Surgical Pathology Unknown Conference
advertisement
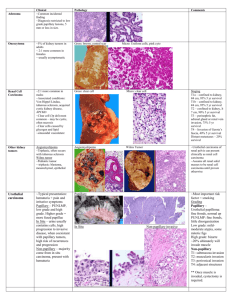
Surgical Pathology Unknown Conference: Case # 1: A 68 year old man presented with hematuria. Upon cystoscopy, a 5 cm ulcerated mass was found. A transurethral resection (TUR) was performed. Diagnosis: 1- Invasive High Grade Urothelial Carcinoma. 2- Small Cell Carcinoma. 3- Secondary Extension of Prostatic Adenocarcinoma . 4- Paraganglioma. Histology: The infitrative lesion is well vascularized showing a vaguely nested appearance. It is composed of large round to polygonal cells with abundant amphophilic granular cytoplasm and modest degree of nuclear pleomorphism. Mitotic figures are lacking. Necrosis was not present. Immunostains reveal positive reactivity for chromogranin and synaptophysin. Focal S100 reactivity was seen. Cytokeratin AE1/AE3 stains were negative. Discussion: Paragagliomas of the urinary bladder are rare tumors that can be misdiagnosed as urothelial carcinoma due to their infiltrative nature, occasionally diffuse architecture and confounding cautery artifact encountered on TUR. Rarely, the lesion is clinically suspected either due to associated symptoms such as hypertension, episodic palpitation/headache on micturition or due to lack of a typical cystscopic appearance of urothelial carcinoma. Making such a distinction is of great importance given the potential differences in prognosis and management between paraganglioma and muscle invasive high grade urothelial carcinoma. Morphologic features such as the presence of focal more typical Zellballen pattern and rich fibrovascular network and the lack of desmoplastic reaction accompanying muscularis propria invasion should raise the possibility of paraganglioma. Immunostains for neuroendocrine markers , S100 (sustentacular pattern) and cytokeratins (-) can help establish the diagnosis. In general, several syndromes have been found to be associated with the risk of development of pheochromocytomas/paragangliomas. These include: multiple endocrine neoplasia type 2 (MEN 2, susceptibility gene: RET), von Hippel-Lindau disease (VHL, susceptibility gene: VHL), neurofibromatosis 1 (NF 1), and paraganglioma syndromes type 1, 3, and 4 (susceptibility genes: succinate dehydrogenase gene, SDH, subunits D, C and B, respectively). Reference: Zhou M, Epstein JI, Young RH. Paraganglioma of the urinary bladder: a lesion that may be misdiagnosed as urothelial carcinoma in transurethral resection specimens. Am J Surg Pathol. 2004 Jan;28(1):94-100. Pawlu C, Bausch B, Reisch N, Neumann HP. Genetic testing for pheochromocytoma-associated syndromes. Ann Endocrinol (Paris). 2005 Jun;66(3):178-85. Case # 2: A 36 year old man underwent a radical nephrectomy for a 32 cm renal mass. On imaging studies, the tumor extended to the retropertineum with secondary metastasis to liver and lung. Diagnosis: 1- Renal Cell Carcinoma with Sarcomatoid Features. 2- Urothelial Carcinoma with Sarcomatoid Features. 3- Dedifferentiated Liposarcoma. 4- Malignant Solitary Fibrous Tumor. Histology: On Low power examination, the relatively well circumscribed tumor demonstrates variable degree of cellularity. Areas of geographic necrosis are easily found. Less cellular areas are composed of relatively bland spindle cells separated by parallel bands of thick collagen featuring a “hemangiopercytoma” like vascular pattern. The densely cellular areas show plump, epithelioid, spindle cells with markedly increased mitotic activity and necrosis. The tumor only focally invaded the renal parenchyma. On immunostains, the tumor cells were positive for CD34 and negative for Actin, CD99, EMA, AE1/AE3, CAM 5.2 and S100. Discussion: Solitary fibrous tumors (SFT) have been reported to rarely originates in renal parenchyma, renal capsule and renal pelvis. Although the current example demonstrated frank histologic features consistent with its clinically mailgnant behavior, other renal SFT’s lacking increased cellularity, pleomorphism, mitotic activity and necrosis are expected to behave in a benign fashion. Therefore, distinguishing an SFT from the more common sarcomatoid renal cell carcinoma is crucially important. The differential of a renal spindle cell tumor should also include monophasic angiomyolipoma, leiomyosarcoma and the rare synovial sarcoma. Immunostains are helpful in confirming a histologic impression of SFT by demonstrating its typical CD34 (+), Bcl2 (+) and SMA (-) phenotype. References: Wang J, Weiss LM, Hu B, Chu P, Zuppan C, Felix D, Rausei-Mills V, Chase DR. Usefulness of immunohistochemistry in delineating renal spindle cell tumours. A retrospective study of 31 cases. Histopathology. 