Module 3
advertisement

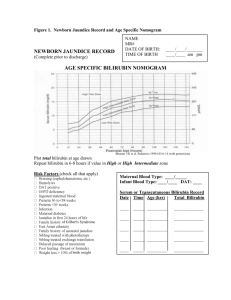
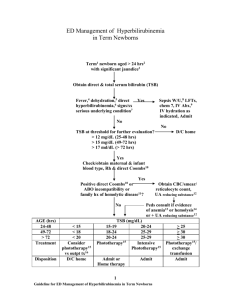
Module 3 Neonatology. Tests (Текстові тестові завдання) 1. Which of the following statements is correct? A. Gestational age of 35 weeks + 5 days should be considered as 36 weeks B. Preterm is defined as a gestation of less than 35 weeks C. Small-for-date babies are more than 42 weeks’ gestation D. Postmature infants are more than 42 weeks’ gestation E. Neonatal period extends up to 30 days of life ANSWER: D. 2. Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Hypothyroidism B. Sickle-cell disease C. Hemolytic disease of newborns D. Exclusive brest feeding E. All is correct ANSWER: E. 3. In the newborn child was diagnosed physiological jaundice and erythema toxicum neonatorum. What treatment should be performed? A. phototherapy and antibiotics B. antibiotics and sorbents C. antibiotics and local anilin dye D. sorbents and infusions E. no need treatment ANSWER: E. 4. In the newborn child was diagnosed transitory dysbacteriosis and physiological jaundice. What treatment should be performed? A. phototherapy and antibiotics B. antibiotics and sorbents C. antibiotics and local anilin dye D. probiotics and infusions E. no need treatment ANSWER: E. 5. For conjugative jaundice is typical the presence of: A. Cytolysis syndrome B. Hepatolienal syndrome C. Direct hyperbilirubinemia D. Hemolytic anemia E. Indirect hyperbilirubinemia ANSWER: E. 6. What changes in the complete blood test are typical for hemolytic disease of the newborn? A. Leucocytosis, anemia B. Thrombocytopenia, neutrophyllosis C. Anemia, reticulocytosis D. Leucocytosis, shift of the formula to the left E. Erythropenia, leucopenia ANSWER: C. 7. A child was born in term with signs of asphyxia. The estimation for Apgar scale on the first minute is 6 points. What is the first step of resuscitation in this case? A. clearing the airways B. warming of the child C. oxygen therapy D. injection of adrenaline E. tactile stimulation ANSWER: A. 8. The child was born with signs of meconial aspiration. What is the first step of resuscitation in this case? A. lower the head downwards, tactile stimulation B. suction of the contents from upper respiratory ways C. intubation of trachea, sanation of airways D. suction of the contents from upper respiratory ways, oxygen therapy E. oxygen therapy, lavage of the tracheobronchial tree ANSWER: C. 9. The child was born with signs of severe asphyxia. Were performed resuscitation actions by ABC- resuscitation. What is the 3rd step of resuscitation? A. tactile stimulation B. suction of the contents from upper respiratory ways C. ventilation support D. oxygen therapy E. indirect heart massage ANSWER: E. 10. The decreased incidence of enteric infections noted in breastfed infants compared with formula-fed infants is MOST likely due to the A. more alkaline stool pH in breastfed infants B. nutritional benefits of human milk on the infant's immune system C. predominance of Bacteroides and Clostridium in the gut of breastfed infants D. presence of protective antibodies against enteric infection in human milk E. sterility of human milk ANSWER: D. 11. Early hospital discharge is defined as the discharge of a newborn earlier than 48 hours following vaginal delivery or 96 hours following cesarean delivery. Of the following, the MOST common reason for readmission to the hospital within 7 days following an early discharge is: A. bacterial sepsis B. congenital heart disease C. gastrointestinal malformation D. hyperbilirubinemia E. metabolic disorders ANSWER: D. 12. Choose the most correct statement for the first grade hypoxic-ischemic encephalopathy: A. newborn has hyperirritability, hyperreflexia, seazures B. newborn has hyporeflexia, muscle atonia, changes on EEG are absent C. newborn has