Prevalence of osteoarthritis in the joints of the appendicular skeleton
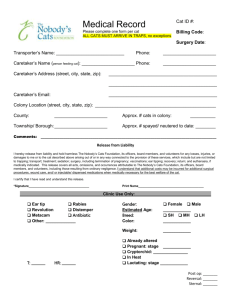
advertisement

Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat By Drs. M.Verruijt Under supervision of: dr. L.I. Slingerland and prof.dr.H.A.W. Hazewinkel Department of Clinical Sciences of Companion Animals Faculty of Veterinary Medicine, Utrecht University M.Verruijt@students.uu.nl Table of Contents pages: Part one: literature study Abstract 2 Introduction 2 General Considerations 3 Prevalence 5 Pathogenesis - the normal joint - the osteoarthritic joint 7 8 Clinical Symptoms 10 Diagnostic possibilities 10 Radiographic symptoms 13 Therapeutical options 14 Prognosis 15 Discussion 15 Conclusion 16 Part two: retrospective study of radiographs Abstract 17 Introduction 17 Materials and methods 17 Results 21 Discussion 27 Conclusion 30 Acknowledgements 30 Literature 31 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 1 Part One: Literature study Abstract Osteoarthritis in cats is not a widely recognised disease, however veterinarians are becoming increasingly aware of its existence. It is believed to be a cause of chronic pain in cats. Studies show a high prevalence in the geriatric cat. No other correlations, for example with obesity, have been demonstrated. The pathogenesis of osteoarthritis is thought to be multifactorial and is not totally understood. The main biochemical change consists of proteoglycan degradation in the joint cartilage. Only little is described with regard to the clinical symptoms in cats. Cats are thought to be able to hide their pain and symptoms. Subtile symptoms like stiffness, behavioural changes and less jumping are indicators for osteoarthritis. These symptoms are often explained by the owner as part of the cat’s process of ageing. Owners are not aware that these symptoms may arise from osteoarthritis and from the pain it causes. Therefore the veterinarian is not consulted. The veterinarian should specifically ask about these symptoms in geriatric cats and make owners aware of the possibility of osteoarthritis in the geriatric cat. Diagnosing osteoarthritis in cats is hard using only general and orthopaedic examination of cats. One of the main concerns is to rule out the possibility of inflammatory arthritis. Often a radiographic image is needed to diagnose osteoarthritis, possibly after sedation of the cat. Radiographic changes can vary, but mostly include narrowing of the joint space, subchondral bone sclerosis and osteophyte formation. Consideration of the therapeutical options and advice to the owner by veterinarians for cats with osteoarthritis should not only include pharmacological or surgical treatment, but also environmental changes. In this way treatment of osteoarthritis in cats is similar to that in other species. The goal of the treatment is to improve the cat’s quality of life through symptomatic and supportive measures. These include NSAIDs, weight reduction and for example placing the food bowls on a low access level for the cat. Osteoarthritis is a non-reversible illness, but in general an acceptable situation for the cat can be achieved with these therapeutical options. Introduction Much is known about osteoarthritis and its clinical importance in dogs. In cats osteoarthritis is a relatively new research topic, of which the clinical importance may not be fully recognised. Unlike dogs, cats do not display the symptoms of osteoarthritis in the same clinically extensive form (8). Dogs are presented at the veterinary clinic because of lameness, unlike cats. Lameness seems to be a rare phenomenon in cats with osteoarthritis. Clinical osteoarthritis in cats is described by inability or unwillingness to jump, jumping shorter distances, less playing behaviour, less grooming behaviour, stiffness and inactivity (3,8,17,34). Because of the lack of evident clinical symptoms, especially to cat owners, cat osteoarthritis might be an unrecognised disease. Several risk factors for osteoarthritis in dogs and some for cats are recognised, but particularly in cats only little is known about osteoarthritis. Risk factors like obesity, gender and breed have been evaluated in some studies, but were not proven significant (8,9,17). No definite conclusions can be made with regard to these factors without further research. For the first part of this report, evaluation of the available literature concerning osteoarthritis in the joints of the appendicular skeleton of cats has been performed and a summary of pathogenesis, risk factors, diagnostic approach, therapeutical options and frequency of osteoarthritis in cats was made. The search for literature was conducted in several different ways. The collection of the University Library of the Faculty of Veterinary Medicine in 2 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 Utrecht was searched. At first this was done by hand, by going through the orthopaedic section of the books in the library. Indexes were searched for the terms “osteoarthritis”, “degenerative joint disease”, “arthritis”, “osteoarthrosis”, “arthrosis” and “DJD”. Afterwards the library collection was searched by the use of the digital catalogue for all of the words described above (the words alone and with the addition of the word “cat” to it) (42). Later on investigation started considering the published articles about osteoarthritis, in which both digital magazines as scientific library magazines were assessed. Searching of the articles was done with assistance of several search engines, c.q. PubMed, VetPortal (including all theses and proceedings) and IVIS were mostly used (39,40,41). The abovementioned terms were also used in these search programs. Subsequently, for the second part of this report, evaluation of the prevalence of osteoarthritis in the joints of the appendicular skeleton on radiographs from the archives of the Division of Diagnostic Imaging of the University Clinic for Companion Animals in Utrecht was performed. In this retrospective study, radiographs were evaluated from cats which were presented at the Clinic. Together with this evaluation of radiographs, the history of the cats was evaluated to identify putative risk factors for osteoarthritis in cats. The evaluation of the radiographs was supervised by a Diagnostic Imaging Specialist. The objective in this research project is to investigate the prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat, as it is thought to be higher as yet recognized. General Considerations At first the definition of the word osteoarthritis is of great importance. In literature many names are given for the same disease. To make clear on which disease this report is about, a brief summary follows. For the sake of completeness table 1 describes the classification of joint diseases (6). Table 1: joint disease classification Non-inflammatory Degenerative joint disease/ osteoarthritis/ osteoarthrosis - primary - secondary Trauma Neoplasia Inflammatory Infectious disease Non infectious disease - immunologic - erosive - non-erosive - immune-mediated Often the word “osteoarthritis” is used. In literature it is defined as “a pathological change of a diarthrodial synovial articulation characterised by the deterioration of articular cartilage, osteophyte formation, bone remodelling, changes in periarticular tissue and a low-grade nonpurulent inflammation of variable degree” (5,9,11,25,30,32,34). The description of a diarthrodial joint is: “two bones, which are covered with joint cartilage and are enclosed by a joint capsule which contains synovial fluid” (28,30). Synovial joints are composed of two or more articulating bones, a joint capsule, joint cavity and articular cartilage. Joint cartilage is the main structure involved in osteoarthritis. Normally the joint cartilage provides a smooth, durable and lowfriction surface which passes on forces from one bone to another and spreads the forces evenly from one joint surface to the other. Joint cartilage consists of chondrocytes, collagen (insoluble protein macromolecules), proteoglycans (large extracellular macromolecules) and water (25,26,31,34). Arthritis is described as inflammation of the joint. With regard to this, a more correct word for the disease referred to in this report is osteoarthrosis or degenerative joint disease, because of the minimal inflammatory component of the disease in comparison to arthritis. Another definition of osteoarthritis is “a non-inflammatory degenerative articular 3 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 joint disease characterised by lack of inflammation in the synovial lining and the presence of a normal or almost normal synovial fluid”(6). In order to understand this definition, it should be clear what “normal or almost normal synovial fluid” is. Hardie defines normal synovial fluid as straw-coloured and viscous fluid, in which the white cell count is low (< 5000 cells/mm3) and neutrophils are rarely seen (18). The viscosity of the fluid is good or slightly diminished and the mucin clot test is normal. In inflammatory arthritis the synovial fluid appears to be yellow to red and the white cell count is high (> 5000 cells/mm3). Neutrophils dominate in the fluid and viscosity is diminished. The mucin clot test is fair to poor. Normal synovial fluid is very viscous because of its high concentration of hyalunoric acid (15,18). Finally osteoarthritis can be seen as a disorder of movable joints characterised by degeneration of articular cartilage and the production of new bone at articular margins (24,28). In this report the name osteoarthritis will be used, referring to the non-inflammatory disease as described above, because it is the most commonly used name in literature. As described in table 1 osteoarthritis can be classified into primary osteoarthritis and secondary osteoarthritis. Primary osteoarthritis, often called idiopathic, is degeneration of cartilage by wear and tear and proceeds with age. Secondary osteoarthritis arises from diseases, which affect joints and supportive tissues (6,25,27,28,34). In humans, secondary osteoarthritis can be divided into 4 main categories: 1. articular diseases (like rheumatoid arthritis and septic arthritis) 2. metabolic diseases (like Wilson disease and ochronosis) 3. endocrine diseases (like Diabetes mellitus) 4. structural deformities (like fractures, dysplasia and Calvé-Legg Perthes disease) (11,28,29) Another way of classifying primary and secondary osteoarthritis is that in primary osteoarthritis there is no apparent reason for the condition other than increasing age. Conversely secondary osteoarthritis occurs as a result of abnormal stresses on a joint and any condition that interferes with normal joint function can cause this (35). In feline veterinary literature the following classification for osteoarthritis, as displayed in table 2, is used: Table 2: osteoarthritis classification in cats Primary osteoarthritis Scottish Fold Osteochondrodysplasia Mucopolysaccharidosis Age-related cartilage degeneration Secondary osteoarthritis Congenital - Hip dysplasia Trauma - Traumatic joint instability - Fractures