulations 2005 Components of Service Service Descriptions/Activities Public health regulatory services All border health protection programmes will be carried out in collaboration with other relevant agencies. Border health protection services Border health protection programmes should: ensure adequate capacity to carry out services and respond to incident and emergent issues undertake surveillance of container-breeding mosquitoes at international sea and airports Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 6 Information and Reporting Requirements identify and monitor border health protection risks (including surveillance) and develop/maintain contingency plans to deal with them respond promptly to interceptions of pests, and cases of imported disease respond promptly to requests for pratique, inspections and certification (eg ship sanitation, fumigation, anthrax control). assess the effectiveness of implementation of public health aspects of border health protection, in conjunction with other agencies (eg, quarantine facilities and practices, vector surveillance and control, radio pratique, potable water, waste disposal) provide sound technical and professional advice on public health issues that are related to border health protection objectives in relation to imported risk goods, disease vector surveillance and control, preparation of contingency plans for emergency response, preparation of submissions as appropriate on proposed pest management strategies contribute (when required) to the preparation of health impact assessments in relation to border health protection threats and eradication and control activities; participate in national, regional and local research survey or response programmes as appropriate; participate in national, regional or local emergency responses as required. All dates apply annually. In February each year, provide the Ministry of Health with: a summary for the previous calendar year of activities undertaken including issuing pratique, undertaking sanitation inspections, ensuring points of entry are maintained in a sanitary condition and free from sources of infection and contamination including vectors and reservoirs; supervision of any deratting, disinfection, disinsection, or decontamination as appropriate; application of control measures to any conveyance; interception responses; and maintenance of effective contingency arrangements; a report on designated airports’ and ports’ ability to meet core capacities as outlined in Annex 1B of the International Health Regulations 2005; forecast of your border health protection surveillance programme for the forthcoming financial year. provide situation reports on activities undertaken during interception responses as required by the Senior Advisor (Border Health Protection), using the format in the biosecurity section of the Environmental Health Protection Manual. Providers are required to advice the Senior Advisor (Border Health Protection) within two hours of the identification and location of an exotic mosquito or mosquitoes of public health significance. Immediately notify the Senior Advisor (Border Health Protection) of any control measures applied to any conveyance that are other than routine, and copy the Office of the Director of Public Health. Immediately, or within 24 hours of occurrence of a public health event or emergency with inter-district, national or potentially international implications, submit a report to the Environmental & Border Health Protection Team and a copy to your Public Health Group, Portfolio Manager, Health and Disability National Service Directorate, Ministry of Health. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 7 5.2.3 Burial and Cremation Health Goal To reduce the incidence and impact of environmental hazards by ensuring the lawful, hygienic and dignified disposal of the dead. Rationale and Key Issues The sanitary disposal of the dead is essential to protect the public health. Objectives To ensure the correct procedures are used for disposal of the dead and any subsequent movement of remains. Key Linkages Funeral directors The public expect burial and cremation activities to be conducted with dignity, sensitivity and with respect for the deceased and their families. Territorial authorities and regional councils Burial Ground/Crematorium Management Trustees. Relevant Legislation Burial and Cremation Act 1964 Cremation Regulations 1973 Burial and Cremation (Removal of Monuments and Tablets) Regulations 1967 Local and Private Acts of Parliament Health Act 1956 Health (Burial) Regulations 1946 New Zealand Public Health and Disability Act 2000 Resource Management Act 1991 Components of Service Service Descriptions/Activities Ensure compliance with Burial and Cremation Act 1964 and regulations Supervise disinterments. Information and Reporting Requirements All dates apply annually. Investigate and follow up incidents and complaints. Advice and assist applicants to export cadavers to ensure public health concerns are addressed. Provide reports to the Ministry of Health as required for: disinterment licence applications burials in special places medical referee nominations other burial and cremation issues. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 8 5.2.4 Contaminated Land Health Goal To reduce the incidence and impact of environmental hazards by preventing or controlling the adverse impacts of corrosive, explosive, flammable, oxidising and toxic hazardous substances. Rationale and Key Issues Human activities in parts of New Zealand have resulted in the contamination of land with substances hazardous to human health. Human exposure may occur through contact with contaminated soil, dust, food and water. This exposure may be hazardous to health and, therefore, needs to be quantified and minimised. Objectives To minimise the impact of contaminated land sites on human health using a risk management and health impact assessment approach. To work with regional councils and territorial authorities in the assessment and management of contaminated land sites in order to minimise any potential or actual effects on human health. Key Linkages Ministry for the Environment (The Ministry has developed a series of 5 guidelines cover the following areas: reporting, application of environmental guideline values, risk screening, classification and information management and investigation and analysis. Their main purpose is to introduce consistency in contaminated land assessment and management throughout the country.) Department of Labour Regional Councils Territorial authorities Relevant Legislation Components of Service Public health regulatory services Work with territorial authorities Hazardous Substances and New Organisms Act 1996 Health Act 1956 Health and Safety in Employment Act 1992 Local Government Act 2002 New Zealand Public Health and Disability Act 2000 Resource Management Act 1991 Service Descriptions/Activities All contaminated land programmes will be carried out in collaboration with other relevant agencies. 1. 2. Information and Reporting Advise, encourage and/or assist territorial authorities and Regional Councils to: locate contaminated land sites and identify contaminants implement health impact assessment systems to ensure contaminated land is remedied, where appropriate, and to minimise adverse effects on human health determine appropriate land use controls for contaminated sites to minimise the risk to the public health. Seek to develop a Memorandum of Understanding (or equivalent) with Regional Councils that describes roles and responsibilities in this area. All reporting dates apply annually. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 9 Requirements 5.2.5 Drinking Water Health Goal To reduce the incidence and impact of environmental hazards by promoting the availability of adequate supplies of safe drinking water to all communities. Rationale and Key Issues Safe drinking water is essential to protect the public health from diseases or harmful contaminants in New Zealand. Water intended for human consumption or for activities such as food preparation should be of such quality that good health is not compromised or threatened. In 2007, the Health Act 1956 was amended to include a regulatory framework to promote safe drinking water supplies. The amended Act defines the competencies, functions and powers of drinking-water assessors and designated officers. The Act also specifies the regulatory duties applying to drinking-water suppliers including the requirement for water suppliers to: be on the Register of Community Drinking Water Supplies in New Zealand; and take all practicable steps to comply with the Drinking Water Standards for New Zealand and, if they are larger than a neighbourhood supply, to provide an adequate supply of safe drinking-water and to prepare and implement a public health risk management plan for their supply. The Resource Management (National Environmental Standards for Sources of Human Drinking Water) Regulations 2007 administered by the Ministry for the Environment came into effect on 20 June 2008. The regulations aim to reduce risks to the quality of water bodies from which the source water for drinking-water supplies is taken. It will do this by preventing discharge and water permits being granted, and preventing the inclusion of permitted activity rules in regional plans, if they will cause drinking water to become unsafe to drink after the existing treatment processes. To implement the national environmental standard, regional councils and consent applicants will need to understand the: likely contaminants that might be associated with a particular activity ability of the various treatment processes used in New Zealand to remove contaminants from the water. The Drinking Water Standards for New Zealand 2005 sets out the quality of water that water suppliers are expected to deliver for public consumption. The publication of the Register of Community Drinking Water Supplies in New Zealand identifies from where communities receive their water, the Priority 2 determinants present, and the public health grading of the supply. The publication of an annual report on the chemical and microbiological quality of drinking water supplies in New Zealand means that the public is made aware of the quality of their water. There are a large number of small community drinking water supplies that do not reach the required standards. This can be due to the poor quality of the water or because they are not monitored and so do no demonstrate whether or not they meet the desirable standard. Suppliers should b encouraged to register their supplies and demonstrate compliance with the desired standards. The drinking water assistance programme (DWAP) has two parts, a Technical Assistance Programme (TAP) and the Capital Assistance Programme (CAP). The TAP provides technical assistance to small water supplies serving less than 5000 people. The TAP assist with preparation of Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 10 specification November 2009 Nationwide Service Framework public health risk management plans, optimisation of small water supplies, options for upgrading or improving supplies and preparation of capital assistance programme applications. The capital assistance programme provides funding to upgrade small water supplies. Objectives To optimise the safety and quality of all drinking water available for public consumption in New Zealand. To prevent the spread of disease to the public through the public water supply. Key Linkages Department of Building and Housing Department of Internal Affairs Drinking Water Suppliers Local Government New Zealand Ministry for the Environment New Zealand Food Safety Authority Territorial authorities and regional councils Relevant Legislation Building Act 2004 Food Act 1981 Health Act 1956 Local Government Act 2002 New Zealand Public Health and Disability Act 2000 Resource Management Act 1991 Components of Service Service Descriptions/Activities Public health regulatory services 1. Drinking water assessor units are to have access to the services of a sufficient number of appointed Drinking Water Assessors to carry out the programme within the public health unit’s region. (P1) NB priorities for action are shown in bold type e.g. (P1) is priority 1. 2. Items (except (a)) are to be performed by, or certified by, a drinkingwater assessor. (see individual priority ranking) 3. Undertake such duties as are required by the Health Act 1956, as amended by the Health (Drinking Water) Amendment Act 2007: Identify all drinking-water suppliers in the Health District, including specified drinking-water suppliers and specified self-suppliers and enter them on the Register [section 69B, 69J, 69K,L,M,N] (P1); All applications for the registration and de-registration of water suppliers and registration, renewal of registration and de-registration of water carriers to be processed within 20 working days [DWA Tech Manual] (P1); Assess water supplier (including water carrier) compliance with the Drinking Water Standards for New Zealand 2005. Report on compliance / non-compliance with duties under the Act to the water supplier within 20 working days [section 69V]. (P1); Provide reports to the Ministry of Health on water suppliers’ compliance with the Health (Act 1956, compliance with Drinking Water Standards for New Zealand 2005 and implementation of their public health risk management Plan (P1); Verify adequacy of water suppliers’ public health risk management plans and provide report to the water supplier within 20 working days [section 69Z] (P1); Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 11 specification November 2009 Nationwide Service Framework Certify implementation of a water supplier’s public health risk management plan at no greater than a three yearly interval and report to the water supplier within 20 working days [section 69Z] (P1); Assess the competence of and, where appropriate, authorise persons to perform drinking water analyses and calibration of water treatment and testing equipment, report to the water supplier within 20 working days [section 69ZL(1) (e)&(f)] (P2); Assess water suppliers’ complaint management procedures and report to the water supplier within 20 working days detailing whether legislative requirements are met [69ZE]. (P2); Assess and process applications for the use of temporary drinking water supplies (P1). 4. Undertake enforcement activities, where appropriate using powers under the Health (Drinking Water) Amendment Act 2007. (P1). Participation in grading of water supplies 1. Carry out public health grading of community drinking water supplies in accordance with the national programme and synchronised with the phasing in of the Drinking Water legislation. 2. Grading of all drinking water supplies with population >500 to be completed by 30 April 2009 and thereafter every two years. Grading reports to be sent to the water supplier within 20 working days of assessment. (P1) Maintain monitoring and surveillance systems 1. Carry out the surveillance of drinking water monitoring by suppliers and maintain the Water Information New Zealand (WINZ) database entries for all community drinking water supplies (P2). 2. Collate microbiological and chemical drinking water quality data and information on public health risk management from all drinking water suppliers listed in the current edition of the Register and transmit the data for the previous calendar year to the Ministry of Health’s science provider before 31 August (P1). 3. Collect and supply water samples and water source data for the Priority 2 determinands identification programme to the Ministry of Health’s science service provider according to their planning schedule and timelines (within 10 days of scheduled sampling date) (P2). 4. Transmit the information of Priority 2 assignation to water suppliers. Advise water suppliers of new Priority 2 assignations(P2). 5. Audit the quality of drinking water supplier’s water quality monitoring records (P1). Advice and information on the quality of drinking water supplies 1. Provide technical advice and information on public health aspects of drinking water supplies and the public health grading of water supplies to water suppliers, including the implications of the Health Act 1956 and the Drinking Water Standards for New Zealand 2005 for their operations (P2). 2. Provide advice and information to the public and organisations on issues of public health significance in respect to drinking water supplies (P2). 3. Take measures to protect and advise the community of appropriate action in the case of contamination of their drinking water supply (P1). 4. Promote the importance of clean, potable drinking water as a high priority for supply authorities (P2). 5. Make timely and professional submissions on national and regional plans and policies, district plans and policies, and local government assessments of drinking water supplies and, where appropriate, Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 12 specification November 2009 Nationwide Service Framework resource consent applications to ensure that the public health effects of drinking water supplies are considered and managed (P2). 6. Work with small drinking water supplies to assist them to prepare public health risk management plans, optimise their supplies and identify options for upgrading to provide safe drinking water supplies (P1). 7. Assist small drinking water supplies to make applications for capital assistance programme funding using Ministry of Health criteria (P1). 