2004 May;44(5):462-71. Wang J, Arber DA, Frankel K, Weiss LM. Large solitary fibrous tumor of the kidney: report of two cases and review of the literature. Am J Surg Pathol. 2001 Sep;25(9):1194-9. Case # 3: A 16 year old male presented with a left testicular mass. A partial orchiectomy was performed. Diagnosis: 1- Endodermal Sinus Tumor. 2- Fibrous Pseudotumor. 3- Mesothelioma. 4- Adenomatoid Tumor. Histology: The 1.8 cm lesion is primarily composed of a dense fibrous tissue with a relatively more cellular central area composed of stellate to spindle cells with features of myofibrobalsts. Vascular structures lined by plump endothelial cells without significant cytologic atypia are present. A modest mixed inflammatory infiltrate is associated, The well circumscribed lesion originates in the tunica albuginea. Underlying testicular parenchyma is spared. No evidence of intratubular germ cell neoplasia is seen. Discussion: Fibrous pseudotumors and proliferative funniculitis (inflammatory pseudotumors) are considered by many as part of a spectrum of non-neoplastic fibroblastic/myofibroblastic proliferations that affects the tunica and paratesticular region. Some examples may demonstrate a pseudosacromatous morphology . Others are almost completely fibrotic and collagenized with associated calcifications. Fibrous pseudotumors can present as multiple nodules and at times as free-lying scrotal masses (corpora libra). They are usually associated with a history of hydrocele or prior trauma or infection. Fibrous and inflammatory pseudotumors are to be distinguished from “fibroma of tunica albuginea” that can carry some morphologic and immunohistochemical (CD34 positivity) resemblance to solitary fibrous tumors of other site. References: Begin LR, Frail D, Brzezinski A. Myofibroblastoma of the tunica testis: evolving phase of so-called fibrous pseudotumor? Hum Pathol. 1990 Aug;21(8):866-8. Jones MA, Young RH, Scully RE. Benign fibromatous tumors of the testis and paratesticular region: a report of 9 cases with a proposed classification of fibromatous tumors and tumor-like lesions. Am J Surg Pathol. 1997 Mar;21(3):296-305. Case # 4: A 60 year old underwent a radical nephrectomy for two separate renal masses each measuring 3 cm in largest diameter. Both tumors shared similar morphologic features. Diagnosis: 1- Epithelioid Angiomyolipoma. 2- Oncocytoma. 3- Hybrid Oncocytic Neoplasm with Oncocytoma and Chromophobe Renal Cell Carcinoma Components. 4- Medullary Carcinoma of Kidney. Histology: Both tumors were composed of an oncocytic epithelial proliferation arranged in solid islands and nests. Focal hyalinized - edematous stroma separating the epithelial islands is seen as characteristically found in renal oncocytomas. In the latter areas, the epithelial cells contain typical round variable sized nuclei with one or more small nucleoli. In other areas, cytologic features of chromophobe cell carcinoma are demonstrated to include the presence of “raisinoid” nuclear morphology imparted by the irregular nuclear membranes and the existence of a vague perinuclear halo. Mitotic figures are absent. Oncocytosis was not present in the submitted non neoplastic kidney. Discussion: Hybrid oncocytic renal neoplasms may be encountered in the setting of Birt-Hogg-Dube (BHD) syndrome. BHD is an autosomal dominant genodermatosis characterized by the development of benign hair follicle tumors (fibrofolliculomas), an increased risk of renal neoplasia and spontaneous pneumothorax. BHD patients can develop multiple, at time bilateral renal tumors with variable morphology to include hybrid oncocytic neoplasms , chromophobe renal cell carcinomas and conventional clear cell carcinomas. In most patients, the non neoplastic renal