Infectious and inflammatory - Viral (calicivirus, coronavirus) - Bacterial (mycoplasma, bite wounds) - Fungal (cryptococcis, histoplasmosis) Nutritional - Hypervitaminosis A Neuropathic Immune-mediated - Rheumatoid arthritis - Progressive Proliferative Polyarthropathy - Systemic Lupus Erythromatosus - Idiopathic Polyarthritides (1,12,25,35) - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 4 Osteoarthritis can also be divided into grades of severeness by the following classification in humans (11) : I. destruction of superficial cartilage on areas of highest pressure and movement. No hyperplasia is present on the margins of cartilage or bone. Joint capsule, synovial membrane and articular margins are normal. II. More extensive destruction of cartilage, but still restrained on areas of highest pressure and movement. No bone is exposed. Early margin hyperplasia (ridge formation) along the edges of the surfaces. No osteophytes or bone remodelling are present. III. Total loss of cartilage on one or more pressure points with exposure of bone and often sclerosis. Distinct osteophytes on the margins of the joint. Change in contour of the joint surfaces. Fibrosing of the capsule. IV. Total loss of cartilage on large areas of the joint surface. Subchondral sclerosis. Irregularity of the joint surface, osteophytes, remodelling, fibrosis of the capsule and synovial membrane (11). In the following paragraphs prevalence, pathogenesis, clinical symptoms, diagnostic possibilities, radiographic symptoms, therapeutical options and prognosis of osteoarthritis in appendicular joints of the cat are described. Prevalence For dogs and humans many studies researching osteoarthritis are available. When it comes to cats, not much has been investigated yet. Some scientists believe that this is due to the fact that cats do not show lameness, but hide their discomfort caused by osteoarthritis, for instance by sleeping more and jumping less high. Because of this hiding, owners do not notice any discomfort in their cat and the cat is not presented to the veterinarian for an examination (4,17,22) . Because of these reasons, the actual prevalence of osteoarthritis is hard to investigate using clinical symptoms. Several researchers stated that the lack of attention for osteoarthritis in cats may be due to the fact that cats have a relative small body and because of their ability to accommodate orthopaedic abnormalities by redistribution of weight bearing forces to other limbs. Another given reason was that owners do not critically assess the gait of their cats and therefore do not notice abnormal gaits, mild lameness or joint stiffness (18,32). At last a possible option for the lack of interest in this disease in the cat, is that signs like stiff gait can be considered to be “normal” for the elderly cat by the owner. Many owners do not feel the need to consult their veterinarian about the stiffness of their cat or the decreased ability to jump, because owners interprete these as normal aged-related changes to which no treatment is necessary. The veterinarian may need to pay special attention to these changes (7). Some investigators looked at the prevalence of osteoarthritis in cats. Not all of them separated spondylosis from appendicular joint osteoarthritis. These terms are different, as osteoarthritis refers to a process concerning a joint with synovial fluid. Spondylosis on the other hand refers to a process that includes an articulation without synovial fluid but does involve an intervertebral disc. By not separating osteoarthritis from spondylosis the total prevalence of osteoarthritis can be different from the real prevalence. Not in all articles exact prevalence is given per joint, but only total prevalence is calculated. An overview of the most useful reports for osteoarthritis is given in table 3. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 5 Table 3: an overview of relevant research Research Criteria for selection Clarke et al (9) - Godfrey - (12) - Hardie (17) - - Clarke and Bennet (8) - - - Kamishina (21) - Assessed joints in cats (n) retrospective 218 cats with visible research joints on non-orthopaedic radiographs of presentation at clinic which: cats > 8 years - 147 shoulders complete medical - 189 elbows record - 26 carpi - 113 hips - 97 stifles - 33 hocks - 46 spines retrospective 292 cats with visible research joints on any sort of radiographs of presentation at the which: unknown clinic frequencies of cats > 1 year shoulders, elbows, complete medical carpi, hips, stifles record and tarsi. Osteoarthritis (n) in 78 cats, but spondylosis deformans was also included in this number. Without: 48 cats had osteoarthritis. Osteoarthritis (% ) 33.9 %, but without spondylosis deformans 22.0%. in 64 cats. 22 .0%. retrospective research cats > 12 years all presentations at the clinic, except polyarthritis complete medical record 100 cats with visible joints on radiographs of which: - 93 shoulders - 71 elbows - 18 hips - 13 stifles - 100 spines In 90 cats, but spondylosis deformans was also included in this number. Without: 64 cats had osteoarthritis. 90.0%, but without spondylosis deformans 64.0%. prospective research cats with clinical signs of osteoarthritis possibility of NSAID administration joints were radiographed under anaesthesia post mortem study mature cats no present trauma 28 cats with visible joints on radiographs In 28 cats, which included - 3 shoulders - 33 elbows - 0 carpi - 27 hips - 4 stifles - 5 hocks 45.0 % for the elbows and 38.0% for the hips. In 156 cats, 312 hip joints were visible on radiographs In 22 cats, in 14.1 %, of which which 11 cats also 7.1 % also had had hip dysplasia hip dysplasia - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 6 One of the researchers, Clarke et al, retrospectively looked at a population of 218 cats, selected by going through the archives of the veterinary hospital of Glasgow between July 1998 and October 2003 (9). In this population 33.9 % of cats was diagnosed with osteoarthritis (78 cats) in at least one joint on the basis of radiographs. These cats were presented at the university clinic for non-orthopaedic reasons. A note has to be made about this research, because this prevalence also included spondylosis deformans. Without spondylosis deformans a total percentage of osteoarthritis can be calculated as 22.0% (9). Godfrey performed a similar study, in which 22.0% of the cats retrospectively had signs of osteoarthritis (12). No data is present about the amount of shoulders, elbows, carpi, hips, stifles and tarsi that have been evaluated. Therefore no conclusions can be made about the prevalence in these joints, but only about the total prevalence (12). Hardie et al retrospectively examined a population of 100 geriatric cats above 12 years old, in which 90.0 % revealed radiological signs of osteoarthritis (17). A note has to be made about this research, because this percentage of osteoarthritis also included spondylosis deformans. Without spondylosis deformans a total percentage of osteoarthritis can be calculated as 64.0%. Also no data is present in the article about the prevalence of osteoarthritis in the graded joints. Therefore no conclusions can be made about the prevalence in these joints, but only about the total prevalence (17). Clarke and Bennet investigated a population of 28 cats with clinical osteoarthritis (8). The study was prospective, to look at the signs and the responses to NSAIDs in these cats. In this research 45.0% osteoarthritis in the elbows and 38.0 % osteoarthritis in the hips was mentioned (8). Kamishina examined 156 mature cats, of unknown age, which were collected from animal shelters after euthanasia (21). Only the hips were assessed in this study. The prevalence of osteoarthritis in the hip joints of these cats was 14.1 % (21). All these studies concluded that osteoarthritis may be an underrecognized problem in elderly cats. Mostly affected were the elbows, shoulders, stifles and hips (4,7,9,12,17,20,36). More research is needed to establish the prevalence of osteoarthritis in the appendicular skeleton of the cat. Thus, the exact prevalence of osteoarthritis in the appendicular skeleton of the cat is not known yet. Pathogenesis The aetiology of osteoarthritis is believed to be multifactorial and is incompletely understood (5,14,24,27,32) . The main structure involved is joint cartilage. The function of normal articular cartilage is to provide a smooth, low-friction joint surface and to pass on and evenly spread the forces from one bone to another (30). The main biochemical change in osteoarthritis occurs in the joint cartilage. In order to understand the changes in osteoarthritis, knowledge of the normal joint is needed. The normal joint Cartilage is a non-innervated avascular tissue, which consists of chondrocytes imbedded in an acellular matrix which exists of proteoglycans, collagen and water. Articular cartilage can histologically be divided in several layers, as is displayed in figure 1 (31). The most superficial layer lies farthest from the subchondral bone and is named the tangential or gliding zone. Cells are flattened and elongated in this layer and are arranged parallel to the joint surface. The second layer is the large transitional zone, which contains more rounded cells which are more randomly arranged. Third layer is the radial zone, which has cells in columns. Last layer is the calcified zone, where the cells are arranged in columns in a calcified matrix. The calcified layer is supported by the subchondral bone plate and joins the subchondral bone at the osteochondral junction (5,30,31). 