hyperirritability, hyperreflexia, tremor, changes on EEG are absent D. newborn has hyporeflexia, muscle atonia, changes on EEG are present E. newborn is in sopor or in coma ANSWER: C. 13. Choose the most correct statement for the third grade hypoxic-ischemic encephalopathy: A. newborn has hyperirritability, hyperreflexia, seazures B. newborn has hyporeflexia, muscle atonia, changes on EEG are absent C. newborn has hyperirritability, hyperreflexia, seazures, changes on EEG are absent D. newborn has hyporeflexia, muscle atonia, changes on EEG are present E. newborn is in sopor or in coma ANSWER: E. 14. Choose the definition of the intranatal period: A. begins from the first signs of the delivery, extends until the birth of the baby B. begins from the zygote formation, lasts up to the 8-th week of gestation C. begins from the 8-th week of gestation, continue up to the end of pregnancy D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth ANSWER: A. 15. Choose the definition of the perinatal period: A. begins from the first signs of the delivery, extends until the birth of the baby B. begins from the zygote formation, lasts up to the 8-th week of gestation C. begins from the 8-th week of gestation, continue up to the end of pregnancy D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth ANSWER: D. 16. Choose the definition of the early neonatal period: A. begins from the first signs of the delivery, extends until the birth of the baby B. begins from the zygote formation, lasts up to the 8-th week of gestation C. begins from the 8-th week of gestation, continue up to the end of pregnancy D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth ANSWER: E. 17. Choose the definition of the neonatal period: A. begins from the birth of the baby, extends until 28 days after birth B. begins from the birth of the baby, extends until 60 days after birth C. begins from 28 weeks of gestation, lasts until the 40 weeks of gestation D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth ANSWER: A. 18. Choose the definition of the late neonatal period: A. begins from the 14-th day of life, lasts until 28 days after birth B. begins from the 7-th day of life, lasts until 28 days after birth C. begins from the birth of the baby, extends until 28 days after birth D. begins from the birth of the baby, extends until 60 days after birth E. begins from the birth of the baby, lasts until 14 days after birth ANSWER: B. 19. Neonatal period consists from the next periods: A. embrional development and placental development B. late antenatal, intranatal and early neonatal C. embrional and perinatal D. early neonatal and late neonatal E. perinatal and early neonatal ANSWER: D. 20. Select the INCORRECT criterion concerning Apgar scale: A. heart rate B. reflex irritability C. skin color D. body temperature E. muscle tone ANSWER: D. 21. When umbilical cord should become dry and should naturally fall off in healthy newborn? A. during 1-2 days of life B. between 5-7-th days of life C. immediately after birth D. between 10-12 days of life E. till the end of the second week of life ANSWER: B. 22. When is recommended to perform first breast feeding for the healthy newborn? A. in delivery room immediately after birth B. during first 5 hours of life C. within 2 hours of life D. at the second day of life E. first feeding should be performed with adapted milk formula ANSWER: A. 23. Choose the INCORRECT reason of the neonatal transient states? A. the environment becomes totally different B. change of barometric pressure C. unstable temperature of surroundings D. fetal hypoxia E. microbic environment ANSWER: D. 24. Choose the CORRECT reason of the neonatal transient states? A. intrauterine infection B. pathological delivery C. unstable temperature of surroundings D. fetal hypoxia E. intrauterine growth restriction