Mary is 44 years old and is complaining of terrible headaches
advertisement

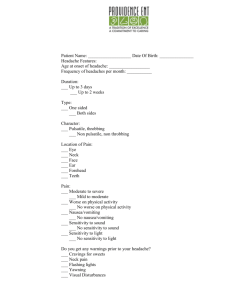
Tension Type Headaches Case Presenation Mary is 44 years old and is complaining of terrible headaches. Ok Mary tell me more about your headaches. Well I get terrible headaches. Nearly every day I seem to get a headache and nothing I do helps them. I am so used to them that I can continue working but it just makes life miserable. I have always been prone to headaches but the last few years they have gotten worse. Can you describe the pain to me? Well it starts at the back of my neck and then moves to both sides at the front of my head. It feels like someone is tightening a band around my head. Also the light sometimes hurts my eyes. Has the type of headache you get changed at all over the last couple of years and how often does it occur? No it’s the same headache I just get it more often. I used to get one or two a month but now I get about 6 a week. Do you get any nausea or vomiting with the headache? No. Tell me about your job and who is at home with you, particularly if you have any major stresses in your life. I work in a small grocery store part time, I’m divorced and my two sons are grown up now so I live alone. I have been on disability since I hurt my back 5 years ago but these headaches I get are far worse than my back pain. Do you feel depressed or anxious at all? Well sometimes I do feel anxious especially about money, which is a constant worry for me. But I don’t think I’m depressed. What do you take for your headaches? I usually take Motrin but now find that it does not help at all in fact I am getting more and more headaches. Sometimes I take eight a day trying to get rid of the pain. April 2005 p. 1 Headache for Educators Project Diagnosis Mary has tension type headaches that are bilateral mild to moderate headaches that she describes as a tight feeling around her head. She is able to continue her usual daily activities with the headaches and has no associated symptoms of nausea, vomiting, or phonophobia although she does have some photophonia. (Table 1). She has chronic tension headaches as they occur more than 15 days a month. Tension headaches that occur less than 15 days a month are called episodic tension type headaches. She may also be getting medication overuse or rebound headaches that are associated with frequent use of any analgesic medication and will not improve until the medication is stopped. She should be screened for depression and anxiety as psychiatric co-morbidity is common in patients with tension type headaches (15) Treatment of episodic tension type headache 1. Simple analgesics, e.g. acetaminophen and ibuprofen, are both more effective than placebo at relieving the pain from tension type headaches. Ibuprofen is more effective than acetaminophen. (17). Level A. 2. Analgesics can be combined with a sedating antihistamine such as promethazine or diphenhydramine.. Level C. 3. Limit treatment to 2 days a week to prevent rebound headaches. Prevention of chronic tension type headache To prevent the onset of medication overuse headache it is preferable to use preventive treatment for chronic tension type headaches. 1. Antidepressants: the tricyclic antidepressants amitriptyline, imipramine and nortriptyline have been shown to prevent chronic daily headaches (CDH) .(1, 11). Start at 10 mg at bedtime and gradually titrate it up. (Level A.) The efficacy of amitriptyline and nortriptyline is higher when combined with stress management.(1). 2. Stress management eg relaxation and cognitive coping. This is more effective when combined with antidepressant medication(1). Muscle relaxation techniques with or without biofeedback training can be used to teach the patient awareness of and control of their physiologic responses. In one study adding biofeedback to relaxation training increased the proportion of patients with a decrease in their headaches from 39% to 54%.(20). 