8. Comment as appropriate on territorial authority plans for sanitary works infrastructure planning (P2). Investigate public health problems arising from drinking water 1. Identify, investigate and follow up as appropriate incidents, complaints and notifications threatening drinking water quality (including tankered and temporary drinking water supplies) using sanitary survey, epidemiological techniques or other relevant methods. Ensure all such events are entered into WINZ database and serious incidents are reported to the Ministry of Health within 24 hours (see 7.5) (P1 for ‘incidents’ as defined by DWA Technical Manual, otherwise P2) 2. Maintain calibrated drinking water testing equipment to enable the public health unit to undertake surveillance (and incident investigation response) testing of Free Available Chlorine, Turbidity and pH (P1) Promote public health knowledge 1. Provide advice on the benefits of water fluoridation when the issue becomes a significant issue in the community (P1) by: supporting health professionals who are promoting the extension or maintenance of fluoridated water supplies ensuring appropriate education material is available to educational institutions, health professionals, territorial authorities, community groups and the public ensuring that messages on fluoridation and oral health are consistent and current and keep all health providers well informed making timely submissions on water fluoridation when appropriate. 2. Assist and work with Māori and other ethnic groups and communities as appropriate to provide advice around the benefits of water fluoridation (P2). See also the Well Child specification. Information and Reporting Requirements All reporting dates apply annually. 1. Report within one month of the end of each quarter on the DWAU activities, according to the agreed work plan for that quarter, using the format specified by the MoH (P1). 2. Before 31 March each year, advise the Ministry of Health of any objections made by drinking water suppliers in respect of Priority 2 determinand assignments specified in December of the previous year (in a form specified by the Ministry of Health) (P2). 3. Before 30 April each year (at a date and in a form specified by the Ministry of Health) provide to the Ministry of Health (P2): A list of water supplies for which data collection has been completed under the Priority 2 determinands identification programme specified for the current financial yea A list of water supplies for which data collection is uncompleted. 4. By 31 August each year, provide to the science service provider (in a form specified by the Ministry of Health) data on microbiological and chemical sampling and the status of public health risk management of drinking water supplies for the calendar year for incorporation in the Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 13 specification November 2009 Nationwide Service Framework Annual Report on the Chemical and Microbiological Quality of Community Drinking- water Supplies (P1). 4. Provide the science service provider with the assessment report on water suppliers’ public health risk management programmes and compliance with the Drinking-Water Standards for New Zealand 2005 [see 1.4] within two calendar months of completion of the assessment (P1). 5. Report serious drinking water incidents (see 5.1) to the Ministry of Health within 24 hours (P1). Notes to above table (P1) Priority One tasks: Where drinking water resources within a public health unit do not allow the completion of all tasks within this specification, tasks in this category must be prioritised for completion in preference to other tasks. (P2) Priority Two tasks: Where drinking water resources within a public health unit do not allow the completion of all tasks within this specification, tasks in this category should not be completed at the expense of completion of Priority one tasks (with the exception being if they can be completed in conjunction with a Priority One task e.g a drinking water supplier’s complaint procedures may be assessed at the same time as a Public Health Grading assessment). 5.2.6 Environmental Noise Health Goal To reduce the incidence and impact of environmental hazards by reducing the adverse health effects of environmental noise on people and communities. Rationale and Key Issues Noise is unwanted or undesirable sound and can materially affect an individual or a community’s health, well-being and enjoyment of their surroundings. As communities grow and urban environments become more densely populated and industrialised, and as traffic increases, the level of background and intrusive noise generally increases. Noise can affect people physically, psychologically and socially. Prolonged exposure to high levels of noise can damage hearing, interfere with communication, be annoying, cause mental and physical fatigue, stressinduced hypertension and ischaemic heart disease, and reduce efficiency. Adverse effects include: interference with speech communication, disturbance of rest and sleep, psycho-physiological, mental health and performance effects, effects on residential behaviour and annoyance, and interference with intended activities. Objectives Key Linkages To ensure that the health effects of environmental and non-occupational noise are considered by territorial authorities in the course of their duties. Ministry for the Environment Department of Labour Environmental Noise Analysis and Advice Service Territorial authorities and regional councils Relevant Legislation New Zealand Public Health and Disability Act 2000 Resource Management Act 1991 Health Act 1956 Health and Safety in Employment Act 1992 Local Government Act 2002 New Zealand Public Health and Disability Act 2000 Civil Aviation Act 1990 Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 14 specification November 2009 Nationwide Service Framework Components of Service Service Descriptions/Activities Public health regulatory services All environmental noise programmes will be carried out in collaboration with other relevant agencies. Liaison with territorial authorities 1. Liaise with territorial authorities on the establishment of goals, objectives, plans and priorities for environmental noise control. Resource Management Act 1991 activities 1. Make timely and professional submissions on national (including national policy statement, national environmental standards and guidelines) and regional plans and policy statements, district plans and, where appropriate, resource consent applications to ensure that the public health effects of adverse environmental noise are considered and managed. 2. Monitor territorial authorities’ actions on environmental and non-occupational noise issues to ensure that health impacts of such noise are minimised. 2. Monitor decisions made under the Resource Management Act 1991 to ensure that the health impacts of environmental and non-occupational noise have been considered. Follow up with territorial authorities where this has not occurred. Information and Reporting Requirements All reporting dates apply annually. 5.2.7 Hazardous Substances Health Goal To reduce the incidence and impact of environmental hazards by reducing the adverse health effects of hazardous substances on people and communities. Rationale and Key Issues Proper management of hazardous substances throughout their life cycle is necessary to avoid adverse health effects either from direct or indirect exposure to hazardous substances or from environmental contamination. At all stages, except where the hazard is in an occupational health setting, responsibility for protecting the public health lie with the Director-General of Health, in association with a number of other agencies. Objectives To protect the public health by minimising the harm from hazardous substances. To maintain good interagency networks to prevent harm to the public health from hazardous substances. Key Linkages Customs, Police and Transport Emergency Services Hazardous Substances and Technical Liaison Committee Ministry for the Environment Environmental Risk Management Authority Ministry of Agriculture and Forestry NZ Fire Service Department of Labour Territorial authorities and regional councils Relevant Legislation Agricultural Compounds and Veterinary Medicines Act 1997 Building Act 2004 Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 15 specification November 2009 Nationwide Service Framework Hazardous Substances and New Organisms Act 1996 Health Act 1956 Health and Safety in Employment Act 1992 Local Government Act 2002 New Zealand Public Health and Disability Act 2000 Resource Management Act 1992 Components of Service Service Descriptions/Activities