ANSWER: C. 25. For transient weight loss is typical: A. loss of up to 5 % of birth weight which may occur during the first 3 to 5 days B. loss of up to 15 % of birth weight which may occur during the first 3 to 5 days C. loss of up to 10 % of birth weight which may occur during the first 7 to 10 days D. loss of up to 15 % of birth weight which may occur during the first 7 to 10 days E. loss of up to 10 % of birth weight which may occur during the first 3 to 5 days ANSWER: E. 26. For transient weight loss is typical: A. loss of up to 3 % of birth weight B. loss of up to 5 % of birth weight C. loss of up to 10 % of birth weight D. loss of up to 15 % of birth weight E. loss of up to 20 % of birth weight ANSWER: C. 27. What is erythema toxicum neonatorum? A. local skin infection B. transient allergic reaction to the environment C. type of allergic dermatitis D. first stage of flegmona in newborns E. rare complication of neonatal sepsis ANSWER: B. 28. Choose the INCORRECT reason of physiological jaundice: A. functional immaturity of liver enzymes system B. destroy of hemoglobin F C. transient hypoproteinemia D. ABO incompatibility E. increased enterohepatic circulation of bilirubin ANSWER: D. 29. Choose the CORRECT reason of physiological jaundice: A. increased activity of liver enzymes system in newborns B. intensive excretion of bilirubin C. Rh - incompatibility D. ABO - incompatibility E. increased enterohepatic circulation of bilirubin ANSWER: E. 30. What is pathogenetic type of physiological jaundice? A. mechanical B. parenchymatous C. hemolytic D. conjugated E. Toxic ANSWER: D. 31. What is name of the transient stool of the newborn? A. melena B. meconium C. hematemesis D. lanugo E. “rice water” stool ANSWER: B. 32. When does appear meconium in healthy newborns? A. during the first few minutes after birth B. during the first few days after birth C. during the first few weeks after birth D. in the case of infection E. it doesn’t appear in healthy newborns ANSWER: B. 33. What should be treatment of physiological jaundice? A. phototherapy B. glucose infusions C. sorbents D. exchange blood transfusion E. *treatment isn’t necessary ANSWER: E. 34. Erb’s palsy is a result of: A. C5-C6 injury B. C6-C7 injury C. C7-C8 injury D. C8-T1 injury E. C5-T1 injury ANSWER: A. 35. Klumpke’s paralyses is a result of: A. C5-C6 injury B. C6-C7 injury C. C7-C8 injury D. C8-T1 injury E. C5-T1 injury ANSWER: C. 36. Kerer’s paralyses is a result of: A. C5-C6 injury B. C6-C7 injury C. C7-C8 injury D. C8-T1 injury E. C5-T1 injury ANSWER: E. 37. What is the possible indication for the lumbar puncture in newborns? A. Convulsive syndrome B. Neonatal meningitis C. Subarachnoid hemorrhage D. Hypertensive-hydrocephalic syndrome E. All is correct ANSWER: E. 38. What should be treatment of uric acid infarct in newborns? A. antibiotics B. glucose infusions C. sorbents D. diuretics E. treatment isn’t necessary ANSWER: E. 39. What should be treatment of hormonal crisis in newborns? A. estrogens B. C. D. E. androgens sorbents infusions treatment isn’t necessary ANSWER: E. 40. Choose CORRECT statement about early jaundice of newborn: A. It’s always pathological B. It appears within first 48 hours of life C. It always disappears till 14 days of life D. TSB level doesn’t exceed 200 mkmol/L E. Sometimes it can occur in healthy newborn ANSWER: A. 41. Choose CORRECT statement about physiological jaundice of newborn: A. It appears within first 48 hours of life B. It appears after 36 hours of life and lasts till 14 days C. It always disappears within 7 days of life D. There is direct hyperbilirubinemia E. It is typical triad: jaundice, anemia, hepatospleenomegaly ANSWER: B. 42. Choose CORRECT statement about physiological jaundice of newborn: A. It appears within first 48 hours of life B. It appears after 24 hours