3. Tizanidine has been shown to reduce the frequency and intensity of chronic daily headaches. (14) 4. SSRIs. There is not much research looking at the effectiveness of SSRIs but they may be helpful particularly in patients with co-morbid depression. Prozac has been shown to increase headache free days and decrease headache intensity. (10) April 2005 p. 2 Headache for Educators Project 5. Botulinium toxin has been shown to prevent migraines and there is some evidence it may be effective in the prevention of CDH. (2, 3) 6. Anticonvulsants. Both gabapentin and topiramate have been shown to decrease headache frequency in small studies.(12, 13) 7. Combination therapy with an antidepressant and an anticonvulsant. 8. Acupuncture has been shown to decrease the severity and frequency of headaches although many of he RCTS were of poor quality. (19, 22).(Level B) Medication Overuse Headache (MOH) or Rebound Headaches Medication overuse headaches can occur when a patient has been taking headache medication usually daily but may be as infrequently as four times a week. The medication may alleviate the headache but as it wears off the headache recurs. Patients with episodic tension type headaches are at risk of developing MOH due to medication overuse. The most common cause of a mix of migraine and tension type headaches occurring on more than 15 days a month is MOH. These patients may have headaches that gradually shift from a migraine type headache to a tension type headache even within a day as the analgesia wears off and the rebound headache develops. The diagnosis of medication overuse headache is important to make as patients rarely respond to prophylactic medication whilst they are overusing acute headache medications. The pathophysiology of MOH is poorly understood but the fact that sometimes the headache does not resolve with the cessation of the medication suggests that there may be permanent changes in the CNS resulting from medication overuse for prolonged periods. The mean duration for the onset of MOH is shortest for triptans (1.7 years) and longest for analgesics (4.7 years). The average monthly dosing associated with onset of MOH is lowest for triptans (18 doses a month) and highest for analgesics (37 doses a month). (4). The drugs most likely to cause MOH are the combination analgesic and caffeine containing medication probably due to their availability over the counter and relatively low cost. Management of MOH. The key to the resolution of MOH headaches is the cessation of the medication. Ideally the medication is abruptly stopped although if the patient is unable to tolerate this due to withdrawal symptoms the dose will have to be titrated down over a twoweek period. In patients using particularly high doses of analgesic medication a day (over 12 tablets) it is preferable to gradually decrease the medication because of serious withdrawal symptoms. (23). Different medications have been used whilst titrating down the medication that is being withdrawn. (Table 3). Non pharmacological methods such as biofeedback may help reduce the withdrawal symptoms. The success rate for treating MOH varies from 50-90%. There is a need April 2005 p. 3 Headache for Educators Project for both physicians and patients to be aware of the risks of MOH and reduce the amount of acute headache medication used and increase the amount of prophylactic medication used. Level A evidence: From multiple well designed RCTS, meta-analyses and systematic reviews. Level B evidence: Scientific support is weaker for example poorly done RCTS,well designed non randomized trials, case control studies, or inconsistent RCTS. Level C: evidence from consensus viewpoint or expert opinion IHS Criteria for Analgesic Overuse Headache. (MOH) 1. Headache for 15 days a month fulfilling at least one of the following characteristics and criteria 3 and 4. a. Bilateral b. Pressing/tightening non pulsating in quality c. Mild/moderate intensity. 2. Intake of simple analgesics for>15 days a month for 3 months 3. Headache has developed or worsened during analgesic overuse 4. Headache resolves or reverts to its previous pattern of analgesic overuse within 2 months after discontinuation of analgesic. Table 3. Expert opinion rather than evidence suggests that analgesia needs to be used over 15 days a month to induce MOH. April 2005 p. 4 Headache for Educators Project IHS Criteria for Tension Headache Medications used in the Treatment of Medication Overuse Headache 1. Parenteral DHE 2. Oral steroids. Level B. 3. Tizanidine. Level B. 4. Triptans. A. Headache lasts from 30 mins to 7 days. B. Headache has at least 2 of the following characteristics. a. Bilateral b. Pressing/tightening non pulsating quality c. Mild/moderate intensity. d. Not aggravated by routine physical activity. 