Public health regulatory services All hazardous substances programmes will be carried out in collaboration with other relevant agencies. Liaison with territorial authorities 1. Liaise with territorial authorities on the establishment of goals, objectives, plans and priorities for hazardous substances control. Audit compliance with relevant Acts and Regulations 1. Audit compliance with, investigate breaches of, and where appropriate, enforce the relevant Acts and Regulations, including: 2. Seek to develop a Memorandum of Understanding (or equivalent) with territorial authorities that describes roles and responsibilities in this area. Polychlorinated biphenyl (PCB) storage and surveillance checks supervision and inspection of imported hazardous substances attending hazardous substances incidents consider and review permissions for applications of vertebrate toxic agent monitoring storage and display of hazardous substances for retail sale. 2. Ensure that the conditions imposed by the HSNO designated officer granting permits for the use of controlled vertebrate toxic agents are complied with. Audits should be conducted to ensure compliance, as appropriate. Maintain an emergency response capacity Maintain effective risk management strategies and action plans for emergency situations involving hazardous substances, including deliberate chemical contamination. Maintain inspection, monitoring and surveillance systems 1. Inspect and report on premises in which PCBs (are used and/or stored). Report on non-compliance with conditions of exemption, and lapsed exemptions. 2. Prepare and update a database of locations for ownership of PCBs. 3. Implement the recommendations on the Investigation and Surveillance of Agrichemical Spraydrift Incidents: guidelines for public health services including providing annual returns from Driftnet to the science provider as requested. 4. Participate in the Chemical Injury and other notifiable condition surveillance systems, including exposures to asbestos in a non-occupational environment. Interagency networking and administrative procedures 1. Represent public health interests at meetings of the Hazardous Substances Technical Liaison Committee (or equivalent body). 2. Provide input into territorial authorities’ hazard and risk assessment and management systems so that risks to public health from hazardous substances are addressed. 3. Maintain networks with PCB holders, the electrical industry and disposal agents to ensure that the storage, transportation and disposal requirements Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 16 specification November 2009 Nationwide Service Framework are environmentally sound. Promote public knowledge Information and Reporting Requirements 4. Seek to develop a Memorandum of Understanding (or equivalent) with other agencies that describes roles and responsibilities in this area (consistent with relevant national MoUs). 1. Promote public knowledge on the risks of non-occupational exposures to hazardous substances by: providing public health advice and information on hazardous substances to the public, health professionals and organisations. Advising on the safe management of hazardous substances such as leadbased paint including their removal and disposal from contaminated areas. All reporting dates apply annually. 1. By 30 June each year provide: Note: summaries for the past year (to 30 June) and estimates for the coming year (1 July to 30 June) of the nature and level of inspection and enforcement services under HSNO Act s98(2), such matters as: - the planned and actual levels of inspection/investigation - emergency responses - compliance orders and infringement notices and warnings issued - a list of the premises or situations inspected - investigations and actions proposed and undertaken - prosecutions. summaries for the past year (1 July to 30 June) of the notifications of hazardous substances hospital admissions injuries and GP notifications reported to the Medical Officer of Health under the HSNO Act s143 including: - the hazardous substances injury classification (eg. toxic or corrosive) - the site/location (workplace, school, home etc) - where available, ethnic breakdown, gender, and age. furnishing information to the Ministry of Health will be sufficient for Medical Officers of Health to meet their statutory requirement to supply the information, in an anonymised form, to the Minister of Health. 2. Provide annual returns to the science provider on the incidence of agrichemical spray drift complaints using the DriftNet surveillance system. 3. Provide copies of VTA permits to ERMANZ every time they are issued. 4. Report to the Ministry of Health as required on: PCB use and storage exemptions HSNO incident or emergency situations 5. Immediately, or within 24 hours of occurrence of a public health event or emergency with inter-district, national or potentially international implications, submit a report to the Environmental and Border Health Protection Team and a copy to your Public Health Operations portfolio manager. Formats for the reports will be outlined in the Hazardous Substances section of the Environmental Health Protection Manual. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 17 specification November 2009 Nationwide Service Framework 5.2.8 Ionising Radiation/Non-Ionising Fields Health Goal To reduce the incidence and impact of environmental hazards by developing strategies to prevent or control the adverse impacts of ionising and non-ionising radiation. Rationale and Key Issues Exposure to radiation can pose a significant threat to the public health. Objectives To work with the National Radiation Laboratory to minimise risk to health from ionising/non-ionising radiation. Key Linkages Hazardous Substances Technical Liaison Committees Ministry for the Environment National Radiation Laboratory Port authorities Transport industry Relevant Legislation Health Act 1956 Microwave Ovens Regulations 1982 Land Transport Act 1988 Local Government Act 2002 Marine Pollution Act 1974 Relevant National Environmental Standards and Policy Statements New Zealand Public Health and Disability Act 2000 Ozone Protection Act 1981 General Harbour (Ship, Cargo and Dock Safety) Regulations 1968 Radiation Protection Act 1965 Radiation Protection Regulations 1982 Resource Management Act 1991 Ministry for the Environment/Ministry of Health National Guidelines for Managing the Effects of Radio-frequency Transmitters. Components of Service Service Descriptions/Activities Public health regulatory services Provide services in accordance with the National Radiation Laboratory Radiation Incident Response Plan. Work cooperatively with the National Radiation Laboratory Activities will include: ensuring that appropriate action is taken to minimise risks and to protect the public health conducting surveillance and evaluation of the management of radiation with reference to statute, guidelines and best practice assessing the health risks associated with exposure to radiation as part of any population health status review identifying and investigating public health risk associated with radiation including epidemiological field investigation where appropriate Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 18 specification November 2009 Nationwide Service Framework developing contingency plans and response capability to deal with radiation contamination/hazard incidents, including counter-terrorism, in accordance with the National Radiation Laboratory Radiation Incidence Response Plan Promote public health knowledge Provide public health advice on the health effects of ionising and nonionising radiation to organisations and the public. Purchase Units, Information and Reporting Requirements All reporting dates apply annually. Immediately, or within 24 hours of occurrence of a public health event or emergency with inter-district, national or potentially international implications, submit a report to the Environmental and Border Health Protection Team and a copy to your Public Health Operations portfolio manager. 