CHURCHILL HOSPITAL- Oxford Cancer Hospital
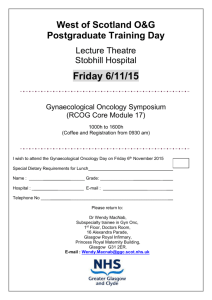
advertisement

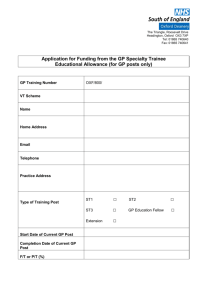
OXFORD DEANERY SPECIALTY TRAINING PROGRAMME IN GYNAECOLOGICAL ONCOLOGY About Oxford Deanery The Oxford Deanery covers the counties of Oxfordshire, Berkshire and Buckinghamshire, with Banbury and Milton Keynes in the North, to Reading and Slough in Berkshire and High Wycombe and Aylesbury in the West. The Oxford Deanery is part of the South Central Strategic Health Authority which serves a large population and covers the regions mentioned above as well as the Wessex Deanery areas of Hampshire and the Isle of Wight. The Oxford Deanery is responsible for the training of some 1500 trainees. The Oxford Deanery is a relatively small deanery with a defined geographical area which serves as a single unit of application. In the majority of cases successful candidates will be asked to preference their choice of location for either one or two years. Some programmes will require successful candidates to indicate a location and specialty. Future placements will usually be based on individual training and educational needs. Please note that applications are to the Oxford Deanery as a whole. This may mean that you may be allocated to any geographic location within the Oxford Deanery depending on training needs. The Subspeciality Gynaecologial Oncology Training Programme The gynaecological oncology training programme is a 2 or 3year programme, starting at StR6 or higher. The trainee must have already completed at least 5 years of Speciality training. The trainee will be monitored for satisfactory progress and subject to annual reviews in the form of ARCPs. Progression on the programme will be dependent upon these reviews and on the RCOG subspeciality reviews. This post has been approved for Specialist Training by the Royal College of Obstetricians and Gynaecologists and will lead to the award of CCT or CESR(CP). The Postgraduate Dean has confirmed that this post has the necessary educational and staffing approvals. Trust Information Oxford Radcliffe Hospital Trust The Oxford Radcliffe Hospitals Trust (ORH) is one of the largest teaching trusts in the country, with a national and international reputation for its services and its role in teaching and research. It employs around 10,000 staff, and has an annual turnover of over £600 million. It provides a district general hospital service for approximately 700,000 people in Oxfordshire and the neighbouring counties. With in excess of 1200 staffed beds, the Trust’s specialist services serve a population of around 2.5 million in Oxfordshire, Buckinghamshire, Berkshire, Wiltshire, Gloucestershire and Northamptonshire. In addition to the normal range of specialist services, the Trust also provides other highly specialised treatment and care for a still wider catchment area. In 2009/10, there were: 614,056 outpatient appointments 123,592 attendances at the emergency departments 79,802 admissions for emergency assessment and treatment 62,062 admissions for treatment as day cases 19,688 admissions for treated as inpatients 8,077 babies delivered CHURCHILL HOSPITAL- Oxford Cancer Hospital The Oxford Gynaecological Cancer Centre was recognized in 2005 as the Regional Centre for the surgical care of women with gynaecological cancer in the Thames Valley Region in accordance with Improving Outcome Guidance (IOG) and the Calman-Hine model for delivery of cancer care. The Centre serves a population of approximately 2 million people. The service moved to the new Oxford Cancer Centre in April 2009, where the surgical cancer care is provided, along with medical and clinical oncology, palliative medicine and all other allied services. In-patient care for the Centre is provided at the Jane Ashley Ward, a 20-bed women’s ward that is shared with the Breast Cancer Team. During the year April 2009-2010, there were over 2500 outpatient appointments, and nearly 300 major surgical procedures performed. Surgical procedures included laparoscopic pelvic and para-aortic lymphadenectomies, total laparoscopic hysterectomies, laparoscopic radical hysterectomies, multiorgan debulking surgery for ovarian cancer including lower and upper abdominal surgery and exenterative procedures. In addition, plans are underway for introducing sentinel lymph node mapping in vulval cancer. DEPARTMENT MEMBERS: Lead Clinician and Director of Training: Mr Sean Kehoe, Consultant Gynaecological Oncologist. Consultants: Dr Ahmed Ahmed, Reader and Consultant Gynaecological Oncologist/Trainer Mr Roberto Tozzi, Consultant Gynaecological Oncologist/Trainer Replacement post, Consultant Gynaecological Oncologist - 2011 Trainees: These include two Clinical Fellows and two rotating trainees (ST3-5 and ST6/7) from the JRH. There is also an ‘SHO’ tier to cover the ward and involved in Hospital at Night. Multidisciplinary team leads Clinical Nurse Specialist: Margaret Instone. Pathology: Dr. Sanjiv Manek. Radiology: Dr. Niall Moore Medical Oncology: Dr. S Nicum. Clinical Oncology: Dr. A Horne. RCOG College Tutor Dr. Rebecca Black, Consultant Obstetrician. Teaching – The Oxford Gynaecological Cancer Centre has been recognized by the RCOG for subspecialty training since 2003 and, has since, been providing