7 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 Figure 1: an overview of joint anatomy A figure taken from (31) The joint capsule is composed of an outer and inner layer. The outer layer is mainly fibrous and, together with the surrounding connective tissue, its function is to support the joint. The inner layer is the synovium and contains blood vessels and nerves. It is important for maintenance of the synovial fluid volume. Synovial fluid has a lubrification and transport function in normal joints (5,30,31). Normal articular cartilage is arranged as a stiff, gel-like substance, which consists of a loose collagen network with chondrocytes and proteoglycan-hyaluronate aggregates. The proteoglycan-hyaluronate aggregates have a high molecular weight and a high charge, creating an osmotic component that attracts water to the cartilage. Because of this water attraction, there is an outward pressure which maintains the stiffness of the cartilage. This arrangement ensures a low-friction interface in the joint, which gives it the possibility to cope with load (18). The osteoarthritic joint The biochemical changes in the joint consist of the loss of proteoglycans. This loss of proteoglycans is particularly important because of their central role in the maintenance of cartilage integrity. Proteoglycan degradation results in reduction of the molecular weight of the aggregates and therefore loss of water from the articular cartilage. This leads to increased friction and together with the loss of stiffness of the collagen network, it might cause mechanical disruption of the cartilage (18). The characteristic structural changes are disorganisation and loss of articular surfaces and proliferation of tissues in and adjacent to these surfaces. The classic morphological changes of osteoarthritic articular cartilage begin with fibrillation. This is a local surface disorganization involving a splitting of the superficial layers of the cartilage. Eventually the splitting extends deeper, whereby it alters the normal arrangement of the collagen bundles. Splitting may extend as far as the junction with subchondral bone. As osteoarthritis progresses fibrillation is joined by synovial hyperplasia and osteophyte formation. The fibrillation and detoriation of articular cartilage leads to exposure of the subchondral bone and more generalised synovial changes. In response to these changes sclerosis of the subchondral bone develops by an incompletely understood pathogenesis. It is believed also the opposite may occur; sclerosis of the subchondral bone decreases local shock absorption. This increases forces on articular - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 8 cartilage, which is followed by changes in the articular cartilage. The joint becomes shaped differently, which is called remodelling. This is thought to be a mechanism to cope with the forces on the joint (46,48,55). Eventually the result is decreased joint motion and function, deformity, possible joint instability (and later on ankylosis) and also pain (27). Bennet described the pathological features of osteoarthritis in cats and dogs at three levels (5) : Changes in articular cartilage, changes in bone and changes in soft tissue. With regard to the articular cartilage the following was described: - Biochemical changes: dehydration and a change in quantity of proteoglycans. - Loss of surface chondrocytes: cartilage cells are lost from the superficial layers of the cartilage. - Flaking and fibrillation: horizontal flaking of the surface layer occurs, followed by splitting, eventually into the calcified layer. The cartilage can eventually be sheared of, which exposes subchondral bone. Fibrillation of the cartilage occurs. - Chondrocyte clumping: formation of clumps or nest of cells. These may be an attempt to repair damaged cartilage. For bone the following was described: - Periarticular osteophytes: marginal proliferations of bone. - Subchondral bone sclerosis: associated with cartilage loss. - Subchondral bone cysts: these are seen in dogs. - Bone remodelling: osteophytes, subchondral sclerosis and cyst formation are parts of bone remodelling. For soft tissue the following was described: - Synovial membrane: hypertrophy and hyperplasia of the lining layer and increased thickness of the supportive connective tissue. - Joint capsule: fibrous thickening of the joint capsule regularly occurs. - Menisci: several changes in menisci occur, as fibrillation, calcification, splitting, shredding, tearing and osseous metaplasia. - Vascular changes: hyperaemia of the bone marrow of the bone occurs and vascular tufts are seen proliferating to the bone-cartilage interface. Vascular proliferation also occurs with osteophyte formation. Hyperemia of the synovial membrane and joint capsule can also be present (5). - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 9 Clinical symptoms Regarding clinical symptoms in cats, relatively little is described. Bennet et al evaluated symptoms in cats by descriptions of owners on a survey list (4). Most seen was unwillingness to jump, jumping less or less high and inactivity. Seldomly a clear limp was reported by owners. In the survey, questions were asked about lifestyle (e.g. jumping on furniture, activity levels, aggressiveness and lameness) and weight of the cat. No significant correlation was seen between lifestyle and osteoarthritis and between weight and osteoarthritis. Bennet did see a higher incidence of osteoarthritis in older cats than in younger cats (4). Clarke et al also evaluated lifestyle, age, breed, gender and weight of a group of cats to find a correlation with osteoarthritis (9). Only age was related significantly in cats with osteoarthritis. Osteoarthritis was diagnosed more frequently in elder cats than in younger ones. No other correlations were found and Clarke et al stated that this is similar to the human severeness of osteoarthritis- clinical lameness relationship (9). In this relation the severeness of osteoarthric changes do not match the clinical symptoms in that human. Sometimes extensive osteoarthritis is present, but without clinical symptoms. Hardie et al describes that cats can compensate for their pain and hide symptoms (17). Owners may see behavioural changes, like grumpiness and more lethargic cats, and inabilities. Inabilities like inadequate grooming behaviour, missing the cat’s litterbox and not jumping high. Seldomly lameness is seen. In cats with chronic pain also subtile findings like constipation, bad posture while urinating or defaecating, incontinence and inadequate grooming can be seen. Hardie et al stated that osteoarthritis can’t be associated with these clinical symptoms (17). Clarke et al researched the effect of meloxicam therapy in cats with osteoarthritis (8). 67.0% of the cats showed changes in jumping behaviour. Clarke stated that weight loss, anorexia, depression, abnormal elimination habits, inadequate grooming, aggression, reduction of jumping, stiffness and lameness are signs of osteoarthritis (8). After therapy 61.0 % of the owners noticed improvement, but no placebo group was available. Shires et al names some possible inheritable causes of osteoarthritis like patella luxation in the Devon Rex, hip dysplasia in Siamese cats and athropathy in Scottish Folds (34). The named clinical symptoms were inadequate grooming behaviour, trouble with jumping on furniture and trouble with getting in/out of the litterbox. Increased irritability may also be present. Obvious lameness was not seen (34). Lascelles et al hypothesed that subjective evaluation by owners and an activity monitor collar can be used for pain measurement in cats (22). This research was done because there was no validated method to measure pain in cats with osteoarthritis. Thirteen cats were part of the research, which all had less activity according to the owners. The cats received meloxicam therapy or a placebo. The research showed that activity increased more in cats with meloxicam therapy than in cats with placebo therapy (22). Activity might be a marker to use for therapy regulation in cats with pain and reduction in activity might also be used as one of the predictive symptoms for the level of discomfort in osteoarthritic cats. Diagnostic possibilities A proper signalment and history taking are thought to be important steps in the diagnosis of osteoarthritis. Mostly affected are elderly cats, therefore it is important to pay special attention to the history in these cats for symptoms like stiffness, behavioural changes and less jumping (5,7,8,9,14) . Caney developed a question survey for owners, which can help to identify locomotion problems like osteoarthritis in cats. The summary of this questionnaire has been displayed in table 4 (7). - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 10 Table 4: questionnaire summary Changes in ability or enthusiasm to: Noticed: Changes in behaviour: Other questions: Go up and/or down stairs Use the cat flap Jump onto/off bed/sofa/lap/etc. Jump or climb into/onto its favourite bed Play Climb trees/fences/etc. Use scratching posts Stiff or stilted gait Limp Vocalizing or hissing in response to moving around or being stroked over joints Grumpy or less happy with people and other animals More withdrawn, less interaction Less active Sleeping in different locations Not coming upstairs Passing urine or faeces in abnormal locations Purring less Reduced appetite Changes in coat condition and/or grooming behaviour, neglecting certain areas, overgrooming certain areas Weight change Muscoskeletal injuries in the past Any affected relatives (especially more common hip dysplasia in Maine Coon and possible Siamese, Burmese, Tonkinese, Oriental and Balinese) (7) In history taking questions should also be asked to rule out other diseases, especially in the geriatric cat. Because of the variety of possible causes of osteoarthritis, underlying diseases must be ruled out. Additionally, profound clinical exam needs to be done, including general examination and orthopaedic examination. One of the difficulties in the orthopaedic examination is the fact that cats dislike the consulting room and will not easily display their gait and jumping behaviour. In order to solve this issue it is possible to ask the owner to capture the gait and jumping of the cat in his normal environment with a camera. In orthopaedic assessment it is also hard to link the reactions to the exam to any orthopaedic pain, because the cat might only resent being handled. Pain score models can be used, but are still hard to apply in cats. An example of a pain scale model for animal pain, the University of Melbourne Pain Scale, is given in table 5. (19). Joint swelling, reduced range of motion and crepitus are not often seen. Joint thickening can be seen more commonly and the mostly affected joint is the elbow joint (7). - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 11 Table 5: University of Melbourne Pain Scale Model Category Physiological data Response to palpation Activity Mental status Posture Vocalisation Descriptor - Within reference range - Dilated pupils - Percentage increase in heart rate: > 20% > 50% >100% - Rectal temperature exceeds reference range - Salivation - No change from preprocedural behaviour - Guards/reacts when touched - Guards/ reacts before touched - At rest: sleeping semiconscious awake - Eating - Restless - Rolling - Submissive - Overtly friendly - Wary - Aggressive - Guarding or protecting affected area (including fetal position) - Lateral recumbence - Sternal recumbence - Sitting or standing, head up - Standing, head hanging down - Moving - Abnormal posture Score 0 2 - Not vocalising - Vocalising when touched - Intermittent vocalisation - Continuous vocalisation 0 2 2 3 1 2 3 1 2 0 2 3 0 0 1 0 2 3 0 1 2 3 2 0 1 1 2 1 2 A table taken from (19) When the clinician suspects that the cat might be suffering from osteoarthritis, the next step in the process should be making radiographic images. The majority of cats can be imaged properly without sedation. If proper positioning is not possible because of the lack of cooperation of the cat, it may be needed to sedate the cat, in which care should be taken because of the age and other diseases of the cat. The ASA classification should be 2 (slightly 12 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 or moderate systemic disease causing no obvious incapacity, geriatric animals) to 3 maximally (mild to moderate systemic disease causing mild symptoms) (16). Synovial fluid collection and cytological and bacteriological evaluation of this fluid are