5,6,8,9,18, 21 C. Both of the following: a. No nausea or vomiting b. No more than one of photophobia or phonophobia. D. Not attributed to another disorder. References 1. 2. 3. 4. 5. April 2005 The International classification of Headache Disorders. Second edition. Cephalgia.2004;Vol 24.suppl 1. Clinical policy: Critical issues in the evaluation and management of patients presenting to the emergency department with acute headache. Annals of Emerg Med. 2002 ;39 (1): 108-22. Puca F, Genco S, Prudenzano MP, Savarese M, Bussone G, D’Amico D. Psychiatric co-morbidity and psychosocial stress in patients with tension type headache from headache centers in Italy. The Italian collaborative group for the study of psychopathological factors in primary headaches. Cephalagia 1999;19:159-64. Schactel BP, Furey SA, Thoden WR. Non prescription ibuprofen and acetaminophen in the treatment of tension type headache. J Clin Pharmacol 1996;36:1120-5. Holroyd KA, O’Donnell FJ, Stensland M, Lipchik GL, Cordingley, G, Carlson B. Management of chronic tension-type headache with tricyclic p. 5 Headache for Educators Project 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. April 2005 antidepressants medication, stress management, and their combination: a randomized controlled trial. JAMA 2001;285:2208-2215. Lance JW, Curran DA. Treatment of chronic tension headache. Lancet.1964; 1236-1239. Blanchard EB, Appelbaum KA, Guarnieri P, Morrill B, Dentinger MP. Five year prospective follow-up on the treatment of chronic headache and/or relaxation. Headache 1987;27:580-3. Saper JR, Lake AE, Cantrell DT, Winner PK, White JR. Chronic daily headache prophylaxis with tizanidine: a double blind, placebo controlled multicenter outcome study. Headache.2002;42: 470-82 Lake AE, Saper JR. Chronic Headache. Neurology.2002;59 (5): Saper JR, Silberstien SD, Lake AE, Winters ME. Double–blind trial of fluoxetine:chronic daily headache and migraine. Headache. 1994;34:497-502. Smuts JA, Baker MK, Smuts HM, Tassen JM, Ossouw E, Barnard PW. Botulinium toxin type A as prophylactic treatment in chronic tension type headache. Cephalgia 1999;19:454. Nicolodi M, Sicuteri F. NMDA negative modulation in the therapy of chronic migraine. Cephalalgia. 1997;17:436 Storey JR, Calder CS, Potter DI. Potential role of topiramate in the treatment of intractable daily headache: a retrospective pilot study. Neurology.1999;52 (supp 2) A211 Vickers AJ, Rees RW, Zollmzn CE et al. Acupuncture for chronic headache in primary care: large pragmatic, randomized trial. BMJ 2004;328:744-47. Melchart D, Linde K, Fischer P, Berman B, White A, Vickers A, Allais G. Acupuncture for idiopathic headache. Cochrane database of systematic reviews. (2) 2004. Limmroth V, Katsarva Z, Fritsche G, Przywara S, diener H. Features of medication overuse headache following overuse of different acute headache drugs. Neurology. 2002;59:1011-1014. McLean W et al. Is there an indication for the use of barbiturate-containing analgesic agents in the treatment of pain? Guidelines for their safe use and withdrawal management. Canadian Pharmacists Association. Can J Clin Pharmacol 2000;7:191-7. Krymchantowski AV, Barbosa JS. Prednisone as initial treatment of analgesic-induced daily headache. Cephalgia 2000;20:107-13. Raskin N. Repetitive intravenous dihydroergotamine as therapy for intractable migraine. Neurology.1986;36:995-997. Bonucelli U, Nuti a, LucettiC, et al. Amitriptyline and dexamethasone combined treatment in drug induced headache. Cephalgia. 1996;16:197-200 Drucker P, Tepper S. Daily sumatriptan for detoxification from rebound headache. Headache.1998;38:687-690. Sheftell F, Rapoport A, Coddon D. Naritriptan in the prophylaxis of transformed migraine. Headache. 1999;39:506-510. p. 6 Headache for Educators Project