excellent opportunities for multi-faceted training in Gynaecological Oncology. The Centre also provides training for outstanding International Fellows who receive structured Gynaecological Oncology training. In addition, Obstetrics and Gynaecology trainees rotate through the centre to complete their core Gynaecological Oncology training module and sometimes the ATSM in Gynae oncology. Research and Audit The Centre has a national and international reputation for conducting excellent research using state of the art methodology. Research activities range from leading on national randomized clinical trials to conducting laboratory-based translational research trials. The centre benefits from established collaborations with world-class research institutes at Oxford such as the Old Road Biomedical Research Campus and the Weatherall Institute of Molecular Medicine. The recent appointment of Dr Ahmed Ahmed as Clinical Reader, who leads a programme in translational research in ovarian cancer, has significantly increased the opportunities of the centre. The SST will be expected to have an active role in both audit and research programmes. If the research component of SST has not been completed, time will be made available to perform the research needed to write 2 publications. Duties of Post – A. PRINCIPAL RESPONSIBILITIES Contribute fully to patient care within the department. Assist the consultants within the department to manage patients. To be involved in the personal training and development and in the teaching of medical students and junior medical colleagues as appropriate. The trainee will be assessed on an annual basis at a formal ARCP review as part of the Oxford Deanery Obstetrics and Gynaecology training scheme and also by the RCOG subspeciality reviews. In addition, there are 3 monthly inhouse meetings with consultant trainers to review progress. A logbook must be maintained both for SST oncology training and the RCOG advanced Core Curriculum. B. DAILY COMMITMENT This subspecialty training focuses on obtaining “hands-on” experience in the relevant multidisciplinary areas in accordance with the RCOG requirements. The duties will be arranged in 6 month ‘blocks’ to accommodate the specific areas of clinical work and research and the obstetrics on-call needs (see attached provisional time table). The timetable may be adjusted to suit training requirement. The post is primarily based at the Churchill Hospital Site. However, the obstetric on call commitment is at the Women’s Centre on the John Radcliffe Hospital Site. C. DESCRIPTION OF WORK PATTERN The SST will be expected to take part in the general Obstetrics and Gynaecology evening/night time/weekend On-Call rota at the JRH. There will be daytime emergency cover of the oncology Unit. When on call, a named consultant will always be On-Call for advice and back-up. The working pattern includes prospective cover and has been constructed to be EWTR compliant. D. TEACHING Participation in Teaching will be encouraged. The undergraduate lecture course in gynaecological oncology and pre-invasive disease occur every 8 weeks and the SST will be occasionally expected to participate in this and in bed-side and clinical teaching for students. The SST will also support and teach Specialist Trainees attached to the Department. E. ADMINISTRATION/MANAGEMENT Completion of reports and records as appropriate. Attendance at appropriate business and departmental management meetings. There will also be opportunities for active participation and management of Multi Disciplinary Team Meetings. Main Conditions of Service Appointments to this programme are subject to the Terms and Conditions of Service (TCS) for Hospital Medical and Dental Staff (England and Wales). In addition appointments are subject to: Applicants having the right to work and be a doctor or dentist in training in the UK Registration with the General Medical Council Pre-employment checks carried out by the Trust HR department, including CRB checks and occupational health clearance. The employing Trust’s offer of employment is expected to be on the following nationally agreed terms: Hours – The working hours for junior doctors in training are now 48-hours (or 52hours if working on a derogated rota) averaged over 26 weeks (six months). Doctors in training also have an individual right to opt-out if they choose to do so, but they cannot opt-out of rest break or leave requirements. However, the contracts for doctors in training make clear that overall hours must not exceed 56 hours in a week (New Deal Contract requirements) across all their employments and any locum work they do. http://www.nhsemployers.org/PlanningYourWorkforce/MedicalWorkforce/EWTD/P ages/EWTD.aspx Pay – you should be paid monthly at the rates set out in the national terms and conditions of service for hospital medical and dental staff and doctors in public health medicine and the community health service (England and Wales), “the TCS”, as amended from time to time. The payscales are reviewed annually. Current rates of pay may be viewed at http://www.nhsemployers.org/PayAndContracts/Pay%20circulars/Pages/PayCircular sMedicalandDental.aspx Pay supplement –depending upon the working pattern and hours of duty you are contracted to undertake by