rarely indicated in cats. For example an indication to evaluate synovia includes the involvement of multiple joints, in which case the examiner should try to rule out the option of polyarthritis (7,15,34) . Radiographic symptoms Diagnostic approach of osteoarthritis in cats is also a new research subject (9,12). Clarke et al evaluated radiographs of 218 cats, in which 33.9 % (74 cats) showed signs of osteoarthritis (9). In 65.3% of the osteoarthrotic joints mild osteophyt formation was present, which suggests that osteophyt formation in the cat is not as extensive as in dogs (9). Kamishina et al evaluated radiographic images of the hips of cats for signs of osteoarthritis together with microscopic evaluation of the joints (21). Low correlation between the radiographically found changes and the microscopic evaluation of the joints was found. In 134 cats in which radiographs were evaluated to be normal, 38 (28.4%) still had mild to moderate histological cartilage lesions at post-mortem evaluation of the hip joints (21). Owens et al investigated which radiographical signs can be used as markers for osteoarthritis (28) . Narrowing of the joint space, osteofyt formation and subchondral bone sclerosis are often seen in dogs. Joint deformities and partial to complete ankylosis of the joint are also named in dogs (28). Signs of synovial effusion and/ or thickened periarticular soft tissue are seen less commonly in cats than in dogs. The incidence of intraarticular soft tissue calcification is seen more commonly in cats than in dogs (25,35). Van Gastel-Jansen defined classical radiographical symptoms of osteoarthritis including irregular joint space, narrowing in some areas of the joint space and normal or enlarged joint spaces within the same joint. The articular surfaces are rough, if the articular cartilage has been destroyed. Osteolytic areas and bone proliferation can be seen on the joint margins and also on the periarticular areas. Free bodies can develop in the synovial fluid (10). Caney describes the following possible radiographic findings: peri-articular new bone formation (in form of osteophytes or enthesiophytes), narrowing of joint spaces, sclerosis of subchondral bone, bone remodelling, soft tissue thickening/swelling around the joint (possibly involving the joint capsule) and joint effusion (7). Osteophytes are first seen as an area of proliferation of mesenchymal tissue in the transitional zone between the synovial membrane and the articular cartilage. The tissue undergoes metaplasia to form bone. After endochondral ossification, it is a prominent feature. It is associated with the appearance of numerous blood vessels and therefore appears to be a vascular reaction associated with new bone formation (5). In order to pathologically score the severeness of the osteoarthritic changes in the cat, the human gradation system from Ghadailly has been proposed (11). The gradation is as following: Degree 1: Destruction of superficial cartilage, on surfaces of highest pressure and movement. No hyperplasia on the margins of cartilage or bone. Capsule, synovial membrane and articular margins are normal. Degree 2: More extensive cartilage destruction, still confined to surfaces of highest pressure and movement, on which no bone is exposed. Early margin hyperplasia (ridge formation) along the margins of the surfaces. No large osteophytes or bone remodelling. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 13 Degree 3: Total loss of cartilage on one ore more pressure surfaces, with exposure of subchondral bone and often bone sclerosis. Clear osteophyt formation on the joint margins. Change of contour of the joint surfaces. Sclerosis of subchondral bone and fibrosis of the capsule. Degree 4: Complete loss of cartilage on large areas of the joint surface. Sclerosis of exposed bone. Irregularity of the surface, osteophytes, remodelling, fibrosis of the capsule and synovial membrane (11). After all of these descriptions of the radiographic and pathologic signs in the osteoarthritic joint the conclusion can be that osteoarthritis in cats can be characterized by narrowing of the joint space, articular cartilage destruction, subchondral bone sclerosis and osteophyte formation (4,6,9,15,21,25,30,31). Therapeutical options Similar to other species, consideration of the therapeutical options and advice to the owner by veterinarians for cats with osteoarthritis should not only include medicamental or surgical treatment, but also environmental changes. The goal of the treatment of osteoarthritis is to improve the quality of life of the cat through symptomatic and supportive measures. These measures should help to increase mobility, reduce pain, reduce the possibility of further joint damage and improve the total quality of life (7,18). Medicamental options are mainly Non Steroidal Anti-Inflammatory Drugs (NSAID’s) for pain relief. Carefulness with the use of NSAID’s is needed, because of the possible side effects. Side effects include reduction of the appetite, vomiting, diarrhoea, occult faecal blood loss, apathy, kidney problems, liver problems and clotting disorders (3,22,23,33,37,38). In the Netherlands a registered NSAID is Tolfenamic acid (Tolfedine®), which has the indication of pain relief in cats. Recently an oral suspension NSAID for long-term use in the cat was registered, Meloxicam (Metacam®) (3,13,37,38). Controversy exists about the use of glucocorticoids, as they have not proven to be efficient. There is even evidence of inhibition of the proteoglycan and collagen synthesis, which gives progression of osteoarthritis in stead of reduction (3,18, 26,32). Weight reduction is important for obese cats. As is thought for dogs, in cats weight normalisation will lead to decreased forces on the joint and thereby possibly less pain while moving the joint. Another helpful adjustment is placing the food and water bowls on a lower level, with easy access for the cat. In this way the cat doesn’t have to jump high to eat or drink. The same can be done with the litter box, it can be placed on a low location and it is even possible to use a litter box with low edges. The cat has easy access to the litter box and if missing the litter box has been a problem, this could solve the problem. A step up can be made between higher objects like the windowsill and the floor, for gradual access instead of a high jump. Unlike dogs it is not easily done to walk the cat on a leash, therefore leash exercise is not always a possible option. Some cats may dislike water, some cats may not, therefore swimming is also not always an option. A replacement of this is inducing extra exercise by strategic placement of the litter box, food and drinking bowls. The cat needs to walk for example to eat or drink. In this way the location is quite easily accessible, but the cat needs to walk towards it and thereby have some exercise. Tempting the cat with snacks is also a way to induce exercise, but care is needed with regard to the development of obesity and unwanted behavioural patterns. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 14 Some cats with osteoarthritis are not able to groom efficiently. One of the options to help the cat with this, is to have the owner brush the cat. The use of padded bedding in the cat‘s basket is recommended for the protection of the joints. Even heated beds can be used, on which the cat will lie with cold weather (6,7,18,26, 32,33,36). Several pet food manufacturers are developing special joint diets or mobility diets. These diets should help the cat with their mobility and reduce osteoarthritic changes in the joints and reduce pain. Although the diets have not been proven to be efficient, it might be worth to try for the osteoarthritic cat owners. For example, one of these diets is the Joint Diet (J/D) from manufacturer Hill’s. Several studies were performed to assess the clinical effectiveness of the diet, but no conclusive difference was seen between cats that were fed the J/D diet and cats that were fed a control diet (43). Last option to be considered is the use of chondroprotective agents and nutraceutical agents. They are also called Disease Modifiyng Osteoarthritic Drugs. Slow acting disease modifying products like Cosequin® can be of use in therapy for osteoarthritis and contain chondrotoin sulphate and glucosamine as main ingredients. Efficacy of the products has not been proven, but they appear to be safe for use in the cat (2,3,30,31,32,33). Prognosis Osteoarthritis is a progressive condition. It is not possible to reverse the changes in the joint. Therefore the prognosis for complete recovery is not good at all. Prognosis for an acceptable life for the cat is fair to good. These cases exclude the cats with severe osteoarthritic changes, that still have extensive pain with analgesics, in which cases euthanasia might even be considered. For cats with mild to moderate osteoarthritis an acceptable status of living can be achieved with therapeutical options like medication and changes to the cat’s environment (18,32) . Discussion The term “osteoarthritis” may (inappropriately) suggest an exclusively inflammatory cause. Both “osteoarthritis” and other terms are used in literature, although the authors report on the same disease. Therefore it is quite difficult to find out what disease is discussed and to draw the right conclusions from that report. Another problem in literature is the fact that not all authors distinguish between osteoarthritis and spondylosis deformans. If this goes unnoticed by the reader false conclusions can be made about, for example, prevalence (9,17). Also the reported prevalence in some reports is not reported as the prevalence per joint. Therefore no conclusions can be made about the amount of osteoarthritis per joint and whether one of the joints is more often affected than other joints (12). Risk factors and prevalence for osteoarthritis in cats are difficult to establish. Obesity is a thought to be a risk factor, but was not shown to be so in some studies. The only established risk factor in cats for osteoarthritis is the age of the cat (4,9). More research is needed to distinguish other risk factors and to obtain a better approximation of the prevalence in the cat. Assessing pain in animals is a very difficult thing to do. Pain score models for evaluation of pain in cats have been developed, for instance the University of Melbourne Pain Scale Model (19) . One should always compare the cat’s normal behaviour with the behaviour at that time in the examination room. However, assessing pain remains difficult, as a cat that is continuously vocalizing may be in pain, but vocalisation could also reflect stress caused by travelling to and being in the examination room. Medicamental options for osteoarthritis consists of the use of NSAIDs. Until recently only tablets were registered for pain relief in cats. Recently a new NSAID (Metacam®) was registered for the use in cats, which is an oral suspension. For therapy reliability this oral 15 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 suspension could be a good choice, because