5.2.9 Public Health Emergency Planning and Response Health Goal To reduce the incidence and impact of environmental hazards on communities and individuals in the event of a public health or other emergency. Rationale and Key Issues The impact of public health emergencies, including civil defence emergencies, can be mitigated if providers have prepared contingency plans. Examples include communicable disease outbreaks, exotic mosquito interceptions and incursions, terrorism threats, and the chemical incidents, as well as flooding or earthquakes. Pre-disaster public health planning and interagency liaison can also improve preparedness for the response and recovery phases, and reduce the overall impacts on the public health, of a disaster. Part six of the National Civil Defence Plan sets out the functions, roles and responsibilities and the Civil Defence Act 1983 sets out the obligations of health sector agencies in relation to civil defence. Section 70 of the Health Act 1956 describes the special powers of the Medical Officer of Health in relation to infectious and notifiable diseases when a national or regional disaster has been declared under the Civil Defence Act, or in the event of special authorities. Objectives To be well prepared for any civil defence emergency or other emergency where there is a risk to public health, including counter-terrorism. To act, in association with other agencies, to protect the public health in the event of such an emergency Key Linkages Relevant Legislation Ambulance Services, Defence Forces, Order of St John, Red Cross Civil Defence Organisation Hazardous Substances Technical Liaison Committee Territorial authorities and regional councils Civil Defence Emergency Management Act 2002 National Civil Defence Plan Hazardous Substances and New Organisms Act 1991 Health Act 1956 Local Government Act 2002 New Zealand Public Health and Disability Act 2000 Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 19 specification November 2009 Nationwide Service Framework Components of Service Service Descriptions/Activities Public health regulatory services All emergency management planning and programmes will be carried out in collaboration with other relevant agencies. Act in emergency situations Take appropriate emergency actions, as the need arises. This includes liaison with and taking directions from other agencies involved. Maintain civil defence and public health emergency planning and response capacity 1. Participate in the development, review and revision of regional and local civil defence contingency planning and ensure they adequately address planning for the provision of: basic sanitary services including basic safe water supplies to communities basic safe shelter safe food to communities basic facilities for the maintenance of personal hygiene removal and hygienic disposal of the dead removal and disposal of hazardous substances prevention and control of communicable disease outbreak 2. Communication with the Ministry of Health. 3. Identify resources needed to support and carry out public health action and maintain an inventory of current resources, including vehicles, communication systems, protective clothing, identification cards and equipment. 4. Maintain, test and regularly review contingency plans for responding effectively to a range of public health emergencies, such as natural disasters, chemical spills, emergent diseases, communicable disease outbreaks, food-borne illnesses or food contamination incidents. Assess risk of emergency Interagency collaboration Promote public health knowledge of emergency planning and Identify predominant natural and human activity hazards (including deliberate contamination) in the region that are likely to give rise to emergency situations affecting public health. 2. Carry out risk assessment of these events and check that emergency planning and response capacity is sufficient to deal with those risks. The plan will include preparedness, mitigation, response and recovery. Participate in national, regional and local meetings, exercises and training opportunities. Provide services for, be directed by, and report to civil defence authorities in the event of an emergency. 3. Seek to develop a Memorandum of Understanding (or equivalent) with Regional Councils which describes roles and responsibilities in this area. Ensure appropriate educational and promotional material is provided to institutions, health professionals, territorial authorities and community groups on the public health aspects of planning for, and responding to, emergency situations. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 20 specification November 2009 Nationwide Service Framework response Information and Reporting Requirements All reporting dates apply annually. Immediately, or within 24 hours of occurrence of a public health event or emergency with inter-district, national or potentially international implications, submit a report to the Environmental and Border Health Protection Team and a copy to your Public Health Operations portfolio manager. 5.2.10 Recreational Waters Health Goal To reduce the incidence and impact of environmental hazards associated with recreational waters. Note: Recreational water includes swimming, spa and thermal pools, and natural water for water contact activity. Rationale and Key Issues Hazards posed by recreational water include unsatisfactory water quality and associated disease risks. Objectives To protect the public health by preventing the risk of disease associated with the public use of recreational waters. To protect the public health by minimising the risk associated with the use of recreational waters. Key Linkages Ministry for the Environment Ministry of Fisheries New Zealand Food Safety Authority Territorial authorities and regional councils Relevant Legislation Fencing of Swimming Pools Act 1987 Health Act 1956 Territorial Authority Bylaws Local Government Act 2002 Resource Management Act 1991 New Zealand Public Health and Disability Act 2000 NZS 5826: 2000 Pool Water Quality Ministry of Health/Ministry for the Environment Microbiological Water Quality Guidelines for Marine and Freshwater Recreational Areas. Components of Service Service Descriptions/Activities Public health regulatory services All border health protection programmes will be carried out in collaboration with other relevant agencies. Work collaboratively with Regional Councils and Territorial 1. Make timely and professional submissions on national and regional plans and policies, district plans and policies and, where appropriate, resource consent applications to ensure that the public health effects of adverse recreational water quality are considered and managed. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 21 specification November 2009 Nationwide Service Framework Authorities 2. Encourage Regional Councils to clearly identify existing or potential recreational waters, which do not meet minimum microbiological water quality guidelines in the Ministry of Health/Ministry for the Environment Microbiological Water Quality Guidelines for Marine and Freshwater Recreational Areas. 3. Encourage the grading of bathing beaches as outlined in the Microbiological Water Quality Guidelines for Marine and Fresh Water Recreational Areas. 4. Provide advice to territorial authorities on the need for warning signs to be placed around areas of high public health risk. 5. Advise Regional Councils to ensure that waters classified as CR (suitable for contact recreational purposes) meet at least the minimum requirements for the protection of health. 6. Seek to develop a Memorandum of Understanding (or equivalent) with Regional Councils, which describes roles and responsibilities in this area. Increase and maintain compliance with legal obligations 1. Encourage territorial authorities to monitor compliance with the Fencing of Swimming Pools Act 1987. Promote public health knowledge 1. Participate in school safety education initiatives for recreational water. See also the tier two Injury Prevention Services service specification. 2. Encourage territorial authorities and pool managers (including school pools) to implement the requirements of NZS5826: 2000 Pool Water to avoid or reduce public health risks. 3. Promote good supervision of preschool children in the vicinity of pools and other recreational waters including promoting guidelines for parents of infants/toddlers (using ‘Before You Take to the Water’ health education resource). Information and Reporting Requirements All reporting dates apply annually. 5.2.11 Resource Management Health Goal To reduce the incidence and impact of environmental inequalities across sectors by ensuring public health issues are identified and addressed in decisions made on the sustainable management of natural and physical resources and social environments. Rationale and Key Issues Land, air and water are the basic elements of the environment necessary to support human life. These elements must be sustainably managed in a way or at a rate that enables people and communities to provide for their social, economical and cultural well-being and for their health and safety. Objectives To ensure that resource management decisions do not impact negatively on the public health To develop strong networks with agencies involved in sustainable resource management. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 22 specification November 2009 Nationwide Service Framework Key Linkages Relevant Legislation Ministry for the Environment Other service providers Regional Councils Territorial authorities. Building Act 2004 Health Act 1956 Resource Management Act 1991 Local Government Act 2002 New Zealand Public Health and Disability Act 2000. Components of Service Service Descriptions/Activities Provide advice and input into activities of linkage agencies 1. Make timely and professional submissions on local government assessments of sanitary works, national policy, standards or guidelines, regional plans and policy statements, and district plans, where appropriate, and resource consent applications to ensure that the public health aspects are considered. 2. Liaise and, where appropriate, undertake joint projects with consent authorities and affected communities to ensure that public health aspects of planning and resource management are considered. 3. Provide technical advice and information to regional and local government. 4. Review and advise on territorial authority annual plans. 5. Seek to develop a Memorandum of Understanding (or equivalent) with Regional Councils that describes roles and responsibilities in this area. 6. Comment as appropriate on territorial authority plans for sanitary works infrastructure planning. Health promotion activities Inform other agencies and the public on the public health aspects of matters relating to sustainable resource management. Information and Reporting Requirements All reporting dates apply annually. 5.2.12 Sewage Treatment and Disposal Health Goal To reduce the incidence and impact of environmental hazards from liquid and solid waste management. Rationale and Key Issues Sewage contains a large number of potential pathogens. Unsatisfactorily managed sewage collection, treatment and disposal can pose a significant threat to public health. Objectives To reduce or prevent any potential health risks from sewage treatment or disposal. Key Linkages Department of Building and Housing Department of Conservation Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 23 specification November 2009 Nationwide Service Framework Ministry for the Environment Public Health Engineering Consultants Territorial authorities and regional councils Relevant Legislation Building Act 2004 Building Regulations 1992 (under review) Health Act 1956 Local Acts of Parliament Local Government Act 2002 Marine Pollution Act 1972 New Zealand Public Health and Disability Act 2000 Resource Management Act 1991 Components of Service Service Descriptions/Activities Public health regulatory services All sewage treatment and disposal programmes will be carried out in collaboration with other relevant agencies. Maintain monitoring surveillance systems 1. Make timely and professional submissions on national and regional plans and policies, district plans and policies, local government assessments of sanitary works and, where appropriate, resource consent applications to ensure that the public health effects of sewage treatment and disposal are considered and managed. 2. Conduct routine surveillance and evaluation of the performance of controlling authority management of public health aspects of the service area with reference to statute, guidelines, standards, resource consent conditions and accepted public health practice, in respect of sewage collection and disposal and the microbiological quality of the receiving water. 3. Investigate and assess the public health need for sewerage systems in areas not adequately serviced. 4. Undertake sanitary surveys as required. 5. Report and make recommendations using Ministry of Health criteria, including prioritising in their region, applications for sanitary works subsidies. 6. Comment as appropriate on territorial authority plans for sanitary works infrastructure planning. Promote public health knowledge and advocate for public health action 1. Promote knowledge of local public sewerage systems and sewage disposal, and advocate for improvement where this is considered necessary. 2. Seek to develop a Memorandum of Understanding (or equivalent) with Regional Councils that describes roles and responsibilities in this area. Information and Reporting Requirements All reporting dates apply annually. and Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 24 specification November 2009 Nationwide Service Framework 5.2.13 Sewage Waste Management Health Goal To reduce the incidence and impact of environmental hazards from gaseous, liquid and solid waste management. Rationale and Key Issues Liquid and solid wastes may contain hazardous materials and can provide a medium to support pathogens and disease vectors. Unsatisfactory operated liquid and solid waste collection, treatment and disposal systems can pose a threat to the public health. Objectives To reduce or eliminate any potential harmful effects of waste management on the public health. To ensure public health issues are identified and addressed in decisions made on the sustainable management of natural physical resources. Key Linkages Department of Conservation Environmental Risk Management Authority (ERMANZ) Ministry for the Environment Territorial authorities and regional councils Relevant Legislation Hazardous Substances and New Organisms Act 1996 Health Act 1956 Litter Act 1979 Local Government Act 2002 Marine Pollution Act 1972 New Zealand Public Health and Disability Act 2000 Resource Management Act 1991 Components of Service Service Descriptions/Activities Public health regulatory services All waste management programmes will be carried out in collaboration with other relevant agencies. Maintain monitoring and surveillance systems 1. Make timely and professional submissions on national and regional plans and policies, district plans and policies, and local government assessments of sanitary works and, where appropriate, resource consent applications to ensure that the public health effects of waste management are considered and managed. 2. Provide a system for routine and regular surveillance and monitoring of significant public health risks in waste management. 3. Undertake waste surveys with other agencies as appropriate. 4. Seek to develop a Memorandum of Understanding (or equivalent) with Regional Councils and Territorial Authorities that describes roles and responsibilities in this area. Information and Reporting Requirements All reporting dates apply annually. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 25 specification November 2009 Nationwide Service Framework 5.2.14 Other Regulatory Activities Health Goal To reduce the incidence and impact of environmental hazards by developing strategies to prevent or control the adverse impacts of environmental health issues. To reduce the incidence and impact of environmental inequalities across sectors. To reduce the incidence and impact of settings-based environmental health issues. Rationale and Key Issues There are many regulatory and health protection activities that are too infrequent, small, or localised to a particular area and, therefore, do not require a separate service specification in their own right to protect the public health. The specification groups these activities together so they are covered and can be included in health protection activities. Objectives To allow for all aspects of regulatory and health protection work to be included in service provision. Key Linkages Territorial authorities and regional councils. Relevant Legislation Components of Service Public health regulatory services Health Act 1956 New Zealand Public Health and Disability Act 2000 Resource Management Act 1991. Service Descriptions/Activities All border health protection programmes will be carried out in collaboration with other relevant agencies. To maintain comprehensive health protection and regulatory services 1. To perform activities and services at a local level where these are considered necessary and are not included elsewhere in the Physical Environment specifications. Information and Reporting Requirements 1. All reporting dates apply annually. 2. Make timely and professional submissions on national and regional plans and policies, district plans and policies and, where appropriate, resource consent applications to ensure that the public health effects of activities are considered and managed. 2. As soon as practicable and not later than 14 days after the occurrence of any emergent issue, unusual event or public health investigation which has potential inter-district, national or international implications, submit a report to the Environmental & Border Health Protection Team and a copy to your Public Health Operations portfolio manager. 