the employer you should be paid a monthly additional pay supplement at the rates set out in paragraph 22 of the TCS. The current payscales may be viewed at http://www.nhsemployers.org/PayAndContracts/Pay%20circulars/Pages/PayCircular sMedicalandDental.aspx . The pay supplement is not reckonable for NHS pension purposes. The pay supplement will be determined by the employer and should be made clear in their offer of employment and subject to monitoring. Pension – you will be entitled to join or continue as a member of the NHS Pension Scheme, subject to its terms and rules, which may be amended from time to time. If you leave the programme for out of programme experience you may have a gap in your pension contributions. More information can be found at http://www.nhsbsa.nhs.uk/pensions Annual Leave – your entitlement to annual leave will be five or six weeks per annum depending on your previous service/incremental point, as set out in paragraphs 205206 of the TCS. The TCS may be viewed at http://www.nhsemployers.org/PAYANDCONTRACTS/JUNIORDOCTORSDENTISTS GPREG/Pages/DoctorsInTraining-JuniorDoctorsTermsAndConditions150908.aspx Sick pay – entitlements are outlined in paragraph 225 of the TCS. Notice –you will be required to give your employer and entitled to receive from them notice in accordance with paragraphs 195-196 of the TCS. Study Leave –the employer is expected to offer study leave in accordance with paragraphs 250-254 of the TCS. Local policy and procedure will be explained at induction. Travel Expenses – the employer is expected to offer travel expenses in accordance with paragraphs 277-308 of the TCS for journeys incurred in performing your duties. Local policy and procedure should be explained at induction. Subsistence expenses – the employer is expected to offer subsistence expenses in accordance with paragraph 311 of the TCS. Local policy and procedure should be explained at induction. Relocation expenses – the employer will have a local policy for relocation expenses based on paragraphs 314 – 315 of the TCS and national guidance at http://www.nhsemployers.org/PAYANDCONTRACTS/JUNIORDOCTORSDENTISTS GPREG/Pages/DoctorsInTraining-JuniorDoctorsTermsAndConditions150908.aspx. You are advised to check eligibility and confirm any entitlement with the employer before incurring any expenditure. Pre-employment checks – all NHS employers are required to undertake preemployment checks. The employer will confirm their local arrangements, which are expected to be in line with national guidance at http://www.nhsemployers.org/RecruitmentAndRetention/Employmentchecks/Pages/Employment-checks.aspx Professional registration – it will be a requirement of employment that you have professional registration with the GMC for the duration of your employment. Though the post is covered by NHS Indemnity, you are strongly advised to register with the MPS for professional indemnity. Health and Safety – all employers have a duty to protect their workers from harm. You should be advised by the employer of local policies and procedures intended to protect your health and safety and expected to comply with these. Disciplinary and grievance procedures – the employer will have local policies and procedures for dealing with any disciplinary concerns or grievances you may have. They should advise you how to access these, not later than eight weeks after commencement of employment. Educational Supervisor – the employer or a nominated deputy (usually the Director of Medical Education) will confirm your supervisor on commencement. General information on the Deanery’s management of Specialty Training programmes, including issues such as taking time out of programme and dealing with concerns or complaints, is available at www.oxforddeanery.nhs.uk and in the national ‘Gold guide’ to Specialty Training at http://www.mmc.nhs.uk Training Rota For SST in Gynaecological Oncology: Week 1 Mon Tue Wed Thurs Fri Sat Sun Week of Nights on call Obstetrics – Mon – Friday. Week 2 Mon Tue Wed Thurs Fri Sat Sun Off Duty Week 3 Mon Tue Wed Thurs Fri Sat Sun Annual Leave Week 4 Mon Tue Wed Thurs Fri Sat Sun Clin Op Op admin Off duty*On call On Call (Nights) MDT Colp Op Op Res On call Week 5 Mon Tue Wed Thurs Fri Sat Sun off Op Op admin off duty* off Op Op Op Res Week 6 Mon Tue Wed Thurs Fri Sat Sun Clin op Colp admin of Duty* MDT op op op Res Week 7 Mon Tue Wed Thurs Fri Sat Sun Clin Op op admin Op on call-days MDT Op Res Op Op Week 8 Mon Tue Wed Thurs Fri Sat Sun Clin Op Op Res Op MDT Op Op Admin Op 40 days Mon – Friday – 5 due to a/l = 35 days Colp = 2 Clin= 4 Op=13.5 MDT = 4 Admin = 2.5 Research =2.5 *Off duty to cover any long theatre sessions = 1.5 TOTAL SESSIONS = 30 In Total 104 weeks in post – annual leave = 6 weeks /year – hence 98 weeks in 2 years. Attachment to other specialities [using weeks 4/5 in the majority- ] 2 weeks palliative care 2 weeks urology 2 weeks Gastrointestinal surgery Attendance at Gestational Trophoblastic workshop [2 days] 2 Weeks – Plastic surgery 2 weeks -Medical Oncology 2 weeks – Clinical Oncology Epidemiology/Administration will be incorporated into the programme. Histopathology/Imaging will be covered within the MDT attendance. Advanced Communication Course costs [3 days] will be covered by the ‘Women’s Cancer Fund’