lots of owners have trouble with giving tablets to their cats. With this new medicamental therapy, one should also be aware of possible side effects. Despite the fact this medicament is relatively safe, it is still a NSAID and side-effects should be monitored by the owners (22,23,33,37,38). Diets were not proven to be efficient yet, but it might be worth to try for the osteoarthritic cat owners (43). Nutraceutical agents and chondroprotective agents are also suggested for cats, but there’s no definitive evidence of the effectiveness of these products. Therefore it is needed to discuss the possibility of use in the cat with the owner, but it should always be mentioned that the effectiveness is not proven (2,30,33). The veterinarian should not only give the owner medicamental options, but should also speak with the owner about environmental issues. These changes might be of greater importance for the cat with osteoarthritis, than the medicamental options given and should be discussed properly (7,18). Conclusion Osteoarthritis in cats may be an under recognised disease, which is receiving quite some attention at the moment. The objective of this literature study was to describe the prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat, as it has been thought to be higher as yet recognized. No definitive remarks on prevalence can be made. Differences and the inclusion of spondylosis deformans in several researches, make it difficult to compare the studies with each other. Carefulness is needed when searching for literature with regard to the nomenclature of the diseases. Often used names are “osteoarthritis”, “osteoarthrosis” and “degenerative joint disease”. Radiographic and pathologic signs of osteoarthritis in cats might not be as extensive as the signs in dogs, but mostly narrowing of the joint space, articular cartilage destruction, subchondral bone sclerosis and osteophyte formation are named. Awareness of osteoarthritis in the elderly cat is needed in veterinarians to be able to learn owners about this new disease in cats. During check-up’s and scheduled vaccination visits veterinarians should ask questions about the lifestyle of the cat in order to detect signs of osteoarthritis and other possible diseases. After diagnosing osteoarthritis in cats, the veterinarian should take time to explain the importance of environmental changes and if necessary explain the possibility of medication to the owner of the cat. Additionally, weight normalisation may be discussed. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 16 Part two: radiographic retrospective study Abstract A retrospective study of 471 radiographic images of cats from the archives of the Division of Diagnostic Imaging of the University Clinic for Companion Animals in Utrecht was performed. All visible joints were evaluated with regard to osteoarthritic changes. Breed, gender, age, weight, diagnosis and (history of) trauma were recorded in each cat. This was done to identify possible risk factors for osteoarthritis in cats. Logistic regression was performed per joint to evaluate putative risk factors (i.e. breed, gender, age, weight, trauma and diagnosis) in the development of osteoarthritis in cats. The prevalence of osteoarthritis in cats in this study was 36.7%. A significant relation was found between age and the degree of osteoarthritic changes in the shoulders (P<0.001), elbows (Pelbow1<0.001 and Pelbow2=0.015) and stifles (P=0.002). Cats are more likely to have osteoarthritic changes, as their age advances. Depending on the joint, the odds of having osteoarthritis increased with a factor of approximately 1.3 per extra year of age. No other putative risk factors were found to be significant. The prevalences of osteoarthritic changes in the evaluated joints are summarised. Not enough data was available to draw conclusions on the prevalence of osteoarthritis in the carpus and tarsus. Most of the osteoarthritic changes in the joints were graded as mild osteoarthritic changes. Less often the changes were graded as severe osteoarthritic changes. Osteoarthritis more often occurs bilaterally than unilaterally in shoulders and hips (P<0.001 for both). If one of the shoulder or hip joints was positive for osteoarthritis, in 86% (shoulders) and 95% (hips) of the cases osteoarthritic changes were also found in the contralateral joint. This report demonstrates an increased odds of having osteoarthritis in the joints of the appendicular skeleton of cats with increasing age, confirming the results of several other researches. Osteoarthritis in the elderly cat may be a new disease for the veterinarian to assess in the geriatric cat. Introduction As a second part of this research project, evaluation of the prevalence of osteoarthritis in the joints of the appendicular skeleton on radiographs from the archives of the Division of Diagnostic Imaging of the University Clinic for Companion Animals in Utrecht was performed. In this retrospective study, radiographs were evaluated from cats which were presented at the University Clinic. Together with this evaluation of radiographs, the history of the cats was evaluated to identify putative risk factors for osteoarthritis in cats (for example weight, age, trauma and other diseases). The evaluation of the radiographs was supervised by a Diagnostic Imaging Specialist. The objective of this report was to find out if the prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat is higher as yet recognized. Materials and methods At first a selection of radiographic material from the department of Diagnostic Imaging of the University Clinic for Companion Animals in Utrecht was made by collecting all radiographic material from cats from May 26th 2004 until January 17th 2007, on which one or more joints are visible. Whenever only a part of the joint was visible or the joint was superimposed on another radio dense structure, the joint was not included in the research. Shoulders were only 17 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 evaluated, when both shoulders were visible and gradable. The other joints were always named 1 (i.e. elbow 1 or stifle 1) if only one of these joints was present on the radiographs. If the contralateral joint of a cat was also visible and gradable, this joint was named 2 (i.e. elbow 2, stifle 2, etcetera). Age, breed, gender, weight, diagnosis and (history of) trauma of the cats were also recorded. These were used to find possible relations between these variables and osteoarthritis. Descriptives of these variables are outlined in the following paragraph: Age: the age of the cat on the day of the radiographic imaging was calculated in years and months, i.e. a cat was for instance 6 years and 3 months old. The ages were then converted to a decimal scale. Age was considered to be a continuous variable for statistical analysis. Breed: Cats from 25 different breeds were included. Each breed was given a number, as described in table 6. The breed selection was done by the information on the chart of the patient. Breed was considered to be a nominal variable for statistical analysis. Table 6: breed classification 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 Domestic Shorthair European Shorthair Siamese Persian Maine Coon Abyssinian Norwegian Forest cat Cornish Rex British Shorthair Havanna Brown Eastern Shorthair Selkirk Rex Turkish Angora Burmese Crossbred Exotic Shorthair Sphinx Holy Birman Bengalese Tonkinese Ragdoll Somali Siberian Russian Blue Devon Rex Gender: 5 different gradations were made for the gender, as described in table 7. Only complete gender information on the charts was used. Gender was considered to be a nominal variable for statistical analysis. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 18 Table 7: gender classification 1 2 3 4 99 Male neutered Female neutered Male Female Unkown Weight: at presenting of the cat at the university clinic, many cats were weighed. All available weights were recorded. The weights were rounded to one decimal. Weight was considered to be a continuous variable for the statistical analysis. Diagnosis: when final diagnosis of a disease in a cat was made, this was also recorded. Later on the diagnoses were grouped into main categories. These categories are described in the table below. Diagnosis was considered to be a nominal variable for the statistical analysis. Table 8: diagnosis classification 1 Main categories of diseases Cardiovascular 2 Pulmonary 3 4 5 6 7 8 9 Gastrointestinal Orthopaedic Nervous Kidney/Urinary tract Endocrine Hepatic Haematologic 10 11 12 Ear nose throat Fever of unknown origin Traumatic cases 13 Neoplasia 14 15 99 Multiple problems Other No Diagnosis Descriptive Hart failures, cardiomyopathies. Special note: liquothorax & HCM is described as cardiovascular. Bronchitis, liquothorax, hernia diaphragmatica (nontrauma), asthma and tracheal problems. Primary lungtumors and lung metastasis were noted as neoplasia. All gastrointestinal diseases, including corpora aliena Non-traumatic orthopaedic cases Central nervous system and peripheral nervous system Urinary tract problems and kidney problems All endocrine disorders All hepatic and cholangial diseases Haematologic disorders, including immune mediated haemolytic anaemia All ear, nose and throat problems Cat presented with fever of unknown origin Car accidents, falling from heights, gunshot wounds, bone fractures, pneumothorax (traumatic), hernia diaphragmatica (traumatic), bite trauma All sorts of tumors, including abdominal, cardiovascular and pulmonary neoplasia Several diseases simultaneously, except trauma Diseases which can not be categorised No definitive diagnosis/ symptoms Trauma: trauma was graded as no known trauma, trauma in present, trauma in past and a combination of trauma in past and present, as described in table 9. For further statistical analysis (logistic regression) the cases were classified as with (a history of) known trauma (1) or not (2). Trauma was considered to be an ordinal variable for the statistical analysis. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 19 Table 9: trauma classification 0 1 2 3 No known trauma Trauma Trauma in past Trauma + trauma in past Osteoarthritis: the visible joints on the obtained radiographic images were graded per joint with regard to visible osteoarthritic changes, as described in table 10. For the logistic regression analysis the cases were regrouped into a group with osteoarthritic changes (1) and a group without (2). Osteoarthritis was considered to be an ordinal variable for the statistical analysis. Table 10: osteoarthritis classification 0 1 2 99 No osteoarthritic changes Mild osteoarthritic changes Severe osteoarthritic changes Joint not visible Overall formation of the joint, osteophyte formation, subchondral bone sclerosis and other abnormalities are evaluated and scaled. The difference between mild and severe osteoarthritic changes was the appearance of a loose fragment in the joint, extensive irregularity of the joint surface and the appearance of large osteophytes. Minimal irregularity of the joint surface and small osteophytes were graded to be mild osteoarthritis. All gradable joints were placed in an excel sheet, whereby also the directions of the taken radiographs were recorded. Mostly these included a dorso-ventral and dextro-sinistral image of the shoulders; a ventro-dorsal and dextro-sinistral image of the hips; a medio-lateral and a posterior-anterior image of the elbows, stifles, carpus and tarsus. If only a ventro-dorsal view of the hips or a dextro-sinistral view of the shoulders was present, this radiograph was also evaluated and graded. Whenever only a dextro-sinistral view of the hips (or a dorso-ventral view of the shoulders) were available for evaluation, these joints were not included in the study, because of not being able to evaluate the complete joint surface. After collection the data was entered into the statistical program “ SPSS 12.0.1 for windows”. Each continuous variable (i.e. age, weight) was tested for normality using the KolmogrovSmirnov test with Lillifors significance correction. The aim of this test was to find out if the continuous variable was distributed parametrically or not. For each joint the frequencies of each grade were tabulated. The prevalence of osteoarthritis per joint was calculated as the number of affected joints divided by the number of included joints. Univariate logistic regression was performed per joint to separately evaluate each putative risk factor (i.e. breed, gender, age, weight, trauma and diagnosis) in the development of osteoarthritis in cats. The Hosmer-Lemeshow goodness-of-fit test was used to evaluate the fit of the regression model. Whenever univariate regression analysis per joint revealed more than one putative risk factor (P<0.05), these risk factors were analysed together using multivariate logistic regression. A backward stepwise (based on likelihood ratio) approach was used. Variables with P>0.05 were removed from analysis. P<0.05 was considered to be significant. A binominal test was performed to investigate the gender distribution in the cats in this report. A Chi-square test was used to determine if the risk of having osteoarthritis in one shoulder or hip was higher if the contralateral joint was already diagnosed with osteoarthritis. Within the group of cats with unilateral osteoarthritis it was assumed that osteoarthritis occurred in the right joint as frequently as in the left joint. 20 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 Results Frequency tables were made of all assessed variables. These are displayed in the tables below. For general view table 11 was made considering the frequencies of ages from the cats. Table 11: age frequencies Age number 1 2 3 4 5 Total Age 0-5 years >5- 10 years >10-15 years > 15 years Missing Frequency (n) 185 138 116 25 7 471 Frequency (%) 39.3 29.3 24.6 5.3 1.5 100.0 The age frequencies of the cats in the research are also displayed in the histogram in figure 2. Figure 2: age frequencies 50 Frequency 40 30 20 10 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Age (years) Subjectively, in figure 2 it seems that the amount of younger cats is higher than the amount of elderly cats in this research. In the first two categories 42 and 50 cats are present, which seems to display that more younger cats (until 2 years of age) are presented at the Division of Diagnostic Imaging of the University Clinic for Companion Animals in Utrecht for radiographic imaging. After 14 years of age the amount of cats presented for a radiographic image diminishes, which may be explained by the average age cats are becoming these days. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 21 The variables age and weight were not distributed parametrically (P<0.001 and P=0.038, respectively) Therefore the median and range are reported in table 12. Table 12: age and weight distribution Age Weight Distributed parametrically No No Median Range 7.0850 4.00 0.25 – 17.17 1.10-8.20 To assess the average bodyweights of the cats versus the age of the cats in the research a histogram has been made. The average weight (with 95% confidence interval) per age category are displayed in figure 3. Figure 3: weight versus age distribution Weight seems to be quite constant throughout the age categories. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 22 The frequencies of different breeds were assessed and outlined in table 13. Table 13: breed frequencies Breed number 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 Breed Domestic Shorthair European Shorthair Siamese Persian Maine Coon Abessian Norwegian Forest cat Cornish Rex British Shorthair Havanna Brown Eastern Shorthair Selkirk Rex Turkish Angora Burmese Crossbred Exotic Shorthair Sphinx Holy Birman Bengalese Tonkinese Ragdoll Somali Siberian Russian Blue Devon Rex Frequency (n) 121 212 18 18 20 2 7 2 20 1 8 1 2 3 14 1 3 7 1 1 3 2 1 2 1 Frequency (%) 25.7 45.0 3.8 3.8 4.2 0.4 1.5 0.4 4.2 0.2 1.7 0.2 0.4 0.6 3.0 0.2 0.6 1.5 0.2 0.2 0.6 0.4 0.2 0.4 0.2 Domestic shorthairs and European shorthairs together represented more than 70% of the presented cats. Most of the cats were European shorthairs (45.0%), followed by Domestic shorthairs (25.7%), Maine Coons (4.2%), Siamese (3.8%), Persians (3.8%) and Crossbreds (3.0%). The distribution of the genders is outlined in table 14. Table 14: gender frequencies Gender number 1 2 3 4 99 Gender Male neutered Female neutered Male Female Unknown Frequency (n) 230 172 36 32 1 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 Frequency (%) 48.8 36.5 7.6 6.8 0.2 23 Slightly more neutered males were present in the cases and somewhat less neutered females, as confirmed by a binomial test, which showed a higher prevalence of neutered males (57.0%, P=0.004). Intact males and females were not presented as much. All cases were assessed for any trauma in past or present. The frequencies are displayed in table 15. Table 15: trauma frequencies Trauma number 0 1 2 3 Trauma No known trauma Trauma Trauma in past Trauma + trauma in past Frequency (n) 382 84 4 1 Frequency (%) 81.1 17.8 0.9 0.2 The table shows that 18.9% of the cases were presented for a history of trauma or had trauma. In 81.1 % of the cases there was no known (history of) trauma. Sixty-six percent of cats with a history of trauma (in the past, recent or both) were male. Finally, all diagnoses were categorized into disease categories. These are displayed below in table 16. Table 16: disease frequencies Disease number 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 99 Disease category Cardiovascular Pulmonary Gastrointestinal Orthopaedic Nervous Kidney/Urinary tract Endocrine Hepatic Haematologic Ear nose throat Fever of unknown origin Traumatic cases Neoplasia Multiple problems Other No Diagnosis Frequency (n) 31 105 25 9 16 18 3 5 7 6 6 80 88 59 6 7 Frequency (%) 6.6 22.3 5.3 1.9 3.4 3.8 0.6 1.1 1.5 1.3 1.3 17.0 18.7 12.5 1.3 1.5 The main disease categories are pulmonary, traumatic cases, neoplasia and multiple problems. Together these categories account for 70.5 % of total cases. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 24 The frequencies of osteoarthritis, visibility of the joints and severeness of osteoarthritis are listed in table 17 and 18 below. The gradations used were no osteoarthritis (0), mild osteoarthritis (1) and severe osteoarthritis (2), as described in table 10. Table 17: osteoarthritis gradation Shoulder 1 Shoulder 2 Elbow 1 Elbow 2 Hip 1 Hip 2 Stifle 1 Stifle 2 Carpus 1 Carpus 2 Tarsus 1 Tarsus 2 Grade 0 Grade 0 (%) Grade 1 Grade 1 (%) Grade 2 179 187 44 25 37 38 23 11 1 0 5 0 38 39.7 9.3 5.3 7.9 8.1 4.9 2.3 0.2 0 1.1 0 51 43 36 7 14 15 5 3 1 0 2 0 10.8 9.1 7.6 1.5 3.0 3.2 1.1 0.6 0.2 0 0.4 0 8 8 9 5 6 4 6 2 0 0 0 0 Grade 2 (%) 1.7 1.7 1.9 1.1 1.3 0.8 1.3 0.4 0 0 0 0 Not Visible: 99 233 233 382 434 414 414 437 455 469 471 464 471 Not Visible: 99 (%) 49.5 49.5 81.1 92.1 87.9 87.9 92.8 96.6 99.6 100 98.5 100 Table 18: osteoarthritis prevalence Shoulder 1 Shoulder 2 Elbow 1 Elbow 2 Hip 1 Hip 2 Stifle 1 Stifle 2 Carpus 1 Carpus 2 Tarsus 1 Tarsus 2 OA positive Visible joints 59 51 45 12 20 19 11 5 1 0 2 0 238 238 89 37 57 57 34 16 2 0 7 0 Total OA in visible joints(%) 24.8 21.4 50.6 32.4 35.1 33.3 32.4 31.3 50.0 0 28.6 0 Grade 1 OA in visible joints (%) 21.4 18.0 40.4 18.9 24.6 26.3 14.7 18.8 50.0 0 28.6 0 Grade 2 OA in visible joints (%) 3.4 3.4 10.1 13.5 10.5 7.0 17.6 12.5 0 0 0 0 Almost 24.8 % and 21.4 % of the visible shoulder joints had osteoarthritic changes. Even 50.6% of the visible elbow 1 joints had osteoarthritic changes, followed by 32.4% in elbow 2. The osteoarthritic hips accounted for 35.1% and 33.3% of the visible hip joints. In Stifle 1 a percentage of 32.4% of visible joints was osteoarthritic and 31.3% in stifle 2. The obtained data for carpus and tarsus were not enough to draw conclusions about these joints. Therefore these data were only summarised, but no statistical analysis were performed. Logistic regression was performed for each joint with the six different variables listed in table 19. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 25 Table 19: logistic regression Breed Gender Age Weight Trauma Diagnosis Shoulder 1 Shoulder 2 Elbow 1 n.s. n.s n.s n.s. n.s n.s s. s. s. s.n.s. n.s n.s n.s n.s n.s n.s n.s n.s Elbow 2 Hip 1 Hip 2 Stifle 1 Stifle 2 n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s s. n.s n.s s. n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s n.s. = not significant; s. = significant; s.n.s = significant after univariate logistic regression, but not significant anymore after multivariate logistic regression. As is shown in table 19 age was a significant risk factor for osteoarthritis in shoulder 1, shoulder 2, elbow 1, elbow 2 and stifle 1. No other risk factors were found to be significantly related to osteoarthritis. Hip 1, hip 2 and stifle 2 were not significantly related to any of the variables. For shoulder 1 age was a significant risk factor (P<0.001). The odds ratio for age was 1.31 after multiple logistic regression. This means that when the age of the cat advances with one year, the odds of developing osteoarthritis in this shoulder must be multiplied with a factor of 1.31. In the univariate logistic regression model shoulder 1 at first age and weight seemed to be risk factors. After the multivariate logistic regression model only age remained. This may be due to the fact that there is a correlation between both variables within the shoulder 1 category, but the age variable was most important. For shoulder 2 age was a significant risk factor (P<0.001). The odds ratio for age was 1.32. In elbow 1 age was a significant risk factor (P<0.001). The odds ratio was 1.25. The same is true for elbow 2, in which age was a significant factor (P=0.015). The odds ratio for elbow 2 was 1.27. For stifle 1 age was a significant factor (P=0.002). The odds ratio was 1.43. No significant risk factors could be distinguished for hip 1, hip 2 and stifle 2. All of the joints that were significantly related to age were placed into tables, for a general overview in which age categories osteoarthritis was seen most. The gradations of osteoarthritis were regrouped