3. Reports Verifying Ongoing Competence of Statutory Officers By 31 July each year, each public health manager will provide a written report to the Environmental & Border Health Protection Team which identifies all statutory officers in the public health unit and provides the following information for each officer: Full name Position (title) Statutory appointments Training attended during the year Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 26 specification November 2009 Nationwide Service Framework Verification that attendance at training relevant for each statutory appointment has been undertaken within the previous 5 years Verification that the personal and practical skills and competencies have been retained Verification that the manager is confident that the officer is competent to exercise the statutory powers, including in emergencies. Note: for medical officers of health, evidence of competence will be provided by their ongoing registration as public health medicine practitioners and their attendance at four out of six medical officer of health training sessions over a two year period. 4. Enforcement Public health units shall furnish quarterly compliance and enforcement returns to the Ministry (in a format to be specified by the Ministry) to enable the Ministry to monitor the level, nature and range of enforcement activity being undertaken. Social Environments - Early Childhood Centres Health Goal To reduce the incidence and impact of settings-based environmental health issues across early childhood education settings. Ministry of Health Expectations The Ministry of Health expects that the service specification will be delivered through the mandate that staff have, in undertaking visits: that the potential licensee has requested a pre-licensing health report and/or the public health unit been invited to undertake visits by the licensee or Ministry of Education officials to address a health concern they may have. The undertaking of visits and provision of environmental health advice to early childhood centres should be part of the more general role in improving, promoting and protecting public health through the early childhood setting. However it needs to be recognised that these do not have a statutory mandate under the Education (Early Childhood Services) Regulations 2008 and that staff are providing advice and seeking cooperation, not exercising statutory powers. Should a centre refuse entry to an officer to undertake these environmental health visits, there is no power of entry or inspection. However, in this instance, it would be appropriate to discuss the centre’s response with the Ministry of Education. Rationale and Key Issues Early childhood centres play an important role in the education, health and life of preschool children and provide excellent avenues for health promotion. Early childhood centres may present a large number of potential risks to children’s health and safety, particularly disease transmission. These risks also have implications for the health and well-being of the wider community, particularly friends, teachers, parents, caregivers and other family members of the children attending the centres. The identification, assessment and management of health and safety risks in the centres is a priority. The Secretary of Education relies on advice from designated officers as to the adequacy and suitability of the health and safety provisions for children attending early childhood centres, particularly in the granting of licences by the Ministry of Education. Prior to using licences for new early childhood education and care centres (ie centre-based services), all prospective service providers are required to obtain health report from the local public health service unit. This is in accordance with Regulation 9(2) in the Education (Early Childhood Services) Regulations 2008. Note that this requirement only applies to new centred-based services only. It does not apply to new or existing home-based or hospital-based services, or existing centred-based services. Section 310(2)(i) of the Education Act 1989 makes this clear in relation to home-based and hospital-based services. In relation to existing centre-based, home-based and hospital-based services, however, health reports are discretionary. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 27 specification November 2009 Nationwide Service Framework Objectives To promote the health and well being of children attending early childhood centres through population-based initiatives. To work intersectorally to promote the health and well-being of children attending early childhood centres. Key Linkages Early Childhood Centre Group, National Office, Ministry of Education, , Ministry of Education Regional Offices Occupational Safety and Health Division (OSH), Department of Labour Department of Building and Housing National and regional Early Childhood Centres Associations Other service providers Territorial authorities. Relevant Legislation Building Act 2004 Building Regulations 1992 (under review) Education Act 1989 Education Amendment Act 2006 Education (Early Childhood Services) Regulations 2008 Education (Home-based Centre) Order 1992 (valid until 2014) Fencing of Swimming Pools Act 1987 Food Act 1981 Food Regulations 1984 Hazardous Substances and New Organisms Act 1996 Health Act 1956 Health (Infectious and Notifiable Diseases) Regulations 1966 Health (Immunisation) Regulations 1995 Food Hygiene Regulations 1974 Health and Safety in Employment Act 1992 New Zealand Public Health and Disability Act 2000 Smokefree Environments Act 1990 Components of Service Service Descriptions/Activities Public health regulatory services All early childhood setting programmes will be carried out in collaboration with other relevant agencies. Increase and maintain compliance with statutory public health requirements 1. Carry out inspections of early childhood centres, in response to requests. Advice and information for 1. Advise early childhood centres on population-based health strategies to improve, promote and protect the health of the children attending. 2. Carry out statutory obligations for licensing of early childhood centres including assessing health and safety risks to ensure compliance with relevant legislation, standards and guidelines. 3. Conduct routine surveillance including compliance by the licensee of the premises with regulatory responsibilities, including Education (Early Childhood Centres) Regulations 1998. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 28 specification November 2009 Nationwide Service Framework early childhood centres 2. Advise on health promotion strategies that will improve the health and wellbeing of children and their family/whānau. 3. Advise early childhood centre staff and parents on health and safety risks to protect the health of children attending. 4. Advise on health and safety requirements for new and proposed centres prior to licensing. 5. Undertake education initiatives where appropriate to improve and protect the health of children attending centres. Communication and liaison 1. Establish and maintain working relationships with the Ministry of Education, the Occupational Safety and Health Division of the Department of Labour, and the licensee to promote good public health practices and standards in early childhood centres. 2. Maintain working relationships that respect the cultures, organisational requirements and philosophies of the various early childhood centre organisations. 3. Make submissions and provide input and feedback where appropriate to relevant documents and legislative changes. Information and Reporting Requirements All reporting dates apply annually. Social Environments -Healthy Urban Design/Form Rationale and Key Issues New Zealand is a relatively urbanised country with more than 85% of its population living in urban/suburban environments. A range of health problems are emerging that are associated with modern urban life. Increased reliance on cars for example, can lead to physical inactivity and increasing levels of obesity. Reliance on private vehicles, congestion and greater travelling distances also cause air pollution. A lack of access to affordable transport can restrict access to basic goods and services. The Healthy Cities/Communities (HCC) project is a World Health Organisation programme that was first started in New Zealand in 1988. There are currently nine HCC in operation. The project strives to improve environmental health and better living conditions in urban areas. Healthy Cities are a recognition that a person’s health is affected by their environment e.g. urban design/form as well as the quality of health care. Local authorities have a key role with the implementation of HCC and there are significant opportunities for HCC programmes to involve Maori. Many local authorities