parenchyma reveals microscopic evidence of “oncocytoisis”. The BHD gene is mapped to chromosome 17p11.2. It encodes a novel protein of yet unknown function (follicullin). Relatives of affected individual can be tested for the presence of a germline BHD mutation to determine if they are at increased risk to develop renal malignancies. References: Pavlovich CP, Grubb RL 3rd, Hurley K, Glenn GM, Toro J, Schmidt LS, Torres-Cabala C, Merino MJ, Zbar B, Choyke P, Walther MM, Linehan WM. Evaluation and management of renal tumors in the Birt-Hogg-Dube syndrome. J Urol. 2005 May;173(5):1482-6. Pavlovich CP, Walther MM, Eyler RA, Hewitt SM, Zbar B, Linehan WM, Merino MJ. Renal tumors in the Birt-Hogg-Dube syndrome. Am J Surg Pathol. 2002 Dec;26(12):1542-52. Case # 5: A 42 year old male underwent a circumcision after a long history of phimosis. Diagnosis: 1. 2. 3. 4. Squamous Intraepithelial Lesion, Low Grade. Warthy Squamous Intraepithelial Lesion (WSIL), High Grade. Ballanitis Circumscripta Plasmacellularis (Zoon Balanitis). Balanitis Xerotica Obliterans (Lichen Sclerosis et Atrophicus). Histology: The epidermis demonstrates focal marked hyperkeratosis and acanthosis. Hydropic degeneration is focally present in the basal layer imparting a vacuolar change at the DE junction. The superficial portion of the lamina propria shows marked edema and homogenization of collagen. A mixed dermal inflammatory infiltrate is seen. There is no evidence of squamous dysplasia. Discussion: Balanatis Xerotica Obliterans (BXO) is a frequent finding in specimens obtained for phimosis. Although the relationship of BXO to carcinoma is not entirely clear, BXO lesions can be found in 30-70% of penile squamous carcinoma resections. The association seems to be stronger with special types of carcinoma such as papillary and verrucous penile carcinoma. Dysplastic or CIS changes can rarely be seen in the epidermis of hyperplastic BXO. References: Velazquez EF, Cubilla AL. Lichen sclerosus in 68 patients with squamous cell carcinoma of the penis: frequent atypias and correlation with special carcinoma variants suggests a precancerous role. Am J Surg Pathol. 2003 Nov;27(11):1448-53. Case # 6: A 59 year old female presented with hematuria. A cystoscopy and transurethral resection was performed. Diagnosis: 1. 2. 3. 4. Diffuse Large B Cell Lymphoma. Small Cell Carcinoma. Lymphoepithelioma Like Carcinoma (LELC) of Urinary Bladder. Severe Chronic Follicular Cystitis. Histology: The epithelial neoplasm is composed of a proliferation of undifferentiated highly atypical cells arranged in a syncitial pattern with indistinct cytoplasmic borders. Characteristic of LELC, the epithelial cells contain large vesicular nuclei with very prominent nucleoli. The latter is associated with a dense obscuring lymphoid infiltrate. The lymphoid cells are smaller in size. Mitotic figures are easily identified. The tumor extensively invades the muscularis propria. The surface urothelium show no evidence of flat carcinoma in situ (CIS). Discussion: LELC is a rare type of urinary bladder carcinoma. The associated dense lymphoid host response could lead to a misdiagnosis of such lesions as malignant lymphoma especially on small TUR biopsies with extensive cautery artifact. Immunostains for cytokeratins AE1/AE3, CK7 and EMA could be of help in such cases. The lymphoid infiltrate is usually composed of a mixture of B and T cells. Unlike their nasopharyngeal counterparts, EBV studies for LMP1 and EBER have been shown to be negative in LELC of bladder. Distinguishing bladder tumors with pure or predominant LELC morphology from other undifferentiated and high grade urothelial carcinoma may have implications on patient management given the relatively higher chemotherapy response rates and the potentials for bladder salvage. References: Lopez-Beltran A, Luque RJ, Vicioso L, Anglada F, Requena MJ, Quintero A, Montironi R. Lymphoepithelioma-like carcinoma of the urinary bladder: a clinicopathologic study of 13 cases. Virchows Arch. 2001 Jun;438(6):552-7. Amin MB, Ro JY, Lee KM, Ordonez NG, Dinney CP, Gulley ML, Ayala AG. Lymphoepithelioma-like carcinoma of the urinary bladder. Am J Surg Pathol. 1994 May;18(5):466-73.