of life and lasts till 14 days C. It always disappears within 7 days of life D. There is indirect hyperbilirubinemia E. It is typical triad: jaundice, anemia, hepatospleenomegaly ANSWER: D. 43. Choose CORRECT statement about physiological jaundice of newborn: A. It appears within first 48 hours of life B. Level of TSB usually doesn’t exceed 250 mkmol/L C. It always disappears within 7 days of life D. There is acholic stool E. It should appear on the third day of life ANSWER: B. 44. What does mean prolonged jaundice of term newborn? A. Lasts longer than 7 days B. Lasts longer than 14 days C. Lasts longer than 21 days D. Lasts longer than 1 month E. All is correct ANSWER: B. 45. What does mean prolonged jaundice of preterm newborn? A. Lasts longer than 7 days B. Lasts longer than 14 days C. Lasts longer than 21 days D. Lasts longer than 1 month E. All is correct ANSWER: C. 46. What can be the reason of prolonged jaundice of newborns? A. Hypothyroidism B. Intrauterine infection C. Brest milk intake D. All is correct E. All is incorrect ANSWER: D. 47. What can be the reason of early jaundice of newborns? A. Hypothyroidism B. Sepsis C. Brest milk intake D. All is correct E. All is incorrect ANSWER: B. 48. What is significant for the hemolytic jaundice? A. Anemia, reticulocytosis, hepatospleenomegaly B. Direct hyperbilirubinemia, acholic stool C. Direct hyperbilirubinemia, colored stool, dark urine D. Indirect hyperbilirubinemia, absence of anemia, normal liver size E. Indirect hyperbilirubinemia, anemia, normal liver size ANSWER: A. 49. What is significant for the conjugated jaundice? A. Anemia, reticulocytosis, hepatospleenomegaly B. Direct hyperbilirubinemia, acholic stool C. Direct hyperbilirubinemia, colored stool, dark urine D. Indirect hyperbilirubinemia, absence of anemia, normal liver size E. Indirect hyperbilirubinemia, anemia, normal liver size ANSWER: D. 50. What is significant for the mechanical jaundice? A. Anemia, reticulocytosis, hepatospleenomegaly B. Direct hyperbilirubinemia, acholic stool C. Direct hyperbilirubinemia, colored stool, dark urine D. Indirect hyperbilirubinemia, absence of anemia, normal liver size E. Indirect hyperbilirubinemia, anemia, normal liver size ANSWER: B. 51. What is significant for the parenchymatous jaundice? A. Anemia, reticulocytosis, hepatospleenomegaly B. Direct hyperbilirubinemia, acholic stool C. Direct hyperbilirubinemia, colored stool, dark urine D. Indirect hyperbilirubinemia, absence of anemia, normal liver size E. Indirect hyperbilirubinemia, anemia, normal liver size ANSWER: C. 52. What does mean “zone 1” according Kramer’s scale? A. Face, neck B. Chest, abdomen C. Pelvis, buttocks, hips D. Arms, legs E. Hands, palms, feet ANSWER: A. 53. What does mean “zone 2” according Kramer’s scale? A. Face, neck B. Chest, abdomen C. Pelvis, buttocks, hips D. Arms, legs E. Hands, palms, feet ANSWER: B. 54. What does mean “zone 3” according Kramer’s scale? A. Face, neck B. Chest, abdomen C. Pelvis, buttocks, hips D. Arms, legs E. Hands, palms, feet ANSWER: C. 55. What does mean “zone 4” according Kramer’s scale? A. Face, neck B. Chest, abdomen C. Pelvis, buttocks, hips D. Arms, legs E. Hands, palms, feet ANSWER: D. 56. What does mean “zone 5” according Kramer’s scale? A. Face, neck B. Chest, abdomen C. Pelvis, buttocks, hips D. Arms, legs E. Hands, palms, feet ANSWER: E. 57. Absence of chin movements during breathing according to Silverman scale can be estimated as: A. O points B. 1 point C. 2 points D. 3 points E. Shouldn’t be estimated ANSWER: A. 58. Mild retraction of sternum during breathing according to Silverman scale can be estimated as: A. O points B. 1 point C. 2 points D. 3 points E. Shouldn’t be estimated ANSWER: B. 59. Surfactant deficiency is the etiological factor of: A. B. C. D. E. Neonatal pneumonia Respiratory