into a group with osteoarthritic changes (1) and a group without (0). This is displayed in tables 20, 21, 22, 23 and 24. Table 20: osteoarthritis and age in shoulder 1 Shoulder 1 0-5 years >5-10 years >10-15 years >15 years Total No osteoarthritis 82 (97.6%) 59 (73.75%) 32 (53.3%) 5 (41.7%) 178 (75.4%) Osteoarthritis 2 (2.4%) 21 (26.25%) 28 (46.7%) 7 (58.3%) 58 (24.6%) Total 84 (100%) 80 (100%) 60 (100.0%) 12 (100%) 236 (100%) Quite a lot of shoulder joints were evaluated. It would seem that above 5 years of age more osteoarthritis is present than below 5 years of age. Above 10 years of age this number even seems to increase. In the > 15 years of age category less joints were evaluated. Possibly in cats > 15 years of age even more osteoarthritis is present, than in cats below 15 years of age. Table 21: osteoarthritis and age in shoulder 2 No osteoarthritis Osteoarthritis Total 0-5 years 82 (97.6%) 2 (2.4%) 84 (100%) Shoulder 2 >5-10 years >10-15 years 64 (80%) 35 (58.3%) 16 (20%) 25 (41.7%) 80 (100%) 60 (100%) >15 years 5 (41.7%) 7 (58.3%) 12 (100%) - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 Total 186 (78.8%) 50 (21.2%) 236 (100%) 26 Of shoulder 2 the same number of joints were evaluated as in shoulder 1, because of the criteria to evaluate both shoulders on the radiographs. Approximately the same distribution can be seen in shoulder 2 as in shoulder 1. Table 22: osteoarthritis and age in elbow 1 Elbow 1 0-5 years >5-10 years >10-15 years >15 years Total No osteoarthritis 23 (82.1%) 15 (45.5%) 5 (26.3%) 0 (0%) 43 (48.9%) Osteoarthritis 5 (17.9%) 18 (54.5%) 14 (73.7%) 8 (100%) 45 (51.1%) Total 28 (100%) 33 (100%) 19 (100%) 8 (100%) 88 (100%) Elbow 1 shows an increase in the number of osteoarthritic cases above 5 years of age. Above 10 years of age and above 15 years of age the prevalence seems to increase even more. Table 23: osteoarthritis and age in elbow 2 Elbow 2 0-5 years >5-10 years >10-15 years >15 years Total No osteoarthritis 9 (81.8%) 11 (84.6%) 5 (55.6%) 0 (0%) 25 (67.6%) Osteoarthritis 2 (18.2%) 2 (15.4%) 4 (44.4%) 4 (100%) 12 (32.4%) Total 11 (100%) 13 (100%) 9 (100%) 4 (100%) 37 (100%) Elbow 2 shows some increase of osteoarthritic cases above 10 years of age, but only little data is available. Table 24: osteoarthritis and age in stifle 1 Stifle 1 0-5 years >5-10 years >10-15 years >15 years No osteoarthritis 16 (94.1%) 5 (55.6%) 2 (40%) 0 (0%) Osteoarthritis 1 (5.9%) 4 (44.4%) 3 (60%) 3 (100%) Total 17 (100%) 9 (100%) 5 (100%) 3 (100%) Stifle 1 shows an increase of osteoarthritis above 5 years of age. Relatively available. Total 23 (67.7%) 11 (32.3%) 34 (100%) little data is Evaluation of the total prevalence of osteoarthritis in this report was done. A total number of 119 cats had osteoarthritis in at least one joint. This accounts for a prevalence of osteoarthritis of 36.7% (119/324). A number of 147 cats were not included in this calculation, as there were no joints present on the radiograph. Chi-square tests revealed that osteoarthritis more often occurs bilaterally than unilaterally in shoulders and hips (P<0.001 for both). If one of the shoulder or hip joints was positive for osteoarthritis, in 86% (shoulders) and 95% (hips) of the cases osteoarthritic changes were also found in the contralateral joint. Discussion High frequencies of osteoarthritis were seen in cats in the shoulders (c.q. 24.8 % for shoulder 1 and 21.4 % for shoulder 2) , elbows (c.q. 50.6% for elbow 1 and 32.4 % for elbow 2) and stifles (c.q. 32.4 % for stifle 1 and 31.3 % for stifle 2). A total percentage of 36.7% was found in this study for cats with at least one joint with signs of osteoarthritis. A significant relationship between age and osteoarthritis status is established in this study. The odds of having osteoarthritis increases with increasing age. Only the hips did not show a significant correlation between the joint osteoarthritis-status and the age of the cat. Two possible explanations can be made for this finding. At first it is possible that no significant correlation - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 27 was found, because of a too low amount of collected hip radiographs. The second explanation consists of the possibility of osteoarthritis at younger age for the hips, because of the disease hip dysplasia which is inherited and the osteoarthritis in these cats starts at young age. More research on this subject is needed to draw definite conclusions. Selection of suitable radiographic material from the archives of the Division of Diagnostic Imaging of the University Clinic for Companion Animals in Utrecht was done by collecting all radiographic images from cats from May 26th 2004 until January 17th 2007, with one or more visible joints. It may seem that these dates are randomly chosen, but this is not the case. All radiographic images later than January 17th 2007 were not obtained, because of a change in the archive system at the Division of Diagnostic Imaging. After this date all radiographs were made digitally and to prevent interpretation bias due to different techniques used to make radiographs, collection of the data was not done beyond January 17th 2007. Because of the amount of collected radiographs (approximately 500 radiographs), collection was not done further back than May 26th 2004. During collection of the different variables in the cats’ patient files, several things were noticed. The cats’ ages were not always known exactly. For example, the day of birth of a cat presented at June 21st 2004, of which the owner did not specifically know the date of birth but only knew the year of birth, was likely to be set at June 21st of that year. At least the year of birth matches in these cats and it is thought not to be of great influence on the age distribution of the cats, although it should be mentioned. Slightly more young cats than elderly cats were radiographed at the University Clinic. It is not known if this is representative for the age distribution in the general cat population. However, the general prevalence of osteoarthritis in this report could be slightly lower than in the general cat population. In most of other researches only geriatric cats were assessed, which may have influenced the outcome of these studies. In this study, a total of 119 cats had a positive osteoarthritis gradation in at least one joint. In the total number of evaluated cats this accounts for a prevalence of 36.7 % (119/324 cats). A number of 147 cats were not included, as there were no joints on the radiograph. If comparison of this research is made with the report of Clarke et al (9) and with the report of Godfrey (12) quite similar prevalences have been reported. Clarke et al stated a prevalence of osteoarthritis of 33.9 % (including spondylosis deformans), which can be recalculated into a percentage of approximately 22.0% for osteoarthritis alone in cats above 8 years of age (9). Godfrey also reported a prevalence of osteoarthritis of 22.0%, in cats above 1 year of age (12). When comparison of this research is made with the report of Hardie (17) a different prevalence is noted. Hardie stated a prevalence for osteoarthritis in cats of 90.0 % (including spondylosis deformans), which can be recalculated in 64.0% for osteoarthritis exclusively (17). The major difference between this research and the study of Hardie is that Hardie only evaluated cats above 12 years of age. This might be an explanation that the total prevalence found in this study is lower as the prevalence found in the study of Hardie. The fact that increasing age increases the odds of having osteoarthritis in elbows, shoulders and stifles supports this supposition. With regard to the cat’s breed many cats were categorised as Domestic Shorthairs or European Shorthairs. There is probably some confusion when it comes to the definition of European Shorthairs and Domestic Shorthairs. European Shorthair is a pedigree and the correct term for housecats that resemble European Shorthairs, but are of unknown descent, is Domestic Shorthair. The assumption is made that the obtained data has too many European Shorthairs in it, possibly caused by incorrect registering in the clinic’s database. Compared to neutered females, more neutered males were presented at the University Clinic. One may consider various explanations for this difference, although none can be definitively proven with this study. Most likely, there are as many females as males in the general cat population. The discrepancy between the amount of presented (neutered) males and females therefore may arise from a higher amount of male cats with medical conditions that require 28 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 radiographic imaging. For instance, in this study there seem to be more males than females with a history of trauma, possibly caused by the larger roaming space of male cats that may contribute to a higher chance of (car or other) accidents. No relation could be found between osteoarthritis and the weight of the cats in this study. Bennet and Clarke also evaluated weight as a possible risk factor in their studies, but no significant correlation was found between osteoarthritis and weight (4,9). When considering this, it is important to distinguish that for the several breeds included in this study, each breed has a different ideal weight. Thus, for example, a Siamese of 5 kilograms may be considered to be obese, but a Maine Coon of 5 kilograms is not considered to be obese. Ideally, body condition would be evaluated as a risk factor for developing osteoarthritis. There does not seem to be a relation between age and weight (figure 3). Therefore it seems unlikely that during the multivariate analyses the effects of weight were overruled by the effects of age. In each of the cases the history was searched for reported trauma. 