in New Zealand are doing work to improve urban planning and design. This includes work to design areas that are well serviced by public transport, are user-friendly for walking and cycling, and have ready access to services and facilities (including hospitals, schools, leisure facilities and supermarkets). It can also include projects to ensure or encourage new building developments to consider things like parking, noise and amenity, access to outdoor space, insulation and sustainable building principles and features. Safe Community accreditation also involves extensive urban planning. The Urban Design Protocol (2005) administered by the Ministry for the Environment is a voluntary commitment by central and local government and other stakeholders, including property developers and investors, to undertake specific urban design initiatives. The protocol therefore affects formal district plans made under the RMA. The New Zealand Urban Design Protocol has a vision of making New Zealand towns and cities more successful through quality urban design.1 It 1 http://www.mfe.govt.nz/publications/urban/design-protocol-mar05/html/index.html Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 29 specification November 2009 Nationwide Service Framework has a wide range of signatories, including central and local government, businesses, sector groups and others. Related to the Protocol are programmes involving Crime Prevention Through Environmental Design (CPTED) (see section on ‘crime prevention’ below) and more recently the Te Aranga Māori Cultural Landscapes Strategy. Initiatives such as Healthy Cities are based on principles identified in the Ottawa Character for Health Promotion (1996). Access to adequate housing is one of the important factors for public health acknowledged in the Ottawa Charter. There is strong evidence that improving urban planning and design including sustainable building principles is an effective way of reducing inequalities in health and improving well being. The potential impact of urban form on public health relates to sense of community and mental health. WHO estimate that by 2020, mental ill health will be the third leading cause of disability life-adjusted years globally. There is strong evidence that the built environment affects the transport-mode choices of both adults and children. A growing body of evidence confirms that neighbourhoods characterized by low density, poorly connected street networks and poor access to shops and services are associated with low levels of walking. Urban sprawl or low walkability appears to be associated with obesity. Traffic exposure decreases walking in children because of parental concerns about safety. Reduced local walking, affects opportunities for causal interactions between neighbourhoods. Objectives To work collaboratively with the local government sector as they develop urban planning related policy, rules etc initiatives which relate to urban design/form. Where appropriate advocate the use of health impact assessment for proposals that include urban design/form. Key Linkages Ministry for the Environment Department of Internal Affairs Department of Building and Housing Ministry of Health’s Health Impact Assessment Support Unit Relevant Legislation 7. Building Act 2004 Resource Management Act 1991 Local Government Act 2002 Components of Service Service Descriptions/Activities Work cooperatively with local government in the development of urban design/form policies that promote health and wellbeing of communities Purchase Units, Information and Reporting Requirements Encourage and assist Council to develop and implement polices through processes such as the review of district plans including variations or plan changes or Long Term Council Community Plans that address the wider determinants of health. Consider becoming a signatory to the NZ Urban Design Protocol (2005) Where appropriate advocate the use of health impact assessment for proposals that include urban design/form. Where appropriate promote the Healthy Cities/communities concept Purchase units are as for the tier two Public Health Services service specifications for Social Environment. All reporting dates apply annually. Exclusions Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 30 specification November 2009 Nationwide Service Framework This service specification excludes services described in the tier two Social Environments Health Promoting Schools service specification that covers policy-level health impact assessment activities; see Social Environments Health promoting Schools tier two service specification. This Physical Environment Public Health service specification relates more directly to project-level health impact assessment methods and approaches used in resource management processes. 8. Quality Requirements The Service must comply with the Provider Quality Standards described in the Operational Policy Framework or, as applicable, Crown Funding Agreement Variations, contracts or service level agreements. Providers of environmental health services should comply with all relevant manuals, standards and guidelines promulgated by the Ministry – this includes in particular the Environmental Health Protection Manual and any other guidance material cited in the relevant tier two (and tier three) service specifications. 9. Purchase Units and Reporting Requirements Purchase Units are defined in the joint DHB and Ministry’s Nationwide Service Framework Data Dictionary. The following Purchase Unit applies to this Service. PU Code PU Description PU Definition PU Unit of Measure Unit of Measure Definition National Collections or payment systems RM00108 Physical Environment Air quality (indoor and outdoor) Biosecurity and quarantine Burial and cremation Contaminated land Drinking water quality Early childhood centres Environmental noise management Hazardous substances Ionising/non-ionising radiation Public Health emergency planning and response Recreational water Resource management Sewage treatment and disposal Shellfish and shellfish water Waste management (liquid and solid waste) Other regulatory activities. Service Service purchased in a block arrangement uniquely agreed at a local level. National Nonadmitted Patient Collection NNPAC (Optional) The Service must comply with the requirements of national data collections (if applicable). 9.1 Additional Reporting Requirements All reporting requirements are detailed in the individual contracts. Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service 31 specification November 2009 Nationwide Service Framework Figure 1: Outcomes-focused Framework for the Environmental Health and Social Environments Societal Housing: quality, affordability, accessibility Pacific and global communities Water incl drinking and recreational Energy Education incl schools and ECCs Sanitation, Sewage, Waste mgmt Urban Planning and Design Exposed populations Industry/Workplaces Indoor and Outdoor Air Quality Social developments incl migration Border health protection (incl trade) Natural disasters and emergency management Sustainable development incl tourism Industry/Workplaces Hazardous substances incl contaminated sites Local Government 10 to 20 years Examples of Medium Term Outcomes 5 to 10 years Climate change Mass gatherings incl World Cup 2011 Environmental Health Indicators Reduction in the incidence and impact of settings-based environmental health issues Measuring, Monitoring, and Reporting of Reduction in the incidence and impact of environmental inequalities across sectors Measuring, Reduction in the incidence and impact of environmental hazards Monitoring, and Reporting of Environment al Health Indicators Level Outcomes Vital Few Outcomes Public health and whanau health are improved through the protection and promotion of healthy communities and healthy environments including the global environment EH Programmes Short Term Outcomes and Outputs EH Programmes EH Programmes and Projects and Projects Service Measuring, Monitoring and Reporting to Funder and Projects 1 to 3 years Supporting Legislation and Policy (eg Health Act 1956, Resource Management Act 1991, Local Government Act 2002, Achieving Health for All People, Public Health Legislation Review, standards including global standards), Intersectoral Service Planning and Delivery, Leadership incl advocacy and champions, Research and Information, Effective Action (including guidelines, best practice, advice and information), Monitoring and Evaluation, New Technologies, Health Impact Assessment (including precautionary approaches, risk perception and risk communication) Public Health Services Regulatory Services and Reporting Physical Environments Health tier two service specification November 2009 Nationwide Service Framework 33