distress syndrome Congenital lung atelectasis Acidosis Asphyxia ANSWER: B. 60. What is usually used for the feeding of newborns whose gestational age is 33-35 weeks? A. Nasogastric tube B. Bottle C. Teaspoon D. Mother’s breast E. Syringe ANSWER: A. 61. For antenatal prophylaxis of the hyaline membrane disease are used: A. antibiotics B. surfactant C. vitamins D. glucocorticoids E. prophylaxis isn’t necessary to perform ANSWER: D. 62. Which treatment of hyaline membrane disease is the most important? A. antibiotics B. surfactant C. vitamins D. glucocorticoids E. oxygen inhalation ANSWER: B. 63. For the premature newborn is typical: A. Opened posterior fontanel B. Opened anterior fontanel C. Skin peeling D. Presence of jaundice E. All is correct ANSWER: E. 64. What is the etiology of hyaline membrane disease? A. Bacterial B. Viral C. Hereditary D. Surfactant deficiency E. All is correct ANSWER: D. 65. Of the following, erythromycin prophylaxis is MOST likely to prevent ocular infection due to: A. Chlamydia trachomatis B. group B streptococci C. Neisseria gonorrhoeae D. Staphylococcus aureus E. Trichomonas vaginalis ANSWER: C. 66. What are the skin lesions of the herpes? A. Scales B. Papules C. Vesicles D. Pustules E. Wheals ANSWER: C. 67. What are the skin lesions of the impetigo? A. Scales B. Ulcers C. Reddish maculae D. Crusts E. Plaques ANSWER: D. 68. What are the skin lesions of the folliculitis? A. Vesicles B. Pustules C. Cysts D. Bullae E. Wheals ANSWER: B. 69. Of the following, the condition that is MOST likely to present with seizures during the first 24 hours of life is A. B. C. D. E. fetal alcohol syndrome herpes simplex infection hypoxic-ischemic encephalopathy organic acidemia urea cycle defect ANSWER: C. 70. What is the medicine of the choice for congenital CMV-infection treatment ? A. Sumamed B. Chloridin C. Acyclovir D. Ampicillin E. Ganciclovir ANSWER: E. 71. Approximately 30%-50% of infants born from Chlamydia-positive mothers will have A. Conjunctivitis B. Dermatitis C. Jaundice D. Pneumoniae E. Pyelonephritis ANSWER: A. 72. What ocular lesion is typical for neonatal toxoplasmosis: A. Chorioretinitis B. C. D. E. Anterior uveitis Keratoconjunctivitis Cataract Optic neuritis ANSWER: A. 73. Hydrocephalus is the most typical for: A. Rubella B. CMV C. Toxoplasmosis D. Lysteriosis E. Syphilis ANSWER: C. 74. Choose the clinical feature of TORCH-syndrome: A. Low birthweight B. Jaundice C. Hepatosplenomegaly D. Seizures E. All is correct ANSWER: E. 75. Toxoplasma gondii belongs to: A. Viruses B. Bacteria C. Fungi D. Parasites E. All is incorrect ANSWER: D. 76. Cat is the definitive host in the contamination mechanism of: A. Staphylococcal infection B. Candidosis C. Lysteriosis D. Toxoplasmosis E. Syphilis ANSWER: D. 77. Raw meat can be the source of contamination with: A. Staphylococcal infection B. Candidosis C. Lysteriosis D. Toxoplasmosis E. Syphilis ANSWER: D. 78. What bacteria can be revealed in darkfield microscopy? A. Trypanosoma cruzi B. Toxoplasma gondii C. Treponema pallidum D. Listeria monocytogenes E. Cytomegalovirus ANSWER: C. 79. What is the medicine of choice for the congenital toxoplasmosis treatment in newborns? A. Spiramycin B. Pyrimethamine C. Penicillin D. Metronidazol E. Ceftriaxon ANSWER: B. 80. What medicine should be used for the congenital syphilis treatment in newborns? A. Pyrimethamine B. Penicillin G C. Ampicillin D. Ceftriaxon E. Acyclovir ANSWER: B. 81. What is the most dangerous period for rubella contacts for pregnant women? A. The first trimester of pregnancy B. The second trimester of pregnancy C. The third trimester of pregnancy D. The last several days before delivery E. Any period of pregnancy ANSWER: A. 82. Cardiac defects development in fetus is the most typical for: A. Congenital toxoplasmosis B. CMV infection C. Congenital