18.9% of the cases had a report of trauma in their history. In 81.1 % of the cases no trauma was present. No significant correlation between trauma and osteoarthritis could be made in this study. In these cases the trauma cases were mostly cases with trauma at the date of presentation (for example a recent car accident). It is believed that osteoarthritis can develop after trauma in a progressive way (1,6,25,35) , but on the day of the trauma obviously no signs of osteoarthritis are present yet. Therefore no correlation between trauma and osteoarthritis could be made. If these cats with trauma would be radiographed later on in their lives, it is possible that a positive correlation could be found between trauma and later development of osteoarthritis. Many cats were presented with pulmonary problems, trauma, neoplasia and multiple problems. Because of the referral status of the University Clinic it is quite logical to see these complex cases presented at the clinic. No correlation could be made between the disease that was diagnosed in the cats and the presence of osteoarthritis. A point of discussion is the evaluation of the radiographs. In total 471 radiographs were graded for osteoarthritis. Over time, the gradation became increasingly easy, because of developed experience. Therefore it might be possible that subtle signs of osteoarthritis were missed at the beginning of the study. However, a diagnostic imaging specialist was always available to help with the interpretation of radiographs in case of doubt. During the evaluation of the obtained radiographic material, it was noticed that not all of the descriptions of radiographic signs described in the first part of this report could be evaluated as such. Part of this can be explained by the radiographic material itself, because these radiographs were mostly taken for non-orthopaedic assessment and not for the joints in question. Irregularity of the joint and osteophyte formation could be seen, in most cases, where dorsoventral and dextrosinistral images were present for comparison. Articular cartilage destruction can not be seen on the radiographic material, but only on for example MRI images or at necropsy. Subchondral bone sclerosis was not seen and was also often difficult to assess, because of the abdominal or thoracic focus of the radiograph. The main used criteria for the osteoarthritic changes graded in these data were therefore the presence of osteophytes and irregularity of the joint surfaces. The visible shoulder and hip joints on the obtained radiographic images consisted of 238 visible pairs of shoulders and 57 pairs of hips. Based on the assumption that osteoarthritis more often occurs bilaterally than unilaterally in shoulders and hips, data was only included if both shoulders or both hips were visible on the radiographs and gradable. Because the data often had only one visible elbow, stifle, tarsus or carpus on the radiograph, these joints were not assessed in pairs. From the 89 cases in which at least one elbow was visible, only in 37 cases a second elbow was present. This was also the case for the stifles, in which both stifles were present in only 16 out of 34 cases in which at least one stifle was present. Carpi and tarsi were scarce on radiographic material. Only 2 cases with one carpus and 7 cases with one tarsus were seen. No statistical analysis could be performed with these 29 - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 low numbers. Therefore no conclusions could be made from the data of the carpi and tarsi with regard to risk factors and prevalence. This also accounts for stifle 2, for which only 16 stifles were available. Conclusion In conclusion the objective in this research project was to investigate the prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat, as it is thought to be higher as yet recognized. After this report and the retrospective evaluation of 471 radiographs it seems that osteoarthritis is more common in cats than thought before. The significance of this finding is unclear, because most of the cats do not show symptoms of this disease or the symptoms aren’t recognised. More research has to be done, to find out what the clinical relevance of osteoarthritis in cats is. A total prevalence of osteoarthritis in cats of 36.7% was found. Several risk factors, (c.q. breed, age, weight, gender, trauma and diagnosis) were analysed and only age seems to be a significant factor in osteoarthritis. In both shoulder joints, the elbows and the stifles a significant correlation was established between osteoarthritis and age. Conclusion of this investigation is that osteoarthritis is more common in elderly cats. This is confirmed by other researchers, for example by Bennet et al and by Clarke et al (4,9). A remarkable finding in this report is that no significant correlation could be found between age and osteoarthritis in the hips, which might suggest that hip osteoarthritis may be more of a problem in younger cats because of inheritable causes. Another remarkable finding of this report is the fact that there is a positive relation between the presence of osteoarthritis in one shoulder and in the contralateral shoulder of the cats. The same relationship was found for the hip joints. This report confirms that elderly cats are at greater risk of developing or having osteoarthritic changes. Acknowledgements The author would like to thank the department of Diagnostic Imaging of the University Clinic for Companion Animals in Utrecht for making the radiographic images available for use in this report. Special thanks goes out to prof. dr. G. Voorhout and drs. E. Auriemma for discussion of the findings and assessment of radiographic material. The author also would like to thank dr. L.I. Slingerland for the daily supervision, critical analysis of this report and the help with the statistical analysis. At last the author would like to thank prof.dr. H.A.W. Hazewinkel for overall supervision and critical analysis of this report. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 30 Literature 1. Allan G.S. Small Animal Practice, clinical radiology: Radiographic features of feline joint diseases. Veterinary Clinical Small Animal. Practice 2000; 2: 281-302. 2. Beale, B.S. Use of nutraceuticals and chondroprotectants in osteoarthritic dogs and cats. Veterinary Clinics of Small Animal Practice 2004; 34: 271-289. 3. Beale, B.S. Orthopedic Problems in Geriatric Dogs and Cats. Veterinary Clinics of Small Animal Practice 2005; 35: 655-674. 4. Bennett D, Clarke S. Feline osteoarthritis. University of Glasgow Veterinary School, ESVOT Congress, Munich; September 2004. 5. Bennet D. Arthritis, its classification, pathogenesis and clinical relevance. Tijdschrift voor Diergeneeskunde 1993; 118: 19S-23S. 6. Brinker W.O, Piermattei D.L, Flo G.L. Chapter 17: Cartilage and Joint Abnormalities. In: Brinker W.O, Piermattei D.L, Flo G.L. Handbook of Small Animal Orthopedics & Fracture Treatment, 2nd ed. 1990: 285-304. 7. Caney S. Feline Arthritis. Veterinary Focus 2007; 17 (3): 11-17. 8. Clarke S.P, Bennet D. Feline osteoarthritis: a prospective study of 28 cases. Journal of Small Animal Practice. 2006; 47: 439-445. 9. Clarke S, Mellor D, Clements D.N, Gemmil T, Farrell M, Carmichael S, Bennet D. Prevalence of radiographic signs of degenerative joint disease in a hospital population of cats. Veterinary Record. 2005; 157: 793-799. 10. Gastel-Jansen, A. van. Radiographs of skeletal diseases in small animals, 1st ed. 1978, Veterinary Faculty University of Utrecht: 11. 11. Ghadially F.N. Chapter 11: Ageing and osteoarthrotic changes in articular cartilage. In: Ghadially F.N. Fine Structure of Synovial Joints, A text and atlas of the ultrastructure of normal and pathological articular tissues, 1st ed. 1983: 236-260. 12. Godfrey D.R. Osteoarthritis in cats: a retrospective radiological study. Journal of Small Animal Practice 2005; 46: 425-429. 13. Gunew, M.N, Menrath V.H, Marshall R.D. Long-term safety, efficacy and palatability of oral meloxicam at 0.01e0.03 mg/kg for treatment of osteoarthritic pain in cats. Journal of Feline Medicine and Surgery 2008; doi:10.1016/j.jfms.2007.10.007. 14. Gunn-Moore D, Considering older cats. Journal of Small Animal Practice 2006; 47: 430. 15. Hans T, Latimer K.S, LeRoy B.E, Bain P.J, Tarpley H.L. Synovial Fluid Findings in Degenerative Joint Disease. Veterinary Clinical Pathology Clerkship Program College - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 31 of Veterinary Medicine, University of Georgia. 2004. 16. Hall L.W., Clarke K.W, Trim C.M. Chapter 1: General Considerations. In: Hall L.W., Clarke K.W, Trim C.M. Veterinary Anesthesia 10th ed. 2001: 15-16. 17. Hardie E.M, Roe C, Fonda M.R. Radiographic evidence of degenerative joint disease in geriatric cats: 100 cases (1994-1997). Journal of the American Veterinary Medical Association. 2002; 220(5): 628-632. 18. Hardie E.M. Small Animal Practice, osteoarthritis: Management of osteoarthritis in cats. Veterinary Clinical Small Animal Practice 1997; 27 (4): 945-953. 19. Hardie E.M. Chapter 4: Recognition of pain behaviour in animals. In: Hellebrekers J.M., Animal Pain 1st ed. 2000: 51-69. 20. Kamishina H, Miyabayashi T, Clemmons R.M, Farese J.P, Uhl E.W, Silver X. High Field (4.7T) Magnetic Resonance Imaging of Feline Hip Joints. Journal of Veterinary Medical Science 2006; 68 (3): 285-288. 21. Kamishina H. “Degenerative Joint Disease of the hip in cats: imaging, pathologic and in vitro studies.” Abstract in Veterinary Radiology & Ultrasound. 2003; 44(6): 743 22. Lascelles B.D.X, Hansen B.D, Roe S, et al. Evaluation of Client-Specific Outcome Measures and Activity Monitoring to Measure Pain Relief in Cats with Osteoarthritis. Journal of Veterinary Internal Medicine 2007; 21: 410-416. 23. Mathews K.A. Chapter 8: Management of pain in cats. In: Hellebrekers J.M., Animal Pain 1st ed. 2000: 131-144. 24. May S.A. Chapter 5: Degenerative joint disease (osteoarthritis, osteoarthrosis, secondary joint disease). In: Houlton J.E.F, Collinson R.W. Manual of small animal arthrology, British Small Animal Veterinary Association, 1st ed. 1994: 62-74. 25. Morgan J.P. Chapter 3: the joints, osteoarthrosis. In: Morgan J.P Radiology in Veterinary Orthopedics, 1 ed.1972: 183-193. 26. Nelson R.W, Couto C.G. Chapter 76: Disorders of the joints. In: Nelson R.W, Couto C.G. Small Internal Medicine, 3rd ed. 2003: 1079-1081. 27. Newton C.D, Lipowitz A.J. Chapter 87:Degenerative Joint Disease and Traumatic. In: Newton C.D, Nunamaker D.M. Textbook of small animal orthopaedics, 1st ed. 1985: 1029-1045. 28. Owens J.M. Chapter 3: the joints. In: Owens J.M. Radiographic Interpretation for the Small Animal Clinician, 1st ed. 1982: 25-51. 29. Pederson N.C. Canine joint disease. Scientific Proceedings, 45th Annual Meeting of the American Animal Hospital Association, 1978: 359-366. - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 32 30. Renberg W.C. Small Animal Practice: Pathophysiology and Management of Arthritis. Veterinary Clinical Small Animal Practice. 2005; 35: 1073-1091. 31. Romich, J.A, Degenerative Joint Disease in Small Animal Practice. Veterinary Technician 1994; 15 (6): 297-303. 32. Scott H.W, McLaughlin R. Chapter 7: Arthrology. In: Scott H.W, McLaughlin R. Feline Orthopedics, 1st ed. 2007: 87-94. 33. Scott H.W. Current medical therapies for canine and feline osteoarthritis. Veterinary Focus 2007; 17 (3): 18-23. 34. Shires P.K, Tilley L.P, Smith W.K. The 5-minute veterinary consult, Canine and Feline Specialty Handbook Musculoskeletal Disorders, 1st ed. 2006: 9-18. 35. Thrall D.E. Chapter 18: radiographic signs of joint disease in dogs and cats. In: Thrall D.E. Textbook of veterinary diagnostic radiology, 5th ed. 2007: 330-332. 36. Wolf A.C. Degenerative Joint Disease in cats. Texas University Proceeding LAVC 2007. 37. Bureau Registratie Diergeneesmiddelen, http://www.cbg-meb.nl 38. FIDIN Repertorium, www.fidin.nl 39. Pubmed, http://www.ncbi.nlm.nih.gov/sites/entrez/ 40. Vetportal, http://vetportal.library.uu.nl/portal.html 41. International Veterinary Information Service, www.ivis.org 42. Library collection of Veterinary Medicine, University of Utrecht, www.library.uu.nl 43. Conference Proceedings Hill’s Global mobility symposium, www.HillsVet.com/ConferenceProceedings - “Prevalence of osteoarthritis in the joints of the appendicular skeleton of the cat” M.Verruijt, 2008 33