rubella D. Herpes E. Congenital syphilis ANSWER: C. 83. Cataracts development in fetus is the most typical for: A. Congenital toxoplasmosis B. Congenital rubella C. CMV infection D. Herpes E. Congenital syphilis ANSWER: B. 84. The classic triad for congenital rubella syndrome is: A. Rush, CNS abnormalities (seizures), eye abnormalities (cataract, microphtalmia) B. Congenital heart defects, jaundice, sensorineural hearing loss C. Eye abnormalities (cataract, microphtalmia), microcefalus, rush D. Eye abnormalities (cataract, microphtalmia), congenital heart defects, sensorineural hearing loss E. Congenital heart defects, sensorineural hearing loss, CNS abnormalities (seizures) ANSWER: D. 85. What is the etiological treatment of congenital cytomegalovirus infection? A. Ampicillin B. Ganciclovir C. Acyclovir D. Pyrimethamine E. There is no etiological treatment ANSWER: B. 86. What medicines should be chosen for the treatment of congenital cytomegalovirus infection? A. Ampicillin and Cefatoxim B. Ampicillin and Amikacin C. Ganclovir and Cytotect D. Acyclovir and Prednison E. Pyrimethamine and Sulfadiazin ANSWER: C. 87. What is the etiological treatment of congenital HSV infection? A. Ampicillin B. Ganciclovir C. Acyclovir D. Pyrimethamine E. There is no etiological treatment ANSWER: C. 88. What infection is NOT included into TORCH-syndrome? A. Syphilis B. Hepatitis B C. Toxoplasmosis D. Tuberculosis E. HIV-infection ANSWER: D. 89. What symptom is the most typical for congenital clamidiosis? A. Jaundice B. Hydrocefalus C. Seizures D. Purulent conjunctivitis E. Maculopapular rash ANSWER: D. 90. What symptom is the most typical for congenital syphilis? A. Cataract B. Meningitis C. Purulent conjunctivitis D. Rinitis E. Hydrocefalus ANSWER: D. 91. Of the following, erythromycin prophylaxis is MOST likely to prevent ocular infection due to: A. Chlamydia trachomatis B. group B streptococci C. Neisseria gonorrhoeae D. Staphylococcus aureus E. Trichomonas vaginalis ANSWER: C. 92. Which of the following statements is NOT true in physiological jaundice? A. It always appears later than 24 hours B. It is due mainly to temporary impaired hepatic clearance of bilirubin C. In premature newborns it may persist for 3-4 weeks D. Direct bilirubin level may be as high as indirect bilirubin level E. It can not be the reason of kernicterus ANSWER: D. 93. Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Fetal hepatitis B. Beta-thalassemia major C. Biliary atresia D. Congenital syphilis E. Hemolytic disease of newborn ANSWER: E. 94. The most frequent reason of neonatal phlegmona development is: A. Infection B. Overcooling C. Compression D. congenital immunodeficiency E. All is correct ANSWER: A. 95. The typical symptom of the neonatal phlegmona is: A. Soft tissues infiltration B. Intoxication syndrome C. Deep scars on the skin D. "Creeping infiltration" E. All is correct ANSWER: E. 96. The typical symptom of the SSS-syndrome is: A. Skin infiltration B. Palms hyperkeratosis C. Deep scars on the skin D. Bullae with bloody content E. Positive Nikolsky’s sign ANSWER: E. 97. For the Ritter’s dermatitis are typical: A. Tonic seizures B. Feet hyperkeratosis C. Hydrocephalus D. Ektropion E. Erosive skin changes ANSWER: E. 98. The most frequent etiological factor of the Ritter’s dermatitis is: A. Chlamydia trachomatis B. Group B streptococci C. Neisseria gonorrhoeae D. Staphylococcus aureus E. Trichomonas vaginalis ANSWER: D. 99. The acholic stool in neonate is typical for the: A. Physiological jaundice B. Haemolytic jaundice C. Mechanical jaundice D. Parenchymatous jaundice E. All is incorrect ANSWER: C. 100. A. B. C. D. E. ANSWER: C. The acholic stool in neonate is one of the typical symptoms for the: Physiological jaundice Haemolytic disease of newborns Bile ducts atresia Fetal hepatitis All is correct